Epigenetic Regulation of Mitochondrial Quality Control Genes in Multiple Myeloma: A Sequenom MassARRAY Pilot Investigation on HMCLs
Abstract
1. Introduction
2. Experimental Section
2.1. DNA Samples
2.2. Gene Expression Profiling (GEP)
2.3. Primer Design for EpiTYPER Assay
2.4. Bisulfite Treatment and PCR Conditions
2.5. Dephosphorylation of Unincorporated Deoxynucleoside Triphosphates, In Vitro Transcription and RNaseA Cleavage
2.6. Mass Spectrometry
2.7. Statistical Analyses
3. Results
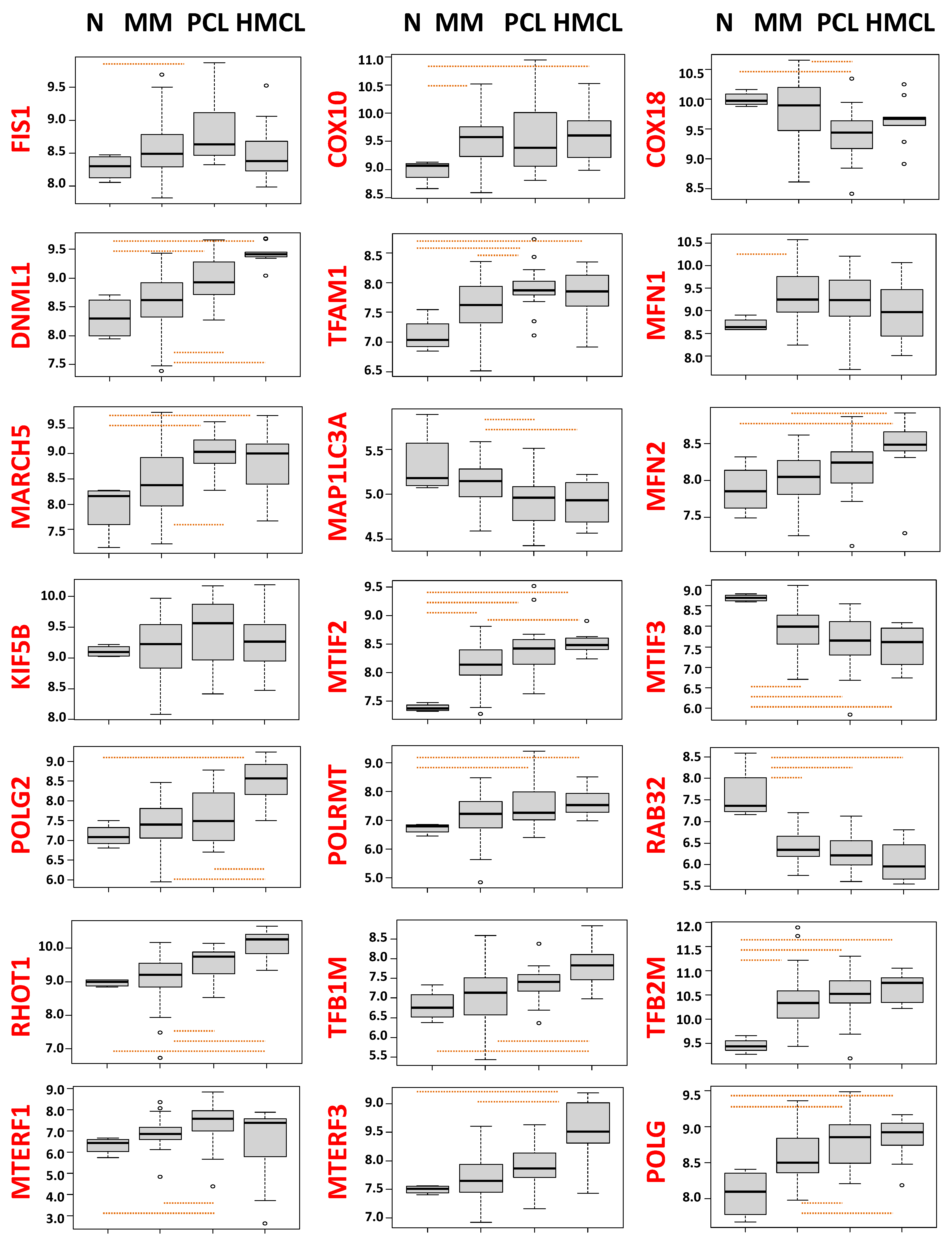
3.1. Dysregulated Expression of Mitochondrial Quality Control Genes in MM and Its More Advanced Stages
3.2. CpG methylation Analysis of Mitochondrial Quality Control Genes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Brigle, K.; Rogers, B. Pathobiology and Diagnosis of Multiple Myeloma. Semin. Oncol. Nurs. 2017, 33, 225–236. [Google Scholar] [CrossRef]
- Kazandjian, D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin. Oncol. 2016, 43, 676–681. [Google Scholar] [CrossRef]
- Korde, N.; Kristinsson, S.Y.; Landgren, O. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM): Novel biological insights and development of early treatment strategies. Blood 2011, 117, 5573–5581. [Google Scholar] [CrossRef] [PubMed]
- Landgren, O.; Kyle, R.A.; Pfeiffer, R.M.; Katzmann, J.A.; Caporaso, N.E.; Hayes, R.B.; Dispenzieri, A.; Kumar, S.; Clark, R.J.; Baris, D.; et al. Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: A prospective study. Blood 2009, 113, 5412–5417. [Google Scholar] [CrossRef] [PubMed]
- Alagpulinsa, D.A.; Szalat, R.E.; Poznansky, M.C.; Shmookler Reis, R.J. Genomic Instability in Multiple Myeloma. Trends Cancer 2020, 6, 858–873. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, O.; Baz, R. Multiple Myeloma Genomics—A Concise Review. Acta Med. Acad. 2019, 48, 57–67. [Google Scholar] [CrossRef]
- Manier, S.; Salem, K.Z.; Park, J.; Landau, D.A.; Getz, G.; Ghobrial, I.M. Genomic complexity of multiple myeloma and its clinical implications. Nat. Rev. Clin. Oncol. 2017, 14, 100–113. [Google Scholar] [CrossRef]
- Weaver, C.J.; Tariman, J.D. Multiple Myeloma Genomics: A Systematic Review. Semin. Oncol. Nurs. 2017, 33, 237–253. [Google Scholar] [CrossRef]
- Morelli, E.; Gulla, A.; Rocca, R.; Federico, C.; Raimondi, L.; Malvestiti, S.; Agosti, V.; Rossi, M.; Costa, G.; Giavaresi, G.; et al. The Non-Coding RNA Landscape of Plasma Cell Dyscrasias. Cancers 2020, 12, 320. [Google Scholar] [CrossRef]
- De Smedt, E.; Lui, H.; Maes, K.; De Veirman, K.; Menu, E.; Vanderkerken, K.; De Bruyne, E. The Epigenome in Multiple Myeloma: Impact on Tumor Cell Plasticity and Drug Response. Front. Oncol. 2018, 8, 566. [Google Scholar] [CrossRef]
- Amodio, N.; D’Aquila, P.; Passarino, G.; Tassone, P.; Bellizzi, D. Epigenetic modifications in multiple myeloma: Recent advances on the role of DNA and histone methylation. Expert Opin. Ther. Targets 2017, 21, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Fulciniti, M.; Amodio, N.; Cea, M.; Maiso, P.; Azab, A.K. Biological Insights into Myeloma and Other B Cell Malignancies. Biomed. Res. Int. 2016, 2016, 5218093. [Google Scholar] [CrossRef]
- Agirre, X.; Castellano, G.; Pascual, M.; Heath, S.; Kulis, M.; Segura, V.; Bergmann, A.; Esteve, A.; Merkel, A.; Raineri, E.; et al. Whole-epigenome analysis in multiple myeloma reveals DNA hypermethylation of B cell-specific enhancers. Genome Res. 2015, 25, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Abdi, J.; Qiu, L.; Chang, H. Micro-RNAs, New performers in multiple myeloma bone marrow microenvironment. Biomark. Res. 2014, 2, 10. [Google Scholar] [CrossRef]
- Popovic, R.; Martinez-Garcia, E.; Giannopoulou, E.G.; Zhang, Q.; Zhang, Q.; Ezponda, T.; Shah, M.Y.; Zheng, Y.; Will, C.M.; Small, E.C.; et al. Histone methyltransferase MMSET/NSD2 alters EZH2 binding and reprograms the myeloma epigenome through global and focal changes in H3K36 and H3K27 methylation. PLoS Genet. 2014, 10, e1004566. [Google Scholar] [CrossRef] [PubMed]
- Walker, B.A.; Wardell, C.P.; Chiecchio, L.; Smith, E.M.; Boyd, K.D.; Neri, A.; Davies, F.E.; Ross, F.M.; Morgan, G.J. Aberrant global methylation patterns affect the molecular pathogenesis and prognosis of multiple myeloma. Blood 2011, 117, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Raimondi, L.; De Luca, A.; Morelli, E.; Giavaresi, G.; Tagliaferri, P.; Tassone, P.; Amodio, N. MicroRNAs: Novel Crossroads between Myeloma Cells and the Bone Marrow Microenvironment. BioMed Res. Int. 2016, 2016, 6504593. [Google Scholar] [CrossRef]
- Pawlyn, C.; Kaiser, M.F.; Heuck, C.; Melchor, L.; Wardell, C.P.; Murison, A.; Chavan, S.S.; Johnson, D.C.; Begum, D.B.; Dahir, N.M.; et al. The Spectrum and Clinical Impact of Epigenetic Modifier Mutations in Myeloma. Clin. Cancer Res. 2016, 22, 5783–5794. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Shukla, S.K.; Gunda, V.; King, R.J.; Singh, P.K. Evaluating the Metabolic Alterations in Pancreatic Cancer. Methods Mol. Biol. 2019, 1882, 221–228. [Google Scholar] [CrossRef]
- Moro, L. Mitochondrial Dysfunction in Aging and Cancer. J. Clin. Med. 2019, 8, 1983. [Google Scholar] [CrossRef]
- Errichiello, E.; Venesio, T. Mitochondrial DNA variants in colorectal carcinogenesis: Drivers or passengers? J. Cancer Res. Clin. Oncol. 2017, 143, 1905–1914. [Google Scholar] [CrossRef]
- Yadav, N.; Chandra, D. Mitochondrial DNA mutations and breast tumorigenesis. Biochim. Biophys. Acta 2013, 1836, 336–344. [Google Scholar] [CrossRef]
- Amer, W.; Toth, C.; Vassella, E.; Meinrath, J.; Koitzsch, U.; Arens, A.; Huang, J.; Eischeid, H.; Adam, A.; Buettner, R.; et al. Evolution analysis of heterogeneous non-small cell lung carcinoma by ultra-deep sequencing of the mitochondrial genome. Sci. Rep. 2017, 7, 11069. [Google Scholar] [CrossRef]
- Hopkins, J.F.; Denroche, R.E.; Aguiar, J.A.; Notta, F.; Connor, A.A.; Wilson, J.M.; Stein, L.D.; Gallinger, S.; Boutros, P.C. Mutations in Mitochondrial DNA From Pancreatic Ductal Adenocarcinomas Associate With Survival Times of Patients and Accumulate as Tumors Progress. Gastroenterology 2018, 154, 1620–1624.e5. [Google Scholar] [CrossRef]
- Roth, K.G.; Mambetsariev, I.; Kulkarni, P.; Salgia, R. The Mitochondrion as an Emerging Therapeutic Target in Cancer. Trends Mol. Med. 2020, 26, 119–134. [Google Scholar] [CrossRef]
- Dai, W.; Jiang, L. Dysregulated Mitochondrial Dynamics and Metabolism in Obesity, Diabetes, and Cancer. Front. Endocrinol. (Lausanne) 2019, 10, 570. [Google Scholar] [CrossRef]
- Maycotte, P.; Marin-Hernandez, A.; Goyri-Aguirre, M.; Anaya-Ruiz, M.; Reyes-Leyva, J.; Cortes-Hernandez, P. Mitochondrial dynamics and cancer. Tumour Biol. 2017, 39, 1010428317698391. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Guha, M.; Kashina, A.; Avadhani, N.G. Mitochondrial dysfunction and mitochondrial dynamics-The cancer connection. Biochim. Biophys. Acta Bioenerg. 2017, 1858, 602–614. [Google Scholar] [CrossRef]
- Vyas, S.; Zaganjor, E.; Haigis, M.C. Mitochondria and Cancer. Cell 2016, 166, 555–566. [Google Scholar] [CrossRef]
- Senft, D.; Ronai, Z.A. Regulators of mitochondrial dynamics in cancer. Curr. Opin. Cell Biol. 2016, 39, 43–52. [Google Scholar] [CrossRef]
- Rehman, J.; Zhang, H.J.; Toth, P.T.; Zhang, Y.; Marsboom, G.; Hong, Z.; Salgia, R.; Husain, A.N.; Wietholt, C.; Archer, S.L. Inhibition of mitochondrial fission prevents cell cycle progression in lung cancer. FASEB J 2012, 26, 2175–2186. [Google Scholar] [CrossRef]
- Mancias, J.D.; Kimmelman, A.C. Mechanisms of Selective Autophagy in Normal Physiology and Cancer. J. Mol. Biol. 2016, 428, 1659–1680. [Google Scholar] [CrossRef]
- Song, I.S.; Kim, H.K.; Lee, S.R.; Jeong, S.H.; Kim, N.; Ko, K.S.; Rhee, B.D.; Han, J. Mitochondrial modulation decreases the bortezomib-resistance in multiple myeloma cells. Int. J. Cancer 2013, 133, 1357–1367. [Google Scholar] [CrossRef]
- Zhan, X.; Yu, W.; Franqui-Machin, R.; Bates, M.L.; Nadiminti, K.; Cao, H.; Amendt, B.A.; Jethava, Y.; Frech, I.; Zhan, F.; et al. Alteration of mitochondrial biogenesis promotes disease progression in multiple myeloma. Oncotarget 2017, 8, 111213–111224. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Ambrosini, S.; Luscher, T.; Paneni, F.; Costantino, S. Epigenetic Control of Mitochondrial Function in the Vasculature. Front. Cardiovasc. Med. 2020, 7, 28. [Google Scholar] [CrossRef]
- D’Aquila, P.; Montesanto, A.; De Rango, F.; Guarasci, F.; Passarino, G.; Bellizzi, D. Epigenetic signature: Implications for mitochondrial quality control in human aging. Aging (Albany NY) 2019, 11, 1240–1251. [Google Scholar] [CrossRef]
- Mohammad, H.P.; Barbash, O.; Creasy, C.L. Targeting epigenetic modifications in cancer therapy: Erasing the roadmap to cancer. Nat. Med. 2019, 25, 403–418. [Google Scholar] [CrossRef]
- Uittenbogaard, M.; Brantner, C.A.; Chiaramello, A. Epigenetic modifiers promote mitochondrial biogenesis and oxidative metabolism leading to enhanced differentiation of neuroprogenitor cells. Cell Death Dis. 2018, 9, 360. [Google Scholar] [CrossRef]
- Fulciniti, M.; Amodio, N.; Bandi, R.L.; Cagnetta, A.; Samur, M.K.; Acharya, C.; Prabhala, R.; D’Aquila, P.; Bellizzi, D.; Passarino, G.; et al. miR-23b/SP1/c-myc forms a feed-forward loop supporting multiple myeloma cell growth. Blood Cancer J. 2016, 6, e380. [Google Scholar] [CrossRef]
- Ronchetti, D.; Agnelli, L.; Pietrelli, A.; Todoerti, K.; Manzoni, M.; Taiana, E.; Neri, A. A compendium of long non-coding RNAs transcriptional fingerprint in multiple myeloma. Sci. Rep. 2018, 8, 6557. [Google Scholar] [CrossRef]
- Barfield, R.T.; Kilaru, V.; Smith, A.K.; Conneely, K.N. CpGassoc: An R function for analysis of DNA methylation microarray data. Bioinformatics 2012, 28, 1280–1281. [Google Scholar] [CrossRef]
- Missiroli, S.; Genovese, I.; Perrone, M.; Vezzani, B.; Vitto, V.A.M.; Giorgi, C. The Role of Mitochondria in Inflammation: From Cancer to Neurodegenerative Disorders. J. Clin. Med. 2020, 9, 740. [Google Scholar] [CrossRef]
- Barbato, A.; Scandura, G.; Puglisi, F.; Cambria, D.; La Spina, E.; Palumbo, G.A.; Lazzarino, G.; Tibullo, D.; Di Raimondo, F.; Giallongo, C.; et al. Mitochondrial Bioenergetics at the Onset of Drug Resistance in Hematological Malignancies: An Overview. Front. Oncol. 2020, 10, 604143. [Google Scholar] [CrossRef]
- O’Sullivan, E.; Goggins, M. DNA methylation analysis in human cancer. Methods Mol. Biol. 2013, 980, 131–156. [Google Scholar] [CrossRef]
| MM1s | KMS11 | Normal Control Cells | MM1s vs. Normal Control Cells | KMS11 vs. Normal Control Cells | |||
|---|---|---|---|---|---|---|---|
| Gene | p-Value | FDR | p-Value | FDR | |||
| COX10 | 0.353 (0.003) | 0.331 (0.009) | 0.528 (0.014) | 3.57 × 10−6 | 1.67 × 10−5 | 2.91 × 10−6 | 1.36 × 10−5 |
| COX18 | 0.054 (0.003) | 0.058 (0.006) | 0.068 (0.007) | 0.134 | 0.250 | 0.406 | 0.421 |
| DNM1L | 0.071 (0.002) | 0.056 (0.002) | 0.065 (0.003) | 0.796 | 0.872 | 0.101 | 0.129 |
| FIS1 | 0.091 (0.014) | 0.104 (0.007) | 0.082 (0.009) | 0.766 | 0.872 | 0.188 | 0.229 |
| KIF5B | 0.043 (0.006) | 0.056 (0.003) | 0.044 (0.003) | 0.473 | 0.698 | 0.055 | 0.077 |
| MAP1LC3A | 0.760 (0.007) | 0.836 (0.005) | 0.262 (0.009) | 8.45 × 10−16 | 7.89 × 10−15 | 6.67 × 10−14 | 9.34 × 10−13 |
| MARCH5 | 0.068 (0.003) | 0.081 (0.006) | 0.057 (0.002) | 0.052 | 0.120 | 8.09 × 10−4 | 0.002 |
| MFN1 | 0.090 (0.014) | 0.105 (0.009) | 0.052 (0.003) | 0.003 | 0.008 | 2.22 × 10−5 | 7.76 × 10−5 |
| MFN2 | 0.064 (0.004) | 0.075 (0.007) | 0.057 (0.004) | 0.177 | 0.292 | 0.029 | 0.046 |
| MTERF | 0.058 (0.009) | 0.159 (0.008) | 0.043 (0.005) | 0.939 | 0.939 | 1.24 × 10−8 | 6.93 × 10−8 |
| MTERFD1 | 0.091 (0.004) | 0.086 (0.009) | 0.056 (0.003) | 1.29 × 10−6 | 7.24 × 10−6 | 0.001 | 0.002 |
| MTIF2 | 0.053 (0.01) | 0.057 (0.004) | 0.039 (0.009) | 0.143 | 0.250 | 0.213 | 0.249 |
| MTIF3 | 0.064 (0.008) | 0.074 (0.008) | 0.049 (0.002) | 0.029 | 0.075 | 0.002 | 0.003 |
| POLG1 | 0.492 (0.014) | 0.525 (0.003) | 0.510 (0.008) | 0.133 | 0.250 | 0.235 | 0.254 |
| POLG2 | 0.060 (0.002) | 0.070 (0.009) | 0.036 (0.003) | 4.14 × 10−5 | 1.45 × 10−4 | 9.26 × 10−4 | 0.002 |
| POLRMT | 0.066 (0.002) | 0.060 (0.005) | 0.027 (0.005) | 9.73 × 10−6 | 3.89 × 10−5 | 0.003 | 0.005 |
| RAB32 | 0.358 (0.003) | 0.596 (0.015) | 0.079 (0.006) | 3.15 × 10−19 | 8.8 × 10−18 | 5.21 × 10−14 | 9.34 × 10−13 |
| RHOT1 | 0.042 (0.003) | 0.048 (0.007) | 0.037 (0.002) | 0.809 | 0.872 | 0.082 | 0.109 |
| TFAM | 0.065 (0.004) | 0.076 (0.003) | 0.047 (0.003) | 0.894 | 0.927 | 1.37x10−4 | 4.27 × 10−4 |
| TFB1M | 0.103 (0.002) | 0.168 (0.008) | 0.088 (0.006) | 0.653 | 0.831 | 1.29x10−5 | 5.15 × 10−0.5 |
| TFB2M | 0.090 (0.010) | 0.077 (0.009) | 0.074 (0.009) | 0.556 | 0.779 | 0.850 | 0.850 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Aquila, P.; Ronchetti, D.; Gallo Cantafio, M.E.; Todoerti, K.; Taiana, E.; Fabiani, F.; Montesanto, A.; Neri, A.; Passarino, G.; Viglietto, G.; et al. Epigenetic Regulation of Mitochondrial Quality Control Genes in Multiple Myeloma: A Sequenom MassARRAY Pilot Investigation on HMCLs. J. Clin. Med. 2021, 10, 1295. https://doi.org/10.3390/jcm10061295
D’Aquila P, Ronchetti D, Gallo Cantafio ME, Todoerti K, Taiana E, Fabiani F, Montesanto A, Neri A, Passarino G, Viglietto G, et al. Epigenetic Regulation of Mitochondrial Quality Control Genes in Multiple Myeloma: A Sequenom MassARRAY Pilot Investigation on HMCLs. Journal of Clinical Medicine. 2021; 10(6):1295. https://doi.org/10.3390/jcm10061295
Chicago/Turabian StyleD’Aquila, Patrizia, Domenica Ronchetti, Maria Eugenia Gallo Cantafio, Katia Todoerti, Elisa Taiana, Fernanda Fabiani, Alberto Montesanto, Antonino Neri, Giuseppe Passarino, Giuseppe Viglietto, and et al. 2021. "Epigenetic Regulation of Mitochondrial Quality Control Genes in Multiple Myeloma: A Sequenom MassARRAY Pilot Investigation on HMCLs" Journal of Clinical Medicine 10, no. 6: 1295. https://doi.org/10.3390/jcm10061295
APA StyleD’Aquila, P., Ronchetti, D., Gallo Cantafio, M. E., Todoerti, K., Taiana, E., Fabiani, F., Montesanto, A., Neri, A., Passarino, G., Viglietto, G., Bellizzi, D., & Amodio, N. (2021). Epigenetic Regulation of Mitochondrial Quality Control Genes in Multiple Myeloma: A Sequenom MassARRAY Pilot Investigation on HMCLs. Journal of Clinical Medicine, 10(6), 1295. https://doi.org/10.3390/jcm10061295









