Evaluation of Brace Treatment Using the Soft Brace Spinaposture: A Four-Years Follow-Up
Abstract
1. Introduction
2. Materials and Methods
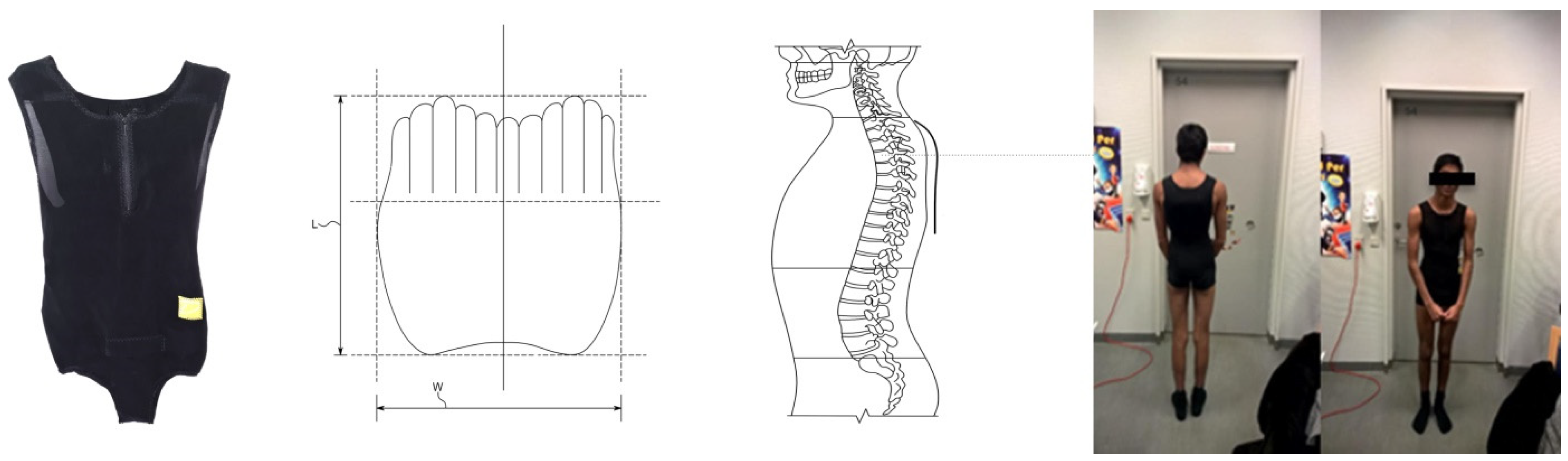
2.1. Inclusion, Bracing and Strengthening Exercises
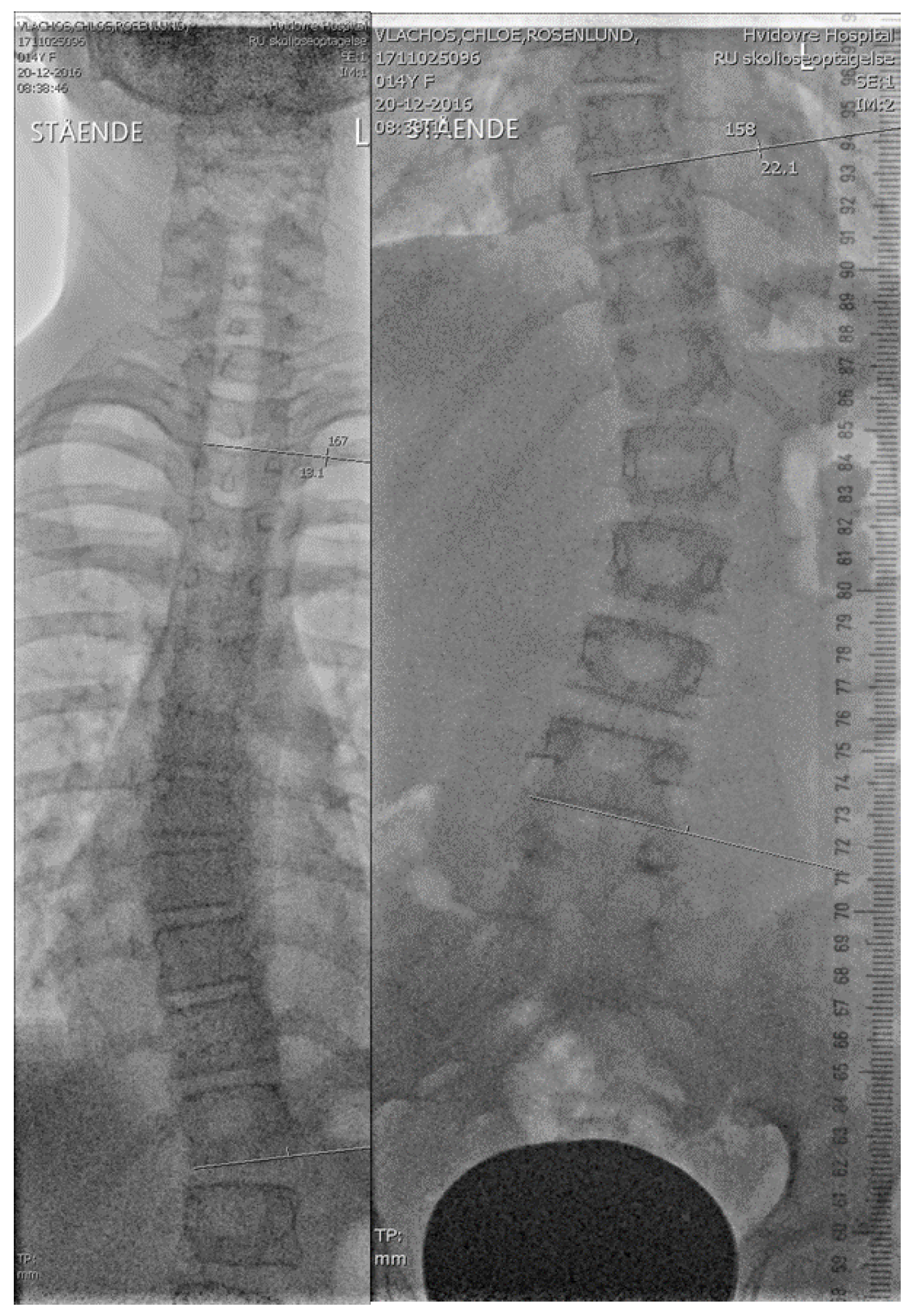
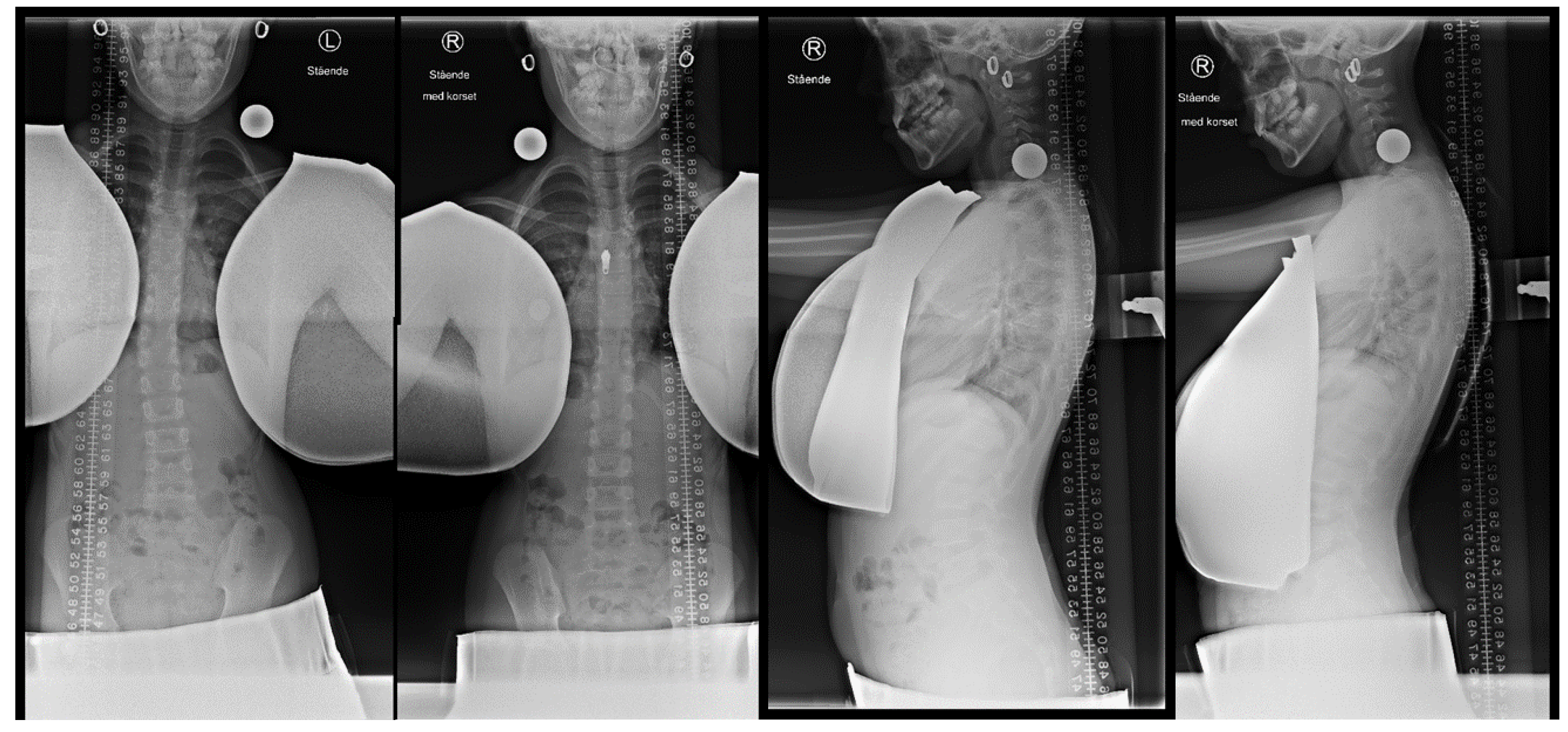
2.2. Initial in-Brace Radiographs
2.3. Outpatient Follow-Up
2.4. Study Assessments and Statistical Analyses
3. Results
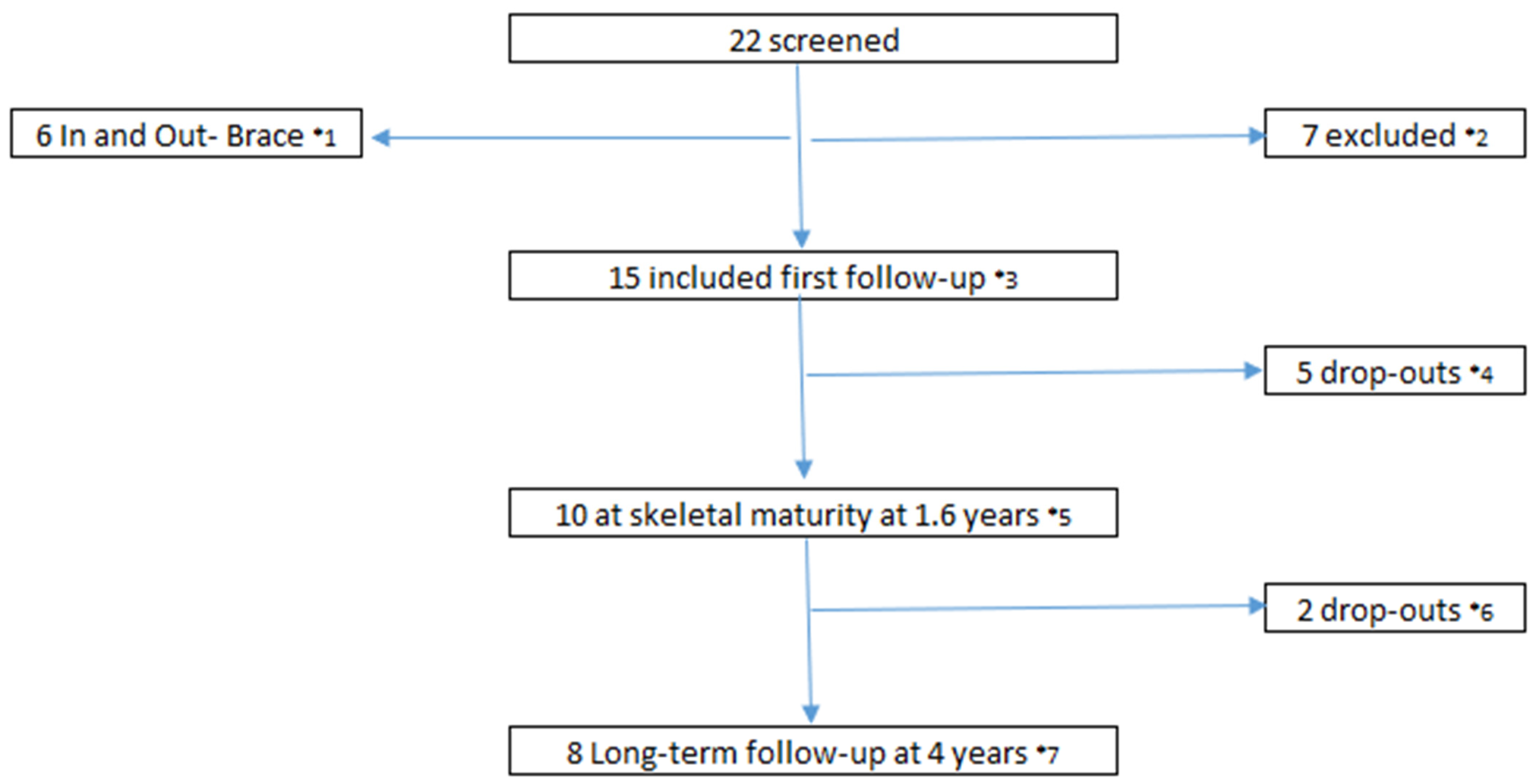
3.1. Population
3.2. In-Brace Correction
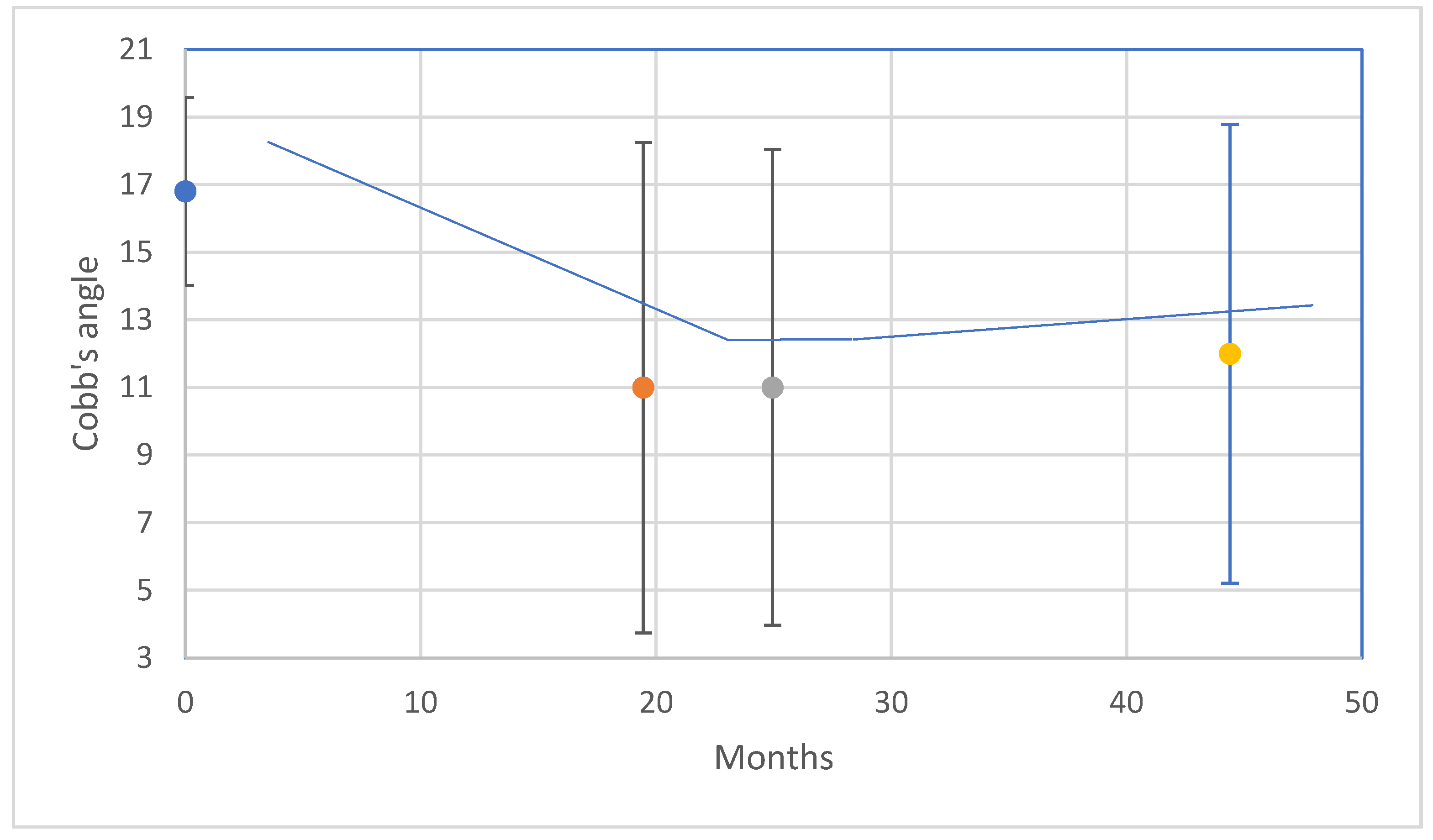
3.3. Follow-Up Study
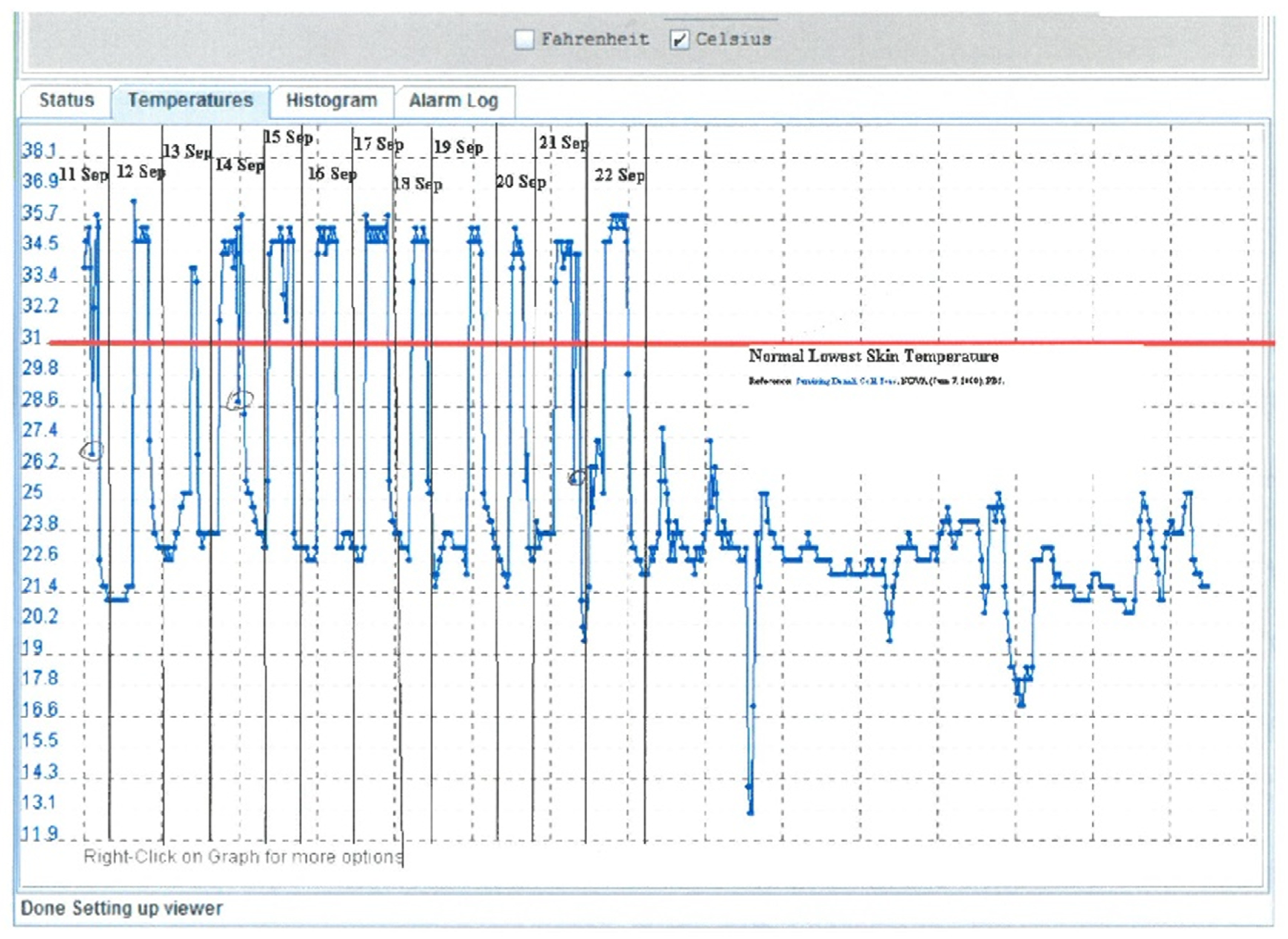
3.4. Brace Compliance and Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Zaina, F. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst. Rev. 2015, 6, CD006850. [Google Scholar] [CrossRef]
- Weiss, H.-R. Is there a body of evidence for the treatment of patients with Adolescent Idiopathic Scoliosis (AIS)? Scoliosis 2007, 2, 19. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.; Wright, J.G.; Dobbs, M.B. Effects of Bracing in Adolescents with Idiopathic Scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef]
- Nachemson, A.L.; Peterson, L.E. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J. Bone Jt. Surg. Am. 1995, 77, 815–822. [Google Scholar] [CrossRef]
- Wiley, J.W.; Thomson, J.D.; Mitchell, T.M.; Smith, B.G.; Banta, J.V. Effectiveness of The Boston Brace in Treatment of Large Curves in Adolescent Idiopathic Scoliosis. Spine 2000, 25, 2326–2332. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Grivas, T.B. Introduction to the “Scoliosis” Journal Brace Technology Thematic Series: Increasing existing knowledge and promoting future developments. Scoliosis 2010, 5, 2–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rivett, L.; Rothberg, A.; Stewart, A.; Berkowitz, R. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathic scoliosis: A comparative study. BMC Musculoskelet. Disord. 2009, 10, 5. [Google Scholar] [CrossRef]
- Reichel, D.; Schanz, J. Developmental psychological aspects of scoliosis treatment. Pediatr. Rehabil. 2003, 6, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Dolan, L.A.; Wright, J.G.; Weinstein, S.L. Correspondence: Effects of Bracing in Adolescents with Idiopathic Scoliosis. N. Engl. J. Med. 2014, 370, 680–681. [Google Scholar] [CrossRef]
- Davies, E.; Norvell, D.; Hermsmeyer, J. Efficacy of bracing versus observation in the treatment of idiopathic scoliosis. Evid. Based Spine Care J. 2011, 2, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, C.J.; Moore, D.P.; Fogarty, E.E.; Dowling, F.E. Adolescent Idiopathic Scoliosis: The effect of brace treatment on the incidence of surgery. Spine 2001, 26, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.-R.; Werkmann, M. Soft braces in the treatment of Adolescent Idiopathic Scoliosis (AIS)—Review of the literature and description of a new approach. Scoliosis 2012, 7, 11, Retraction: Scoliosis 2013, 8, 7. [Google Scholar] [CrossRef]
- Costa, L.; Schlosser, T.P.C.; Jimale, H.; Homans, J.F.; Kruyt, M.C.; Castelein, R.M. The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 2145. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.-R. SpineCor vs. natural history—Explanation of the results obtained using a simple biomechanical model. Stud. Health Technol. Inform. 2008, 140, 133–136. [Google Scholar] [PubMed]
- van Loon, P.J.M.; Kühbauch, B.A.G.; Thunnissen, F.B. Forced Lordosis on the Thoracolumbar Junction Can Correct Coronal Plane Deformity in Adolescents with Double Major Curve Pattern Idiopathic Scoliosis. Spine 2008, 33, 797–801. [Google Scholar] [CrossRef]
- Weiss, H.-R.; Tournavitis, N.; Seibel, S.; Kleban, A. A Prospective Cohort Study of AIS Patients with 40° and More Treated with a Gensingen Brace (GBW): Preliminary Results. Open Orthop. J. 2017, 11, 1558–1567. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Fusco, C.; Minozzi, S.; Atanasio, S.; Zaina, F.; Romano, M. Exercises reduce the progression rate of adolescent idiopathic scoliosis: Results of a comprehensive systematic review of the literature. Disabil. Rehabil. 2008, 30, 772–785. [Google Scholar] [CrossRef] [PubMed]
- Adams, W. Lectures on the Pathology and Treatment of Lateral and Other Forms of Curvature of the Spine; Churchill: London, UK, 1882, 2nd ed. Available online: https://wellcomecollection.org/works/qc5xzydx (accessed on 1 December 2021).
- Wong, C. Mechanism of right thoracic adolescent idiopathic scoliosis at risk for progression; a unifying pathway of development by normal growth and imbalance. Scoliosis 2015, 10, 1–5. [Google Scholar] [CrossRef]
- Donzelli, S.; Zaina, F.; Negrini, S. End growth results analysis related to Risser score, Cobb degrees, and curve types at the beginning of the treatment. Scoliosis 2013, 8, O10. [Google Scholar] [CrossRef][Green Version]
- Coillard, C.; Circo, A.B.; Rivard, C.H. A prospective randomized controlled trial of the natural history of idiopathic scoliosis versus treatment with the SpineCor brace. Sosort Award 2011 winner. Eur. J. Phys. Rehabil. Med. 2014, 50, 479–487. [Google Scholar] [CrossRef][Green Version]
- Kouwenhoven, J.-W.M.; Smit, T.H.; van der Veen, A.J.; Kingma, I.; van Dieën, J.H.; Castelein, R.M. Effects of Dorsal Versus Ventral Shear Loads on the Rotational Stability of the Thoracic Spine: A biomechanical porcine and human cadaveric study. Spine 2007, 32, 2545–2550. [Google Scholar] [CrossRef]
- Lomax, M.; Tasker, L.; Bostanci, O. An electromyographic evaluation of dual role breathing and upper body muscles in response to front crawl swimming. Scand. J. Med. Sci. Sports 2014, 25, e472–e478. [Google Scholar] [CrossRef]
- Wong, C.; Adriansen, J.; Jeppsen, J.; Balslev-Clausen, A. Intervariability in radiographic parameters and general evaluation of a low-dose fluoroscopic technique in patients with idiopathic scoliosis. Acta Radiol. Open 2021, 10. [Google Scholar] [CrossRef]
- Langensiepen, S.; Semler, O.; Sobottke, R.; Fricke, O.; Franklin, J.; Schönau, E.; Eysel, P. Measuring procedures to determine the Cobb angle in idiopathic scoliosis: A systematic review. Eur. Spine J. 2013, 22, 2360–2371. [Google Scholar] [CrossRef]
- Moe, J.H.; Kettleson, D.N. Idiopathic scoliosis. Analysis of curve patterns and the preliminary results of Milwau-kee-brace treatment in one hundred sixty-nine patients. J. Bone Jt. Surg. Am. 1970, 52, 1509–1533. [Google Scholar] [CrossRef]
- Rahman, T.; Borkhuu, B.; Littleton, A.G.; Sample, W.; Moran, E.; Campbell, S.; Rogers, K.; Bowen, J.R. Electronic monitoring of scoliosis brace wear compliance. J. Child. Orthop. 2010, 4, 343–347. [Google Scholar] [CrossRef]
- Panjabi, M.M.; Brand, R.A., Jr.; White, A.A., 3rd. Mechanical properties of the human thoracic spine as shown by three-dimensional load-displacement curves. J. Bone Jt. Surg. Am. 1976, 58, 642–652. [Google Scholar] [CrossRef]
- Simony, A.; Hansen, E.J.; Christensen, S.B.; Carreon, L.Y.; Andersen, M.Ø. Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur. Spine J. 2016, 25, 3366–3370. [Google Scholar] [CrossRef] [PubMed]
- Knott, P.; Pappo, E.; Cameron, M.; Demauroy, J.C.; Rivard, C.; Kotwicki, T.; Zaina, F.; Wynne, J.; Stikeleather, L.; Bettany-Saltikov, J.; et al. SOSORT 2012 consensus paper: Reducing X-ray exposure in pediatric patients with scoliosis. Scoliosis 2014, 9, 4. [Google Scholar] [CrossRef]
- Zhang, Y.; Hedo, R.; Rivera, A.; Rull, R.; Richardson, S.; Tu, X.M. Post hoc power analysis: Is it an informative and meaningful analysis? Gen. Psychiatry 2019, 32, e100069. [Google Scholar] [CrossRef]
- Soucacos, P.N.; Zacharis, K.; Gelalis, J.; Soultanis, K.; Kalos, N.; Beris, A.; Xenakis, T.; Johnson, E.O. Assessment of curve progression in idiopathic scoliosis. Eur. Spine J. 1998, 7, 270–277. [Google Scholar] [CrossRef] [PubMed]
| Pt *1 | Age *2 | Sex *3 | Risser | Mena *4 | Type of Scoliosis *7 | AIS Events *8 | MR col. *9 | CA FV *14 | CA SM *15 | CA LT *16 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14.6 | male | 2 | - *5 | high de-TS | - | - | 9.6 | 6.85 | 9.1 |
| 2 | 9.1 | fem | 0 | 12.2 | high de-TS | Back pain *10 | MR ia *13 | 10.85 | 16.5 | 14.9 |
| 3 | 14.8 | fem | 1 | 15.7 | s-s de-TLS | Anisomelia *11 | - | 1.3 | 3.7 | 0.65 |
| 4 | 13.9 | male | 1 | - *5 | de-TLS | - | - | 7.4 | −0.7 | −2.3 |
| 5 | 10.9 | fem | 1 | 12 | s-s de-TLS | - | - | 1.45 | 4.95 | 6.05 |
| 6 | 15.2 | male | 2 | - *5 | low de-TLS | - | - | 3.75 | - | - |
| 7 | 9.7 | fem | 0 | pm *6 | s-s de-TLS | - | - | 4.2 | 4.4 | −0.35 |
| 8 | 13.5 | fem | 0 | 14.4 | s-s de-TLS | Back pain *12 | MR ia *13 | 0.8 | - | - |
| 9 | 15.1 | fem | 1 | 15.3 | low de-TS | - | - | 2.45 | - | |
| 10 | 14.6 | fem | 2 | 15.5 | low de-TS | - | - | 2.7 | 3.8 | - |
| 11 | 7.2 | fem | 0 | pm *6 | s-s ju-deTLS | - | - | 3.5 | 1.4 | - |
| 12 | 12.8 | fem | 0 | 13.6 | s-s de-TLS | - | - | 4.45 | −3.8 | −0.1 |
| 13 | 11.5 | fem | 0 | 13 | C si-TLS | - | - | 2.2 | −0.4 | −3.25 |
| 14 | 7 | male | 0 | - *5 | C ju-deTLS | - | - | 14.4 | - | - |
| 15 | 15.2 | fem | 2 | 14.8 | s-s de-TLS | Back pain | MR *13 | 4.9 | - | - |
| Achieved in the Present Study | Expected Number of “Improved/Straight” or “Stable” * | ||||
|---|---|---|---|---|---|
| Risser | N | Improved/Straight | Stable | Improved/Straight or Stable | |
| 0–1 | 11 | 5 | 6 | 11 | 6 (42%) |
| 0–2 | 15 | 6 | 9 | 15 | 9 (71%) |
| Pt *1 | Time in Brace *2 | DM/C *3 | A.Ver. *4 | Metha.A. *5 | NashMoe *6 |
|---|---|---|---|---|---|
| 1 | 12.3 | →straight | Th3→Th12 | 13.4 | 0→0 |
| 2 | 36.6 | →straight | Th4→Th5 | 5.9 | 0→0 |
| 3 | 28.8 | →straight | Th5 | 6.2 | 0→0 |
| 4 | 13.7 | deTLS | Th12→Th11 | 14.9 | 0→0 |
| 5 | 22.3 | →straight | Th12→Th11 | 11.4 | 0→0 |
| 6 | 6.8 | low de-TLS | Th8→Th10 | 4.5 | 0→0 |
| 7 | 24.7 | →straigh | Th9 | 1.5 | 0→0 |
| 8 | 8.3 | s-s TL | Th9 | 7.3 | 1→1 |
| 9 | 7.1 | low dTS | Th10 | 11 | 0→1 |
| 10 | 16.7 | low dTS | Th9 | 11.3 | 0→0 |
| 11 | 12.6 | →straight | Th9→Th10 | 19.5 | 0→0 |
| 12 | 12.8 | s-s de-TLS | Th12 | 10.4 | 0→0 |
| 13 | 34 | C si-TLS | Th10 | 21.2 | 0→1 |
| 14 | 4.5 | C ju-deTLS | Th12→Th11 | 27.8 | 0→1 |
| 15 | 8.1 | s-s de-TLS | Th10 | 13.4 | 0→0 |
| Pt *1 | Brace events *2 | Brace Change | Exercise *3 |
|---|---|---|---|
| 1 | - | - | schroth |
| 2 | Sum *4 & Irr *5 & BP *6 | - | schroth |
| 3 | Sum *4 & Irr *5 | - | schroth |
| 4 | - | - | - |
| 5 | - | - | - |
| 6 | E *10 | - | - |
| 7 | - | - | - |
| 8 | BP *7 & E *10 | chea *8 | schroth |
| 9 | Irr *5 &E *10 | prov/chea *9 | schroth |
| 10 | - | - | schroth |
| 11 | OM *11 | - | - |
| 12 | - | - | - |
| 13 | - | - | - |
| 14 | E *10 & OM *11 | - | Roolfing |
| 15 | E *10 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, C.; Andersen, T.B. Evaluation of Brace Treatment Using the Soft Brace Spinaposture: A Four-Years Follow-Up. J. Clin. Med. 2022, 11, 264. https://doi.org/10.3390/jcm11010264
Wong C, Andersen TB. Evaluation of Brace Treatment Using the Soft Brace Spinaposture: A Four-Years Follow-Up. Journal of Clinical Medicine. 2022; 11(1):264. https://doi.org/10.3390/jcm11010264
Chicago/Turabian StyleWong, Christian, and Thomas B. Andersen. 2022. "Evaluation of Brace Treatment Using the Soft Brace Spinaposture: A Four-Years Follow-Up" Journal of Clinical Medicine 11, no. 1: 264. https://doi.org/10.3390/jcm11010264
APA StyleWong, C., & Andersen, T. B. (2022). Evaluation of Brace Treatment Using the Soft Brace Spinaposture: A Four-Years Follow-Up. Journal of Clinical Medicine, 11(1), 264. https://doi.org/10.3390/jcm11010264





