Multiple Allergen Simultaneous Test-Immunoblot Assay for Immunoglobulin E Detection in Patients with Isolated Allergic Conjunctivitis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
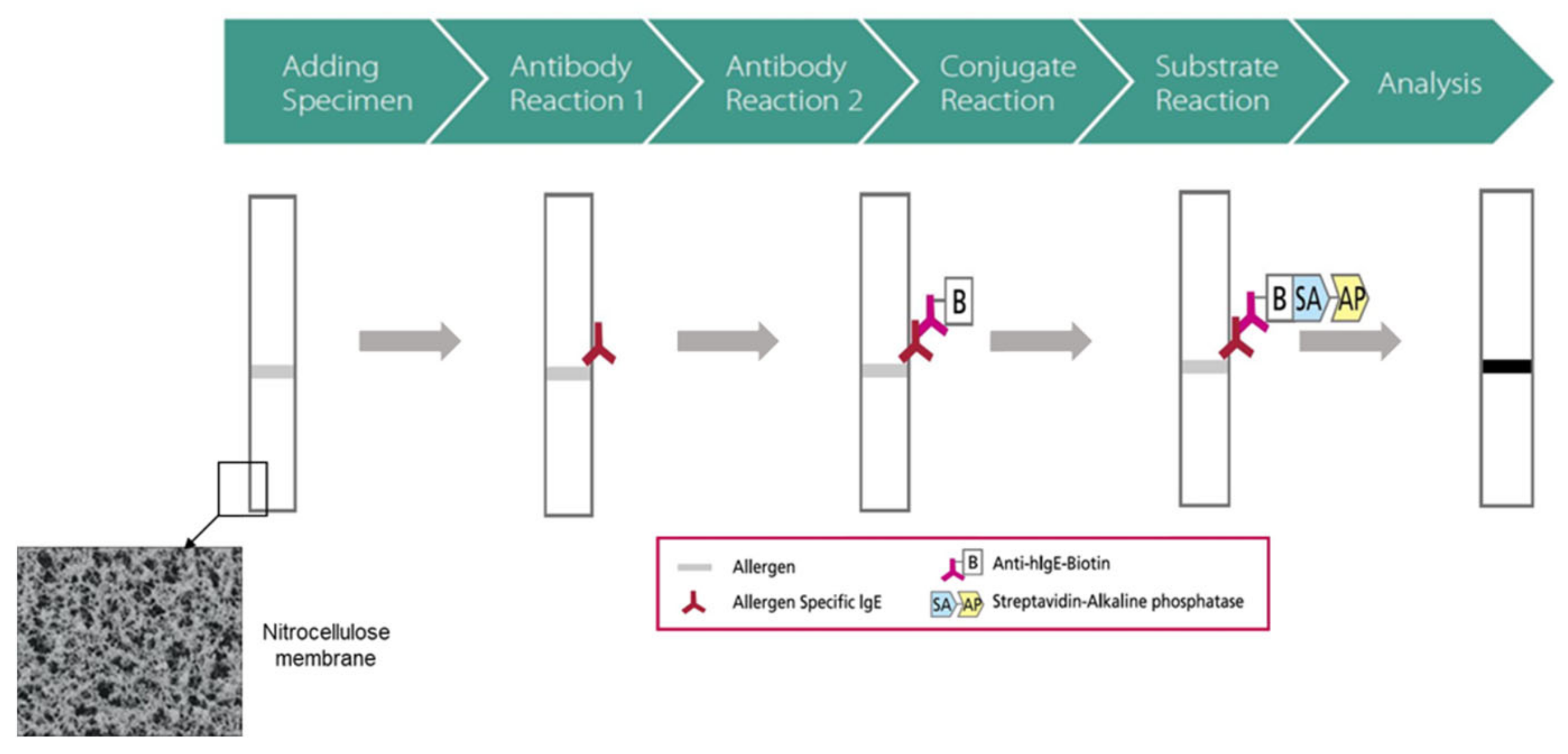
2.2. MAST-Immunoblot Assay
2.3. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. MAST-Immunoblot Assay (Overall)
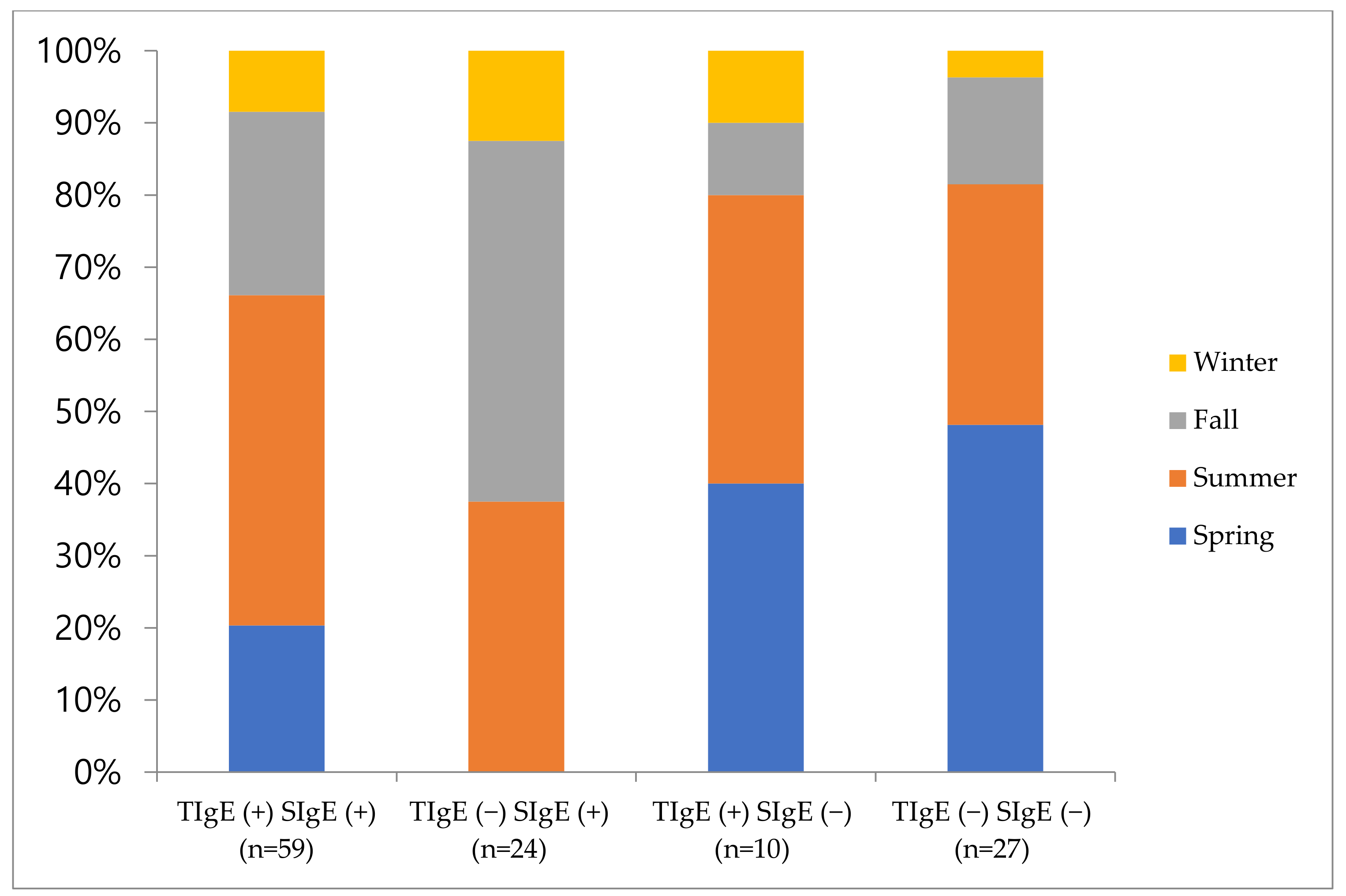
3.3. Subgroup Analysis of MAST-Immunoblot Assay
3.4. Effect of Sex and Age on MAST-Immunoblot Assay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, A.W. A practical guide to anaphylaxis. Am. Fam. Physician 2003, 68, 1325–1332. [Google Scholar] [PubMed]
- Petricek, I.; Prost, M.; Popova, A. The differential diagnosis of red eye: A survey of medical practitioners from eastern europe and the middle east. Ophthalmologica 2006, 220, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Bielory, L. Allergic conjunctivitis and the impact of allergic rhinitis. Curr. Allergy Asthma Rep. 2010, 10, 122–134. [Google Scholar] [CrossRef]
- Pitt, A.D.; Smith, A.F.; Lindsell, L.; Voon, L.W.; Rose, P.W.; Bron, A.J. Economic and quality-of-life impact of seasonal allergic conjunctivitis in oxfordshire. Ophthalmic Epidemiol. 2004, 11, 17–33. [Google Scholar] [CrossRef]
- Platt, M.P.; Wulu, J.A. Rational Approach to Allergy Testing. Otolaryngol. Clin. N. Am. 2017, 50, 1103–1110. [Google Scholar] [CrossRef]
- Leonardi, A.; De Dominicis, C.; Motterle, L. Immunopathogenesis of ocular allergy: A schematic approach to different clinical entities. Curr. Opin. Allergy Clin. Immunol. 2007, 7, 429–435. [Google Scholar] [CrossRef]
- Leonardi, A.; Borghesan, F.; Faggian, D.; Depaoli, M.; Secchi, A.G.; Plebani, M. Tear and serum soluble leukocyte activation markers in conjunctival allergic diseases. Am. J. Ophthalmol. 2000, 129, 151–158. [Google Scholar] [CrossRef]
- Sampath, V.; Tupa, D.; Graham, M.T.; Chatila, T.A.; Spergel, J.M.; Nadeau, K.C. Deciphering the black box of food allergy mechanisms. Ann. Allergy Asthma Immunol. 2017, 118, 21–27. [Google Scholar] [CrossRef]
- Kim, Y.H.; Yu, B.J.; Kim, W.J.; Kim, J.E.; Lee, G.H.; Lee, K.A.; Cho, J.H. Correlation between skin prick test and mast-immunoblot results in patients with chronic rhinitis. Asian Pac. J. Allergy Immunol. 2013, 31, 20–25. [Google Scholar]
- Park, K.H.; Lee, J.; Sim, D.W.; Lee, S.C. Comparison of Singleplex Specific IgE Detection Immunoassays: ImmunoCAP Phadia 250 and Immulite 2000 3gAllergy. Ann. Lab. Med. 2018, 38, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Simons, F.E.; Johnston, L.; Gu, X.; Simons, K.J. Suppression of the early and late cutaneous allergic responses using fexofenadine and montelukast. Ann. Allergy Asthma Immunol. 2001, 86, 44–50. [Google Scholar] [CrossRef]
- Gradman, J.; Wolthers, O.D. Suppressive effects of topical mometasone furoate and tacrolimus on skin prick testing in children. Pediatr. Dermatol. 2008, 25, 269–270. [Google Scholar] [CrossRef] [PubMed]
- Corren, J.; Shapiro, G.; Reimann, J.; Deniz, Y.; Wong, D.; Adelman, D.; Togias, A. Allergen skin tests and free ige levels during reduction and cessation of omalizumab therapy. J. Allergy Clin. Immunol. 2008, 121, 506–511. [Google Scholar] [CrossRef]
- Shah, K.M.; Rank, M.A.; Dave, S.A.; Oslie, C.L.; Butterfield, J.H. Predicting which medication classes interfere with allergy skin testing. Allergy Asthma Proc. 2010, 31, 477–482. [Google Scholar] [CrossRef]
- Birch, K.; Pearson-Shaver, A.L. Allergy Testing; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Sadreddini, H.A.; Starkey, E.S. Drug allergy: Diagnosis and management of drug allergy in adults, children and young people; a look at nice guidance. Arch. Dis. Child. Educ. Pract. Ed. 2016, 101, 239–242. [Google Scholar] [CrossRef][Green Version]
- Jang, W.R.; Nahm, C.H.; Kim, J.H.; Lim, D.H.; Jang, T.Y.; Moon, Y.S.; Kim, J.J. Allergen specific ige measurement with polycheck allergy: Comparison of three multiple allergen simultaneous tests. Korean J. Lab. Med. 2009, 29, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Park, K.H.; Kim, H.S.; Kim, K.W.; Sohn, M.H.; Kim, C.H.; Lee, J.S.; Hong, C.S.; Park, J.W. Specific ige measurement using advansure(r) system: Comparison of detection performance with immunocap(r) system in korean allergy patients. Clin. Chim. Acta 2012, 413, 914–919. [Google Scholar] [CrossRef]
- Jiang, X.D.; Li, G.Y.; Dong, Z.; Zhu, D.D. Correlation analysis of two serum-specific immunoglobulin e test systems and skin-prick test in allergic rhinitis patients from northeast china. Am. J. Rhinol. Allergy 2011, 25, 116–119. [Google Scholar] [CrossRef]
- Miyazaki, D.; Takamura, E.; Uchio, E.; Ebihara, N.; Ohno, S.; Ohashi, Y.; Okamoto, S.; Satake, Y.; Shoji, J.; Namba, K.; et al. Japanese guidelines for allergic conjunctival diseases 2020. Allergol. Int. Off. J. Jpn. Soc. Allergol. 2020, 69, 346–355. [Google Scholar] [CrossRef]
- De Amici, M.; Ciprandi, G. The age impact on serum total and allergen-specific ige. Allergy Asthma Immunol. Res. 2013, 5, 170–174. [Google Scholar] [CrossRef]
- Roberts, G.; Pfaar, O.; Akdis, C.A.; Ansotegui, I.J.; Durham, S.R.; Gerth van Wijk, R.; Halken, S.; Larenas-Linnemann, D.; Pawankar, R.; Pitsios, C.; et al. EAACI Guidelines on Allergen Immunotherapy: Allergic rhinoconjunctivitis. Allergy 2018, 73, 765–798. [Google Scholar] [CrossRef]
- Nolte, H.; Maloney, J.; Nelson, H.S.; Bernstein, D.I.; Lu, S.; Li, Z.; Kaur, A.; Zieglmayer, P.; Zieglmayer, R.; Lemell, P.; et al. Onset and dose-related efficacy of house dust mite sublingual immunotherapy tablets in an environmental exposure chamber. J. Allergy Clin. Immunol. 2015, 135, 1494–1501 e1496. [Google Scholar] [CrossRef]
- Calderon, M.A.; Penagos, M.; Sheikh, A.; Canonica, G.W.; Durham, S. Sublingual immunotherapy for treating allergic conjunctivitis. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef] [PubMed]
- Niggemann, B.; Jacobsen, L.; Dreborg, S.; Ferdousi, H.A.; Halken, S.; Host, A.; Koivikko, A.; Koller, D.; Norberg, L.A.; Urbanek, R.; et al. Five-year follow-up on the pat study: Specific immunotherapy and long-term prevention of asthma in children. Allergy 2006, 61, 855–859. [Google Scholar] [CrossRef]
- Chinthrajah, R.S.; Hernandez, J.D.; Boyd, S.D.; Galli, S.J.; Nadeau, K.C. Molecular and cellular mechanisms of food allergy and food tolerance. J. Allergy Clin. Immunol. 2016, 137, 984–997. [Google Scholar] [CrossRef] [PubMed]
- Ohn, J.; Paik, S.H.; Doh, E.J.; Park, H.S.; Yoon, H.S.; Cho, S. Allergen sensitization pattern by sex: A cluster analysis in korea. Ann. Dermatol. 2017, 29, 735–741. [Google Scholar] [CrossRef]
- El-Nahas, H.A.; El-Beshbishi, S.N.; Azab, M.S.; Zaalouk, T.; Elsheikha, H.M.; Saleh, A.B.; El-Shazly, A.M. Diagnostic criteria for house dust mites sensitized allergic patients. J. Egypt Soc. Parasitol. 2007, 37, 1113–1124. [Google Scholar] [PubMed]
- Abdel-Salam, B.K. Seasonal population of acarus siro mites and effects of their faeces on allergenic immunological disorder modulated by garlic in albino rat. Allergol. Immunopathol. 2012, 40, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.W.; Lee, H.B.; Kang, I.J.; Kim, S.W.; Park, K.S.; Kook, M.H.; Kim, B.S.; Baek, H.S.; Kim, J.H.; Kim, J.K.; et al. The revised edition of korean calendar for allergenic pollens. Allergy Asthma Immunol. Res. 2012, 4, 5–11. [Google Scholar] [CrossRef]
- Jung, S.W.; Oh, E.J.; Lee, J.; Kim, Y.; Kim, S.Y.; Kim, Y.; Park, Y.J. Usefulness of total ige in predicting positive allergen specific ige tests in korean subjects. Korean J. Lab. Med. 2010, 30, 660–667. [Google Scholar] [CrossRef][Green Version]
- Zhang, L.; Han, B.; Zhang, Z.; Liu, A.; Liu, G.; Du, Z.; Yao, Y.; Qi, Q. Skin prick test of inhalative allergens for patients with allergic rhinitis in yichang. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2014, 28, 98–101. [Google Scholar] [PubMed]
- Emanuel, I.A. In vitro testing for allergy diagnosis. Otolaryngol. Clin. N. Am. 2003, 36, 879–893. [Google Scholar] [CrossRef]
- Ownby, D.R.; Bailey, J. Comparison of mast with radioallergosorbent and skin tests for diagnosis of allergy in children. Am. J. Dis. Child. 1986, 140, 45–48. [Google Scholar] [CrossRef]
- Ahmed, I.; Nasreen, S. Frequency of raised serum ige level in childhood atopic dermatitis. J. Pak. Med. Assoc. 2007, 57, 431–434. [Google Scholar] [PubMed]
- Sunyer, J.; Anto, J.M.; Castellsague, J.; Soriano, J.B.; Roca, J. Total serum ige is associated with asthma independently of specific ige levels. The spanish group of the european study of asthma. Eur. Respir. J. 1996, 9, 1880–1884. [Google Scholar] [CrossRef] [PubMed]
- Salo, P.M.; Arbes, S.J., Jr.; Jaramillo, R.; Calatroni, A.; Weir, C.H.; Sever, M.L.; Hoppin, J.A.; Rose, K.M.; Liu, A.H.; Gergen, P.J.; et al. Prevalence of allergic sensitization in the united states: Results from the national health and nutrition examination survey (nhanes) 2005–2006. J. Allergy Clin. Immunol. 2014, 134, 350–359. [Google Scholar] [CrossRef]
- Johnson, C.C.; Peterson, E.L.; Ownby, D.R. Gender differences in total and allergen-specific immunoglobulin e (ige) concentrations in a population-based cohort from birth to age four years. Am. J. Epidemiol. 1998, 147, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Uekert, S.J.; Akan, G.; Evans, M.D.; Li, Z.; Roberg, K.; Tisler, C.; Dasilva, D.; Anderson, E.; Gangnon, R.; Allen, D.B.; et al. Sex-related differences in immune development and the expression of atopy in early childhood. J. Allergy Clin. Immunol. 2006, 118, 1375–1381. [Google Scholar] [CrossRef]
- Warm, K.; Backman, H.; Lindberg, A.; Lundback, B.; Ronmark, E. Low incidence and high remission of allergic sensitization among adults. J. Allergy Clin. Immunol. 2012, 129, 136–142. [Google Scholar] [CrossRef]
- Nakazawa, T.; Houjyo, S.; Dobashi, K.; Sato, K. Influence of aging and sex on specific ige antibody production. Intern Med. 1994, 33, 396–401. [Google Scholar] [CrossRef]
- Gomez, C.R.; Boehmer, E.D.; Kovacs, E.J. The aging innate immune system. Curr. Opin. Immunol. 2005, 17, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Sansoni, P.; Vescovini, R.; Fagnoni, F.; Biasini, C.; Zanni, F.; Zanlari, L.; Telera, A.; Lucchini, G.; Passeri, G.; Monti, D.; et al. The immune system in extreme longevity. Exp. Gerontol. 2008, 43, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Geha, R.S.; Jabara, H.H.; Brodeur, S.R. The regulation of immunoglobulin e class-switch recombination. Nat. Rev. Immunol. 2003, 3, 721–732. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, M.; Kishimoto, S. Ige antibody formation and aging. I. Age-related changes in ige antibody formation and avidity for the dnp-determinant in mice. J. Immunol. 1979, 123, 263–268. [Google Scholar] [PubMed]
| Allergen | Total (100%, n = 120) | Spring (24.2%, n = 29) | Summer (40.8%, n = 49) | Fall (26.7%, n = 32) | Winter (8.3%, n = 10) |
|---|---|---|---|---|---|
| TIgE | 57.5 | 51.7 | 63.3 | 50.0 | 60.0 |
| D. farinae | 36.7 | 27.6 | 46.9 | 31.3 | 30.0 |
| D. pteronyssinus | 34.2 | 17.2 | 44.9 | 34.4 | 30.0 |
| Tyrophagus putr. | 17.5 | 6.9 | 22.4 | 21.9 | 10.0 |
| Alternaria | 15.8 | 3.4 | 24.5 | 12.5 | 20.0 |
| House dust | 14.2 | 17.2 | 16.3 | 6.3 | 20.0 |
| Mugwort | 11.7 | 3.4 | 6.1 | 31.3 | 0.0 |
| Cat | 10.8 | 3.4 | 14.3 | 9.4 | 20.0 |
| Ragweed | 9.2 | 3.4 | 8.2 | 15.6 | 10.0 |
| Oxeye-daisy | 8.3 | 0.0 | 6.1 | 15.6 | 20.0 |
| Japanese hop | 8.3 | 3.4 | 6.1 | 15.6 | 10.0 |
| Birch-Alder mix | 8.3 | 6.9 | 6.1 | 12.5 | 10.0 |
| Rye pollen | 7.5 | 10.3 | 4.1 | 9.4 | 10.0 |
| Dandelion | 6.7 | 0.0 | 4.1 | 15.6 | 10.0 |
| Acarus siro | 5.8 | 13.8 | 4.1 | 0.0 | 10.0 |
| Milk | 5.0 | 6.9 | 6.1 | 3.1 | 0.0 |
| Cedar, Japan | 5.0 | 3.4 | 8.2 | 3.1 | 0.0 |
| Cladosporium | 5.0 | 0.0 | 4.1 | 6.3 | 20.0 |
| Russian Thistle | 4.2 | 0.0 | 6.1 | 6.3 | 0.0 |
| Egg white | 4.2 | 0.0 | 2.0 | 9.4 | 10.0 |
| Cockroach | 3.3 | 0.0 | 6.1 | 3.1 | 0.0 |
| Peach | 3.3 | 3.4 | 4.1 | 0.0 | 10.0 |
| Mackerel | 3.3 | 0.0 | 2.0 | 9.4 | 0.0 |
| Sycamore mix | 3.3 | 0.0 | 4.1 | 3.1 | 10.0 |
| Pigweed | 3.3 | 0.0 | 6.1 | 3.1 | 0.0 |
| Bermuda grass | 2.5 | 0.0 | 2.0 | 3.1 | 10.0 |
| Sweet vernal grass | 2.5 | 3.4 | 2.0 | 0.0 | 10.0 |
| Dog | 2.5 | 6.9 | 2.0 | 0.0 | 0.0 |
| Orchard grass | 2.5 | 3.4 | 4.1 | 3.1 | 0.0 |
| Hazelnut | 2.5 | 3.4 | 0.0 | 3.1 | 10.0 |
| Acacia | 2.5 | 0.0 | 2.0 | 3.1 | 10.0 |
| Sallow willow | 2.5 | 3.4 | 2.0 | 0.0 | 10.0 |
| CCD mix | 2.5 | 3.4 | 2.0 | 3.1 | 0.0 |
| Reed | 2.5 | 3.4 | 2.0 | 0.0 | 10.0 |
| Timothy grass | 2.5 | 3.4 | 4.1 | 3.1 | 0.0 |
| Oak, White | 2.5 | 6.9 | 0.0 | 0.0 | 10.0 |
| Crab | 1.7 | 0.0 | 2.0 | 3.1 | 0.0 |
| Honey bee | 1.7 | 0.0 | 2.0 | 0.0 | 10.0 |
| Potato | 1.7 | 0.0 | 2.0 | 0.0 | 10.0 |
| Soybean | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Pine | 0.8 | 0.0 | 0.0 | 0.0 | 10.0 |
| Poplar mix | 0.8 | 0.0 | 0.0 | 0.0 | 10.0 |
| Pork | 0.8 | 3.4 | 0.0 | 0.0 | 0.0 |
| Aspergillus | 0.8 | 0.0 | 0.0 | 3.1 | 0.0 |
| Cucumber | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Wheat flour | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Penicillium | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Latex | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Cacao | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Pupa | 0.8 | 0.0 | 0.0 | 3.1 | 0.0 |
| Mango | 0.8 | 0.0 | 2.0 | 0.0 | 0.0 |
| Banana | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Raw chestnut | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Buckwheat meal | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Candida albicans | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Guinea pig | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Peanut | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Sesame | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Number of Patients (%) | Age (Years) | M:F | |
|---|---|---|---|
| Group 1; TIgE (+) SIgE (+) | 59 (49.2) | 33.6 ± 18.2 | 22:37 |
| Group 2; TIgE (−) SIgE (+) | 24 (20.0) | 34.2 ± 16.3 | 4:20 |
| Group 3; TIgE (+) SIgE (−) | 10 (8.3) | 42.1 ± 16.0 | 5:5 |
| Group 4; TIgE (−) SIgE (−) | 27 (22.5) | 39.1 ± 17.2 | 1:26 |
| p value | 0.154 | 0.002 |
| Sex (Male vs. Female) | Total (n = 120) | Male (n = 32) | Female (n = 88) | p value |
|---|---|---|---|---|
| Age | 35.7 ± 17.5 | 33.3 ± 16.9 | 36.55 ± 17.7 | 0.345 |
| TIgE(+):TIge(−) | 69:51 (57.5%:42.5%) | 27:5 (84.4%:15.6%) | 42:46 (47.7%:52.3%) | <0.001 |
| SIgE(+):SIge(−) | 83:37 (69.2%:30.8%) | 26:6 (81.2%:18.8%) | 57:31 (64.8%:35.2%) | 0.084 |
| AIgE(+):AIge(−) | 93:27 (77.5%:22.5%) | 31:1 (96.9%:3.1%) | 62:26 (70.5%:29.5%) | 0.001 |
| Age (young vs. old) | Total (n = 120) | Young group(n = 70) | Old group (n = 50) | p value |
| Sex (male:female) | 32:88 | 20:50 | 12:38 | 0.577 |
| TIgE(+): TIge(−) | 69:51 (57.5%:42.5%) | 45:25 (64.3%:35.7%) | 24:26 (48.0%:52.0%) | 0.075 |
| SIgE(+): SIge(−) | 83:37 (69.2%:30.8%) | 54:16 (77.1%:22.9%) | 29:21 (58.0%:42.0%) | 0.025 |
| AIgE(+):AIge(−) | 93:27 (77.5%:22.5%) | 58:12 (82.9%:17.1%) | 35:15 (70.0%:30.0%) | 0.096 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, J.Y.; Lee, H.; Chung, J.L.; Kim, Y.J.; Kim, J.Y.; Tchah, H. Multiple Allergen Simultaneous Test-Immunoblot Assay for Immunoglobulin E Detection in Patients with Isolated Allergic Conjunctivitis. J. Clin. Med. 2021, 10, 960. https://doi.org/10.3390/jcm10050960
Han JY, Lee H, Chung JL, Kim YJ, Kim JY, Tchah H. Multiple Allergen Simultaneous Test-Immunoblot Assay for Immunoglobulin E Detection in Patients with Isolated Allergic Conjunctivitis. Journal of Clinical Medicine. 2021; 10(5):960. https://doi.org/10.3390/jcm10050960
Chicago/Turabian StyleHan, Jung Yeob, Hun Lee, Jae Lim Chung, Young Jun Kim, Jae Yong Kim, and Hungwon Tchah. 2021. "Multiple Allergen Simultaneous Test-Immunoblot Assay for Immunoglobulin E Detection in Patients with Isolated Allergic Conjunctivitis" Journal of Clinical Medicine 10, no. 5: 960. https://doi.org/10.3390/jcm10050960
APA StyleHan, J. Y., Lee, H., Chung, J. L., Kim, Y. J., Kim, J. Y., & Tchah, H. (2021). Multiple Allergen Simultaneous Test-Immunoblot Assay for Immunoglobulin E Detection in Patients with Isolated Allergic Conjunctivitis. Journal of Clinical Medicine, 10(5), 960. https://doi.org/10.3390/jcm10050960








