Mechanical Thrombectomy in Stroke. Experience from Switching from Stent Retriever Only to Stent Retriever Combined with Aspiration Catheter
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Image Analysis
2.3. Thrombectomy Technique
2.4. Statistical Analysis
3. Results
Study Population
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jovin, T.G.; Chamorro, A.; Cobo, E.; De Miquel, M.A.; Molina, C.A.; Rovira, A.; Román, L.S.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thr ombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Berkhemer, O.A.; Fransen, P.S.S.; Beumer, D.; Berg, L.A.V.D.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.H.; et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef]
- Lapergue, B.; Blanc, R.; Gory, B.; Labreuche, J.; Duhamel, A.; Marnat, G.; Saleme, S.; Costalat, V.; Bracard, S.; Desal, H.; et al. Effect of Endovascular Contact Aspiration vs Stent Retriever on Revascularization in Patients With Acute Ischemic Stroke and Large Vessel Occlusion. JAMA 2017, 318, 443–452. [Google Scholar] [CrossRef]
- Maus, V.; Henkel, S.; Riabikin, A.; Riedel, C.; Behme, D.; Tsogkas, I.; Hesse, A.C.; Abdullayev, N.; Jansen, O.; Wiesmann, M.; et al. The SAVE Technique: Large-Scale Experience for Treatment of Intracranial Large Vessel Occlusions. Clin. Neuroradiol. 2018, 29, 669–676. [Google Scholar] [CrossRef]
- Maus, V.; Behme, D.; Kabbasch, C.; Borggrefe, J.; Tsogkas, I.; Nikoubashman, O.; Wiesmann, M.; Knauth, M.; Mpotsaris, A.; Psychogios, M.N. Maximizing First-Pass Complete Reperfusion with SAVE. Clin. Neuroradiol. 2018, 28, 327–338. [Google Scholar] [CrossRef]
- Zaidat, O.O.; Yoo, A.J.; Khatri, P.; Tomsick, T.A.; Von Kummer, R.; Saver, J.L.; Marks, M.P.; Prabhakaran, S.; Kallmes, D.F.; Fitzsimmons, B.-F.M.; et al. Recommendations on Angiographic Revascularization Grading Standards for Acute Ischemic Stroke. Stroke 2013, 44, 2650–2663. [Google Scholar] [CrossRef]
- Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Dávalos, A.; Guidetti, D.; Larrue, V.; Lees, K.R.; Medeghri, Z.; Machnig, T.; et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Volny, O.; Krajina, A.; Belaskova, S.; Bar, M.; Cimflova, P.; Herzig, R.; Sanak, D.; Tomek, A.; Köcher, M.; Rocek, M.; et al. Mechanical thrombectomy performs similarly in real world practice: A 2016 nationwide study from the Czech Republic. J. Neurointerv. Surg. 2017, 10, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke|Enhanced Reader. Available online: Moz-extension://ce03b620-5a16-6f4b-9f06-5ef87b4b00a9/enhanced-reader.html?openApp&pdf=https%3A%2F%2Fwww.nejm.org%2Fdoi%2Fpdf%2F10.1056%2FNEJMoa1415061%3FarticleTools%3Dtrue (accessed on 8 November 2020).
- Nikoubashman, O.; Büsen, M.; Wiesmann, M. Necessary Catheter Diameters for Mechanical Thrombectomy with ADAPT. Am. J. Neuroradiol. 2017, 38, 2277–2281. [Google Scholar] [CrossRef]
- Machi, P.; Jourdan, F.; Ambard, D.; Reynaud, C.; Lobotesis, K.; Sanchez, M.; Bonafé, A.; Costalat, V. Experimental evaluation of stent retrievers’ mechanical properties and effectiveness. J. NeuroInterv. Surg. 2017, 9, 257–263. [Google Scholar] [CrossRef]
- Massari, F.; Henninger, N.; Lozano, J.D.; Patel, A.; Kuhn, A.L.; Howk, M.; Perras, M.; Brooks, C.; Gounis, M.J.; Kan, P.; et al. ARTS (Aspiration–Retriever Technique for Stroke): Initial clinical experience. Interv. Neuroradiol. 2016, 22, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Humphries, W.; Hoit, D.; Doss, V.T.; Elijovich, L.; Frei, D.; Loy, D.; Dooley, G.; Turk, A.S.; Chaudry, I.; Turner, R.; et al. Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J. NeuroInterv. Surg. 2015, 7, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Hong, J.M.; Lee, S.-J.; Joo, I.S.; Lim, Y.C.; Kim, S.Y. The combined use of mechanical thrombectomy devices is feasible for treating acute carotid terminus occlusion. Acta Neurochir. 2013, 155, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.-H.; Kim, Y.-W.; Hwang, Y.-H.; Park, J.; Hwang, J.-H. Switching Strategy for Mechanical Thrombectomy of Acute Large Vessel Occlusion in the Anterior Circulation. Stroke 2013, 44, 3577–3579. [Google Scholar] [CrossRef]
- Munich, S.A.; Vakharia, K.; Levy, E.I. Overview of Mechanical Thrombectomy Techniques. Clin. Neurosurg. 2019, 85 (Suppl. 1), S60–S67. [Google Scholar] [CrossRef]
- Brehm, A.; Maus, V.; Tsogkas, I.; Colla, R.; Hesse, A.C.; Gera, R.G.; Psychogios, M.-N. Stent-retriever assisted vacuum-locked extraction (SAVE) versus a direct aspiration first pass technique (ADAPT) for acute stroke: Data from the real-world. BMC Neurol. 2019, 19, 65. [Google Scholar] [CrossRef]
- Khatri, P.; Abruzzo, T.; Yeatts, S.D.; Nichols, C.; Broderick, J.P.; Tomsick, T.A. For the IMS I and II Investigators Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology 2009, 73, 1066–1072. [Google Scholar] [CrossRef]
- Goyal, M.; Jadhav, A.P.; Bonafe, A.; Diener, H.; Pereira, V.M.; Levy, E.; Baxter, B.; Jovin, T.; Jahan, R.; Menon, B.K.; et al. Analysis of Workflow and Time to Treatment and the Effects on Outcome in Endovascular Treatment of Acute Ischemic Stroke: Results from the SWIFT PRIME Randomized Controlled Trial. Radiology 2016, 279, 888–897. [Google Scholar] [CrossRef]
- Shi, Z.-S.; Liebeskind, D.S.; Xiang, B.; Ge, S.G.; Feng, L.; Albers, G.W.; Budzik, R.; Devlin, T.; Gupta, R.; Jansen, O.; et al. Predictors of Functional Dependence Despite Successful Revascularization in Large-Vessel Occlusion Strokes. Stroke 2014, 45, 1977–1984. [Google Scholar] [CrossRef]
- Nikoubashman, O.; Dekeyzer, S.; Riabikin, A.; Keulers, A.; Reich, A.; Mpotsaris, A.; Wiesmann, M. True First-Pass Effect: First-Pass Complete Reperfusion Improves Clinical Outcome in Thrombectomy Stroke Patients. Stroke 2019, 50, 2140–2146. [Google Scholar] [CrossRef] [PubMed]
- Zaidat, O.O.; Castonguay, A.C.; Linfante, I.; Gupta, R.; Martin, C.O.; Holloway, W.E.; Mueller-Kronast, N.; English, J.D.; Dabus, G.; Malisch, T.W.; et al. First pass effect: A new measure for stroke thrombectomy devices. Stroke 2018, 49, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Velasco, A.; Buerke, B.; Stracke, C.P.; Berkemeyer, S.; Mosimann, P.J.; Schwindt, W.; Alcázar, P.; Cnyrim, C.; Niederstadt, T.; Chapot, R.; et al. Comparison of a Balloon Guide Catheter and a Non–Balloon Guide Catheter for Mechanical Thrombectomy. Radiology 2016, 280, 169–176. [Google Scholar] [CrossRef]
- Brinjikji, W.; Starke, R.M.; Murad, M.H.; Fiorella, D.; Pereira, V.M.; Goyal, M.; Kallmes, D.F. Impact of balloon guide catheter on technical and clinical outcomes: A systematic review and meta-analysis. J. NeuroInterv. Surg. 2018, 10, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Goldhoorn, R.-J.B.; Duijsters, N.; Majoie, C.B.; Roos, Y.B.; Dippel, D.W.; Van Es, A.C.; Vos, J.A.; Boiten, J.; Van Oostenbrugge, R.J.; Van Zwam, W.H.; et al. Balloon Guide Catheter in Endovascular Treatment for Acute Ischemic Stroke: Results from the MR CLEAN Registry. J. Vasc. Interv. Radiol. 2019, 30, 1759–1764.e6. [Google Scholar] [CrossRef] [PubMed]
- Bourcier, R.; Saleme, S.; Labreuche, J.; Mazighi, M.; Fahed, R.; Blanc, R.; Gory, B.; Kyheng, M.; Marnat, G.; Bracard, S.; et al. More than three passes of stent retriever is an independent predictor of parenchymal hematoma in acute ischemic stroke. J. NeuroInterv. Surg. 2018, 11, 625–629. [Google Scholar] [CrossRef]
- Zaidat, O.O.; Ribo, M.; Mattle, H.P.; Saver, J.L.; Bozorgchami, H.; Yoo, A.J.; Ehm, A.; Kottenmeier, E.; Cameron, H.L.; Qadeer, A.R.; et al. Health economic impact of first-pass success among patients with acute ischemic stroke treated with mechanical thrombectomy: A United States and European perspective. J. NeuroInterv. Surg. 2020, 1–7. [Google Scholar] [CrossRef]
| Parameter | Overall (n = 70) | SO (n = 33) | CA (n = 37) | p Value |
|---|---|---|---|---|
| Site of occlusion | 0.262 | |||
| Carotid | 13 | 5 | 8 | |
| M1 | 42 | 18 | 24 | |
| M2 | 15 | 10 | 5 | |
| Age (yrs ± SD) | 71.6 ± 13.4 | 74.2 ± 10.2 | 69.2 ± 15.6 | 0.061 |
| Male sex | 31 | 14 | 17 | 0.813 |
| Atrial fibrillation | 30 | 15 | 15 | 0.810 |
| Diabetes | 19 | 8 | 11 | 0.788 |
| Arterial hypertension | 57 | 27 | 30 | 1.000 |
| Coronary heart disease | 35 | 18 | 17 | 0.632 |
| Dyslipidemia | 31 | 15 | 16 | 1.000 |
| ASPECTS: median, (IQR) | 8, (7–9) | 8, (7–9) | 8, (7–8) | 0.873 |
| NIHSS on admission: median, (IQR) | 17, (14–21) | 17, (14–21) | 16, (14–19) | 0.191 |
| Symptoms to thrombectomy (mean ± SD) | 4:17 ± 1:10 | 4:16 ± 1:25 | 4:17 ± 0:53 | 0.476 |
| iv-rTPa | 42 (60%) | 20 (60.6%) | 22 (59.5%) | 1.000 |
| Goal | SO | CA | OR (95% CI) | p Value |
|---|---|---|---|---|
| First pass mTICI 3 | 6 (18%) | 17 (46%) | 3.83 (1.28–11.44) | 0.016 |
| Procedure success— mTICI 2b-3 | 28 (84.8%) | 35 (94.6%) | 3.13 (0.56–17.34) | 0.193 |
| Total number of passes needed | 2.09 | 1.76 | N/A | 0.114 |
| Mean duration of the procedure (minutes ± SD) | 64 ± 34 | 49 ± 21 | N/A | 0.017 |
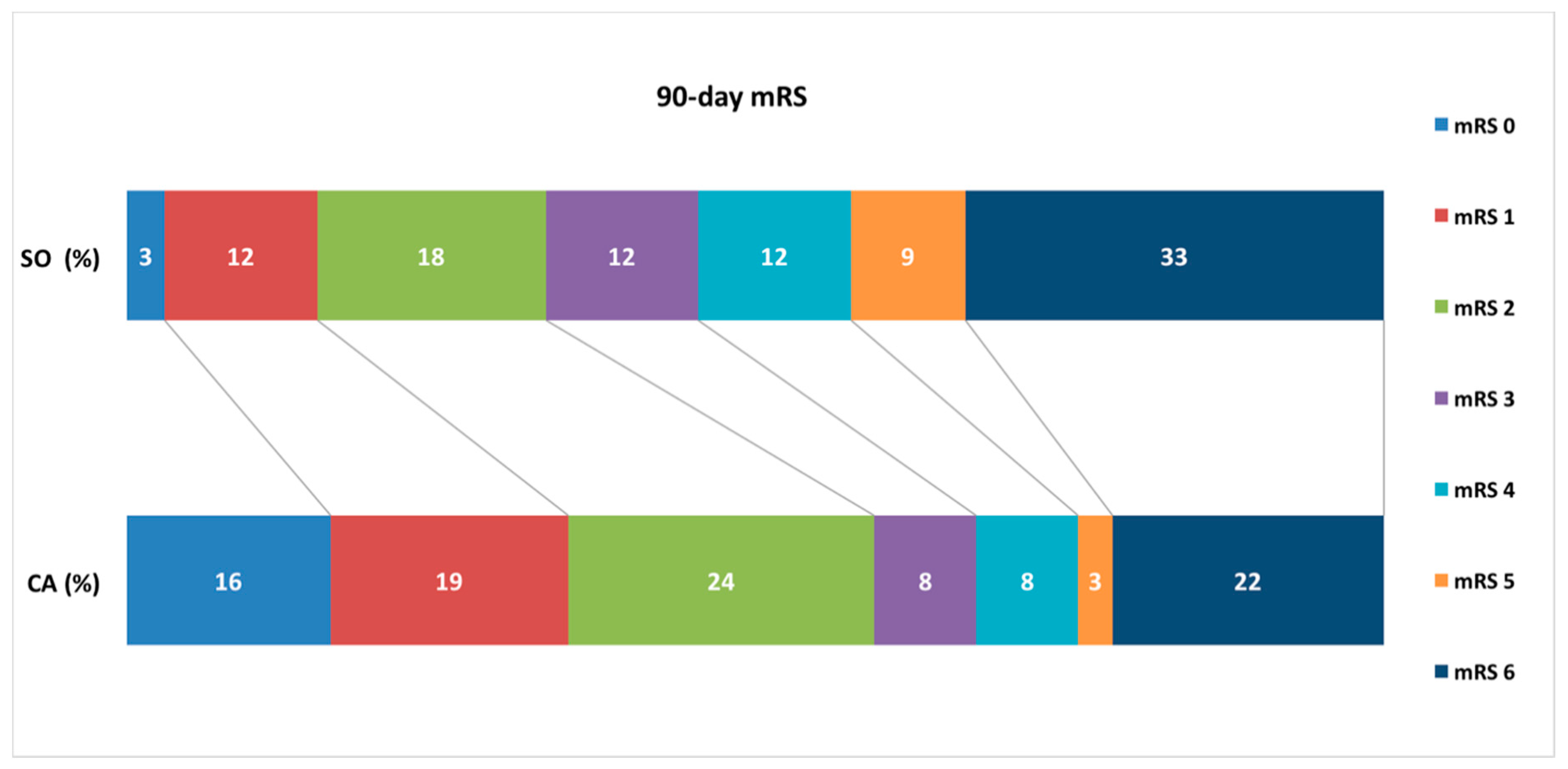
| 90-day mRS: median, (IQR) | 4, (2–6) | 2, (1–4) | N/A | 0.031 |
| Δ NIHSS (± SD) (excluding deaths) | 6.7 ± 4.0 | 9.3 ± 5.1 | N/A | 0.025 |
| Post interv SAH | 2 | 1 | 0.43 (0.04–4.98) | 0.499 |
| sICH | 3 | 5 | 1.56 (0.34–7.11) | 0.564 |
| ENT | 4 | 2 | 0.41 (0.07–2.43) | 0.328 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meder, G.; Żuchowski, P.; Skura, W.; Palacz-Duda, V.; Świtońska, M.; Nowaczewska, M.; Sokal, P. Mechanical Thrombectomy in Stroke. Experience from Switching from Stent Retriever Only to Stent Retriever Combined with Aspiration Catheter. J. Clin. Med. 2021, 10, 1802. https://doi.org/10.3390/jcm10091802
Meder G, Żuchowski P, Skura W, Palacz-Duda V, Świtońska M, Nowaczewska M, Sokal P. Mechanical Thrombectomy in Stroke. Experience from Switching from Stent Retriever Only to Stent Retriever Combined with Aspiration Catheter. Journal of Clinical Medicine. 2021; 10(9):1802. https://doi.org/10.3390/jcm10091802
Chicago/Turabian StyleMeder, Grzegorz, Paweł Żuchowski, Wojciech Skura, Violetta Palacz-Duda, Milena Świtońska, Magdalena Nowaczewska, and Paweł Sokal. 2021. "Mechanical Thrombectomy in Stroke. Experience from Switching from Stent Retriever Only to Stent Retriever Combined with Aspiration Catheter" Journal of Clinical Medicine 10, no. 9: 1802. https://doi.org/10.3390/jcm10091802
APA StyleMeder, G., Żuchowski, P., Skura, W., Palacz-Duda, V., Świtońska, M., Nowaczewska, M., & Sokal, P. (2021). Mechanical Thrombectomy in Stroke. Experience from Switching from Stent Retriever Only to Stent Retriever Combined with Aspiration Catheter. Journal of Clinical Medicine, 10(9), 1802. https://doi.org/10.3390/jcm10091802








