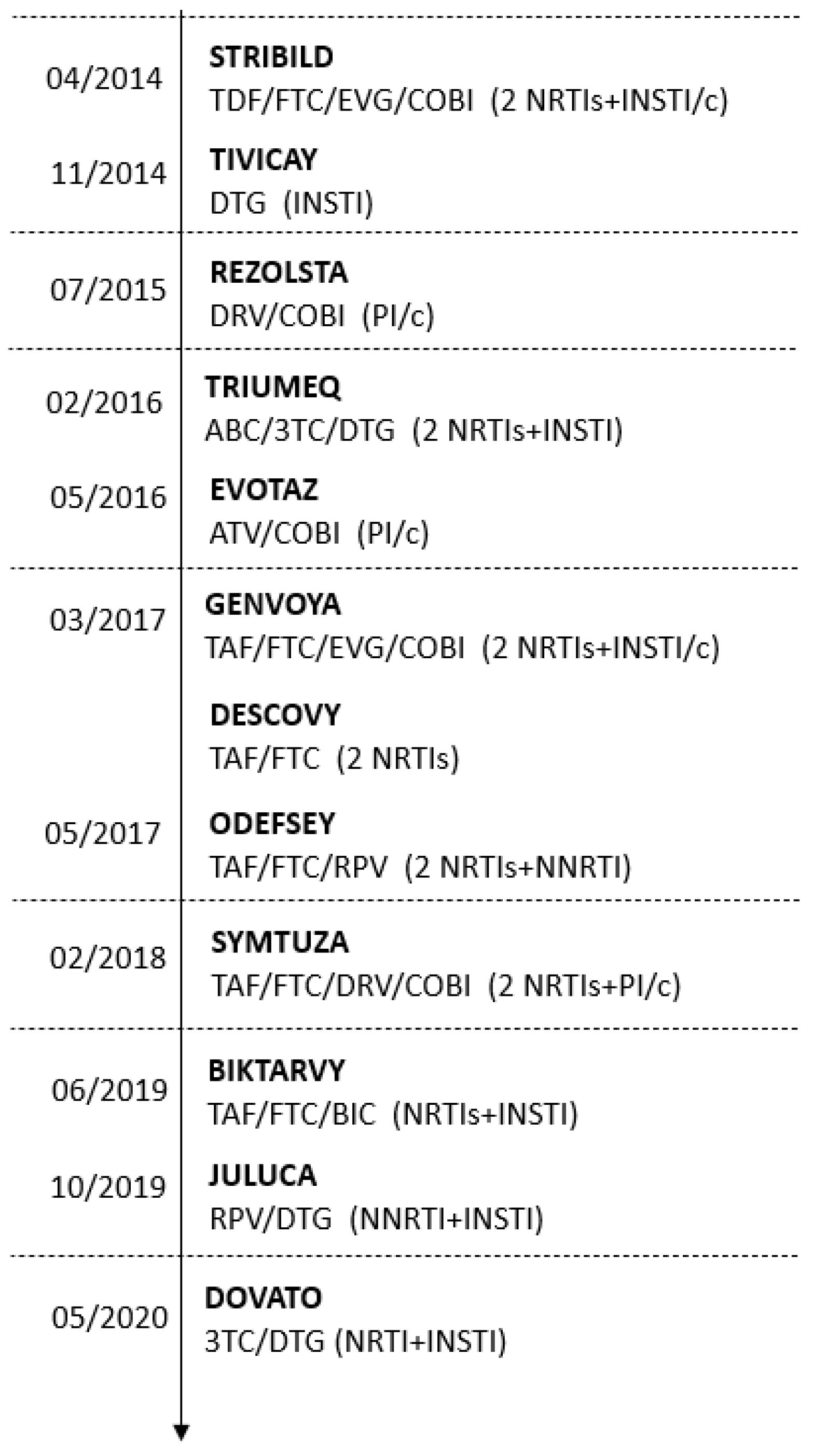
Evolution in Real-World Therapeutic Strategies for HIV Treatment: A Retrospective Study in Southern Italy, 2014–2020
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Distributions of Patient Characteristics and ART Regimens during 2014–2020
3.2. Switching Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global AIDS Update. 2016. Available online: https://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf (accessed on 16 November 2021).
- HIV-Causal Collaboration; Ray, M.; Logan, R.; Sterne, J.A.; Hernandez-Diaz, S.; Robins, J.M.; Sabin, C.; Bansi, L.; van Sighem, A.; de Wolf, F.; et al. The effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS 2010, 24, 123–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. August 2021. Available online: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf (accessed on 16 November 2021).
- European AIDS Clinical Society (EACS). EACS Guidelines, Version n.11.0. EACS. 2021. Available online: https://www.eacsociety.org/media/final2021eacsguidelinesv11.0_oct2021.pdf (accessed on 16 November 2021).
- Società Italiana Malattie Infettive e Tropicali (SIMIT). Linee Guida Italiane Sull’utilizzo della Terapia Antiretrovirale e la Gestione Diagnostico-Clinica delle Persone con Infezione da HIV-1; 8 Edizione, 2017 [Use of Antiretroviral Drugs and Diagnostic-Clinical Management of People with HIV-1 Infection; 8 Edition, 2017]. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_2696_allegato.pdf (accessed on 16 November 2021).
- Tseng, A.; Seet, J.; Phillips, E.J. The evolution of three decades of antiretroviral therapy: Challenges, triumphs and the promise of the future. Br. J. Clin. Pharmacol. 2015, 79, 182–194. [Google Scholar] [CrossRef] [Green Version]
- Ryom, L.; Cotter, A.; De Miguel, R.; Beguelin, C.; Podlekareva, D.; Arribas, J.R.; Marzolini, C.; Mallon, P.; Rauch, A.; Kirk, O.; et al. 2019 update of the European AIDS Clinical Society Guidelines for treatment of people living with HIV version 10.0. HIV Med. 2020, 21, 617–624. [Google Scholar] [CrossRef] [PubMed]
- European AIDS Clinical Society (EACS). EACS Guidelines, Version n.10.0. EACS. 2019. Available online: https://www.eacsociety.org/media/2019_guidelines-10.0_final.pdf (accessed on 16 November 2021).
- Clay, P.G.; Nag, S.; Graham, C.M.; Narayanan, S. Meta-Analysis of Studies Comparing Single and Multi-Tablet Fixed Dose Combination HIV Treatment Regimens. Medicine 2015, 94, e1677. [Google Scholar] [CrossRef]
- Comelli, A.; Izzo, I.; Donato, F.; Celotti, A.; Foca, E.; Pezzoli, C.; Castelli, F.; Quiros-Roldan, E. Disengagement and reengagement of HIV continuum of care in a single center cohort in northern Italy. HIV Res. Clin. Pract. 2019, 20, 1–11. [Google Scholar] [CrossRef]
- Lagi, F.; Kiros, S.T.; Campolmi, I.; Giache, S.; Rogasi, P.G.; Mazzetti, M.; Bartalesi, F.; Trotta, M.; Nizzoli, P.; Bartoloni, A.; et al. Continuum of care among HIV-1 positive patients in a single center in Italy (2007–2017). Patient Prefer. Adher. 2018, 12, 2545–2551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galli, M.; Borderi, M.; Viale, P. HIV policy in Italy and recommendations across the HIV care continuum. Infez. Med. 2020, 28, 17–28. [Google Scholar] [PubMed]
- Quiros-Roldan, E.; Magro, P.; Carriero, C.; Chiesa, A.; El Hamad, I.; Tratta, E.; Fazio, R.; Formenti, B.; Castelli, F. Consequences of the COVID-19 pandemic on the continuum of care in a cohort of people living with HIV followed in a single center of Northern Italy. AIDS Res. Ther. 2020, 17, 59. [Google Scholar] [CrossRef] [PubMed]
- Nappi, A.; Perrella, A.; Bellopede, P.; Lanza, A.; Izzi, A.; Spatarella, M.; Sbreglia, C. Safety of new DAAs for chronic HCV infection in a real life experience: Role of a surveillance network based on clinician and hospital pharmacist. Infect. Agent Cancer 2017, 12, 12. [Google Scholar] [CrossRef] [Green Version]
- Antinori, A.; Marcotullio, S.; Andreoni, M.; Ammassari, A.; d’Arminio Monforte, A.; Galli, M.; Girardi, E.; Mazzotta, F.; Mussini, C.; Puoti, M.; et al. Italian guidelines for the use of antiretroviral agents and the diagnostic-clinical management of HIV-1 infected persons. New Microbiol. 2015, 38, 299–328. [Google Scholar]
- Astuti, N.; Maggiolo, F. Single-Tablet Regimens in HIV Therapy. Infect. Dis. Ther. 2014, 3, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eaton, E.F.; Tamhane, A.; Davy-Mendez, T.; Mathews, W.C.; Moore, R.D.; Saag, M.S.; Mugavero, M.J. Trends in antiretroviral therapy prescription, durability and modification: New drugs, more changes, but less failure. AIDS 2018, 32, 347–355. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Updated Recommendations on Service Delivery for the Treatment and Care of People Living with HIV; World Health Organization: Geneva, Switzerland, 2021. Available online: https://www.who.int/publications/i/item/9789240023581 (accessed on 16 November 2021).
- World Health Organization. Guidelines on the Public Health Response to Pretreatment HIV Drug Resistance: July 2017; World Health Organization: Geneva, Switzerland, 2017. Available online: https://apps.who.int/iris/handle/10665/255880 (accessed on 16 November 2021).
- Tao, X.; Lu, Y.; Zhou, Y.; Zhang, L.; Chen, Y. Efficacy and safety of the regimens containing tenofovir alafenamide versus tenofovir disoproxil fumarate in fixed-dose single-tablet regimens for initial treatment of HIV-1 infection: A meta-analysis of randomized controlled trials. Int. J. Infect. Dis. 2020, 93, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Winston, A.; Post, F.A.; DeJesus, E.; Podzamczer, D.; Di Perri, G.; Estrada, V.; Raffi, F.; Ruane, P.; Peyrani, P.; Crofoot, G.; et al. Tenofovir alafenamide plus emtricitabine versus abacavir plus lamivudine for treatment of virologically suppressed HIV-1-infected adults: A randomised, double-blind, active-controlled, non-inferiority phase 3 trial. Lancet HIV 2018, 5, e162–e171. [Google Scholar] [CrossRef]
- Dorjee, K.; Choden, T.; Baxi, S.M.; Steinmaus, C.; Reingold, A.L. Risk of cardiovascular disease associated with exposure to abacavir among individuals with HIV: A systematic review and meta-analyses of results from 17 epidemiologic studies. Int. J. Antimicrob. Agents 2018, 52, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Antinori, A.; Di Biagio, A.; Marcotullio, S.; Sarmati, L.; Andreoni, M.; Angarano, G.; Chirianni, A.; d’Arminio Monforte, A.; Di Perri, G.; Galli, M.; et al. Evidence-based renewal of the Italian guidelines for the use of antiretroviral agents and the diagnostic-clinical management of HIV-1 infected persons. New Microbiol. 2018, 41, 247–255. [Google Scholar]

| 2014 N = 349 | 2015 N = 375 | 2016 N = 319 | 2017 N = 293 | 2018 N = 292 | 2019 N = 393 | 2020 N = 234 | F Value 1/ χ2 Value (df) 1 | p Value | |
|---|---|---|---|---|---|---|---|---|---|
| Male (%) | 74.8 | 69.3 | 75.9 | 80.9 | 78.4 | 71.0 | 75.6 | 17.0 (6) | 0.009 |
| Age | |||||||||
| Mean (years) | 42.7 | 43.6 | 42.3 | 41.8 | 41.2 | 41.4 | 42.4 | 2.1 (6; 2248) | 0.055 |
| ≥50 years | 26.1 | 24.0 | 28.2 | 25.3 | 20.2 | 22.1 | 24.4 | 7.1 (6) | 0.314 |
| Non-Italian origin (%) | 16.3 | 28.3 | 21.6 | 20.8 | 22.9 | 17.6 | 18.8 | 20.8 (6) | 0.002 |
| STR (%) | 48.4 | 44.5 | 58.6 | 54.6 | 58.6 | 64.1 | 81.2 | 99.7 (6) | <0.0001 |
| MTR (%) | 51.6 | 55.5 | 41.4 | 45.4 | 41.4 | 35.9 | 18.8 | ||
| NRTI backbones (%) | |||||||||
| ABC/3TC | 10.3 | 15.7 | 22.6 | 23.5 | 27.1 | 18.6 | 17.1 | 1361.9 (36) | <0.0001 |
| TDF/FTC | 65.0 | 62.1 | 61.8 | 58.0 | 7.5 | 3.8 | 6.0 | ||
| TAF/FTC | 10.9 | 57.2 | 69.0 | 68.4 | |||||
| ART regimen (%) | |||||||||
| 2 NRTIs + PI | 39.5 | 30.4 | 19.4 | 21.8 | 22.9 | 20.9 | 8.5 | 387.9 (30) | <0.0001 |
| 2 NRTIs + NNRTI | 27.2 | 23.2 | 19.7 | 18.1 | 12.3 | 12.7 | 15.0 | ||
| 2 NRTIs + INSTI | 10.0 | 24.8 | 44.5 | 49.1 | 54.5 | 55.7 | 67.9 | ||
| Others | 23.2 | 21.6 | 16.3 | 10.9 | 9.9 | 9.2 | 6.0 | ||
| DTG + 3TC 2 | 0.3 | 1.5 | 1.3 | ||||||
| DTG/3TC 2 | 1.3 |
| 2014 N = 1779 | 2015 N = 1935 | 2016 N = 2066 | 2017 N = 2055 | 2018 N = 2093 | 2019 N = 2191 | 2020 N = 2137 | F Value/ χ2 Value (df) 1 | p Value | |
|---|---|---|---|---|---|---|---|---|---|
| Male (%) | 73.0 | 73.7 | 73.9 | 74.2 | 75.0 | 75.0 | 75.0 | 3.7 (6) | 0.716 |
| Age | |||||||||
| Mean (years) | 46.2 | 46.8 | 47.2 | 47.4 | 47.6 | 47.8 | 48.1 | 7.6 (6; 14249) | <0.0001 |
| ≥50 years | 35.2 | 38.5 | 40.2 | 42.8 | 44.7 | 45.6 | 47.2 | 87.6 (6) | <0.0001 |
| Non-Italian origin (%) | 16.0 | 14.6 | 15.3 | 15.6 | 16.2 | 15.9 | 14.8 | 3.5 (6) | 0.743 |
| STR (%) | 31.5 | 39.1 | 43.0 | 51.5 | 56.0 | 60.6 | 77.3 | 1123.0 (6) | <0.0001 |
| MTR (%) | 68.5 | 60.9 | 57.0 | 48.5 | 44.0 | 39.4 | 22.7 | ||
| NRTI backbones (%) | |||||||||
| ABC/3TC | 16.5 | 16.1 | 17.1 | 21.4 | 23.8 | 24.4 | 22.7 | 6868.8 (54) | <0.0001 |
| TDF/FTC | 58.5 | 57.7 | 58.0 | 56.6 | 29.0 | 4.5 | 2.1 | ||
| TAF/FTC | 0.8 | 30.1 | 56.3 | 60.1 | |||||
| ART regimen (%) | |||||||||
| 2 NRTIs + PI | 43.7 | 37.0 | 29.3 | 23.8 | 19.7 | 17.3 | 16.5 | 3100.1 (30) | <0.0001 |
| 2 NRTIs + NNRTI | 30.6 | 32.7 | 31.9 | 28.1 | 23.4 | 20.8 | 17.1 | ||
| 2 NRTIs + INSTI | 1.5 | 5.0 | 13.0 | 27.6 | 39.6 | 46.6 | 50.8 | ||
| Others | 24.2 | 25.2 | 25.5 | 19.8 | 15.7 | 13.3 | 10.7 | ||
| DTG + RPV or DTG + 3TC | 0.1 | 0.3 | 0.7 | 1.6 | 2.0 | 2.3 | |||
| DTG/RPV or DTG/3TC | 2.6 |
| To | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total | 2 NRTIs + PI | 2 NRTIs + INSTI | 2 NRTIs + NNRTI | DTG/RPV or DTG/3TC | DTG + RPV or DTG + 3TC | Others | ||
| N | % | % | % | % | % | % | ||
| From | 2 NRTIs + PI | 161 | - | 80.1 | 5.6 | 1.9 | 3.7 | 8.7 |
| 2 NRTI + INSTI | 102 | 18.6 | - | 19.6 | 13.7 | 30.4 | 17.6 | |
| 2 NRTIs + NNRTI | 145 | 4.1 | 55.2 | - | 4.1 | 33.8 | 2.8 | |
| DTG + RPV or DTG + 3TC | 8 | - | 25.0 | - | 12.5 | 50.0 | 12.5 | |
| DTG/RPV or DTG/3TC | 4 | - | - | 50.0 | 25.0 | - | 25.0 | |
| Others | 134 | 12.7 | 43.3 | 2.2 | 6.7 | 6.7 | 28.4 | |
| Total | 554 | 7.6 | 48.6 | 6.1 | 6.1 | 17.9 | 13.7 | |
| To | ||||||
|---|---|---|---|---|---|---|
| Total | TDF/FTC | ABC/3TC | TAF/FTC | TDF/3TC | ||
| N | % | % | % | % | ||
| From | TDF/FTC | 648 | - | 4.2 | 95.8 | - |
| ABC/3TC | 72 | - | - | 100.0 | - | |
| TAF/FTC | 33 | 30.3 | 66.7 | - | 3.0 | |
| TDF + 3TC | 3 | - | - | 100.0 | - | |
| ZDV/3TC | 2 | - | 100.0 | - | - | |
| Total | 758 | 1.3 | 6.7 | 91.8 | 0.1 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papa, N.; Cammarota, S.; Citarella, A.; Atripaldi, L.; Bernardi, F.F.; Fogliasecca, M.; Giugliano, N.; Trama, U.; Spatarella, M. Evolution in Real-World Therapeutic Strategies for HIV Treatment: A Retrospective Study in Southern Italy, 2014–2020. J. Clin. Med. 2022, 11, 161. https://doi.org/10.3390/jcm11010161
Papa N, Cammarota S, Citarella A, Atripaldi L, Bernardi FF, Fogliasecca M, Giugliano N, Trama U, Spatarella M. Evolution in Real-World Therapeutic Strategies for HIV Treatment: A Retrospective Study in Southern Italy, 2014–2020. Journal of Clinical Medicine. 2022; 11(1):161. https://doi.org/10.3390/jcm11010161
Chicago/Turabian StylePapa, Nunzia, Simona Cammarota, Anna Citarella, Luigi Atripaldi, Francesca F. Bernardi, Marianna Fogliasecca, Nello Giugliano, Ugo Trama, and Micaela Spatarella. 2022. "Evolution in Real-World Therapeutic Strategies for HIV Treatment: A Retrospective Study in Southern Italy, 2014–2020" Journal of Clinical Medicine 11, no. 1: 161. https://doi.org/10.3390/jcm11010161
APA StylePapa, N., Cammarota, S., Citarella, A., Atripaldi, L., Bernardi, F. F., Fogliasecca, M., Giugliano, N., Trama, U., & Spatarella, M. (2022). Evolution in Real-World Therapeutic Strategies for HIV Treatment: A Retrospective Study in Southern Italy, 2014–2020. Journal of Clinical Medicine, 11(1), 161. https://doi.org/10.3390/jcm11010161





