Wide Variation in Post-Void Residual Management after Urogynecologic Surgery: A Survey of Urogynecologists’ Practices
Abstract
1. Introduction
2. Materials and Methods
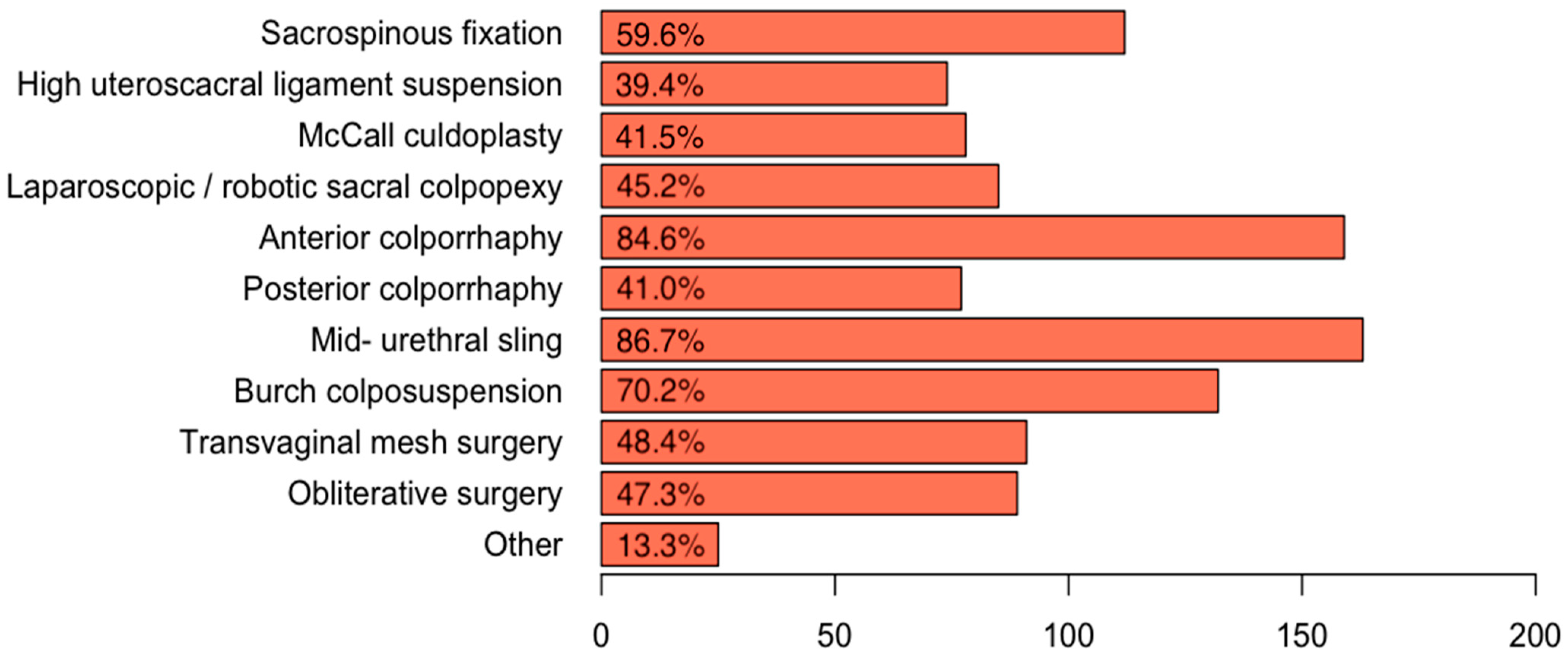
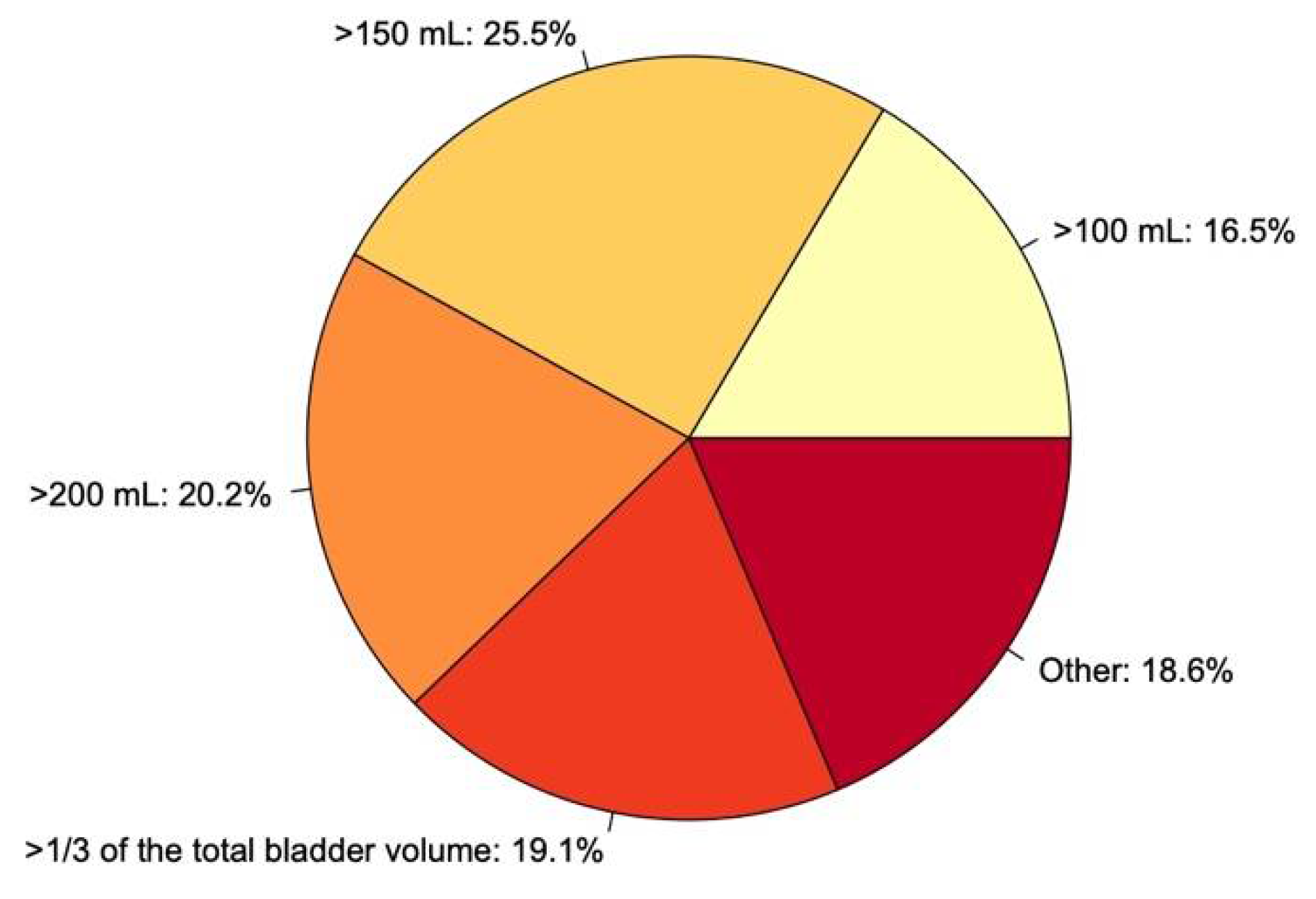
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, F.J.; Holman, C.D.J.; Moorin, R.E.; Tsokos, N. Lifetime Risk of Undergoing Surgery for Pelvic Organ Prolapse. Obstet. Gynecol. 2010, 116, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Matthews, C.A.; Conover, M.M.; Pate, V.; Funk, M.J. Lifetime Risk of Stress Urinary Incontinence or Pelvic Organ Prolapse Surgery. Obstet. Gynecol. 2014, 123, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Partoll, L.M. Efficacy of tension-free vaginal tape with other pelvic reconstructive surgery. Am. J. Obstet. Gynecol. 2002, 186, 1292–1298. [Google Scholar] [CrossRef]
- Geller, E.J. Prevention and management of postoperative urinary retention after urogynecologic surgery. Int. J. Women‘s Health 2014, 6, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Hakvoort, R.; Elberink, R.; Vollebregt, A.; Ploeg, T.; Emanuel, M. How long should urinary bladder catheterisation be continued after vaginal prolapse surgery? A randomised controlled trial comparing short term versus long term catheterisation after vaginal prolapse surgery. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 828–830. [Google Scholar] [CrossRef]
- Shatkin-Margolis, A.; Yook, E.; Hill, A.M.; Crisp, C.C.; Yeung, J.; Kleeman, S.; Pauls, R.N. Self-Removal of a Urinary Catheter After Urogynecologic Surgery. Obstet. Gynecol. 2019, 134, 1027–1036. [Google Scholar] [CrossRef]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int. Urogynecology J. 2010, 21, 5–26. [Google Scholar] [CrossRef] [PubMed]
- Natale, F.; La Penna, C.; Saltari, M.; Piccione, E.; Cervigni, M. Voiding dysfunction after anti-incontinence surgery. Minerva Ginecol. 2009, 61, 167–172. [Google Scholar]
- Madersbacher, H.; Cardozo, L.; Chapple, C.; Abrams, P.; Toozs-Hobson, P.; Young, J.S.; Wyndaele, J.-J.; de Wachter, S.; Campeau, L.; Gajewski, J.B. What are the causes and consequences of bladder overdistension?: ICI-RS 2011. Neurourol. Urodyn. 2012, 31, 317–321. [Google Scholar] [CrossRef]
- Carter-Brooks, C.M.; Zyczynski, H.M.; Moalli, P.A.; Brodeur, P.G.; Shepherd, J.P. Early catheter removal after pelvic floor reconstructive surgery: A randomized trial. Int. Urogynecology J. 2018, 29, 1203–1212. [Google Scholar] [CrossRef]
- Kleeman, S.; Goldwasser, S.; Vassallo, B.; Karram, M. Predicting postoperative voiding efficiency after operation for incontinence and prolapse. Am. J. Obstet. Gynecol. 2002, 187, 49–52. [Google Scholar] [CrossRef]
- Foster, R.T.; Borawski, K.M.; South, M.M.; Weidner, A.C.; Webster, G.D.; Amundsen, C.L. A randomized, controlled trial evaluating 2 techniques of postoperative bladder testing after transvaginal surgery. Am. J. Obstet. Gynecol. 2007, 197, 627.e1–627.e4. [Google Scholar] [CrossRef]
- Pulvino, J.Q.; Duecy, E.E.; Buchsbaum, G.M.; Flynn, M.K. Comparison of 2 Techniques to Predict Voiding Efficiency After Inpatient Urogynecologic Surgery. J. Urol. 2010, 184, 1408–1412. [Google Scholar] [CrossRef] [PubMed]
- Tunitsky-Bitton, E.; Murphy, A.M.; Barber, M.D.; Goldman, H.B.; Vasavada, S.P.; Jelovsek, J.E. Assessment of voiding after sling: A randomized trial of 2 methods of postoperative catheter management after midurethral sling surgery for stress urinary incontinence in women. Am. J. Obstet. Gynecol. 2015, 212, 597.e1–597.e9. [Google Scholar] [CrossRef]
- Boyd, S.S.; Tunitsky-Bitton, E.; O’Sullivan, D.M.; Steinberg, A.C. Postoperative Catheter Management after Pelvic Reconstructive Surgery. Female Pelvic Med. Reconstr. Surg. 2018, 24, 188–192. [Google Scholar] [CrossRef]
- Hooton, T.M.; Bradley, S.F.; Cardenas, D.D.; Colgan, R.; Geerlings, S.E.; Rice, J.C.; Saint, S.; Schaeffer, A.J.; Tambayh, P.A.; Tenke, P.; et al. Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin. Infect. Dis. 2010, 50, 625–663. [Google Scholar] [CrossRef] [PubMed]
- Alexandrou, E.; Ray-Barruel, G.; Carr, P.J.; Frost, S.A.; Inwood, S.; Higgins, N.; Lin, F.; Alberto, L.; Mermel, L.; Rickard, C.M.; et al. Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes Worldwide. J. Hosp. Med. 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Stallard, S.; Prescott, S. Postoperative urinary retention in general surgical patients. Br. J. Surg. 1988, 75, 1141–1143. [Google Scholar] [CrossRef]
- Huang, H.; Dong, L.; Gu, L. The timing of urinary catheter removal after gynecologic surgery. Medicine 2020, 99, e18710. [Google Scholar] [CrossRef]
- Geller, E.J.; Hankins, K.J.; Parnell, B.A.; Robinson, B.L.; Dunivan, G.C. Diagnostic Accuracy of Retrograde and Spontaneous Voiding Trials for Postoperative Voiding Dysfunction. Obstet. Gynecol. 2011, 118, 637–642. [Google Scholar] [CrossRef]
- Dieter, A.A.; Conklin, J.L.; Willis-Gray, M.G.; Desai, S.; Grant, M.; Bradley, M.S. A Systematic Review of Randomized Trials Investigating Methods of Postoperative Void Trials Following Benign Gynecologic and Urogynecologic Surgeries. J. Minim. Invasive Gynecol. 2021. [Google Scholar] [CrossRef] [PubMed]
- International Continence Society. Urinary Retention. Available online: https://www.ics.org/committees/standardisation/terminologydiscussions/urinaryretention (accessed on 29 April 2021).
- Steinberg, B.J.; Finamore, P.S.; Sastry, D.N.; Holzberg, A.S.; Caraballo, R.; Echols, K.T. Postoperative urinary retention following vaginal mesh procedures for the treatment of pelvic organ prolapse. Int. Urogynecology J. 2010, 21, 1491–1498. [Google Scholar] [CrossRef]
- Boyd, S.S.; O’Sullivan, D.M.; Tunitsky-Bitton, E. A Comparison of Two Methods of Catheter Management After Pelvic Reconstructive Surgery. Obstet. Gynecol. 2019, 134, 1037–1045. [Google Scholar] [CrossRef]
- Choong, S.; Emberton, M. Acute urinary retention. BJU Int. 2000, 85, 186–201. [Google Scholar] [CrossRef] [PubMed]
- De Souza, G.M.; Costa, W.S.; Bruschini, H.; Sampaio, F.J. Morphological analysis of the acute effects of overdistension on the extracellular matrix of the rat urinary bladder wall. Ann. Anat. Anat. Anz. 2004, 186, 55–59. [Google Scholar] [CrossRef]
- Kesty, K.; Edenfield, A.; Castro, D.; Medina, L.; Naser, M.; Manríquez, V.; Swift, S. Subjective versus objective determination of bladder emptying following urogynecological surgery: “do you feel that you completely emptied your bladder?”. Int. Urogynecology J. 2020, 31, 1899–1905. [Google Scholar] [CrossRef]
- Willis-Gray, M.G.; Wu, J.M.; Field, C.; Pulliam, S.; Husk, K.E.; Brueseke, T.J.; Geller, E.J.; Connolly, A.; Dieter, A.A. Is a Postvoid Residual Necessary? A Randomized Trial of Two Postoperative Voiding Protocols. Female Pelvic Med. Reconstr. Surg. 2021, 27, e256–e260. [Google Scholar] [CrossRef]
- Siedhoff, M.T.; Wright, K.N.; Misal, M.A.; Molina, A.L.; Greene, N.H. Postoperative Urinary Retention after Benign Gynecologic Surgery with a Liberal versus Strict Voiding Protocol. J. Minim. Invasive Gynecol. 2021, 28, 351–357. [Google Scholar] [CrossRef] [PubMed]
| Variable n = 204 | N (%) |
|---|---|
| Present position | |
| Consultant | 173 (85.2%) |
| Fellow | 12 (5.9%) |
| Resident | 18 (8.9%) |
| Age | |
| 25–30 years | 3 (1.5%) |
| 31–40 years | 35 (17.2%) |
| 41–50 years | 71 (34.8%) |
| >50 years | 95 (46.6%) |
| Country | |
| United Kingdom | 69 (33.8%) |
| Austria | 33 (16.2%) |
| Canada | 24 (11.8%) |
| Switzerland | 22 (10.8%) |
| Germany | 19 (9.3%) |
| France | 9 (4.4%) |
| United States | 6 (2.9%) |
| Italy | 3 (1.5%) |
| Czech Republic | 2 (1%) |
| Israel | 2 (1%) |
| Serbia | 2 (1%) |
| Slovenia | 2 (1%) |
| Australia | 1 (0.5%) |
| China | 1 (0.5%) |
| Columbia | 1 (0.5%) |
| Egypt | 1 (0.5%) |
| Finland | 1 (0.5%) |
| New Zealand | 1 (0.5%) |
| Poland | 1 (0.5%) |
| Sweden | 1 (0.5%) |
| The Netherlands | 1 (0.5%) |
| Hospital | |
| Public hospital | 98 (48%) |
| University hospital | 94 (46%) |
| Private practice | 42 (21%) |
| Other | 5 (2.5%) |
| Years of clinical experience | |
| 0–5 | 10 (4.9%) |
| 5–10 | 24 (11.8%) |
| 10–15 | 32 (15.7%) |
| >15 | 138 (67.7%) |
| Pelvic organ prolapse surgeries per year | |
| 0–5 | 12 (5.9%) |
| 5–15 | 17 (8.3%) |
| 16–30 | 36 (17.6%) |
| 31–50 | 33 (16.2%) |
| 50–100 | 59 (28.9%) |
| >100 | 47 (23%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marschalek, M.-L.; Umek, W.; Koelbl, H.; Veit-Rubin, N.; Bodner-Adler, B.; Husslein, H. Wide Variation in Post-Void Residual Management after Urogynecologic Surgery: A Survey of Urogynecologists’ Practices. J. Clin. Med. 2021, 10, 1946. https://doi.org/10.3390/jcm10091946
Marschalek M-L, Umek W, Koelbl H, Veit-Rubin N, Bodner-Adler B, Husslein H. Wide Variation in Post-Void Residual Management after Urogynecologic Surgery: A Survey of Urogynecologists’ Practices. Journal of Clinical Medicine. 2021; 10(9):1946. https://doi.org/10.3390/jcm10091946
Chicago/Turabian StyleMarschalek, Marie-Louise, Wolfgang Umek, Heinz Koelbl, Nikolaus Veit-Rubin, Barbara Bodner-Adler, and Heinrich Husslein. 2021. "Wide Variation in Post-Void Residual Management after Urogynecologic Surgery: A Survey of Urogynecologists’ Practices" Journal of Clinical Medicine 10, no. 9: 1946. https://doi.org/10.3390/jcm10091946
APA StyleMarschalek, M.-L., Umek, W., Koelbl, H., Veit-Rubin, N., Bodner-Adler, B., & Husslein, H. (2021). Wide Variation in Post-Void Residual Management after Urogynecologic Surgery: A Survey of Urogynecologists’ Practices. Journal of Clinical Medicine, 10(9), 1946. https://doi.org/10.3390/jcm10091946







