Superior Orbicularis Oris Muscle Activity in Children Surgically Treated for Bilateral Complete Cleft Lip and Palate
Abstract
1. Introduction
2. Materials and Methods
- At rest with the lips relaxed.
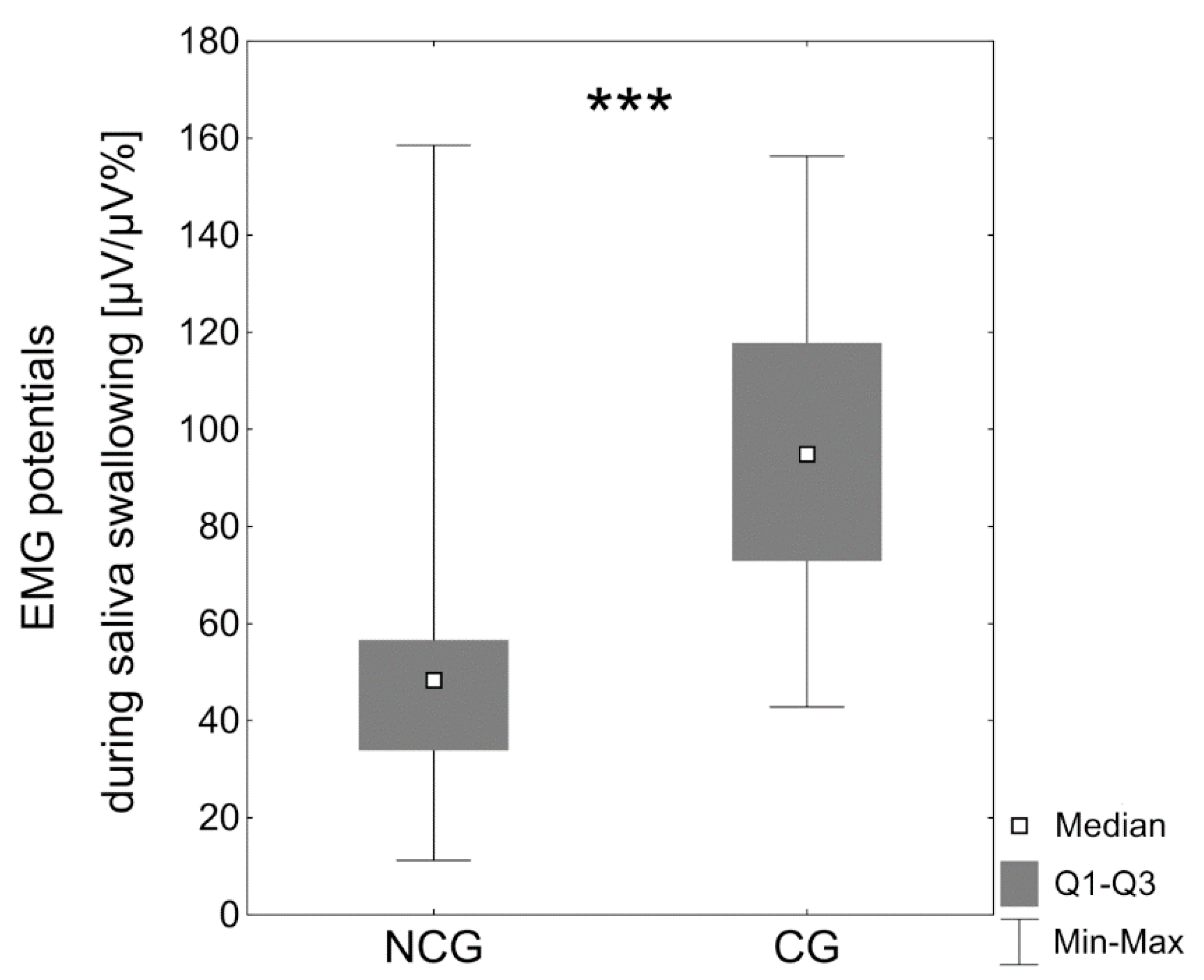
- Saliva swallowing.
- Protrusion of the lips.
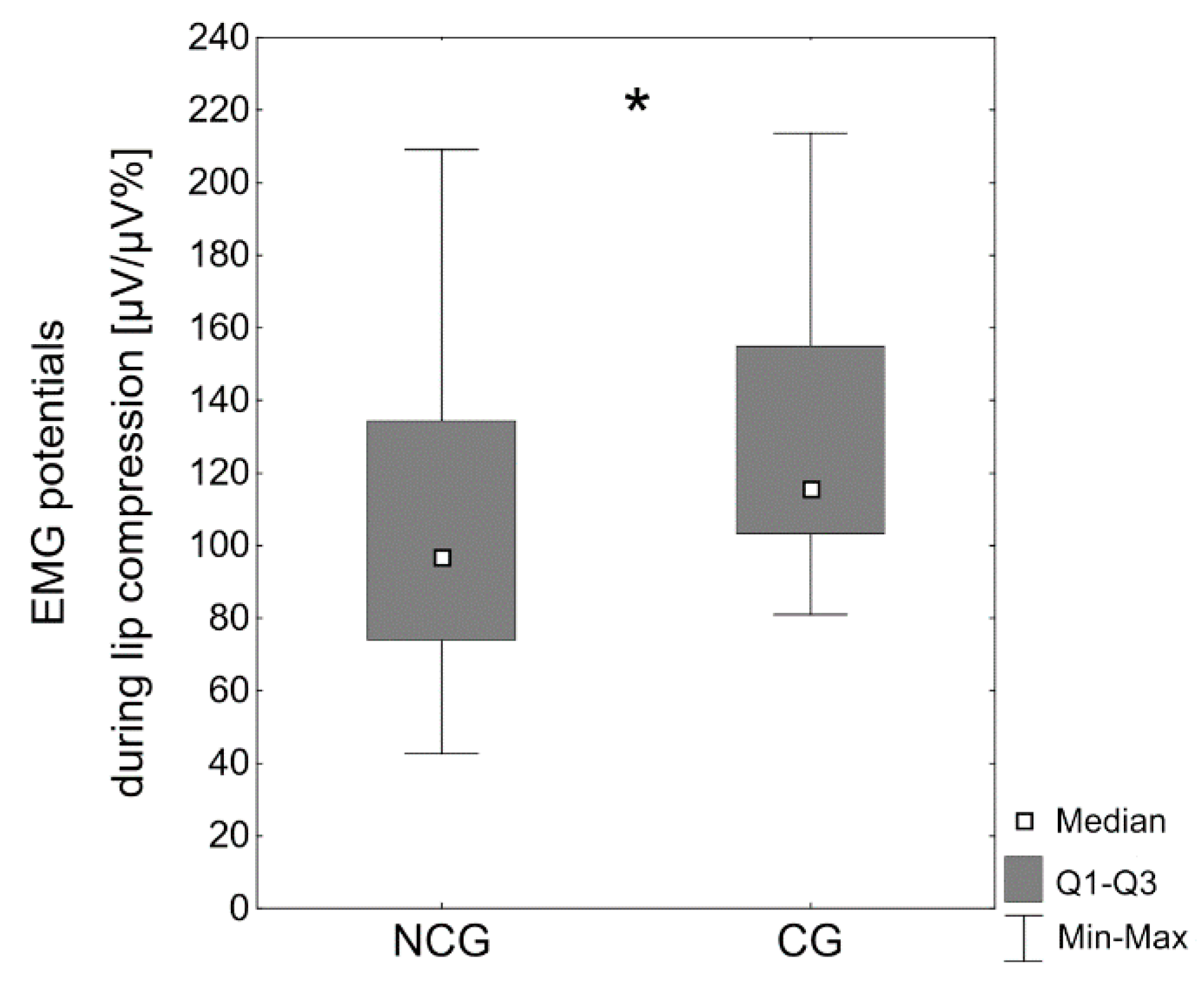
- Compression of the lips.
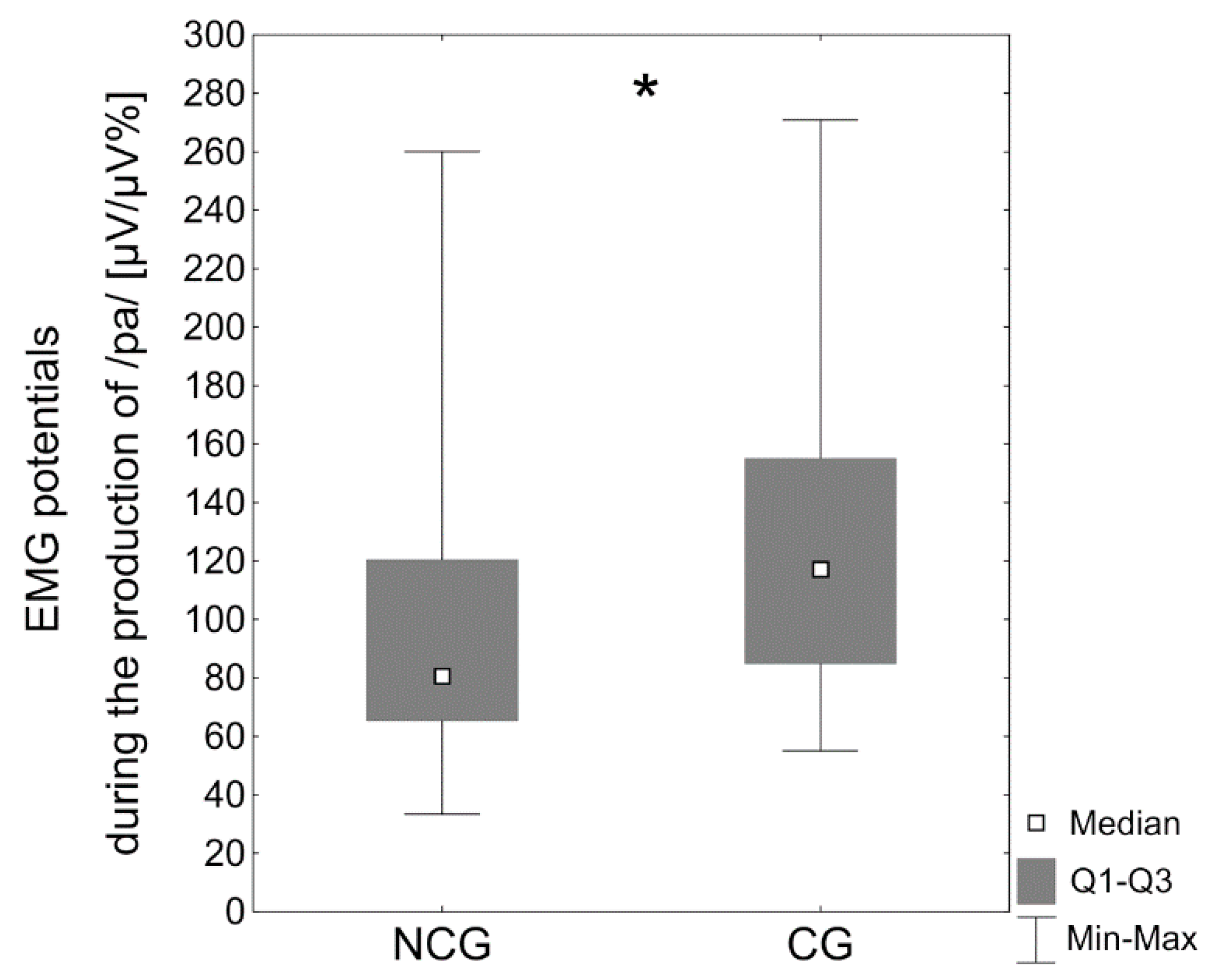
- Formation of the bilabial phoneme /p/ associated with the vowel /a/ in a consonant/vowel context.
- Formation of the bilabial phoneme /b/ associated with the vowel /a/ in a consonant/vowel context.
- Formation of the bilabial phoneme /m/ associated with the vowel /a/ in a consonant/vowel context.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Proffit, W.R. Equilibrium theory revisited: Factors influencing position of the teeth. Angle Orthod. 1978, 48, 175–186. [Google Scholar]
- World Health Organization (WHO). Global Strategies to Reduce the Healthcare Burden of Craniofacial Anomalies; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Mossey, P.A.; Little, J.; Munger, R.G.; Dixon, M.J.; Shaw, W.C. Cleft lip and palate. Lancet 2009, 374, 1773–1785. [Google Scholar] [CrossRef]
- Brons, S.; Meulstee, J.W.; Loonen, T.G.; Nada, R.M.; Kuijpers, M.A.; Bronkhorst, E.M.; Bergé, S.J.; Maal, T.J.; Kuijpers-Jagtman, A.M. Three-dimensional facial development of children with unilateral cleft lip and palate during the first year of life in comparison with normative average faces. PeerJ 2019, 7, e7302. [Google Scholar] [CrossRef]
- Posnick, J.C.; Kinard, B.E. Challenges in the successful reconstruction of cleft lip and palate: Managing the nasomaxillary deformity in adolescence. Plast. Reconstr. Surg. 2020, 145, 591e–603e. [Google Scholar] [CrossRef]
- Kulewicz, M.; Dudkiewicz, Z. Craniofacial morphological outcome following treatment with three different surgical protocols for complete unilateral cleft lip and palate: A preliminary study. Int. J. Oral Maxillofac. Surg. 2010, 39, 122–128. [Google Scholar] [CrossRef]
- Urbanova, W.; Klimova, I.; Brudnicki, A.; Polackova, P.; Kroupova, D.; Dubovska, I.; Rachwalski, M.; Fudalej, P.S. The Slav-cleft: A three-center study of the outcome of treatment of cleft lip and palate. Part 1: Craniofacial morphology. J. Craniomaxillofac. Surg. 2016, 44, 1767–1776. [Google Scholar] [CrossRef] [PubMed]
- Valentová-Strenačiková, S.; Malina, R. Effects of early and late cheiloplasty on anterior part of maxillary dental arch development in infants with unilateral complete cleft lip and palate. PeerJ 2016, 4, e1620. [Google Scholar] [CrossRef]
- Salgado, K.R.; Wendt, A.R.; Fernandes Fagundes, N.C.; Maia, L.C.; Normando, D.; Leão, P.B. Early or delayed palatoplasty in complete unilateral cleft lip and palate patients? A systematic review of the effects on maxillary growth. J. Craniomaxillofac. Surg. 2019, 47, 1690–1698. [Google Scholar] [CrossRef] [PubMed]
- Desmedt, D.J.; Maal, T.J.; Kuijpers, M.A.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M.; Fudalej, P.S. Nasolabial symmetry and esthetics in cleft lip and palate: Analysis of 3D facial images. Clin. Oral Investig. 2015, 19, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.D.; Leonard, A.G.; Burden, D.J.; McSherry, P.F. A comparison of craniofacial form in Northern Irish children with unilateral cleft lip and palate treated with different primary surgical techniques. Cleft Palate Craniofac. J. 2004, 41, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zheng, Q.; Lu, D.; Huang, N.; Li, J.; Li, S.; Wang, Y.; Shi, B. Timing of palate repair affecting growth in complete unilateral cleft lip and palate. J. Craniomaxillofac. Surg. 2012, 40, e358–e362. [Google Scholar] [CrossRef]
- Vura, N.; Gaddipati, R.; Palla, Y.; Kumar, P. An intraoral appliance to retract the protrusive premaxilla in bilateral cleft lip patients presenting late for primary lip repair. Cleft Palate Craniofac. J. 2018, 55, 622–625. [Google Scholar] [CrossRef] [PubMed]
- Latham, R. Development and structure of the premaxillary deformity in bilateral cleft lip and palate. Br. J. Plast. Surg. 1973, 26, 1–11. [Google Scholar] [CrossRef]
- Seo, H.J.; Denadai, R.; Lo, L.J. Long-term nasal growth after primary rhinoplasty for bilateral cleft lip nose deformity: A three-dimensional photogrammetric study with comparative analysis. J. Clin. Med. 2019, 8, 602. [Google Scholar] [CrossRef]
- Mulliken, J.B.; Wu, J.K.; Padwa, B.L. Repair of bilateral cleft lip: Review, revisions, and reflections. J. Craniofac. Surg. 2003, 14, 609–620. [Google Scholar] [CrossRef]
- Liu, Y.; Huang, H.; Shi, B.; Wang, Y. The influence of lip repair on the growth of craniofacial structures in bilateral cleft lip and palate patients with unoperated palate from childhood to adulthood. J. Craniofac. Surg. 2020, 31, 1218–1222. [Google Scholar]
- Handelman, C.S.; Pruzansky, S. Occlusion and dental profile with complete bilateral cleft lip and palate. Angle Orthod. 1968, 38, 185–198. [Google Scholar]
- Silva Filho, O.G.; Valladares Neto, J.; Capelloza Filho, L.; Souza Freitas, J.A. Influence of lip repair on craniofacial morphology of patients with complete bilateral cleft lip and palate. Cleft Palate Craniofac. J. 2003, 40, 144–153. [Google Scholar] [CrossRef]
- Bardach, J. The influence of cleft lip repair on facial growth. Cleft Palate J. 1990, 27, 76–78. [Google Scholar]
- Bardach, J.; Eisbach, K.J. The influence of primary unilateral cleft lip repair of facial growth. Part I: Lip pressure. Cleft Palate J. 1977, 14, 88–97. [Google Scholar]
- Carvajal, R.; Miralles, R.; Cauvi, D.; Berger, B.; Carvajal, A.; Bull, R. Superior orbicularis oris muscle activity in children with and without cleft lip and palate. Cleft Palate Craniofac. J. 1992, 29, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Szyszka-Sommerfeld, L.; Woźniak, K.; Matthews-Brzozowska, T.; Kawala, B.; Mikulewicz, M. Electromyographic analysis of superior orbicularis oris muscle function in children surgically treated for unilateral complete cleft lip and palate. J. Craniomaxillofac. Surg. 2017, 45, 1547–1551. [Google Scholar] [CrossRef] [PubMed]
- Genaro, K.F.; Trindade, A.S.; Trindade, I.E.K. Electromyographic analysis of lip muscle function in operated cleft subjects. Cleft Palate Craniofac. J. 1994, 31, 56–60. [Google Scholar] [CrossRef]
- Carvajal, R.; Miralles, M.R.; Ravera, M.J.; Cauvi, D.; Manns, A.; Carvajal, A. Electromyographic and cephalometric findings in patients with unilateral cleft lip and palate after use of a special removable appliance. Cleft Palate Craniofac. J. 1994, 31, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Normando, A.D.; da Silva Filho, O.G.; Capelozza Filho, L. Influence of surgery on maxillary growth in cleft lip and/or palate patients. J. Craniomaxillofac. Surg. 1992, 20, 111–118. [Google Scholar] [CrossRef]
- Li, Y.; Shi, B.; Song, Q.G.; Zuo, H.; Zheng, Q. Effects of lip repair on maxillary growth and facial soft tissue development in patients with a complete unilateral cleft of lip, alveolus and palate. J. Craniomaxillofac. Surg. 2006, 34, 355–361. [Google Scholar] [CrossRef]
- Xu, X.; Cao, C.; Zheng, Q.; Shi, B. The influence of four different treatment protocols on maxillofacial growth in patients with unilateral complete cleft lip, palate, and alveolus. Plast. Reconstr. Surg. 2019, 144, 180–186. [Google Scholar] [CrossRef]
- Capelozza Filho, L.; Normando, A.D.; da Silva Filho, O.G. Isolated influences of lip and palate surgery on facial growth: Comparison of operated and unoperated male adults with UCLP. Cleft Palate Craniofac. J. 1996, 33, 51–56. [Google Scholar] [CrossRef]
- Göz, G.; Joos, U.; Schilli, W. The influence of lip function on the sagittal and transversal development of the maxilla in cleft patients. Scand. J. Plast. Reconstr. Surg. 1987, 21, 31–34. [Google Scholar] [CrossRef]
- Hermann, N.V.; Jensen, B.L.; Dahl, E.; Bolund, S.; Kreiborg, S. Craniofacial comparisons in 22-month-old lip-operated children with unilateral complete cleft lip and palate and unilateral incomplete cleft lip. Cleft Palate Craniofac. J. 2000, 37, 303–317. [Google Scholar] [CrossRef]
- Semb, G. A study of facial growth in patients with bilateral cleft lip and palate treated by the Oslo CLP Team. Cleft Palate Craniofac. J. 1991, 28, 22–39. [Google Scholar] [CrossRef]
- Nicolau, P.J. The orbicularis oris muscle: A functional approach to its repair in the cleft lip. Br. J. Plast. Surg. 1983, 36, 141–153. [Google Scholar] [CrossRef]
- Woźniak, K.; Piątkowska, D.; Lipski, M.; Mehr, K. Surface electromyography in orthodontics—A literature review. Med. Sci. Monit. 2013, 19, 416–423. [Google Scholar] [PubMed]
- Szyszka-Sommerfeld, L.; Budzyńska, A.; Lipski, M.; Kulesza, S.; Woźniak, K. Assessment of masticatory muscle function in patients with bilateral complete cleft lip and palate and posterior crossbite by means of electromyography. J. Healthc. Eng. 2020, 2020, 8828006. [Google Scholar] [CrossRef]
- Szyszka-Sommerfeld, L.; Lipski, M.; Woźniak, K. Surface electromyography as a method for diagnosing muscle function in patients with congenital maxillofacial abnormalities. J. Healthc. Eng. 2020, 2020, 8846920. [Google Scholar] [CrossRef] [PubMed]
- Szyszka-Sommerfeld, L.; Woźniak, K.; Matthews-Brzozowska, T.; Kawala, B.; Mikulewicz, M.; Machoy, M. The electrical activity of the masticatory muscles in children with cleft lip and palate. Int. J. Paediatr. Dent. 2018, 28, 257–265. [Google Scholar] [CrossRef]
- Ravera, M.J.; Miralles, R.; Santander, H.; Valenzuela, S.; Villaneuva, P.; Zúniga, C. Comparative study between children with and without cleft lip and cleft palate, Part 2: Electromyograhic analysis. Cleft Palate Craniofac. J. 2000, 37, 286–291. [Google Scholar] [CrossRef]
- Woźniak, K.; Piątkowska, D.; Lipski, M. The influence of natural head position on the assessment of facial morphology. Adv. Clin. Exp. Med. 2012, 21, 743–749. [Google Scholar] [PubMed]
- Woźniak, K.; Piątkowska, D.; Szyszka-Sommerfeld, L.; Buczkowska-Radlińska, J. Impact of functional appliances on muscle activity: A surface electromyography study in children. Med. Sci. Monit. 2015, 21, 246–253. [Google Scholar]
- Gustafsson, M.; Ahlgren, J. Mentalis and orbicularis oris activity in children with incompetent lips: An electromyographic and cephalometric study. Acta Odontol. Scand. 1975, 33, 355–363. [Google Scholar] [CrossRef]
- Li, W.; Lin, J.; Fu, M. Electromyographic investigation of masticatory muscles in unilateral cleft lip and palate patients with anterior crossbite. Cleft Palate Craniofac. J. 1998, 35, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Nuño-Licona, A.; Cavazos, E., Jr.; Angeles-Medina, F. Electromyographic changes resulting from orthodontic correction of class III malocclusion. Int. J. Paediatr. Dent. 1993, 3, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Ciccone de Faria Tdos, S.; Hallak Regalo, S.C.; Thomazinho, A.; Vitti, M.; de Felicĩo, C.M. Masticatory muscle activity in children with a skeletal or dentoalveolar open bite. Eur. J. Orthod. 2010, 32, 453–458. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hortis-Dzierzbicka, M.; Radkowska, E.; Stecko, E.; Dudzinski, L.; Fudalej, P.S. Speech outcome in complete unilateral cleft lip and palate—A comparison of three methods of the hard palate closure. J. Oral Rehabil. 2014, 41, 809–815. [Google Scholar] [CrossRef]
- Herreras Mercado, R.; Simpson, K.; Bellom-Rohrbacher, K.H. Effect of prompts for restructuring oral muscular phonetic targets (PROMPT) on compensatory articulation in children with cleft palate/lip. Glob. Pediatr. Health 2019, 6, 1–12. [Google Scholar] [CrossRef]
- Nikhila, K.G.; Prasad, H. A study on patterns of compensatory articulation errors with reference to age of surgery in children with repaired cleft lip and palate. Glob. J. Otolaryngol. 2017, 7, 555706. [Google Scholar] [CrossRef]
- O’Dwyer, N.J.; Quinn, P.T.; Guitar, B.E.; Andrews, G.; Neilson, P.D. Procedures for verification of electrode placement in EMG studies of orofacial and mandibular muscles. J. Speech Lang. Hear. Res. 1981, 24, 273–288. [Google Scholar] [CrossRef]
- Rudney, J.D.; Ji, Z.; Larson, C.J. The prediction of saliva swallowing frequency in humans from estimates of salivary flow rate and the volume of saliva swallowed. Arch. Oral Biol. 1995, 40, 507–512. [Google Scholar] [CrossRef]
- Silva Filho, O.G.; Lauris, R.C.; Capelozza Filho, L.; Semb, G. Craniofacial morphology in adult patients with unoperated complete bilateral cleft lip and palate. Cleft Palate Craniofac. J. 1998, 35, 111–119. [Google Scholar] [CrossRef] [PubMed]

| Variable | Cleft Group Mean Age 9.6 ± 1.9 | Noncleft Group Mean Age 9.2 ± 1.7 | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Gender | Females | 10 | 50 | 34 | 60 |
| Males | 10 | 50 | 23 | 40 | |
| Total | 20 | 100 | 57 | 100 | |
| Place of residence | City | 8 | 40 | 35 | 61 |
| Village | 12 | 60 | 22 | 39 | |
| Total | 20 | 100 | 57 | 100 | |
| Speech disorders | No | 2 | 10 | 57 | 100 |
| Yes | 18 | 90 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Lip seal | Competent | 10 | 50 | 57 | 100 |
| Incompetent | 10 | 50 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Facial profile | Straight | 7 | 35 | 50 | 88 |
| Concave | 6 | 30 | 0 | 0 | |
| Convex | 7 | 35 | 7 | 12 | |
| Total | 20 | 100 | 57 | 100 | |
| Vertical overlap | ≥0 <3 mm | 5 | 25 | 57 | 100 |
| ≥3 mm | 6 | 30 | 0 | 0 | |
| Reverse | 9 | 45 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Overjet | ≥0 <3 mm | 5 | 25 | 57 | 100 |
| ≥3 mm | 6 | 30 | 0 | 0 | |
| Negative | 9 | 45 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Angle class | I | 5 | 25 | 57 | 100 |
| II | 4 | 20 | 0 | 0 | |
| III | 11 | 55 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Posterior crossbite | No | 2 | 10 | 57 | 100 |
| Unilateral | 4 | 20 | 0 | 0 | |
| Bilateral | 14 | 70 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Lateral open bite | No | 7 | 35 | 57 | 100 |
| Yes | 13 | 65 | 0 | 0 | |
| Total | 20 | 100 | 57 | 100 | |
| Activity | 1 Examination | 2 Examination | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Min | Q1 | Mdn | Q3 | Max | Min | Q1 | Mdn | Q3 | Max | |
| Rest | 6.33 | 12.4 | 19.9 | 32.5 | 65.8 | 8.67 | 13.5 | 22.0 | 34.8 | 66.6 |
| Swallowing of saliva | 27.2 | 38.5 | 62.3 | 108.4 | 270.1 | 29.6 | 39.2 | 62.5 | 108.2 | 273.0 |
| Compression of the lips | 48.2 | 91.0 | 125.4 | 150.5 | 209.0 | 47.2 | 90.1 | 127.7 | 151.3 | 210.8 |
| /pa/ | 33.1 | 57.0 | 98.8 | 134.2 | 265.8 | 33.2 | 58.71 | 103.0 | 136.5 | 263.9 |
| /ba/ | 56.7 | 79.0 | 92.0 | 120.9 | 269.5 | 56.2 | 81.9 | 96.5 | 120.0 | 267.9 |
| /ma/ | 34.6 | 66.1 | 92.6 | 155.0 | 260.0 | 34.1 | 65.5 | 96.7 | 156.9 | 262.5 |
| Activity | Cleft Group (CG) | Noncleft Group (NCG) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min | Q1 | Mdn | Q3 | Max | n | Min | Q1 | Mdn | Q3 | Max | |
| Rest | 20 | 4.6 | 13.2 | 20.3 | 25.9 | 50.3 | 57 | 5.7 | 9.0 | 15.4 | 30.1 | 66.5 |
| Swallowing of saliva | 20 | 42.8 | 72.9 | 94.9 | 117.8 | 156.3 | 57 | 11.2 | 33.9 | 48.3 | 56.6 | 158.5 |
| Compression of the lips | 20 | 94.7 | 105.0 | 115.6 | 143.2 | 202.7 | 57 | 42.6 | 74.0 | 96.9 | 134.3 | 209.0 |
| /pa/ | 20 | 55.0 | 84.8 | 117.2 | 155.1 | 270.9 | 57 | 33.4 | 65.3 | 80.6 | 120.4 | 260.1 |
| /ba/ | 20 | 44.1 | 73.7 | 94.9 | 108.8 | 154.9 | 57 | 40.0 | 70.6 | 94.4 | 121.4 | 269.5 |
| /ma/ | 20 | 27.8 | 56.9 | 88.0 | 139.2 | 248.7 | 57 | 30.5 | 61.0 | 85.4 | 120.9 | 167.7 |
| Variable | n | Min | Q1 | Mdn | Q3 | Max | |
|---|---|---|---|---|---|---|---|
| Lip seal | Competent | 10 | 42.8 | 55.6 | 72.9 | 80.2 | 98.9 |
| Incompetent | 10 | 93.7 | 99.3 | 117.8 | 127.5 | 156.3 | |
| Facial profile | Straight or convex | 14 | 42.8 | 60.5 | 79.4 | 96.1 | 99.3 |
| Concave | 6 | 111.7 | 123.9 | 127.5 | 137.5 | 156.3 | |
| Angle class | I or II | 9 | 42.8 | 60.5 | 76.6 | 80.2 | 98.9 |
| III | 11 | 51.7 | 96.1 | 111.7 | 127.5 | 156.3 | |
| Overjet | ≥0 mm | 11 | 42.8 | 55.6 | 76.6 | 91.1 | 98.9 |
| Negative | 9 | 93.7 | 99.3 | 123.9 | 127.5 | 156.3 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szyszka-Sommerfeld, L.; Machoy, M.E.; Wilczyński, S.; Lipski, M.; Woźniak, K. Superior Orbicularis Oris Muscle Activity in Children Surgically Treated for Bilateral Complete Cleft Lip and Palate. J. Clin. Med. 2021, 10, 1720. https://doi.org/10.3390/jcm10081720
Szyszka-Sommerfeld L, Machoy ME, Wilczyński S, Lipski M, Woźniak K. Superior Orbicularis Oris Muscle Activity in Children Surgically Treated for Bilateral Complete Cleft Lip and Palate. Journal of Clinical Medicine. 2021; 10(8):1720. https://doi.org/10.3390/jcm10081720
Chicago/Turabian StyleSzyszka-Sommerfeld, Liliana, Monika Elżbieta Machoy, Sławomir Wilczyński, Mariusz Lipski, and Krzysztof Woźniak. 2021. "Superior Orbicularis Oris Muscle Activity in Children Surgically Treated for Bilateral Complete Cleft Lip and Palate" Journal of Clinical Medicine 10, no. 8: 1720. https://doi.org/10.3390/jcm10081720
APA StyleSzyszka-Sommerfeld, L., Machoy, M. E., Wilczyński, S., Lipski, M., & Woźniak, K. (2021). Superior Orbicularis Oris Muscle Activity in Children Surgically Treated for Bilateral Complete Cleft Lip and Palate. Journal of Clinical Medicine, 10(8), 1720. https://doi.org/10.3390/jcm10081720







