Opiophobia in Emergency Department Healthcare Providers: A Survey in Western Switzerland
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Recruitment and Instrument
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
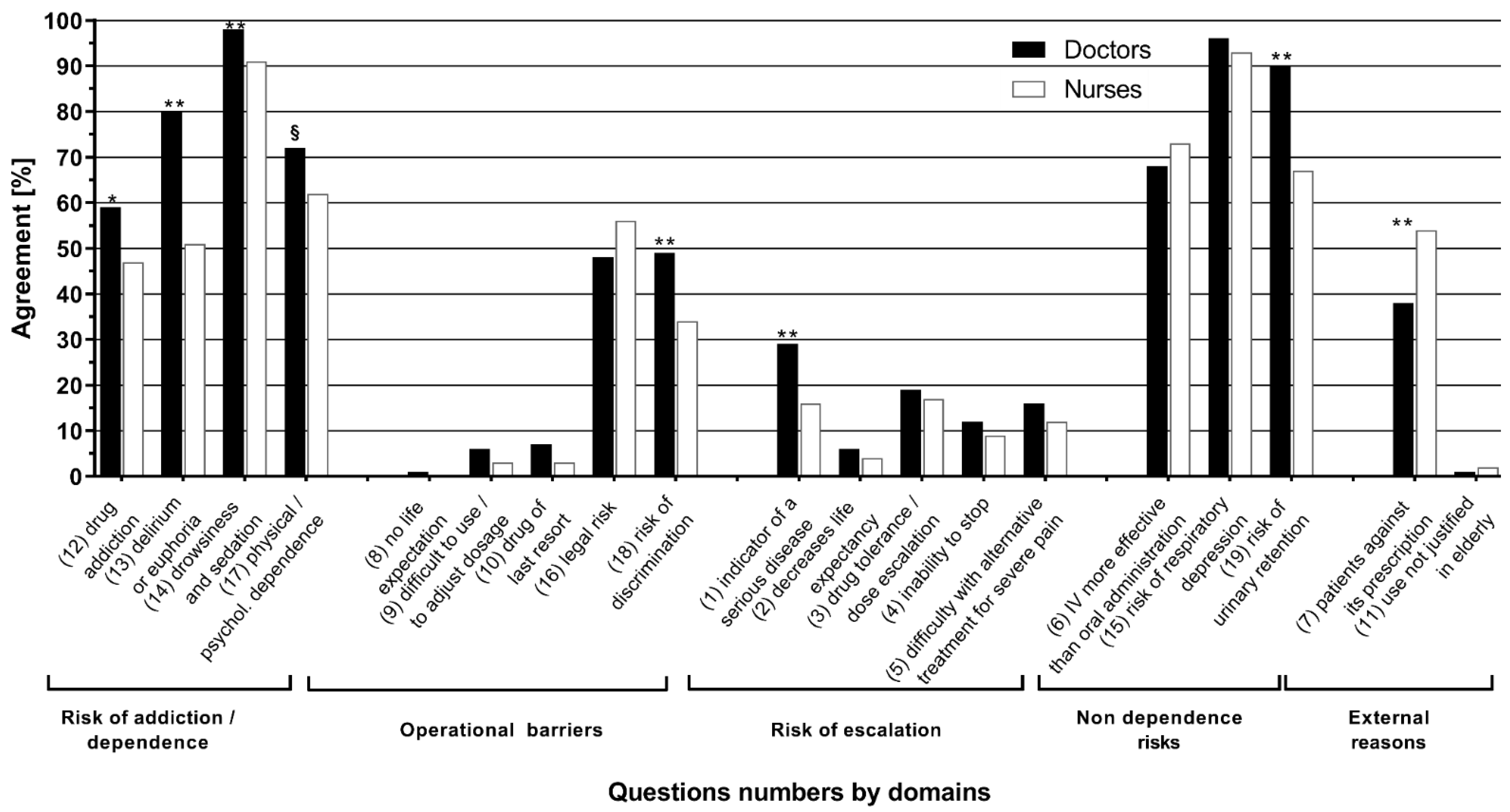
| Question N° | Components | |
|---|---|---|
| Risk of addiction/dependence | 20 | |
| 12 | Risk of drug addiction | |
| 13 | Risk of delirium or euphoria | |
| 14 | Risk of drowsiness and sedation | |
| 17 | Risk of physical and/or psychological dependence | |
| Maximal points: | ||
| Operational reasons for not using morphine | 25 | |
| 8 | The prescription of morphine means that there is no life expectation | |
| 9 | It is difficult to use and dose morphine | |
| 10 | Morphine is a drug of last resort | |
| 16 | Legal risk compared to other drugs | |
| 18 | Risk of discrimination | |
| Maximal points: | ||
| Risk of escalation | ||
| 1 | It means it is serious | |
| 2 | It decreases life expectancy | |
| 3 | The patient can get used to the drug quickly and one takes the risk of increasing the dose | |
| 4 | Once treatment is initiated, there is the risk of being unable to stop | |
| 5 | The early use of morphine makes it difficult to use any other treatment in severe pain | |
| Maximal points: | 25 | |
| Other (nondependence) risks | 15 | |
| 6 | IV administration is more effective than oral administration | |
| 15 | Risk of respiratory depression | |
| 19 | Risk of urinary retention | |
| Maximal points: | ||
| External (nonoperational) reasons for not using morphine | 10 | |
| 7 | The patients are against the prescription of morphine | |
| 11 | Sensation of pain decreases with age in the elderly, which does not justify its use | |
| Maximal points: | ||
| Total points: | 95 |
Appendix B
| Checklist Item | Explanation | Line Number | |
|---|---|---|---|
| Describe survey design | The target population was the emergency department (ED) nurses and doctors of nine teaching hospitals of French-speaking Switzerland and working in the ED at the time of the survey | 81–83 | |
| Ethics | Ethics approval | The study was exempted from formal review on June 28th 2016 by a decision of the Human Research Ethics Committee of the State of Vaud based on the Swiss Federal Act on Research involving Human Beings, because the survey was anonymous, voluntary, and without health–related data. | 77–79 |
| Informed consent | The welcome page presented briefly the goal of the study, that it would take approximately 15 min to complete, and that all responses were confidential and anonymous. Consent was indicated when respondents clicked on the ‘Go to Survey’ button from this page. | 107–108 | |
| Data protection | Data were collected using the online plateform SurveyMonkey®. No personal identifier was linked to survey results. The anonymous dataset was kept on password protected professional computers, behind an institutional firewall. | 102–103 | |
| Development and testing | The survey instrument used three validated questionnaires. The survey was extensively tested by the authors to ensure that no typing errors existed. | 84–98 | |
| Open survey versus closed survey | The survey was open and not password protected. | NA | |
| Contact mode | Head doctors of each ED emailed to every nurse or doctor an information letter inviting them to participate in the study and containing the internet link of the questionnaire and a unique personal identifier | 102–107 | |
| Advertising the survey | Head doctors of each ED emailed to every nurse or doctor an information letter inviting them to participate in the study and containing the internet link of the questionnaire and a unique personal identifier | 102–107 | |
| Web/E-mail | This was a web-based survey, available online on the platform SurveyMonkey® | 102 | |
| Context | The questionnaire was available online on the platform SurveyMonkey® | 102 | |
| Mandatory/voluntary | it was a voluntary survey | 102–108 | |
| Incentives | No incentives were offered | 109 | |
| Time/Date | Data were collected between September 2016 and April 2017 | 81–82 | |
| Randomization of items or questionnaires | Items in the questionnaires were not randomized nor alternated | Not mentioned in manuscript | |
| Adaptive questioning | Adaptive questioning was not used | Not mentioned in manuscript | |
| Number of Items | Our survey presented 3 questionnaires:
| 84–93 | |
| Number of screens (pages) | The full survey was distributed over 6 screens | Not mentioned in manuscript | |
| Completeness check | All survey items were mandatory. Completeness was checked after submission of each screen of the questionnaire had been submitted, and missing items were highlighted | Not mentioned in manuscript | |
| Review step | Respondents were able to change their responses once submitted through a Back button | Not mentioned in manuscript | |
| Unique site visitor | We did not determine unique visitors to ensure that respondents completed the survey only once | Not mentioned in manuscript | |
| View rate (Ratio of unique survey visitors/unique site visitors) | Not applicable | ||
| Participation rate (Ratio of unique visitors who agreed to participate/unique first survey page visitors) | Not applicable | ||
| Completion rate | The invitation to fill the questionnaire was sent to 916 healthcare providers (372 doctors and 544 nurses). In total, 511 surveys were completed online, with a response rate of 56%, having significant variation between centers: from 28% to 85% (p < 0.001). The rate was similar between doctors (57%) and nurses (52%) (p = 0.16) | 133–135 | |
| Cookies used | No | Not mentioned in manuscript | |
| IP check | No | Not mentioned in manuscript | |
| Log file analysis | No | Not mentioned in manuscript | |
| Registration | No | Not mentioned in manuscript | |
| Handling of incomplete questionnaires | All questionnaire, including those terminated early were analyzed | 129–130 | |
| Questionnaires submitted with an atypical timestamp | No respondents were removed from the survey | Not mentioned in manuscript | |
| Statistical correction | Not applied | Not mentioned in manuscript | |
References
- Gueant, S.; Taleb, A.; Borel-Kuhner, J.; Cauterman, M.; Raphael, M.; Nathan, G.; Ricard-Hibon, A. Quality of pain management in the emergency department: Results of a multicentre prospective study. Eur. J. Anaesthesiol. 2011, 28, 97–105. [Google Scholar] [CrossRef]
- Albrecht, E.; Taffe, P.; Yersin, B.; Schoettker, P.; Decosterd, I.; Hugli, O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: A 10 yr retrospective study. Br. J. Anaesth. 2013, 110, 96–106. [Google Scholar] [CrossRef]
- Schug, S.; Palmer, G.; Scott, D.; Halliwell, R.; Trinca, J. APM:SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine, 4th ed.; Acute Pain Management: Scientific Evidence; ANZCA & FPM: Melbourne, Australia, 2015; Volume 4. [Google Scholar]
- Decosterd, I.; Hugli, O.; Tamches, E.; Blanc, C.; Mouhsine, E.; Givel, J.C.; Yersin, B.; Buclin, T. Oligoanalgesia in the emergency department: Short-term beneficial effects of an education program on acute pain. Ann. Emerg. Med. 2007, 50, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Louriz, M.; Belayachi, J.; Madani, N.; Abidi, K.; Dendane, T.; Belabes Benchekroun, A.; Zeggwagh, A.A.; Abouqal, R. Practices and perceived barriers regarding pain management among Emergency Department physicians: A nationwide multicenter survey in Moroccan hospitals. Acute Med. Surg. 2016, 3, 360–363. [Google Scholar] [CrossRef]
- Morgan, J. American opiophobia: Customary underutilization of opioid analgesics. Adv. Alcohol Subst. Abus. 1985, 5, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Bennett, D.S.; Carr, D.B. Opiophobia as a barrier to the treatment of pain. J. Pain Palliat. Care Pharmacother. 2002, 16, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Covington, E. Opiophobia, Opiophilia, Opioagnosia. Pain Med. 2000, 1, 217–223. [Google Scholar] [CrossRef]
- Ferreira, M.; Verloo, H.; Vieira, M.; Marques-Vidal, P. Attitudes towards morphine use among nurses and physicians working in French-speaking Switzerland. Nurs. Res. Rev. 2013, 3, 141–153. [Google Scholar] [CrossRef][Green Version]
- Verloo, H.; Mpinga, E.K.; Ferreira, M.; Rapin, C.H.; Chastonay, P. Morphinofobia: The situation among the general population and health care professionals in North-Eastern Portugal. BMC Palliat. Care 2010, 9, 15. [Google Scholar] [CrossRef]
- Tamayo-Sarver, J.H.; Dawson, N.V.; Hinze, S.W.; Cydulka, R.K.; Wigton, R.S.; Albert, J.M.; Ibrahim, S.A.; Baker, D.W. The effect of race/ethnicity and desirable social characteristics on physicians’ decisions to prescribe opioid analgesics. Acad. Emerg. Med. 2003, 10, 1239–1248. [Google Scholar] [CrossRef]
- Heins, A.; Grammas, M.; Heins, J.K.; Costello, M.W.; Huang, K.; Mishra, S. Determinants of variation in analgesic and opioid prescribing practice in an emergency department. J. Opioid Manag. 2006, 2, 335–340. [Google Scholar] [CrossRef]
- Barnett, M.L.; Olenski, A.R.; Jena, A.B. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N. Engl. J. Med. 2017, 376, 663–673. [Google Scholar] [CrossRef]
- Cheng, F.J.; Wu, C.H.; Syue, Y.J.; Yen, P.C.; Wu, K.H. Association of physician risk tolerance with ED CT use for isolated dizziness/vertigo patients. Am. J. Emerg. Med. 2014, 32, 1284–1288. [Google Scholar] [CrossRef] [PubMed]
- Gerrity, M.; White, K.; DeVellis, R.; Dittus, R. Physicians’reaction to uncertainty: Refining the constructs and scales. Motiv. Emot. 1995, 19, 175–191. [Google Scholar] [CrossRef]
- Pearson, S.D.; Goldman, L.; Orav, E.J.; Guadagnoli, E.; Garcia, T.B.; Johnson, P.A.; Lee, T.H. Triage decisions for emergency department patients with chest pain: Do physicians’ risk attitudes make the difference? J. Gen. Intern. Med. 1995, 10, 557–564. [Google Scholar] [CrossRef]
- Vuille, M.; Foerster, M.; Foucault, E.; Hugli, O. Pain assessment by emergency nurses at triage in the emergency department: A qualitative study. J. Clin. Nurs. 2017, 127, 669–676. [Google Scholar] [CrossRef]
- Ferreira, M.; Verloo, H.; Mabire, C.; Vieira, M.M.; Marques-Vidal, P. Psychometric evaluation of the French version of the questionnaire attitudes towards morphine use; a cross-sectional study in Valais, Switzerland. BMC Nurs. 2014, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Bovier, P.A.; Perneger, T.V. Stress from uncertainty from graduation to retirement—A population-based study of Swiss physicians. J. Gen. Intern. Med. 2007, 22, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Royston, P.; Ambler, G.; Sauerbrei, W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int. J. Epidemiol. 1999, 28, 964–974. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar] [CrossRef]
- Hoppe, J.A.; Kim, H.; Heard, K. Association of emergency department opioid initiation with recurrent opioid use. Ann. Emerg. Med. 2015, 65, 493–499.e4. [Google Scholar] [CrossRef]
- Goldberg, D.S. On the erroneous conflation of opiophobia and the undertreatment of pain. Am. J. Bioeth. 2010, 10, 20–22. [Google Scholar] [CrossRef]
- Strayer, R.J.; Motov, S.M.; Nelson, L.S. Something for pain: Responsible opioid use in emergency medicine. Am. J. Emerg. Med. 2017, 35, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Berterame, S.; Erthal, J.; Thomas, J.; Fellner, S.; Vosse, B.; Clare, P.; Hao, W.; Johnson, D.T.; Mohar, A.; Pavadia, J.; et al. Use of and barriers to access to opioid analgesics: A worldwide, regional, and national study. Lancet 2016, 387, 1644–1656. [Google Scholar] [CrossRef]
- Verloo, H.; Cohen, C.; Borloz, C.; Kabengele, E.M.; Chastonay, P. Risks associated with the use of morphine for analgesia: Attitudes and perceptions amongst nursing students in French-speaking Switzerland. Nursing 2013, 3, 1–8. [Google Scholar] [CrossRef][Green Version]
- Patanwala, A.E.; Keim, S.M.; Erstad, B.L. Intravenous opioids for severe acute pain in the emergency department. Ann. Pharm. 2010, 44, 1800–1809. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Santucci, C.; Radrezza, S.; Erthal, J.; Berterame, S.; Corli, O. Trends in the consumption of opioids for the treatment of severe pain in Europe, 1990–2016. Eur. J. Pain 2019, 23, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Corradi-Dell’Acqua, C.; Foerster, M.; Sharvit, G.; Trueb, L.; Foucault, E.; Fournier, Y.; Vuilleumier, P.; Hugli, O. Pain management decisions in emergency hospitals are predicted by brain activity during empathy and error monitoring. Br. J. Anaesth. 2019, 123, e284–e292. [Google Scholar] [CrossRef]
- Endres, M.L.; Camp, R.; Milner, M. Is ambiguity tolerance malleable? Experimental evidence with potential implications for future research. Front. Psychol. 2015, 6, 619. [Google Scholar] [CrossRef] [PubMed]
| All * (N = 511) | Nurses (N = 283) | Doctors (N = 212) | p-Value | |
|---|---|---|---|---|
| Women, n (%) | 311 (63) | 203 (72) | 108 (51) | <0.001 |
| Median postgraduate experience: | ||||
| Total, years (IQR) π | 10 (4; 17) | 12 (7; 20) | 5.5 (2; 12) | <0.001 |
| In the ED, years (IQR) | 4 (1; 10) | 7 (3; 14) | 2 (1; 5) | <0.001 |
| Pain management training, n (%) | 104 (21) | 20 (7.1) | 84 (81) | <0.001 |
| Nationality | <0.001 | |||
| Swiss, n (%) | 260 (51) | 123 (43) | 137 (65) | |
| European, n (%) | 217 (42) | 152 (54) | 65 (31) | |
| Non European, n (%) | 14 (2.9) | 7 (2.5) | 8 (3.8) | |
| Missing, n (%) | 19 (3.7) | 1 (0.4) | 2 (0.9) | |
| Hospital, | <0.001 | |||
| University, n (%) | 167 (32) | 74 (26) | 88 (42) | |
| Non university, n (%) | 271 (53) | 169 (60) | 94 (44) | |
| unknown, n (%) | 73 (14) | 40 (14) | 30 (14) | |
| Mean scores | ||||
| ATMS ¶, points (SD **) | 44.7 (8.7) | 43.0 (8.5) | 46.5 (8.5) | <0.001 |
| SUS §, points (SD) | 22.6 (6.7) | 21.6 (6.4) | 23.9 (6.9) | <0.001 |
| RTS ¥, points (SD) | 14.1 (4.1) | 14.0 (4.1) | 14.1 (4.0) | 0.55 |
| ATMS, Points (SD) | Subscales Points (SD) | |||||
|---|---|---|---|---|---|---|
| Addiction/ Dependence | Operational | Escalation | Non-Dependence Risks | External Risks | ||
| Profession | ||||||
| Nurse | 43.0 (8.5) | 12.8 (3.8) | 8.0 (2.4) | 7.4 (2.9) | 11.1 (1.9) | 3.8 (1.2) |
| Doctor | 46.9 (8.5) | 14.8 (3.6) | 8.4 (2.6) | 8.4 (3.1) | 11.9 (2.3) | 3.5 (1.1) |
| p-value | <0.001 | <0.001 | 0.06 | 0.005 | <0.001 | <0.001 |
| Postgraduate experience * | ||||||
| 0–3 years | 49.4 (8.1) | 15.2 (3.3) | 9.2 (2.7) | 9.5 (3.4) | 11.7 (2.1) | 3.9 (1.2) |
| 4–7 years | 46.1 (8.2) | 14.0 (3.8) | 8.2 (2.2) | 8.3 (2.8) | 11.9 (1.9) | 3.7 (1.1) |
| 8–12 years | 44.2 (7.4) | 13.8 (3.4) | 7.8 (2.3) | 7.5 (3.0) | 11.5 (2.0) | 3.6 (1.0) |
| 13–19 years | 41.7 (9.1) | 12.8 (4.2) | 7.8 (2.5) | 6.7 (2.3) | 11.0 (2.5) | 3.5 (1.1) |
| 20–39 years | 41.2 (8.0) | 12.1 (3.7) | 7.5 (2.5) | 6.9 (2.6) | 10.8 (2.4) | 3.8 (1.3) |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | 0.099 |
| ED experience * | ||||||
| 0–4 years | 46.9 (8.4) | 14.5 (3.5) | 8.5 (2.5) | 8.5 (3.2) | 11.7 (2.0) | 3.7 (1.1) |
| >4 years | 42.2 (8.3) | 12.7 (3.9) | 7.7 (2.4) | 7.1 (2.7) | 11.1 (2.4) | 3.6 (1.1) |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | 0.006 | 0.37 |
| Origin | ||||||
| Switzerland | 43.7 (8.6) | 13.4 (3.8) | 7.9 (2.3) | 7.6 (2.9) | 11.2 (2.2) | 3.6 (1.1) |
| Europe | 45.5 (8.6) | 13.8 (3.8) | 8.3 (2.6) | 8.0 (3.0) | 11.6 (2.2) | 3.8 (1.2) |
| Extra-European | 49.3 (9.9) | 14.7 (4.7) | 9.7 (3.6) | 8.9 (3.8) | 11.8 (2.8) | 4.1 (1.1) |
| Unknown | 47.3 (10.4) | 14.8 (2.9) | 8.8 (3.0) | 7.0 (3.7) | 11.8 (1.7) | 4.3 (1.7) |
| p-value | 0.01 | 0.29 | 0.02 | 0.13 | 0.14 | 0.04 |
| Variables | Total | Addiction Risk | Operational | Escalation | Other Risks | Non Operational | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| * Coefficients (95% CI) | p | * Coefficients (95% CI) | p | * Coefficients (95% CI) | p | * Coefficients (95% CI) | p | * Coefficients (95% CI) | p | * Coefficients (95% CI) | p | |
| Intercept | 44.3 (40.1–48.1) | <0.001 | 15.4 (13.7–17.2) | <0.001 | 7.5 (6.3–8.7) | <0.001 | 8.1 (6.7–9.4) | <0.001 | 10.4 (9.3–11.4) | <0.001 | 2.9 (2.4–3.5) | <0.001 |
| Profession | ||||||||||||
| Doctor | Réf. | 0.004 | Réf. | <0.001 | Réf. | 0.83 | Réf. | 0.15 | Réf. | 0.01 | Réf. | <0.001 |
| Nurse | −2.4 (−4.0–−0.7) | −1.7 (−2.5–−1.0) | 0.5 (−0.4–0.5) | −0.4 (−1.0–0.2) | −0.8 (−1.2–−0.3) | 0.5 (0.2–0.7) | ||||||
| Postgraduate experience | ||||||||||||
| 0–3 years | Réf. | Réf. | Réf. | Réf. | Réf. | Réf. | ||||||
| 4–7 years | −2.5 (− 4.8–−0.3) | 0.03 | −0.8 (−1.8–0.25) | 0.14 | −0.9 (−1.6–−0.2) | 0.01 | −0.9 (−1.7–−0.1) | 0.03 | 0.3 (0.2–0.9) | 0.27 | −0.3 (−0.6–0.02) | 0.07 |
| 8–12 years | −4.3 (−6.6–−2.0) | <0.001 | −1.1 (−2.1–0.1) | 0.06 | −1.3 (−2.0–−0.6) | <0.001 | −1.7 (−2.5–−0.8) | <0.001 | 0.1 (−0.6–0.7) | 0.82 | −0.4 (−0.7–−0.1) | 0.02 |
| 13–19 years | −6.1 (−8.5–−3.7) | <0.001 | −1.8 (−2.9–−0.7) | 0.001 | −1.1 (−1.8–−0.3) | 0.005 | −2.4 (−3.3–−1.6) | <0.001 | −0.3 (−1.0–0.3) | 0.31 | −0.4 (−0.8–−0.1) | 0.01 |
| 20–39 years | −6.0 (−8.4–−3.6) | <0.001 | −2.1 (−3.2–−1.0) | <0.001 | −1.4 (−2.1–−0.6) | <0.001 | −2.0 (−2.9–−1.1) | <0.001 | −0.4 (−1.1–0.2) | 0.21 | −0.2 (−0.5–0.2) | 0.36 |
| Nationality | ||||||||||||
| Swiss | Réf. | Réf. | Réf. | Réf. | Réf. | Réf. | ||||||
| European | 2.5 (1.0–4.0) | 0.001 | 0.8 (0.1–3.0) | 0.03 | 0.3 (−0.1–0.8) | 0.15 | 0.7 (0.2–1.3) | 0.01 | 0.6 (0.2–1.0) | 0.006 | 0.1 (−0.1–0.3) | 0.49 |
| Non-European | 4.7 (0.6–8.8) | 0.02 | 1.1 (−0.8–3.0) | 0.27 | 1.7 (0.5–3.0) | 0.007 | 1.1 (−0.3–2.6) | 0.13 | 0.3 (−0.8–1.5) | 0.55 | 0.5 (−0.1–1.0) | 0.12 |
| Unknown | 17.5 (1.6–33.3) | 0.03 | 3.3 (−4.0–10.7) | 0.38 | 0.1 (−4.7–5.0) | 0.96 | 9.5 (3.9–15.1) | 0.001 | 1.7 (−2.6–6.0) | 0.44 | 2.9 (0.7–5.1) | 0.01 |
| SUS ¶ (for each additional point) | 0.24 (0.13–0.35) | <0.001 | 0.03 (−0.02–0.08) | 0.25 | 0.1 (0.04–0.11) | <0.001 | 0.06 (0.02–0.10) | 0.002 | 0.04 (0.01–0.07) | 0.013 | 0.04 (0.02–0.5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertrand, S.; Meynet, G.; Taffé, P.; Della Santa, V.; Fishman, D.; Fournier, Y.; Frochaux, V.; Ribordy, V.; Rutschmann, O.T.; Hugli, O. Opiophobia in Emergency Department Healthcare Providers: A Survey in Western Switzerland. J. Clin. Med. 2021, 10, 1353. https://doi.org/10.3390/jcm10071353
Bertrand S, Meynet G, Taffé P, Della Santa V, Fishman D, Fournier Y, Frochaux V, Ribordy V, Rutschmann OT, Hugli O. Opiophobia in Emergency Department Healthcare Providers: A Survey in Western Switzerland. Journal of Clinical Medicine. 2021; 10(7):1353. https://doi.org/10.3390/jcm10071353
Chicago/Turabian StyleBertrand, Sarah, Gabriel Meynet, Patrick Taffé, Vincent Della Santa, Daniel Fishman, Yvan Fournier, Vincent Frochaux, Vincent Ribordy, Olivier T. Rutschmann, and Olivier Hugli. 2021. "Opiophobia in Emergency Department Healthcare Providers: A Survey in Western Switzerland" Journal of Clinical Medicine 10, no. 7: 1353. https://doi.org/10.3390/jcm10071353
APA StyleBertrand, S., Meynet, G., Taffé, P., Della Santa, V., Fishman, D., Fournier, Y., Frochaux, V., Ribordy, V., Rutschmann, O. T., & Hugli, O. (2021). Opiophobia in Emergency Department Healthcare Providers: A Survey in Western Switzerland. Journal of Clinical Medicine, 10(7), 1353. https://doi.org/10.3390/jcm10071353






