Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study
Abstract
1. Introduction
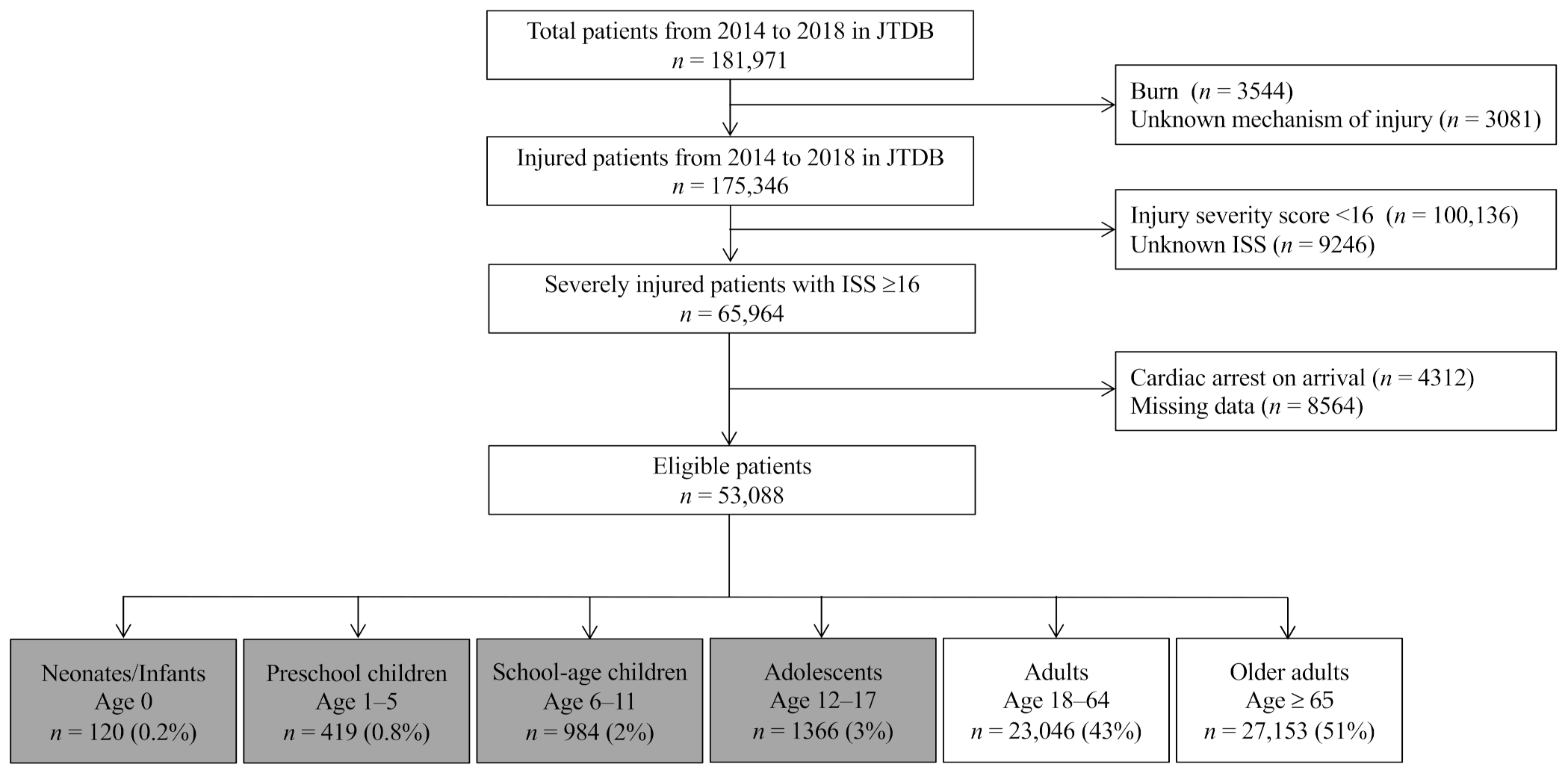
2. Materials and Methods
2.1. Study Setting and Population
2.2. Data Collection
2.3. Ethics Statement
2.4. Statistical Analysis
3. Results
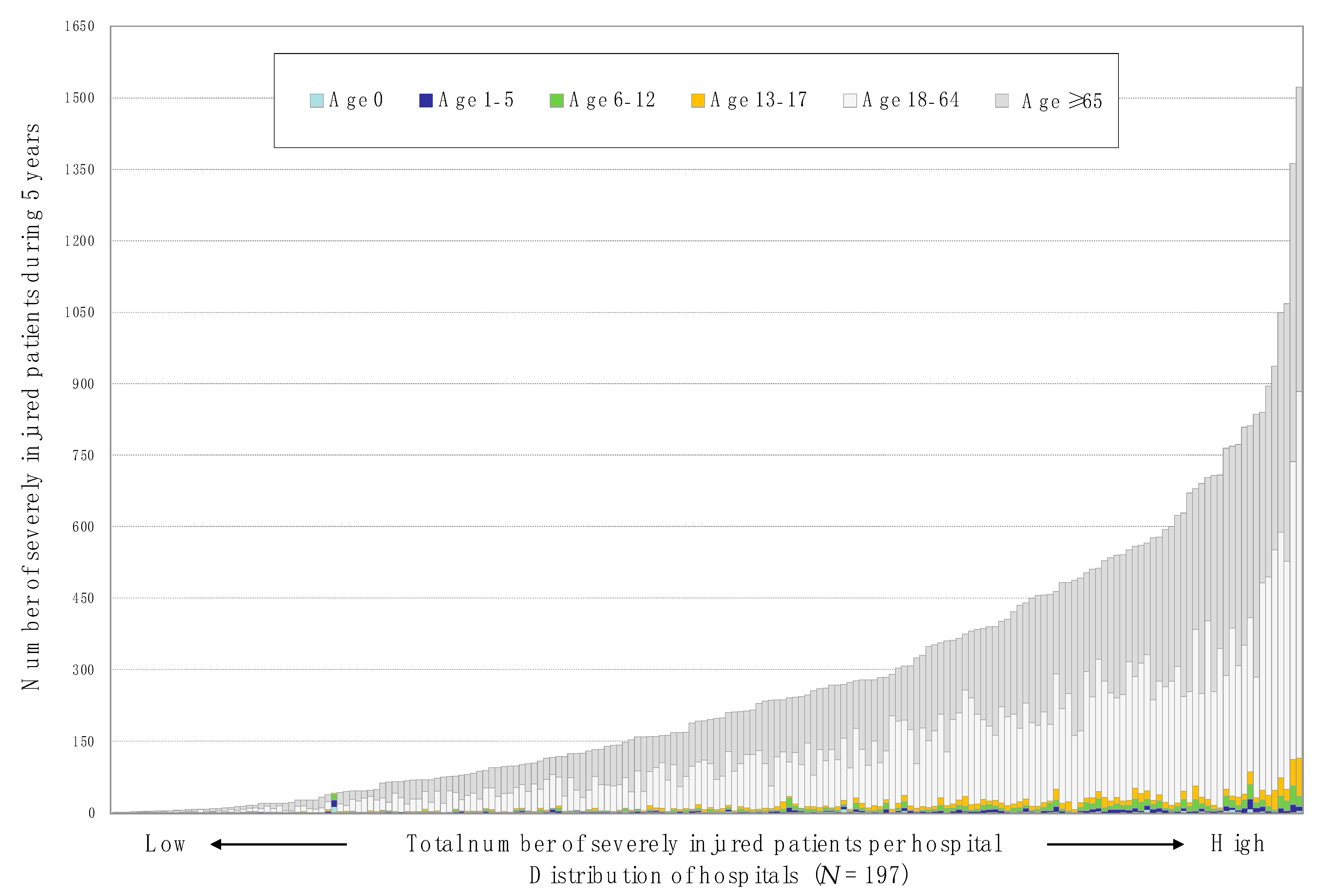
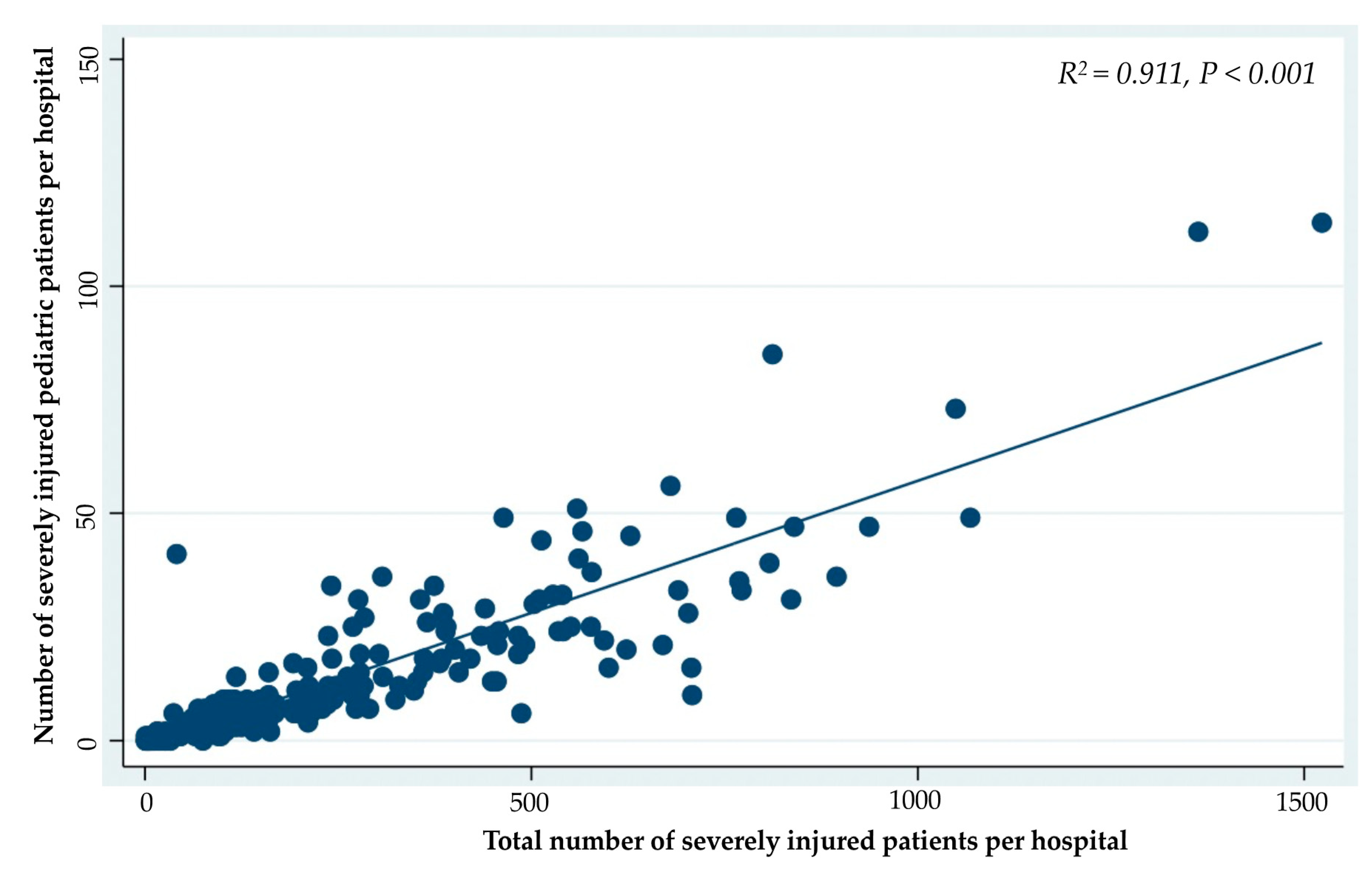
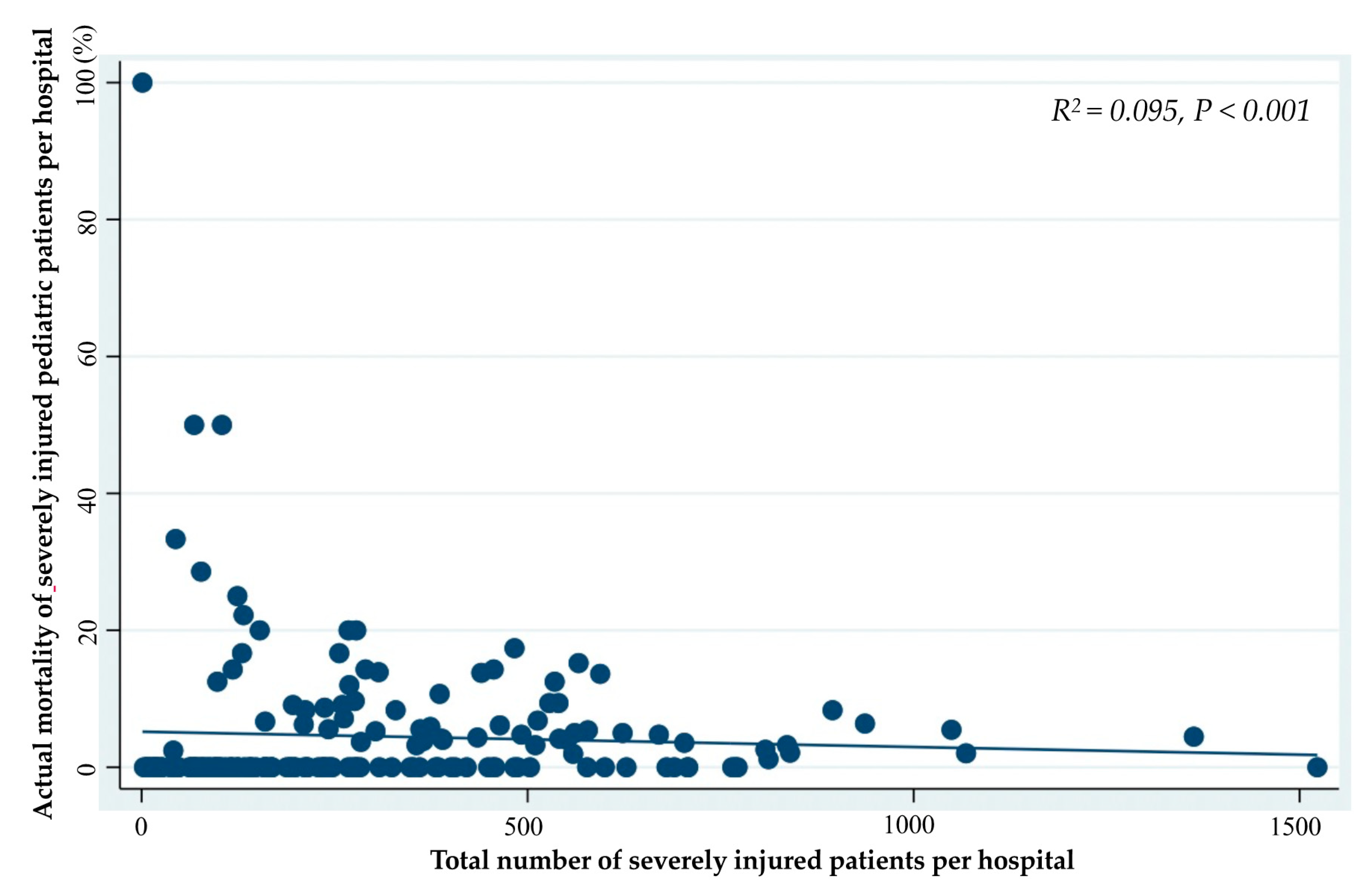
3.1. Correlation Analysis
3.2. Comparison of High-Volume Hospitals with the Low-Volume Hospitals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- McCarthy, A.; Curtis, K.; Holland, A.J.A. Paediatric trauma systems and their impact on the health outcomes of severely injured children: An integrative review. Injury 2016, 47, 574–585. [Google Scholar] [CrossRef] [PubMed]
- Janssens, L.; Holtslag, H.R.; van Beeck, E.F.; Leenen, L.P.H. The effect of regionalization of pediatric trauma care in the Netherlands: A surveillance-based before-after study. J. Trauma Acute Surg. 2012, 73, 1284–1287. [Google Scholar] [CrossRef] [PubMed]
- Doolin, E.J.; Browne, A.M.; DiScala, C. Pediatric trauma center criteria: An outcomes analysis. J. Pediatr. Surg. 1999, 34, 885–889. [Google Scholar] [CrossRef]
- Walther, A.E.; Pritts, T.A.; Falcone, R.A.; Hanseman, D.H.; Robinson, B.R.H. Teen trauma without the drama: Outcomes of adolescents treated at Ohio adult versus pediatric trauma centers. J. Trauma Acute Surg. 2014, 77, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M.; Endo, A.; Shiraishi, A.; Otomo, Y. Age-related characteristics and outcomes for patients with severe trauma: Analysis of Japan’s Nationwide trauma registry. Ann. Emerg. Med. 2019, 73, 281–290. [Google Scholar] [CrossRef]
- Sewalt, C.A.; Wiegers, E.J.A.; Cenema, E.; Lecky, F.E.; Schuit, S.C.E.; Den Hartog, D.; Lingsma, H.F. The volume-outcome relationship in severely injured patients: A systematic review and meta-analysis. J. Trauma Acute Surg. 2018, 85, 810–819. [Google Scholar] [CrossRef]
- Zacher, M.T.; Kanz, K.-G.; Hanschen, M.; Haberle, S.; Griensven, M.V.; Lefering, R.; Bühren, V.; Biberthaler, P.; Huber-Wagner, S.; TraumaRegister DGU®. Association between volume of severely injured patients and mortality in German trauma hospitals. Br. J. Surg. 2015, 102, 1213–1219. [Google Scholar] [CrossRef]
- Aoki, M.; Abe, T.; Saito, D.; Hagiwara, S.; Oshima, K. Severe trauma patient volume was associated with decreased mortality. Eur. J. Trauma Emerg. Surg. 2020, 1–8. [Google Scholar] [CrossRef]
- Caputo, L.M.; Salottolo, K.M.; Slone, D.S.; Mains, C.W.; Bar-Or, D. The relationship between patient volume and mortality in American trauma centres: A systematic review of the evidence. Injury 2014, 45, 478–486. [Google Scholar] [CrossRef]
- Morimura, N.; Kitano, M.; Hayashi, M.; Doi, T.; Fujita, T. Establishment of a local government designated major trauma centre process of introduction to the Yokohama city major trauma centre. J. Jpn. Assoc. Surg. Trauma 2017, 31, 79–86. [Google Scholar]
- Japan Trauma Data Bank. Available online: https://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2019e.pdf (accessed on 23 October 2020).
- Pearson, G.; Shann, F.; Barry, P.; Vyas, J.; Thomas, D.; Powell, C.; Field, D. Should paediatric intensive care be centralized? Trent versus Victoria. Lancet 1997, 349, 1213–1217. [Google Scholar] [CrossRef]
- McGrath, P.D.; Wennberg, D.E.; Dickens, J.D.; Siewers, A.E.; Lucas, F.L.; Malenka, D.J.; Kellett, M.A., Jr.; Ryan, T.J., Jr. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA 2000, 284, 3139–3144. [Google Scholar] [CrossRef]
- Begg, C.B.; Cramer, L.D.; Hoskins, W.J. Impact of hospital volume on operative mortality for major cancer surgery. JAMA 1998, 280, 1747–1751. [Google Scholar] [CrossRef]
- Chih-Yuan, F.; Bajani, F.; Tatebe, L.; Butler, C.; Starr, F.; Dennis, A.; Kaminsky, M.; Messer, T.; Schlanser, V.; Kramer, K.; et al. Right hospital, right patients: Penetrating injury patients treated at high-volume penetrating trauma centers have lower mortality. J. Trauma Acute Care Surg. 2019, 86, 961–966. [Google Scholar]
- Lansink, K.W.W.; Leenen, L.P.H. Do designated trauma systems improve outcome? Curr. Opin. Crit. Care 2007, 13, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.A.; Vernard, A.C.; Bottiggi, A.J.; Chang, P.K.; Talley, C.L.; Tucker, B. Influence of in-house attending presence on trauma outcomes and hospital efficiency. J. Am. Coll. Surg. 2014, 218, 734–738. [Google Scholar] [CrossRef]
- Sampalis, J.S.; Lavoie, A.; Williams, J.I.; Mulder, D.S.; Kalina, M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J. Trauma 1993, 34, 252–261. [Google Scholar] [CrossRef]
- Macnab, A.J.; Wensley, D.F.; Sun, C. Cost-benefit of trained transport teams: Estimates for head-injured children. Prehosp. Emerg. Care 2001, 5, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Dieppe, C.; Lo, T.Y.M.; McFadzean, J.; Rowney, D.A. Specialist team retrieval of head injured patients: Fact, fiction, of formula? Intensive Care Med. 2009, 35, 334–338. [Google Scholar] [CrossRef]
- Hewes, H.A.; Christensen, M.; Taillac, P.P.; Mann, N.C.; Jacobsen, K.K.; Fenton, S.J. Consequence of pediatric undertriage and overttriage in a statewide trauma system. J. Trauma Acute Care Surg. 2017, 83, 662–667. [Google Scholar] [CrossRef]
- Larson, J.T.; Dietrich, A.M.; Abdessalam, S.F.; Werman, H.A. Effective use of the air ambulance for pediatric trauma. J. Trauma 2004, 56, 89–93. [Google Scholar] [CrossRef]
- Brohi, K.; Gruen, R.L.; Holcomb, J.B. Why are bleeding trauma patients still dying? Intensive Care Med. 2019, 45, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L.; et al. Epidemiology of traumatic brain injury in Europe: A living systematic review. J. Neurotrauma 2018, 33, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Toida, C.; Muguruma, T.; Gakumazawa, M.; Shinohara, M.; Abe, T.; Takeuchi, I.; Morimura, N. Age- and severity-related in-hospital mortality trends and risks of severe traumatic brain injury in Japan: A nationwide 10-year retrospective study. J. Clin. Med. 2021, 10, 1072. [Google Scholar] [CrossRef]
- Adzemovic, T.; Murray, T.; Jenkins, P.; Ottosen, J.; Iyegha, U.; Raghavendran, K.; Napolitano, L.M.; Hemmila, M.R.; Gipson, J.; Park, P.; et al. Should they stay or should they go? Who benefits from interfacility transfer to a higher-level trauma center following initial presentation at a lower-level trauma center. J. Trauma Acute Care Surg. 2019, 86, 952–960. [Google Scholar] [CrossRef]
- Brown, B.B.; Gestring, M.L.; Leeper, C.M.; Sperry, J.L.; Peitzman, A.B.; Billiar, T.R.; Gaines, B.A. The value of the injury severity score in pediatric trauma: Time for a new definition of severe injury? J. Trauma Acute Care Surg. 2017, 82, 995–1001. [Google Scholar] [CrossRef] [PubMed]
| R2 | p-Value | |
|---|---|---|
| Correlation between the Number of Total Patients and the Number of Severely Injured Pediatric Patients Who Underwent | ||
| Interhospital transportation | 0.453 | <0.001 |
| Urgent treatment | ||
| Blood transfusion within 24 h | 0.499 | <0.001 |
| Transcatheter arterial embolization | 0.286 | <0.001 |
| Craniotomy and/or craterization | 0.435 | <0.001 |
| Thoracotomy | 0.117 | <0.001 |
| Celiotomy | 0.325 | <0.001 |
| Variables | All Hospitals | High-Volume Hospitals | Low-Volume Hospitals | p-Value |
|---|---|---|---|---|
| (176 Hospitals) | (13 Hospitals) | (163 Hospitals) | ||
| Total number of severely injured patients | 52,834 | 40,397 | 12,437 | |
| Total number per institution, (median, min–max) | 235 (1–1523) | 840 (765–1523) | 210 (1–708) | <0.001 |
| 0 year | 0 (0–12) | 1 (0–7) | 0 (0–12) | 0.005 |
| 1–5 years | 1(0–22) | 9 (1–22) | 1 (0–14) | <0.001 |
| 6–12 years | 3 (0–39) | 17 (4–39) | 3 (0–24) | <0.001 |
| 13–17 years | 5 (2–80) | 24 (10–80) | 4 (0–29) | <0.001 |
| 18–64 years | 93 (0–770) | 435 (238–770) | 89 (0–374) | <0.001 |
| ≥65 years | 113 (0–639) | 461 (358–639) | 99 (0–43) | <0.001 |
| PEDIATRIC | ||||
| Total number of severely injured pediatric patients | 2889 | 2139 | 750 | |
| Total number of severely injured pediatric patients per institution, (median, min–max) | 10 (1–114) | 47 (31–114) | 9 (1–56) | <0.001 |
| Blunt trauma, number of pediatric patients per institution, (median, min–max) | 10 (1–113) | 47 (31–113) | 9 (1–56) | <0.001 |
| Transport type, number of pediatric patients per institution, (median, min–max) | ||||
| Ambulance | 8 (0–96) | 28 (8–96) | 7 (0–43) | <0.001 |
| Ambulance with physician | 0 (0–31) | 3 (0–31) | 0 (0–24) | <0.001 |
| Helicopter with physician | 0 (0–61) | 9 (0–61) | 0 (0–12) | <0.001 |
| Transfer process, number of pediatric patients per institution, (median, min–max) | ||||
| From the scene | 8 (3–109) | 38 (20–109) | 7 (0–49) | <0.001 |
| From the other hospital | 2 (0–36) | 11 (3–36) | 1 (0–28) | <0.001 |
| Injury region, number of pediatric patients per institution, (median, min–max) | ||||
| Polytrauma | 3 (0–64) | 17 (4–64) | 3 (0–24) | <0.001 |
| Head injury with AIS ≥3 | 7 (0–73) | 27 (19–73) | 7 (0–44) | <0.001 |
| Facial injury with AIS ≥3 | 0 (0–6) | 0 (0–6) | 0 (0–4) | 0.022 |
| Neck injury with AIS ≥3 | 0 (0–2) | 0 (0–2) | 0 (0–1) | 0.231 |
| Chest injury with AIS ≥3 | 3 (0–63) | 19 (5–63) | 3 (0–25) | <0.001 |
| Abdominal and pelvic injury with AIS ≥3 | 1 (0–18) | 7 (1–18) | 1 (0–12) | <0.001 |
| Spinal injury with AIS ≥3 | 0 (0–9) | 4 (0–9) | 0 (0–9) | <0.001 |
| Upper extremity injury with AIS ≥3 | 0 (0–10) | 0 (0–10) | 0 (0–3) | <0.001 |
| Lower extremity injury with AIS ≥3 | 1 (0–35) | 7 (1–35) | 1 (0–12) | <0.001 |
| ISS score range, total number of severely injured pediatric patients | ||||
| 16–25 | 2018 | 1491 | 527 | <0.001 |
| >25 | 871 | 648 | 223 | <0.001 |
| Revised trauma score per institution, (median, min–max) | 7.15 (4.00–7.84) | 7.12 (6.39–7.06) | 7.16 (4.00–7.84) | 0.874 |
| TRISS score per institution, (median, min–max) | 0.93 (0.48–0.99) | 0.93 (0.79–0.95) | 0.93 (0.48–0.99) | 0.516 |
| Urgent treatment, number of pediatric patients per institution, (median, min–max) | ||||
| Blood transfusion within 24 h | 1 (0–21) | 7 (1–21) | 1 (0–17) | <0.001 |
| Urgent transcatheter arterial embolization | 0 (0–12) | 2 (0–12) | 0 (0–10) | 0.004 |
| Craniotomy and/or craterization | 1 (0–15) | 6 (0–15) | 1 (0–11) | <0.001 |
| Thoracotomy | 0 (0–2) | 0 (0–2) | 0 (0–1) | 0.068 |
| Celiotomy | 0 (0–5) | 2 (0–5) | 0 (0–5) | <0.001 |
| Predicted mortality per institution, (median, min–max) | 6.74 (1.04–51.57) | 7.18 (4.67–20.89) | 6.62 (1.04–51.57) | 0.516 |
| Actual in-hospital mortality per institution, (median, min–max) | 0 (0–100) | 2.13 (0–8.33) | 0 (0–100) | 0.246 |
| SMR score range per institution, (median, min–max) | 0 (0–4.87) | 0.31 (0–0.79) | 0 (0–4.87) | 0.244 |
| Number of institutions stratified by SMR score range per institution, (frequency, %) | ||||
| 0.00–1.00 | 158 (90) | 13 (100) | 145 (89) | 0.206 |
| >1.00 | 18 (10) | 0 (0) | 18 (11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toida, C.; Muguruma, T.; Gakumazawa, M.; Shinohara, M.; Abe, T.; Takeuchi, I.; Morimura, N. Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study. J. Clin. Med. 2021, 10, 1422. https://doi.org/10.3390/jcm10071422
Toida C, Muguruma T, Gakumazawa M, Shinohara M, Abe T, Takeuchi I, Morimura N. Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study. Journal of Clinical Medicine. 2021; 10(7):1422. https://doi.org/10.3390/jcm10071422
Chicago/Turabian StyleToida, Chiaki, Takashi Muguruma, Masayasu Gakumazawa, Mafumi Shinohara, Takeru Abe, Ichiro Takeuchi, and Naoto Morimura. 2021. "Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study" Journal of Clinical Medicine 10, no. 7: 1422. https://doi.org/10.3390/jcm10071422
APA StyleToida, C., Muguruma, T., Gakumazawa, M., Shinohara, M., Abe, T., Takeuchi, I., & Morimura, N. (2021). Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study. Journal of Clinical Medicine, 10(7), 1422. https://doi.org/10.3390/jcm10071422






