Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
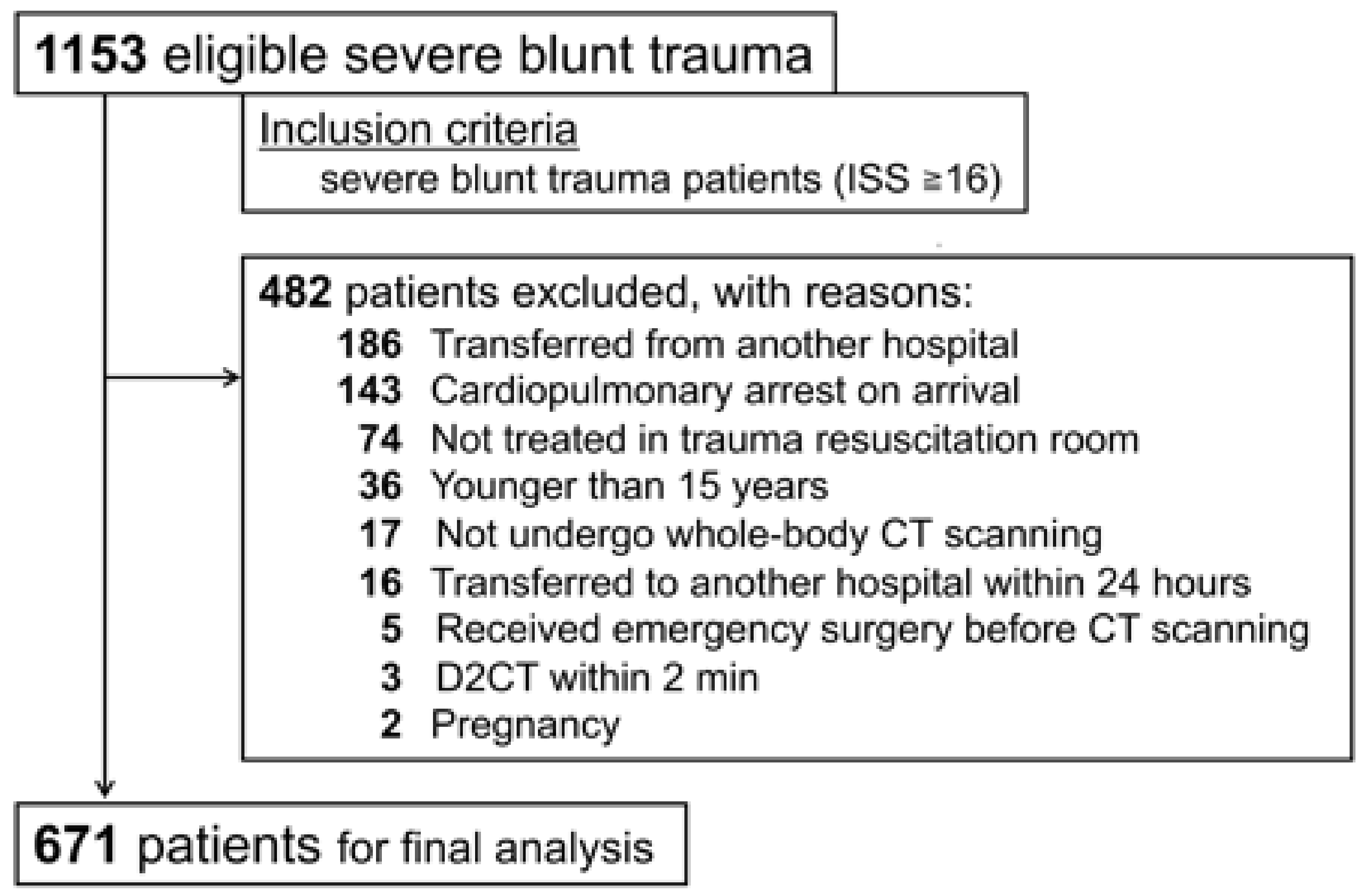
2.2. Patient Population
2.3. Trauma Management Policy
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
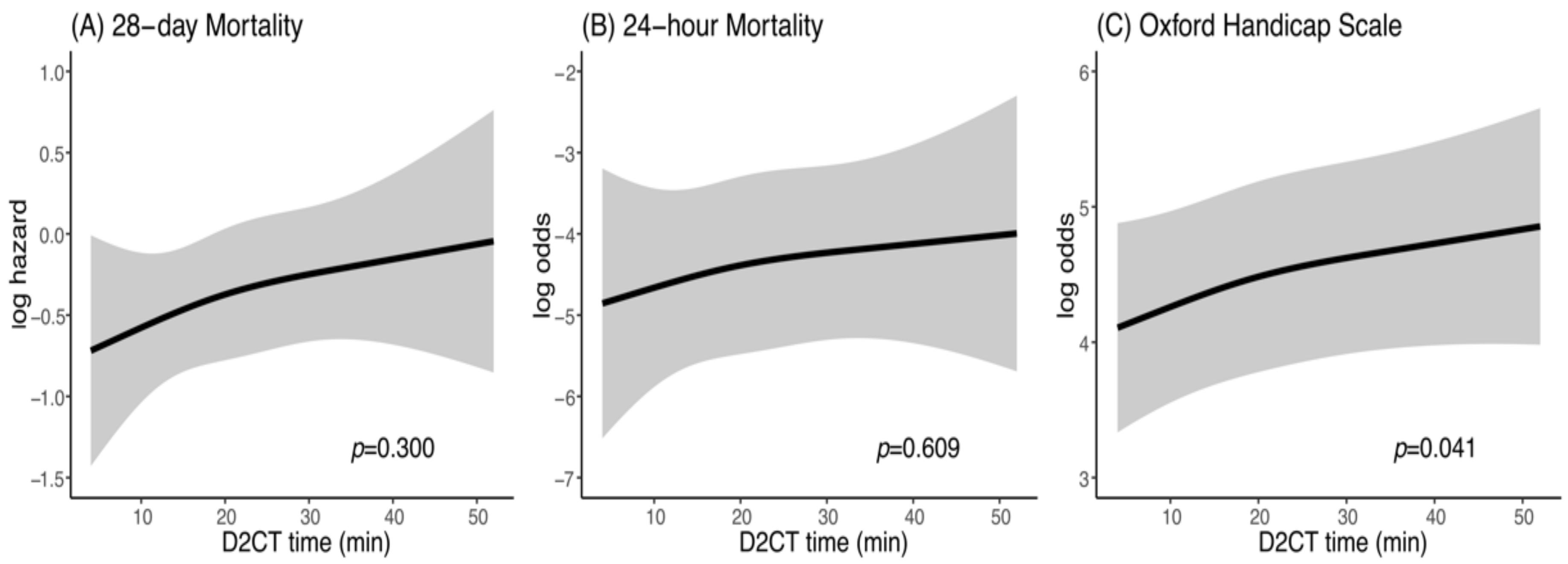
3.2. Effect of Earlier Door-to-CT Time on Mortality
3.3. Effect of Earlier Door-to-CT Time by Cause of Death
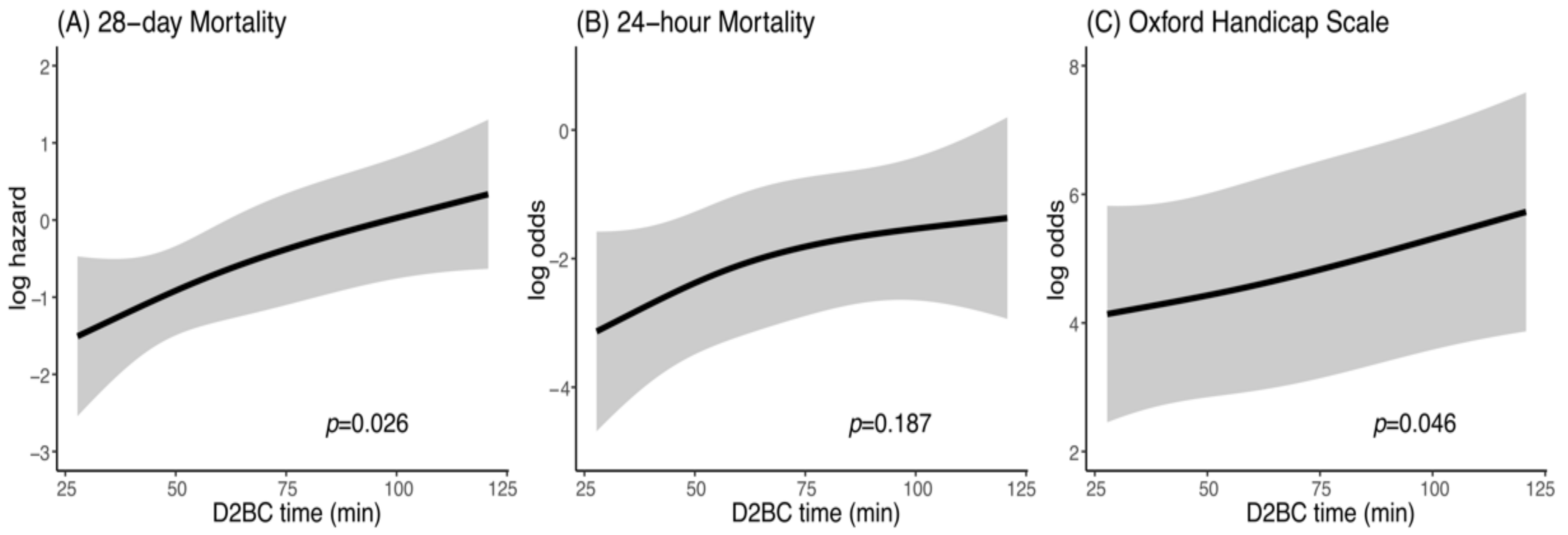
3.4. Effect of Earlier Door-to-Bleeding Control Time on Mortality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Injuries and Violence. The Facts. Available online: https://apps.who.int/iris/bitstream/handle/10665/149798/9789241508018_eng.pdf?sequence=1 (accessed on 12 February 2020).
- Sauaia, A.; Moore, F.A.; Moore, E.E.; Moser, K.S.; Brennan, R.; Read, R.A.; Pons, P.T. Epidemiology of trauma deaths: A reassessment. J. Trauma Acute Care Surg. 1995, 38, 185–193. [Google Scholar] [CrossRef]
- Harvin, J.A.; Maxim, T.; Inaba, K.; Martinez-Aguilar, M.A.; King, D.R.; Choudhry, A.J.; Zielinski, M.D.; Akinyeye, S.; Todd, S.R.; Griffin, R.L.; et al. Mortality after emergent trauma laparotomy: A multicenter, retrospective study. J. Trauma Acute Care Surg. 2017, 83, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Kotwal, R.S.; Montgomery, H.R.; Kotwal, B.M.; Champion, H.R.; Butler, F.K.; Mabry, R.L.; Cain, J.S.; Blackbourne, L.H.; Mechler, K.K.; Holcomb, J.B. Eliminating preventable death on the battlefield. Arch Surg. 2011, 146, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.B.; Pati, S. Optimal trauma resuscitation with plasma as the primary resuscitative fluid: The surgeon’s perspective. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Deunk, J.; Dekker, H.M.; Brink, M.; van Vugt, R.; Edwards, M.J.; van Vugt, A.B. The value of indicated computed tomography scan of the chest and abdomen in addition to the conventional radiologic work-up for blunt trauma patients. J. Trauma Acute Care Surg. 2007, 63, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Mistral, T.; Brenckmann, V.; Sanders, L.; Bosson, J.L.; Ferretti, G.; Thony, F.; Galvagno, S.M.; Payen, J.F.; Bouzat, P. Clinical judgment is not reliable for reducing whole-body computed tomography scanning after isolated high-energy blunt trauma. Anesthesiology 2017, 126, 1116–1124. [Google Scholar] [CrossRef] [PubMed]
- Langdorf, M.I.; Medak, A.J.; Hendey, G.W.; Nishijima, D.K.; Mower, W.R.; Raja, A.S.; Baumann, B.M.; Anglin, D.R.; Anderson, C.L.; Lotfipour, S.; et al. Prevalence and clinical import of thoracic injury identified by chest computed tomography but not chest radiography in blunt trauma: Multicenter prospective cohort study. Ann. Emerg. Med. 2015, 66, 589–600. [Google Scholar] [CrossRef]
- Weninger, P.; Mauritz, W.; Fridrich, P.; Spitaler, R.; Figl, M.; Kern, B.; Hertz, H. Emergency room management of patients with blunt major trauma: Evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J. Trauma Acute Care Surg. 2007, 62, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Gralla, J.; Spycher, F.; Pignolet, C.; Ozdoba, C.; Vock, P.; Hoppe, H. Evaluation of a 16-MDCT scanner in an emergency department: Initial clinical experience and workflow analysis. AJR Am. J. Roentgenol. 2005, 185, 232–238. [Google Scholar] [CrossRef]
- Kanz, K.G.; Paul, A.O.; Lefering, R.; Kay, M.V.; Kreimeier, U.; Linsenmaier, U.; Mutschler, W.; Huber-Wagner, S. Trauma management incorporating focused assessment with computed tomography in trauma (FACTT)—Potential effect on survival. J. Trauma Manag. Outcomes 2010, 4, 4. [Google Scholar] [CrossRef]
- Sierink, J.C.; Treskes, K.; Edwards, M.J.; Beuker, B.J.; den Hartog, D.; Hohmann, J.; Dijkgraaf, M.G.; Luitse, J.S.; Beenen, L.F.; Hollmann, M.W.; et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): A randomised controlled trial. Lancet 2016, 388, 673–683. [Google Scholar] [CrossRef]
- Hilbert, P.; Zur Nieden, K.; Hofmann, G.O.; Hoeller, I.; Koch, R.; Stuttmann, R. New aspects in the emergency room management of critically injured patients: A multi-slice CT-oriented care algorithm. Injury 2007, 38, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Wurmb, T.E.; Frühwald, P.; Hopfner, W.; Keil, T.; Kredel, M.; Brederlau, J.; Roewer, N.; Kuhnigk, H. Whole-body multislice computed tomography as the first line diagnostic tool in patients with multiple injuries: The focus on time. J. Trauma Manag. Outcomes 2009, 66, 658–665. [Google Scholar] [CrossRef]
- Saltzherr, T.P.; Bakker, F.C.; Beenen, L.F.; Dijkgraaf, M.G.; Reitsma, J.B.; Goslings, J.C. Randomized clinical trial comparing the effect of computed tomography in the trauma room versus the radiology department on injury outcomes. Br. J. Surg. 2012, 99, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Jin, P.H.; Goslings, J.C.; Ponsen, K.J.; van Kuijk, C.; Hoogerwerf, N.; Luitse, J.S. Assessment of a new trauma workflow concept implementing a sliding CT scanner in the trauma room: The effect on workup times. J. Trauma Acute Care Surg. 2008, 64, 1320–1326. [Google Scholar] [CrossRef]
- Lee, K.L.; Graham, C.A.; Lam, J.M.; Yeung, J.H.; Ahuja, A.T.; Rainer, T.H. Impact on trauma patient management of installing a computed tomography scanner in the emergency department. Injury 2009, 40, 873–875. [Google Scholar] [CrossRef]
- Huber-Wagner, S.; Mand, C.; Ruchholtz, S.; Kühne, C.A.; Holzapfel, K.; Kanz, K.G.; van Griensven, M.; Biberthaler, P.; Lefering, R. Effect of the localisation of the CT scanner during trauma resuscitation on survival—A retrospective, multicentre study. Injury 2014, 45, 76–82. [Google Scholar] [CrossRef]
- Kinoshita, T.; Yamakawa, K.; Matsuda, H.; Yoshikawa, Y.; Wada, D.; Hamasaki, T.; Ono, K.; Nakamori, Y.; Fujimi, S. The survival benefit of a novel trauma workflow that includes immediate whole-body computed tomography, surgery, and interventional radiology, all in one trauma resuscitation room: A retrospective historical control study. Ann. Surg. 2019, 269, 370–376. [Google Scholar] [CrossRef]
- Committee of the Japan Association of Traumatology. The Japan Advanced Trauma Evaluation and Care (JATEC), 5th ed.; Herusu Shuppan Co Inc.: Tokyo, Japan, 2016. [Google Scholar]
- Harrell, F.E., Jr. Package ‘rms’. Available online: https://cran.r-project.org/web/packages/rms/rms.pdf (accessed on 12 February 2020).
- Antman, E.M.; Anbe, D.T.; Armstrong, P.W.; Bates, E.R.; Green, L.A.; Hand, M.; Hochman, J.S.; Krumholz, H.M.; Kushner, F.G.; Lamas, G.A.; et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction-executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J. Am. Coll. Cardiol. 2004, 44, 671–719. [Google Scholar]
- Saver, J.L. Time is brain-quantified. Stroke 2006, 37, 263–266. [Google Scholar] [CrossRef]
- Meizoso, J.P.; Ray, J.J.; Karcutskie, C.A., IV; Allen, C.J.; Zakrison, T.L.; Pust, G.D.; Koru-Sengul, T.; Ginzburg, E.; Pizano, L.R.; Schulman, C.I.; et al. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: The golden 10 minutes. J. Trauma Acute Care Surg. 2016, 81, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.R.; Trooskin, S.Z.; Doshi, P.J.; Greenwald, L.; Mode, C.J. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J. Trauma Acute Care Surg. 2002, 52, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A.; Medina, M.; Cotton, B.A.; Rahbar, E.; Wade, C.E.; Cohen, A.M.; Beeler, A.M.; Burgess, A.R.; Holcomb, J.B. Are we delivering two standards of care for pelvic trauma? Availability of angioembolization after hours and on weekends increases time to therapeutic intervention. J. Trauma Acute Care Surg. 2014, 76, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Uyeda, J.W.; LeBedis, C.A.; Penn, D.R.; Soto, J.A.; Anderson, S.W. Active hemorrhage and vascular injuries in splenic trauma: Utility of the arterial phase in multidetector CT. Radiology 2014, 270, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Iacobellis, F.; Scaglione, M.; Brillantino, A.; Scuderi, M.G.; Giurazza, F.; Grassi, R.; Noschese, G.; Niola, R.; Al Zuhir, N.Y.; Romano, L. The additional value of the arterial phase in the CT assessment of liver vascular injuries after high-energy blunt trauma. Emerg. Radiol. 2019, 26, 647–654. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n = 671 |
|---|---|
| Age, years | 51 (35–65) |
| Sex, male | 463 (69.0%) |
| Mechanism of injury | |
| Motor vehicle accident | 370 (55.1%) |
| Fall from a height | 161 (24.0%) |
| Fall down steps | 52 (7.7%) |
| Ground-level fall | 32 (4.8%) |
| Crushed between objects | 16 (2.4%) |
| Others | 40 (6.0%) |
| GCS total score | 13 (8–14) |
| HR, beats per min | 91 (78–108) |
| Systolic BP, mm Hg | 131 (78–108) |
| Shock index ≥ 1 | 140 (20.9%) |
| RR, per min | 22 (18–28) |
| BT, °Celsius | 36.5 (36.0–36.8) |
| RTS | 7.1 (6.0–7.8) |
| Hb, g/dL | 13.1 (11.8–14.4) |
| pH | 7.39 (7.34–7.42) |
| Lactate, mmol/L | 2.4 (1.6–3.6) |
| PT-INR | 1.1 (1.1–1.2) |
| Activated partial thromboplastin time, s | 29.9 (27.0–35.8) |
| AIS Head ≥ 3 | 477 (71.1%) |
| AIS Face ≥ 3 | 11 (1.6%) |
| AIS Chest ≥ 3 | 351 (52.3%) |
| AIS Abdomen ≥ 3 | 126 (18.7%) |
| AIS Extremities ≥ 3 | 232 (34.5%) |
| Injury Severity Score | 26 (21–35) |
| Probability of survival | 0.91 (0.71–0.97) |
| Emergency bleeding control procedure | 163 (24.3%) |
| Bleeding control surgery | 65 (9.7%) |
| Interventional radiology | 133 (19.8%) |
| Intracranial surgery | 174 (25.9%) |
| Parameter | Value |
|---|---|
| Door-to-CT time, min | 19 (12–27) |
| Door-to-bleeding control time, min | 57 (45–75) |
| 28-day mortality | 112 (17%) |
| Exsanguination | 27 (4%) |
| TBI | 73 (11%) |
| MODS | 5 (1%) |
| Sepsis | 2 (1%) |
| Respiratory | 2 (1%) |
| Others | 3 (1%) |
| 24-h mortality | 65 (10%) |
| Exsanguination | 27 (4%) |
| TBI | 36 (5%) |
| MODS | 0 (0%) |
| Sepsis | 0 (0%) |
| Respiratory | 2 (1%) |
| Others | 0 (0%) |
| Oxford Handicap Scale | 3 (2–5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murao, S.; Yamakawa, K.; Kabata, D.; Kinoshita, T.; Umemura, Y.; Shintani, A.; Fujimi, S. Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 1522. https://doi.org/10.3390/jcm10071522
Murao S, Yamakawa K, Kabata D, Kinoshita T, Umemura Y, Shintani A, Fujimi S. Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(7):1522. https://doi.org/10.3390/jcm10071522
Chicago/Turabian StyleMurao, Shuhei, Kazuma Yamakawa, Daijiro Kabata, Takahiro Kinoshita, Yutaka Umemura, Ayumi Shintani, and Satoshi Fujimi. 2021. "Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 7: 1522. https://doi.org/10.3390/jcm10071522
APA StyleMurao, S., Yamakawa, K., Kabata, D., Kinoshita, T., Umemura, Y., Shintani, A., & Fujimi, S. (2021). Effect of Earlier Door-to-CT and Door-to-Bleeding Control in Severe Blunt Trauma: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(7), 1522. https://doi.org/10.3390/jcm10071522







