Pregnancy Outcomes and Maternal Insulin Sensitivity: Design and Rationale of a Multi-Center Longitudinal Study in Mother and Offspring (PROMIS)
Abstract
1. Introduction
2. Materials and Methods
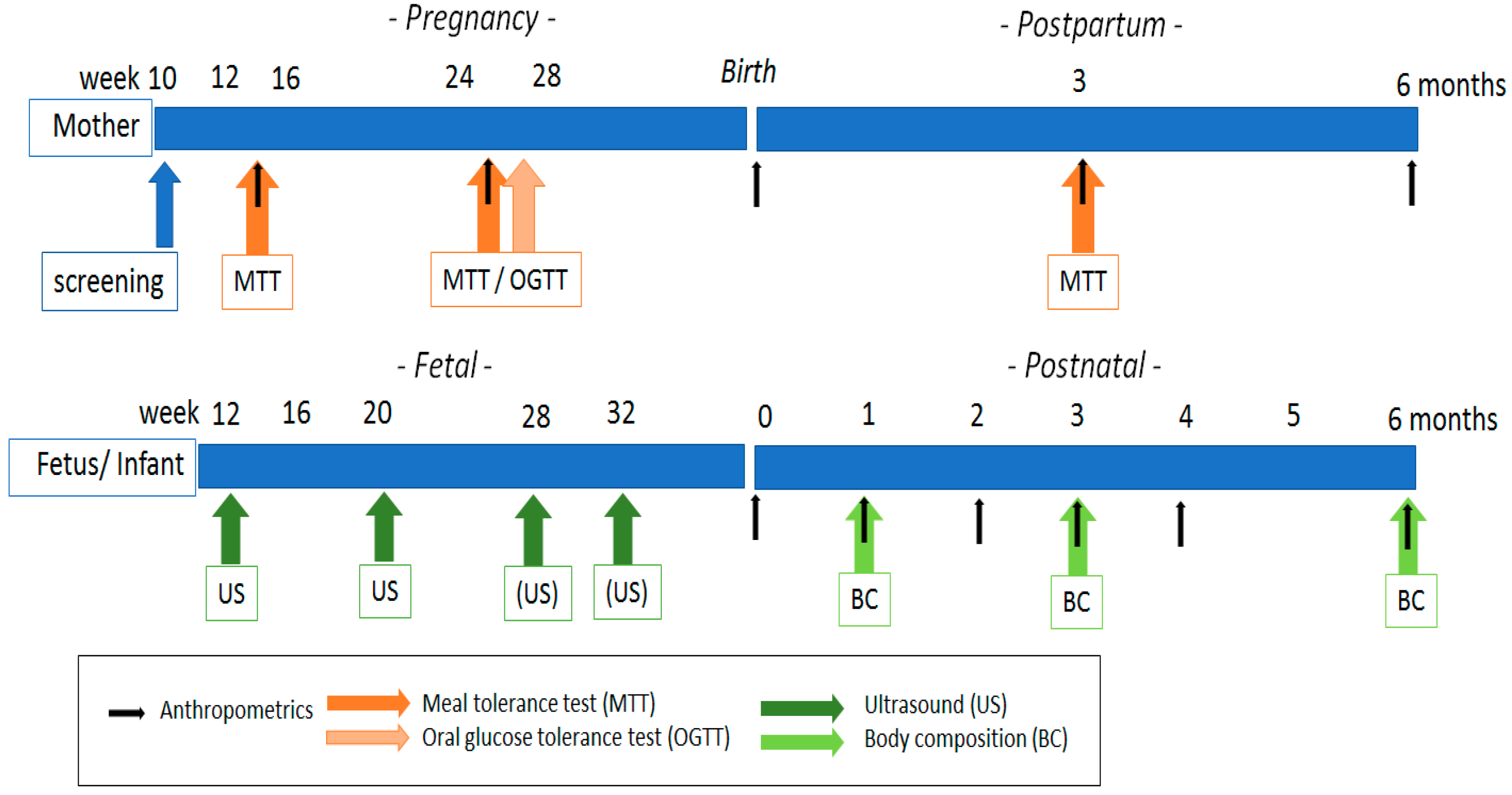
2.1. Overall Study Design
2.2. In-and Exclusion Criteria
2.3. Recruitment
2.4. Meal Tolerance and Oral Glucose Tolerance Testing
2.5. Sample Size Calculation
2.6. Interim Analysis
2.7. Data Collection
2.7.1. Maternal Measurements
2.7.2. Fetal Measurements
2.7.3. Neonatal and Infant Measurements
2.7.4. Diet and Behavioral Data
2.7.5. Other Outcomes
2.8. Statistical Analysis
2.9. Database
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sonagra, A.D.; Biradar, S.M.; Dattatreya, K.; Murthy, D.S.J. Normal pregnancy—A state of insulin resistance. J. Clin. Diagn. Res. 2014, 8, CC01–CC03. [Google Scholar] [CrossRef]
- Marcinkevage, J.A.; Narayan, K.V. Gestational diabetes mellitus: Taking it to heart. Prim. Care Diabetes 2011, 5, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Devlieger, R.; Casteels, K.; Van Assche, F.A. Reduced adaptation of the pancreatic B cells during pregnancy is the major causal factor for gestational diabetes: Current knowledge and metabolic effects on the offspring. Acta Obstet. Gynecol. Scand. 2008, 87, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Bellmann, O.; Hartmann, E. Influence of pregnancy on the kinetics of insulin. Am. J. Obstet. Gynecol. 1975, 122, 829–833. [Google Scholar] [CrossRef]
- Baeyens, L.; Hindi, S.; Sorenson, R.L.; German, M.S. β-Cell adaptation in pregnancy. Diabetes Obes. Metab. 2016, 18, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Rieck, S.; Kaestner, K.H. Expansion of β-cell mass in response to pregnancy. Trends Endocrinol. Metab. 2010, 21, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.A.; Ehrenberg, H. The short-and long-term implications of maternal obesity on the mother and her offspring. BJOG Int. J. Obstet. Gynaecol. 2006, 113, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Xu, X.; Yan, Y. Estimated global overweight and obesity burden in pregnant women based on panel data model. PLoS ONE 2018, 13, e0202183. [Google Scholar] [CrossRef]
- Lengte en gewicht van personen, ondergewicht en overgewicht; vanaf 1981. Available online: https://www.cbs.nl/nl-nl/cijfers/detail/81565NED?dl=35805 (assessed on 23 February 2021).
- HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N. Engl. J. Med. 2008, 358, 1991–2002. [Google Scholar] [CrossRef]
- Seshiah, V.; Cynthia, A.; Balaji, V.; Balaji, M.S.; Ashalata, S.; Sheela, R.; Thamizharasia, M.; Arthia, T. Detection and care of women with gestational diabetes mellitus from early weeks of pregnancy results in birth weight of newborn babies appropriate for gestational age. Diabetes Res. Clin. Pract. 2008, 80, 199–202. [Google Scholar] [CrossRef]
- Phillips, P.J. Oral glucose tolerance testing. Aust. Fam. Physician 2012, 41, 391. [Google Scholar] [PubMed]
- Ko, G.T.; Chan, J.C.; Woo, J.; Lau, E.; Yeung, V.T.; Chow, C.; Cockram, C.S. The reproducibility and usefulness of the oral glucose tolerance test in screening for diabetes and other cardiovascular risk factors. Ann. Clin. Biochem. 1998, 35, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Benhalima, K.; Van Crombrugge, P.; Moyson, C.; Verhaeghe, J.; Vandeginste, S.; Verlaenen, H.; Vercammen, C.; Maes, T.; Dufraimont, E.; De Block, C.; et al. Characteristics and pregnancy outcomes across gestational diabetes mellitus subtypes based on insulin resistance. Diabetologia 2019, 62, 2118–2128. [Google Scholar] [CrossRef] [PubMed]
- Cobelli, C.; Dalla Man, C.; Sparacino, G.; Magni, L.; De Nicolao, G.; Kovatchev, B.P. Diabetes: Models, signals, and control. IEEE Rev. Biomed. Eng. 2009, 2, 54–96. [Google Scholar] [CrossRef]
- van Dijk, T.H.; Boer, T.S.; Havinga, R.; Stellaard, F.; Kuipers, F.; Reijngoud, D. Quantification of hepatic carbohydrate metabolism in conscious mice using serial blood and urine spots. Anal. Biochem. 2003, 322, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cosmed the metabolic company. PEAPOD, the world’s gold standard for non-invasive Infant body composition assessment. Available online: https://www.cosmed.com/en/products/body-composition/pea-pod (assessed on 23 February 2021).
- DIABETES MELLITUS EN ZWANGERSCHAP versie 3.0. de Otterlo werkgroep en Cie Kwaliteitsdocumenten NVOG. 2018. Available online: https://www.nvog.nl (assessed on 23 February 2021).
- Muscogiuri, G.; Sarno, G.; Gastaldelli, A.; Savastano, S.; Ascione, A.; Colao, A.; Orio, F. The good and bad effects of statins on insulin sensitivity and secretion. Endocr. Res. 2014, 39, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.M. Obesity, insulin resistance, and pregnancy outcome. Reproduction 2010, 140, 365–371. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, M.; Prins, S.M.; de Valk, H.W.; Evers, I.M.; Visser, G.H.A.; Mol, B.J.M. Stand van zaken Diabetes gravidarum. Behandeling vermindert kans op complicaties. Ned. Tijdschr. Geneeskd. 2011, 155, A2291. [Google Scholar]
- van Leeuwen, M.; Louwerse, M.; Opmeer, B.; Limpens, J.; Serlie, M.; Reitsma, J.; Mol, B.W.J. Glucose challenge test for detecting gestational diabetes mellitus: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 393–401. [Google Scholar] [CrossRef]
- Flahault, A.; Cadilhac, M.; Thomas, G. Sample size calculation should be performed for design accuracy in diagnostic test studies. J. Clin. Epidemiol. 2005, 58, 859–862. [Google Scholar] [CrossRef]
- Research Electronic Data Capture (REDCap). Available online: https://redcap.vanderbilt.edu (assessed on 23 February 2021).
- Harpenden Skinfold Caliper. Available online: http://www.harpenden-skinfold.com/measurements.html (assessed on 23 February 2021).
- Marshall, N.E.; Murphy, E.J.; King, J.C.; Haas, E.K.; Lim, J.Y.; Wiedrick, J.; Thornburg, K.L.; Purnell, J.Q. Comparison of multiple methods to measure maternal fat mass in late gestation, 2. Am. J. Clin. Nutr. 2016, 103, 1055–1063. [Google Scholar] [CrossRef]
- Durnin, J.; Rahaman, M.M. The assessment of the amount of fat in the human body from measurements of skinfold thickness. Br. J. Nutr. 1967, 21, 681–689. [Google Scholar] [CrossRef]
- Villar, J.; Ismail, L.C.; Victora, C.G.; O Ohuma, E.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; A Jaffer, Y.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Methods and Development: Head Circumference-for-Age, Arm Circumference-for-Age, Triceps Skinfold-for-Age and Subscapular Skinfold-for-Age; World Health Organization: Geneva, Switzerland, 2007.
- Molag, M. Towards Transparent Development of Food Frequency Questionnaires: Scientific Basis of the Dutch FFQ-TOOL tm: A Computer System to Generate, Apply and Process FFQs. Ph.D. Thesis, Wageningen University, Wageningen, The Netherland, 2010. [Google Scholar]
- Hunot, C.; Fildes, A.; Croker, H.; Llewellyn, C.H.; Wardle, J.; Beeken, R.J. Appetitive traits and relationships with BMI in adults: Development of the Adult Eating Behaviour Questionnaire. Appetite 2016, 105, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Rabin, R.; Charro, F.D. EQ-SD: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Chasan-taber, L.; Schmidt, M.D.; Roberts, D.E.; Hosmer, D.; Markenson, G.; Freedson, P.S. Development and validation of a pregnancy physical activity questionnaire. Med. Sci. Sports Exerc. 2004, 36, 1750–1760. [Google Scholar] [CrossRef]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Llewellyn, C.H.; van Jaarsveld, C.H.; Johnson, L.; Carnell, S.; Wardle, J. Development and factor structure of the Baby Eating Behaviour Questionnaire in the Gemini birth cohort. Appetite 2011, 57, 388–396. [Google Scholar] [CrossRef]
- World Health Organization. Global Report on Diabetes. 2016; WHO: Geneva, Switzerland, 2017.
- Maegawa, Y.; Sugiyama, T.; Kusaka, H.; Mitao, M.; Toyoda, N. Screening tests for gestational diabetes in Japan in the 1st and 2nd trimester of pregnancy. Diabetes Res. Clin. Pract. 2003, 62, 47–53. [Google Scholar] [CrossRef]
- Rijkelijkhuizen, J.M.; Girman, C.J.; Mari, A.; Alssema, M.; Rhodes, T.; Nijpels, G.; Kostense, P.J.; Stein, P.P.; Eekhoff, E.M.; Heine, R.J.; et al. Classical and model-based estimates of beta-cell function during a mixed meal vs. an OGTT in a population-based cohort. Diabetes Res. Clin. Pract. 2009, 83, 280–288. [Google Scholar] [CrossRef]
| Screening | Week 12–16 | Week 20 | Week 24–26 | Week 28 | Week 32 | Week 36 | Birth | |
|---|---|---|---|---|---|---|---|---|
| Visit number | Visit 1 | Visit 2 | Routine 1 | Visits 3 and 4 | Visit 5 | Visit 6 | Phone call | Routine 2 |
| Visit window | ≤12 weeks | ±1 week | ±2 weeks | ±1 week | ±1 week | ±1 week | ±1 week | +2 weeks |
| Informed consent | X | |||||||
| Inclusion/exclusion criteria | X | |||||||
| Baseline and demographics | X | |||||||
| Maternal anthropometrics | X | X | X | X | ||||
| Fasting or random blood glucose | X | |||||||
| Blood parameters (for MTT) | X | X | ||||||
| Blood parameters (for OGTT) | X | |||||||
| Maternal skinfolds and fundal height | X | X | ||||||
| Fetal sonography | X | X | X | |||||
| FFQ | X | X | ||||||
| PPAQ | X | X | X | |||||
| Sensory questionnaire | X | |||||||
| EQ-5D | X | X | X | |||||
| AEBQ | X | X | ||||||
| Birth outcomes | X | |||||||
| Neonatal adiposity and anthropometrics | X | |||||||
| Intake drugs, alcohol, smoking | X | X | ||||||
| Maternal complications | X | X | X | X | X | |||
| Neonatal complications | X |
| 1 Month Postpartum | 2 Months Postpartum | 3 Months Postpartum | 4 Months Postpartum | 6 Months Postpartum | |
|---|---|---|---|---|---|
| Visit number | Visit 7 | Routine 1 | Visit 8 | Routine 1 | Visit 9 |
| Visit window (days) | ±1 week | ±3 days | ±1 week | ±3 days | ±1 week |
| Maternal anthropometrics | X | X | |||
| Blood parameters MTT | X | ||||
| Skinfolds | X | X | |||
| Food Frequency Questionnaire | X | X | X | ||
| IPAQ | X | X | |||
| EQ-D5 | X | X | X | ||
| AEBQ | X | X | X | ||
| BEBQ | X | X | X | ||
| Infant adiposity and anthropometrics | X | X | X | X | X |
| Peapod/skinfolds | X | X | X | ||
| Maternal complications | X | X | X | X | X |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kdekian, A.; Sietzema, M.; Scherjon, S.A.; Lutgers, H.; van der Beek, E.M. Pregnancy Outcomes and Maternal Insulin Sensitivity: Design and Rationale of a Multi-Center Longitudinal Study in Mother and Offspring (PROMIS). J. Clin. Med. 2021, 10, 976. https://doi.org/10.3390/jcm10050976
Kdekian A, Sietzema M, Scherjon SA, Lutgers H, van der Beek EM. Pregnancy Outcomes and Maternal Insulin Sensitivity: Design and Rationale of a Multi-Center Longitudinal Study in Mother and Offspring (PROMIS). Journal of Clinical Medicine. 2021; 10(5):976. https://doi.org/10.3390/jcm10050976
Chicago/Turabian StyleKdekian, Anoush, Maaike Sietzema, Sicco A. Scherjon, Helen Lutgers, and Eline M. van der Beek. 2021. "Pregnancy Outcomes and Maternal Insulin Sensitivity: Design and Rationale of a Multi-Center Longitudinal Study in Mother and Offspring (PROMIS)" Journal of Clinical Medicine 10, no. 5: 976. https://doi.org/10.3390/jcm10050976
APA StyleKdekian, A., Sietzema, M., Scherjon, S. A., Lutgers, H., & van der Beek, E. M. (2021). Pregnancy Outcomes and Maternal Insulin Sensitivity: Design and Rationale of a Multi-Center Longitudinal Study in Mother and Offspring (PROMIS). Journal of Clinical Medicine, 10(5), 976. https://doi.org/10.3390/jcm10050976





