An Evaluation of Medication Prescribing Patterns for Acute Migraine in the Emergency Department: A Scoping Review
Abstract
1. Introduction
- What classes of medication were most frequently prescribed for the acute treatment of acute migraine in the ED?
- What are the rates at which narcotic and migraine specific medications are prescribed in the ED?
- What factors influenced preferred treatment of migraine in the ED?
- What factors precluded adherence to evidence-based migraine guidelines?
- How can migraine treatment in ED be more consistent with current evidence-based guidelines?
2. Experimental Section
2.1. Eligibility Criteria
2.1.1. Types of Participants
2.1.2. Concept
2.1.3. Types of Study
2.2. Methods
- A search of MEDLINE, Cochrane, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) was conducted, followed by an analysis of words contained in the title and abstract, as well as index terms used to describe relevant articles.
- All identified keywords and index terms were used to conduct a second search using the following databases: Ovid MEDLINE, Cochrane Library/Systematic Reviews, PubMed, CINAHL, PsycINFO and Excerpta Medica database (EMBASE).
- A manual search as conducted to ensure all relevant studies were included.
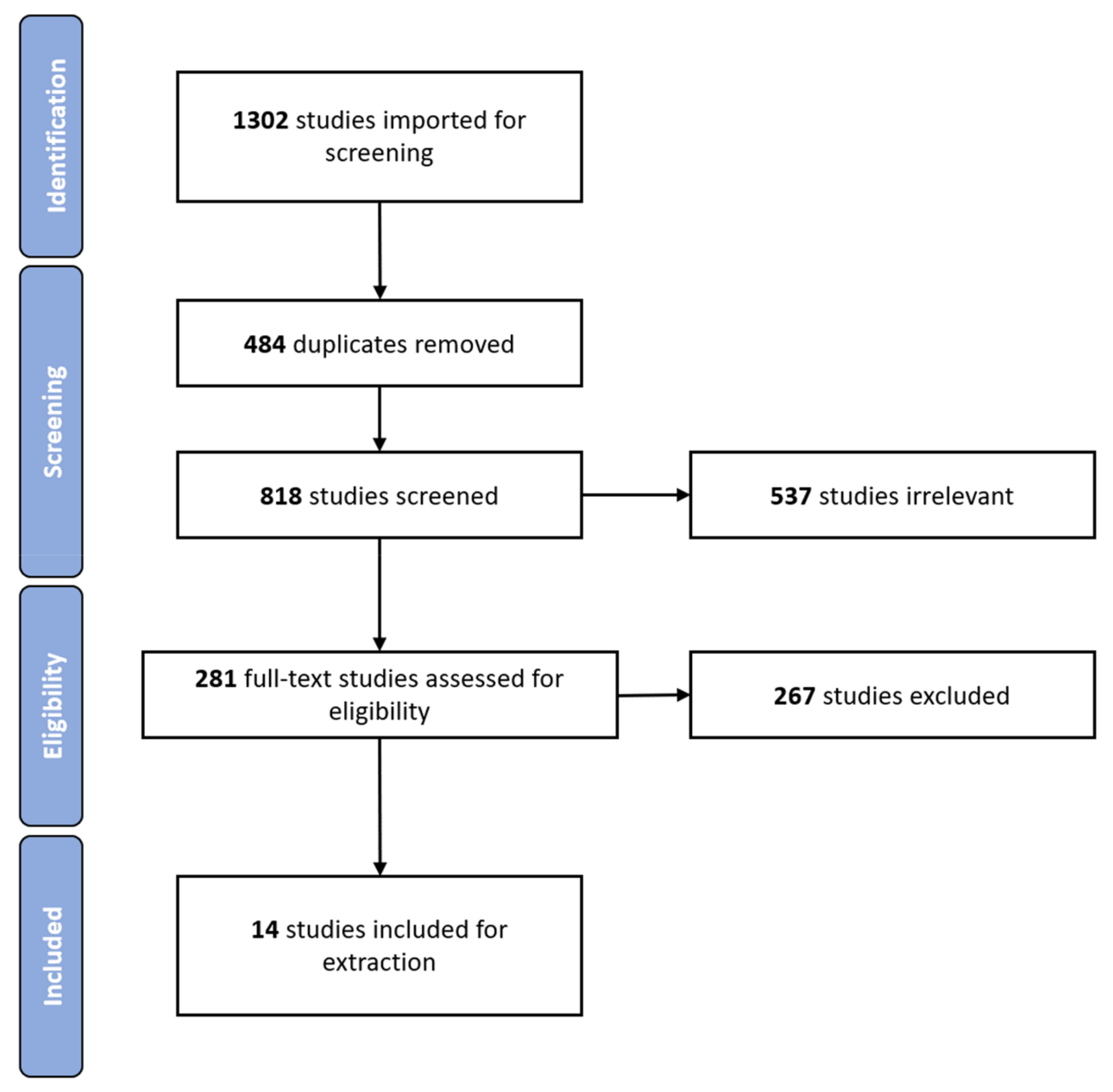
2.3. Screening and Data Extraction
3. Results
| Author, Year | Country and Setting | Main Aim of the Study | Study Type | Study Size | Age (Mean Years, Unless Stated Otherwise) | Gender | Migraine Population and Definition | Medication |
| Gunasekera, 2020 [17] | Australia: St Vincent’s Hospital, Melbourne | To determine whether the emergency department (ED) prescribed medications were consistent with national guidelines. | Retrospective cohort study | 744 patients | 36.4 | M 25%, F 75% |
| Opioids and generalized prescribing patterns |
| Minen, 2020 [18] | United States: 2 urgent care locations, New York | To examine the treatment and management of migraine patients admitted in the ED, focusing on discrepancies between prescribed therapies and the American Headache Society (AHS) migraine management guidelines. | Retrospective chart review | 78 patients | 32.5 | M 20.5%, F 79.5% |
| Generalized prescribing patterns |
| Shao, 2020 [19] | United States: Baylor Scott & White Health services, Texas | To describe the use of opioid and non-opioid medication in patients admitted to ED with migraine and compare demographics between opioid users and non-opioid users in the same group. | Retrospective study using electronic health records |
| 44.5 | M 14.1%, F 85.9% |
| Opioids and generalized prescribing patterns. |
| Ruzek, 2019 [20] | United states: 4 suburban EDs, New Jersey | To determine how migraine treatment in the ED has changed between the years 1999–2000 and 2014, with a secondary goal of ascertaining if there was a change in the return rate to ED in 72 h over the years. | Retrospective cohort study |
| Chart review: 38 72-h return group: 38 | M 11%, F 89% (chart review) M 16%, F 84% (72-h return group) | Migraine diagnosis based on an ED physician diagnosis of migraine coded with the respective ICD-9 code | Generalized prescribing patterns |
| Shao, 2017 [1] | Australia: A large metropolitan ED, Queensland | To identify the varying demographics of patients which presented to the ED with a migraine and analyze the trends in medication treatments and prescriptions for the migraine. | Retrospective study of clinical records | 2228 patients | Migraine patients: 37.05ED population: 46.17 | M 29%, F 71% | Migraine diagnosis required both
| Generalized prescribing patterns. |
| Young, 2017 [21] | United states: 3 emergency departments, Connecticut | To explore and describe treatment habits in three different settings: an academic medical center, a non-academic urban ED, and a community ED | Retrospective cross-sectional analysis of consecutive adult emergency visits |
| 36 (Median) | M 17.3%, F 82.7% | Migraine diagnosis based on ICD-9 code for migraine or one of tis variations ICD-9 code 346 or 346 | Opioids and generalized prescribing patterns |
| Berberian, 2016 [22] | United States: An academic emergency department, Pennsylvania | To determine the frequency with which parenteral narcotic analgesia is used to treat acute migraine in an academic ED and to compare the cost and length of stay between patients treated with narcotic vs. non-narcotic treatments | Retrospective cohort study |
| Not stated | Not stated | Migraine diagnosis based on both chief complaint and ICD-9 codes for Migraine taken from electronic records | Opioids prescribing patterns |
| Cheng, 2016 [23] | Australia: 2 metropolitan hospital EDs, Melbourne | To analyze the demographics, presentation, management, and outcomes of patients who presented to the ED with a migraine, making a comparison between first presenters and those with a history of migraine. | Retrospective cohort study | 356 patients | 37.8 | M 25.2%, F 74.8% | Migraine diagnosis defined by fulfilling
| Generalized prescribing patterns |
| Friedman, 2015 [7] | United states: Randomly selected EDs, multiple sites across the US | To make a comparison between the frequency of current medications given to patients with acute migraines in EDs within the United States (US) with those used in 1998. The authors also aimed to identify factors related to the use of opioids | Retrospective study using 2010 data from the Hospital Ambulatory Medical Care Survey (NHAMCS) |
| Not stated | Not stated | Patients with a ICD-9 coded discharge diagnosis of migraine | Generalized prescribing patterns |
| Supapol, 2013 [24] | Canada: 12 emergency departments, Ontario | To evaluate the prevalence of opioid therapy as a primary treatment for migraine headache in 12 Ontario EDs by randomly selecting 100 migraine patient charts | Retrospective study | 100 randomly selected patient charts | not stated | Not stated | Migraine diagnosis defined though clinical charts with a National Ambulatory Care Reporting System (NACRS) most responsible diagnosis (MRDX) coding of migraine | Opioid prevalence |
| Valade, 2011 [25] | France: 20 general emergency departments, multiple sites across France | To determine the proportion of headache patients diagnosed with migraine, and to ascertain demographic and clinical characteristics of these patients and describe the treatment and follow-up they received. | Prospective observational study |
| 37.6 | M 25.5%, F 74.5% | Migraine diagnosis based on a questionnaire completed by an ed physician containing:
| General prescribing patterns |
| Tornabene, 2009 [26] | United States: 2 emergency departments, California | To examine and compare the treatment type and throughput times of migraine patients between an urban and suburban ED, and between patients that visited the ED multiple times (repeaters) vs. only once (non-repeaters). | Retrospective review of patient records |
| Repeaters: 40.9 Non-repeaters: 39.5 | Repeaters: M 36.2%, F 63.8% Non-repeater: M 24.2%, F 75.8% | Based on 2 criteria:
| Opioids versus non-opioid prescribing patterns |
| Wasay, 2006 [27] | Pakistan: An emergency department, Karachi | To discern whether Internation Headache Society (IHS) guidelines were being met within a tertiary care hospital ED in Pakistan. | Retrospective cohort study | 161 patients | 34 | M 36%, F 64% | Migraine diagnosis based on the IHSC criteria | Opioids versus non-opioid prescribing patterns |
| Freidman, 2009 [28] | United States: 2 Emergency departments, New York | To determine the proportion of migraine patients presenting to ED who were treated with migraine-specific therapy as well as to note the amount of unnecessary neuroimaging studies performed. | Retrospective cohort study | 156 patients | Not stated | M 19.8%, F 80.2% | Migraine diagnosis based on patients with the ICD-9 codes 346.0, 346.1, or 346.9 and a primary diagnosis of migraine | Migraine specific versus non migraine specific therapy |
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Shao, E.; Hughes, J.; Eley, R. The presenting and prescribing patterns of migraine in an Australian emergency department: A descriptive exploratory study. World J. Emerg. Med. 2017, 8, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Group, Global Burden of Disease Neurological Disorders Collaboration. Global, regional, and national burden of neurological disorders during 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017, 16, 877–897. [Google Scholar] [CrossRef]
- Report, Deloitte Access Economics. Migraine in Australia Whitepaper; Deloitte: London, UK, 2018; p. 38. [Google Scholar]
- Gustavsson, A.; Svensson, M.; Jacobi, F.; Allgulander, C.; Alonso, J.; Beghi, E.; Dodel, R.; Ekman, M.; Faravelli, C.; Fratiglioni, L.; et al. Cost of disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 718–779. [Google Scholar] [CrossRef]
- Olesen, J.; Gustavsson, A.; Svensson, M.; Wittchen, H.U.; Jonsson, B.; CDBE2010 study group; European Brain Council. The economic cost of brain disorders in Europe. Eur. J. Neurol. 2012, 19, 155–162. [Google Scholar] [CrossRef]
- Hawkins, K.; Wang, S.; Rupnow, M.F. Indirect cost burden of migraine in the United States. J. Occup. Environ. Med. 2007, 49, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; West, J.; Vinson, D.R.; Minen, M.T.; Restivo, A.; Gallagher, E.J. Current management of migraine in US emergency departments: An analysis of the National Hospital Ambulatory Medical Care Survey. Cephalalgia 2015, 35, 301–309. [Google Scholar] [CrossRef]
- Schappert, S.M.; Rechtsteiner, E.A. Ambulatory medical care utilization estimates for 2006. In National Health Statistics Reports; CDC: Atlanta, GA, USA, 2008; pp. 1–29. [Google Scholar]
- Diamond, M.; Cady, R. Initiating and optimizing acute therapy for migraine: The role of patient-centered stratified care. Am. J. Med. 2005, 118 (Suppl. 1), 18S–27S. [Google Scholar] [CrossRef]
- Orr, S.L.; Friedman, B.W.; Christie, S.; Minen, M.T.; Bamford, C.; Kelley, N.E.; Tepper, D. Management of Adults With Acute Migraine in the Emergency Department: The American Headache Society Evidence Assessment of Parenteral Pharmacotherapies. Headache 2016, 56, 911–940. [Google Scholar] [CrossRef] [PubMed]
- Marmura, M.J.; Silberstein, S.D.; Schwedt, T.J. The acute treatment of migraine in adults: The american headache society evidence assessment of migraine pharmacotherapies. Headache 2015, 55, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Langer-Gould, A.M.; Anderson, W.E.; Armstrong, M.J.; Cohen, A.B.; Eccher, M.A.; Iverson, D.J.; Potrebic, S.B.; Becker, A.; Larson, R.; Gedan, A.; et al. The American Academy of Neurology’s top five choosing wisely recommendations. Neurology 2013, 81, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Gelfand, A.A.; Goadsby, P.J. A Neurologist’s Guide to Acute Migraine Therapy in the Emergency Room. Neurohospitalist 2012, 2, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Bigal, M.E.; Serrano, D.; Buse, D.; Scher, A.; Stewart, W.F.; Lipton, R.B. Acute migraine medications and evolution from episodic to chronic migraine: A longitudinal population-based study. Headache 2008, 48, 1157–1168. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Khalil, H.; Peters, M.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Parker, D. An Evidence-Based Approach to Scoping Reviews. Worldviews Evid. Based. Nurs. 2016, 13, 118–123. [Google Scholar] [CrossRef]
- Gunasekera, L.; Akhlaghi, H.; Sun-Edelstein, C.; Heywood, J.; Sanders, L. Overuse of opioids for acute migraine in an Australian emergency department. Emerg. Med. Australas. 2020, 32, 763–768. [Google Scholar] [CrossRef]
- Minen, M.T.; Zhou, K.; Miller, L. A Brief Look at Urgent Care Visits for Migraine: The Care Received and Ideas to Guide Migraine Care in this Proliferating Medical Setting. Headache 2020, 60, 542–552. [Google Scholar] [CrossRef]
- Shao, Q.; Rascati, K.L.; Lawson, K.A.; Wilson, J.P. Patterns and predictors of opioid use among migraine patients at emergency departments: A retrospective database analysis. Cephalalgia 2020, 40, 1489–1501. [Google Scholar] [CrossRef] [PubMed]
- Ruzek, M.; Richman, P.; Eskin, B.; Allegra, J.R. ED treatment of migraine patients has changed. Am. J. Emerg. Med. 2019, 37, 1069–1072. [Google Scholar] [CrossRef]
- Young, N.; Silverman, D.; Bradford, H.; Finkelstein, J. Multicenter prevalence of opioid medication use as abortive therapy in the ED treatment of migraine headaches. Am. J. Emerg. Med. 2017, 35, 1845–1849. [Google Scholar] [CrossRef]
- Berberian, J.; Fischer, M. The utilization of narcotic analgesia in the treatment of migraine headaches. Acad. Emerg. Med. 2016, 23, S162–S163. [Google Scholar]
- Cheng, C.T.; Law, G.T.W.M.; Roman, C.; Tan, G.; Mitra, B. Evaluation of the assessment and management of acute migraines in two Australian metropolitan emergency departments. J. Emerg. Med. Trauma Acute Care 2016, 2016, 10. [Google Scholar] [CrossRef]
- Supapol, W.; Ackerman, M.; Worster, A. Assessing emergency department quality of migraine care in an Ontario Local Health Integrated Network. Can. J. Emerg. Med. 2013, 15 (Suppl. 1). [Google Scholar]
- Valade, D.; Lucas, C.; Calvel, L.; Plaisance, P.; Derouet, N.; Meric, G.; Lanteri-Minet, M.; Giroud, M. Migraine diagnosis and management in general emergency departments in France. Cephalalgia 2011, 31, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Tornabene, S.V.; Deutsch, R.; Davis, D.P.; Chan, T.C.; Vilke, G.M. Evaluating the use and timing of opioids for the treatment of migraine headaches in the emergency department. J. Emerg. Med. 2009, 36, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Wasay, M.; Zaki, K.S.; Khan, S.U.; Rehmani, R. Narcotic analgesics for acute migraine in the emergency room: Are we meeting Headache Societies’ guidelines? J. Headache Pain 2006, 7, 413–415. [Google Scholar] [CrossRef][Green Version]
- Friedman, D.; Feldon, S.; Holloway, R.; Fisher, S. Utilization, diagnosis, treatment and cost of migraine treatment in the emergency department. Headache 2009, 49, 1163–1173. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.; West, J. Lack of evolution of Emergency Department treatment of migraine. J. Pain 2014, 15, S10. [Google Scholar] [CrossRef]
- Peretz, A.; Dujari, S.; Cowan, R.; Minen, M. ACEP Guidelines on Acute Nontraumatic Headache Diagnosis and Management in the Emergency Department, Commentary on Behalf of the Refractory, Inpatient, Emergency Care Section of the American Headache Society. Headache 2020, 60, 643–646. [Google Scholar] [CrossRef]
- Kelly, A.M.; Knott, J.; Bennetts, S.; Huckson, S.; Management, N.I.f.C.S.N.E.C.P. Treatment of migraine in Australian Emergency Departments. Emerg. Med. Australas. 2009, 21, 333–334. [Google Scholar] [CrossRef]
- Lipton, R.B.; Bigal, M.E.; Diamond, M.; Freitag, F.; Reed, M.L.; Stewart, W.F.; Group, A.A. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007, 68, 343–349. [Google Scholar] [CrossRef]
- Antonaci, F.; Sances, G.; Guaschino, E.; De Cillis, I.; Bono, G.; Nappi, G. Meeting patient expectations in migraine treatment: What are the key endpoints? J. Headache Pain 2008, 9, 207–213. [Google Scholar] [CrossRef]
- Reuter, U. GBD 2016: Still no improvement in the burden of migraine. Lancet Neurol. 2018, 17, 929–930. [Google Scholar] [CrossRef]
- Karimi, L.; Crewther, S.G.; Wijeratne, T.; Evans, A.E.; Afshari, L.; Khalil, H. The Prevalence of Migraine with Anxiety among Genders. Front. Neurol. 2020, 11, 569405. [Google Scholar] [CrossRef] [PubMed]
- Pringsheim, T.; Becker, W.J. Triptans for symptomatic treatment of migraine headache. BMJ 2014, 348, g2285. [Google Scholar] [CrossRef] [PubMed]
- Wijeratne, T.; Grisold, W.; Dodick, D.; Carroll, W. World Brain Day 2019: Migraine, the painful truth. Lancet Neurol. 2019, 18, 914. [Google Scholar] [CrossRef]
| Author | Key Findings | Additional Observations |
| Gunasekera, 2020 [17] |
|
|
| Minen, 2020 [18] |
|
|
| Shao, 2020 [19] |
| After controlling for covariates, several predictors of index date opioid use were found this included:
|
| Ruzek, 2019 [20] |
|
|
| Shao, 2017 [1] |
|
|
| Young, 2017 [21] |
|
|
| Berberian, 2016 [22] |
|
|
| Cheng, 2016 [23] |
|
|
| Friedman, 2015 [7] |
|
|
| Supapol, 2013 [24] |
|
|
| Valade, 2011 [25] |
|
|
| Tornabene, 2009 [26] |
|
|
| Wasay, 2006[27] |
|
|
| Freidman,2009 [28] |
| The cost of radiological investigations was a major contributing factor to the overall financial burden of emergency care for migraine patients. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, J.H.; Karimi, L.; Wijeratne, T. An Evaluation of Medication Prescribing Patterns for Acute Migraine in the Emergency Department: A Scoping Review. J. Clin. Med. 2021, 10, 1191. https://doi.org/10.3390/jcm10061191
Lim JH, Karimi L, Wijeratne T. An Evaluation of Medication Prescribing Patterns for Acute Migraine in the Emergency Department: A Scoping Review. Journal of Clinical Medicine. 2021; 10(6):1191. https://doi.org/10.3390/jcm10061191
Chicago/Turabian StyleLim, Jun Hua, Leila Karimi, and Tissa Wijeratne. 2021. "An Evaluation of Medication Prescribing Patterns for Acute Migraine in the Emergency Department: A Scoping Review" Journal of Clinical Medicine 10, no. 6: 1191. https://doi.org/10.3390/jcm10061191
APA StyleLim, J. H., Karimi, L., & Wijeratne, T. (2021). An Evaluation of Medication Prescribing Patterns for Acute Migraine in the Emergency Department: A Scoping Review. Journal of Clinical Medicine, 10(6), 1191. https://doi.org/10.3390/jcm10061191








