Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort
Abstract
1. Introduction
2. Materials and Methods
Patients
3. Clinical Evaluation
4. Statistical Analysis
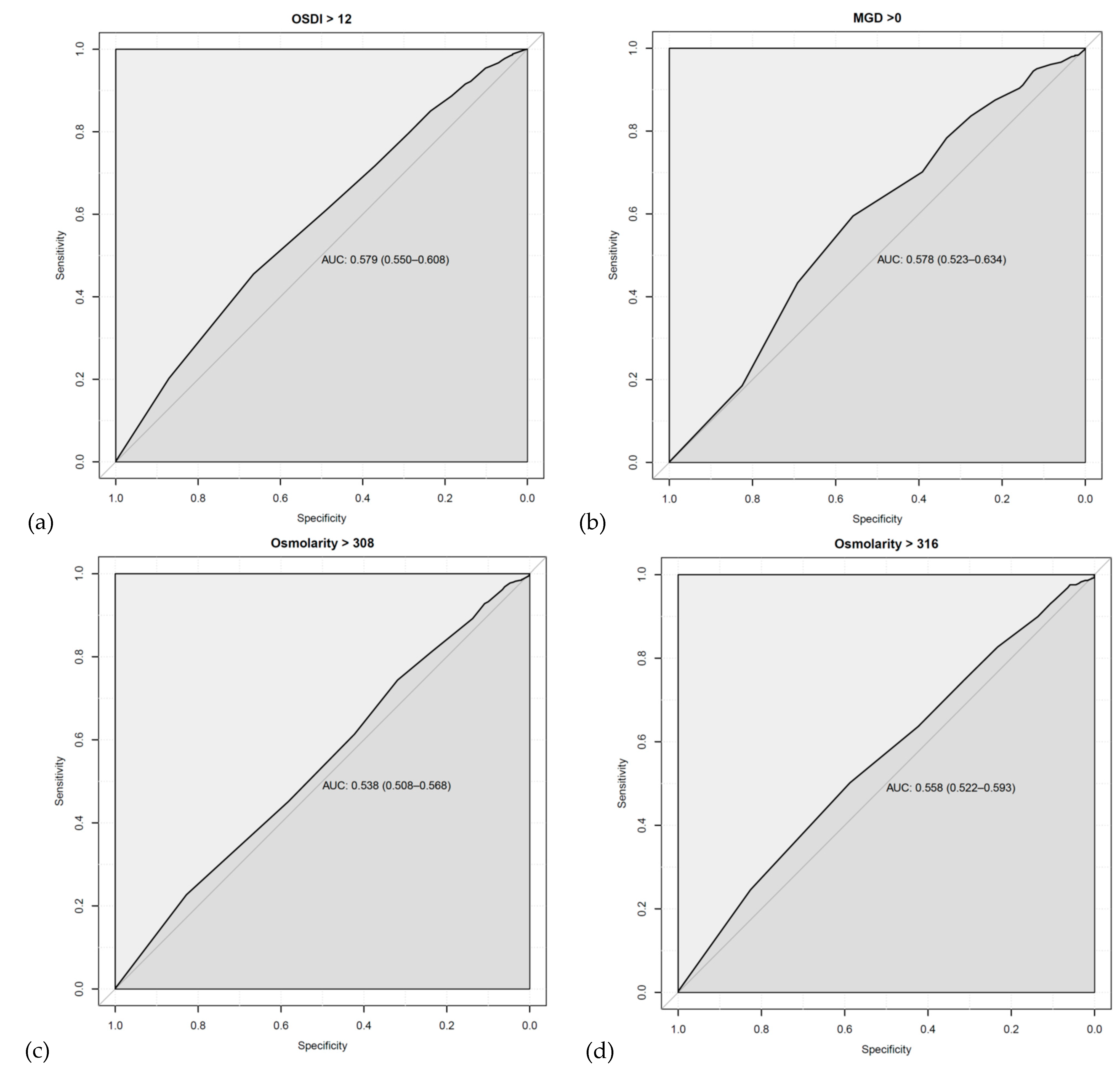
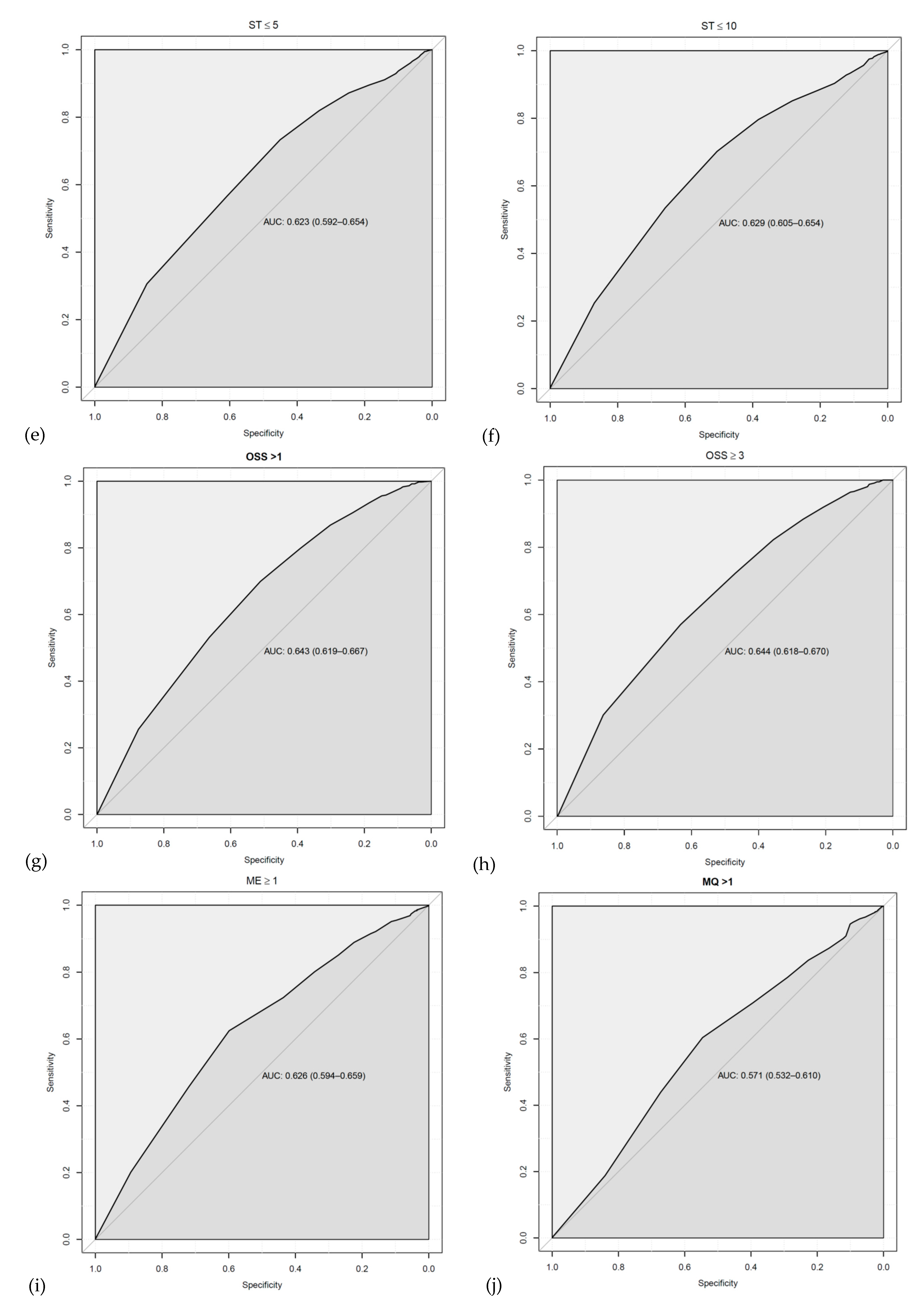
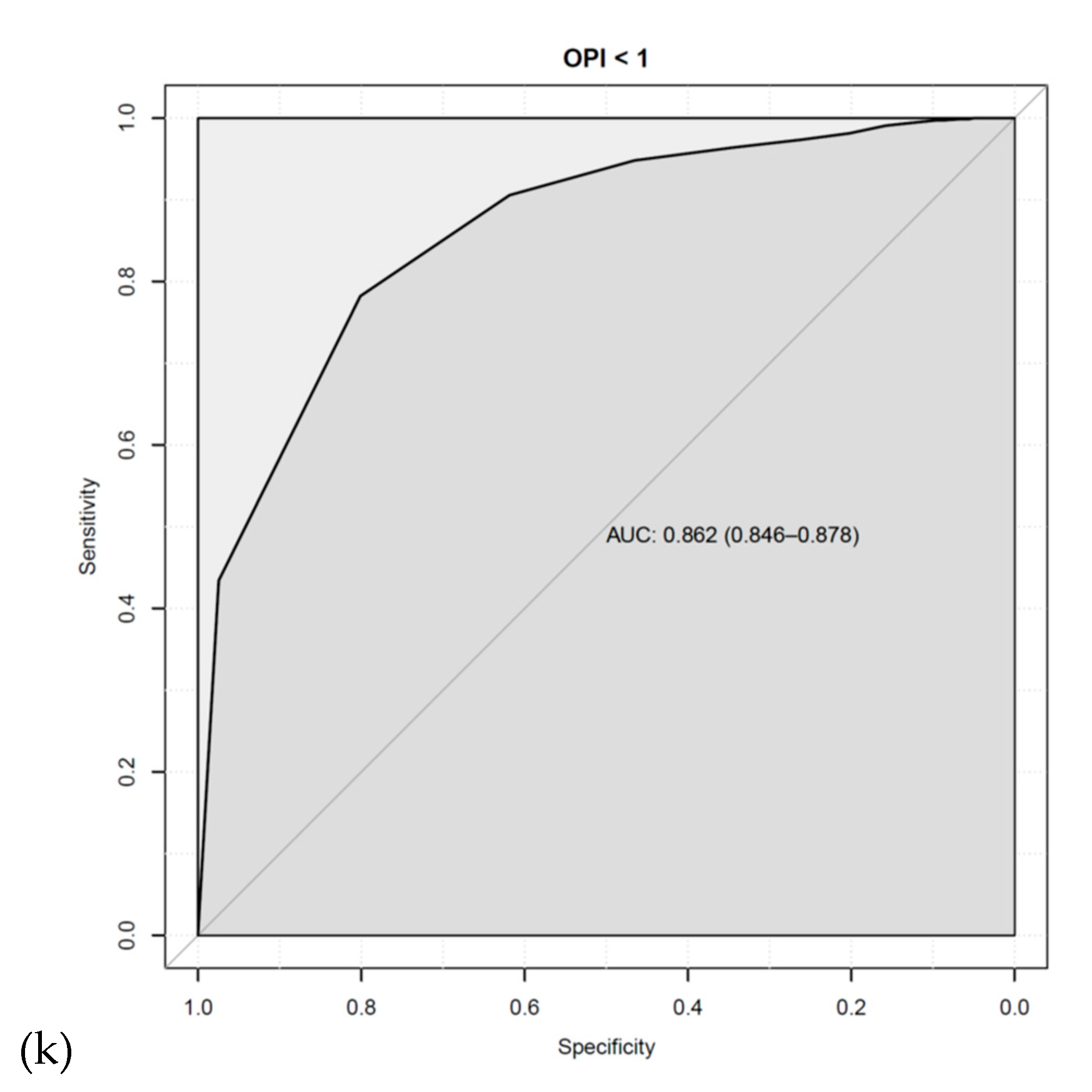
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.-S.; Schaumberg, D.; Uchino, M.; Vehof, J. Tfos dews ii epidemiology report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef]
- O’Brien, P.D.; Collum, L.M. Dry eye: Diagnosis and current treatment strategies. Curr. Allergy Asthma Rep. 2004, 4, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Danjo, Y. Diagnostic usefulness and cutoff value of Schirmer’s I test in the Japanese diagnostic criteria of dry eye. Graefes Arch. Clin. Exp. Ophthalmol. 1997, 235, 761–766. [Google Scholar] [CrossRef]
- Alves, M.; Reinach, P.S.; Paula, J.S.; e Cruz, A.A.V.; Bachette, L.; Faustino, J.; Aranha, F.P.; Vigorito, A.; de Souza, C.A.; Rocha, E.M. Comparison of diagnostic tests in distinct well-defined conditions related to dry eye disease. PLoS ONE 2014, 9, e97921. [Google Scholar] [CrossRef]
- Yazdani, M.; Chen, X.; Tashbayev, B.; Utheim, Ø.A.; Ræder, S.; Hua, Y.; Eidet, J.R.; Stojanovic, A.; Dartt, D.A.; Utheim, T.P. Evaluation of the ocular surface disease index questionnaire as a discriminative test for clinical findings in dry eye disease patients. Curr. Eye Res 2019, 6, 1–7. [Google Scholar] [CrossRef]
- Bartlett, J.D.; Keith, M.S.; Sudharshan, L.; Snedecor, S.J. Associations between signs and symptoms of dry eye disease: A systematic review. Clin. Ophthalmol. 2015, 9, 1719. [Google Scholar] [CrossRef]
- Tashbayev, B.; Yazdani, M.; Arita, R.; Fineide, F.; Utheim, T.P. Intense pulsed light treatment in meibomian gland dysfunction: A concise review. Ocul. Surf. 2020, 18, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Norn, M. Desiccation of the precorneal film: I. Corneal wetting-time. Acta Ophthalmol. 1969, 47, 865–880. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, D.F.; Millar, T.J.; Raju, S.R. Tear film stability: A review. Exp Eye Res 2013, 117, 28–38. [Google Scholar] [CrossRef]
- Smith, J.; Nichols, K.K.; Baldwin, E.K. Current patterns in the use of diagnostic tests in dry eye evaluation. Cornea 2008, 27, 656–662. [Google Scholar] [CrossRef]
- Willcox, M.D.; Argüeso, P.; Georgiev, G.A.; Holopainen, J.M.; Laurie, G.W.; Millar, T.J.; Papas, E.B.; Rolland, J.P.; Schmidt, T.A.; Stahl, U. TFOS DEWS II tear film report. Ocul. Surf. 2017, 15, 366–403. [Google Scholar] [CrossRef] [PubMed]
- Cho, P.; Brown, B.; Chan, I.; Conway, R.; Yap, M. Reliability of the tear break-up time technique of assessing tear stability and the locations of the tear break-up in Hong Kong Chinese. Optom Vis. Sci. 1992, 69, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Lemp, M.A.; Hamill, J.R. Factors affecting tear film breakup in normal eyes. Arch Ophthal. 1973, 89, 103–105. [Google Scholar] [CrossRef]
- Vanley, G.T.; Leopold, I.H.; Gregg, T.H. Interpretation of tear film breakup. Arch Ophthal. 1977, 95, 445–448. [Google Scholar] [CrossRef]
- Lee, J.H.; Kee, C.W. The significance of tear film break-up time in the diagnosis of dry eye syndrome. Korean J. Ophthalmol. 1988, 2, 69–71. [Google Scholar] [CrossRef]
- Tavares, F.P.; Fernandes, R.S.; Bernardes, T.F.; Bonfioli, A.A.; Soares, E. Dry eye disease. Semin. Ophthalmol. 2010, 25, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J. Diagnosis of dry eye. Surv. Ophthalmol. 2001, 45, S221–S226. [Google Scholar] [CrossRef]
- Mengher, L.S.; Bron, A.J.; Tonge, S.R.; Gilbert, D.J. Effect of fluorescein instillation on the pre-corneal tear film stability. Curr. Eye Res. 1985, 4, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Abelson, M.B.; Ousler, G.W.; Nally, L.A.; Welch, D.; Krenzer, K. Alternative reference values for tear film break up time in normal and dry eye populations . In Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3; Springer: New York, NY, USA, 2002; pp. 1121–1125. [Google Scholar]
- Abelson, R.; Lane, K.J.; Rodriguez, J.; Johnston, P.; Angjeli, E.; Ousler, G.; Montgomery, D. A single-center study evaluating the effect of the controlled adverse environment (CAESM) model on tear film stability. Clin. Ophthalmol. 2012, 6, 1865. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pflugfelder, S.C.; Tseng, S.C.; Sanabria, O.; Kell, H.; Garcia, C.G.; Felix, C.; Feuer, W.; Reis, B.L. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea 1998, 17, 38. [Google Scholar] [CrossRef]
- Kim, K.T.; Kim, J.-h.; Kong, Y.T.; Chae, J.B.; Hyung, S. Reliability of a new modified tear breakup time method: Dry tear breakup time. Graefes Arch Clin Exp Ophthalmol 2015, 253, 1355–1361. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, M.; Chen, X.; Tashbayev, B.; Utheim, Ø.A.; Ræder, S.; Lagli, N.; Stojanovic, A.; Dartt, D.A.; Utheim, T.P. Tear production levels and dry eye disease severity in a large Norwegian cohort. Curr. Eye Res 2018, 43, 1465–1470. [Google Scholar] [CrossRef]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthal 2000, 118, 615–621. [Google Scholar] [CrossRef]
- Ousler, G.W., III; Hagberg, K.W.; Schindelar, M.; Welch, D.; Abelson, M.B. The ocular protection index. Cornea 2008, 27, 509–513. [Google Scholar] [CrossRef]
- Bron, A.J.; Evans, V.E.; Smith, J.A. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea 2003, 22, 640–650. [Google Scholar] [CrossRef]
- Geerling, G.; Tauber, J.; Baudouin, C.; Goto, E.; Matsumoto, Y.; O’Brien, T.; Rolando, M.; Tsubota, K.; Nichols, K.K. The international workshop on meibomian gland dysfunction: Report of the subcommittee on management and treatment of meibomian gland dysfunction. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2050–2064. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing; Team, R.C.: Vienna, Austria, 2020. [Google Scholar]
- Ichihashi, Y.; Ide, T.; Kaido, M.; Ishida, R.; Hatou, S.; Tsubota, K. Short break-up time type dry eye has potential ocular surface abnormalities. Taiwan J. Ophthalmol. 2015, 5, 68–71. [Google Scholar] [CrossRef]
- Foulks, G.N. Challenges and pitfalls in clinical trials of treatments for dry eye. Ocul. Surf. 2003, 1, 20–30. [Google Scholar] [CrossRef]
- Savini, G.; Prabhawasat, P.; Kojima, T.; Grueterich, M.; Espana, E.; Goto, E. The challenge of dry eye diagnosis. Clin. Ophthalmol. 2008, 2, 31–55. [Google Scholar] [CrossRef]
- Javadi, M.-A.; Feizi, S. Dry eye syndrome. J. Ophthalmic Vis. Res. 2011, 6, 192. [Google Scholar] [PubMed]
- Tsubota, K.; Yokoi, N.; Shimazaki, J.; Watanabe, H.; Dogru, M.; Yamada, M.; Kinoshita, S.; Kim, H.-M.; Tchah, H.-W.; Hyon, J.Y. New perspectives on dry eye definition and diagnosis: A consensus report by the Asia Dry Eye Society. Ocul. Surf. 2017, 15, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H. TFOS DEWS II diagnostic methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef]
- Zou, K.H.; O’Malley, A.J.; Mauri, L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 2007, 115, 654–657. [Google Scholar] [CrossRef]
- Crampton, J.; Abelson, M.; Ousler, G., III; Pflugfelder, S.; De Paiva, C.; Forbes, M.; Power, D. Correlation of the controlled adverse environment (CAE) model with a murine model of experimental dry eye in assessing the ability of topical doxycycline to prevent corneal barrier disruption. Investig. Ophthalmol. Vis. Sci. 2007, 48, 402. [Google Scholar]
- D’Arienzo, P.; Ousler, G.W.; Schindelar, M.S. A comparison of two marketed artificial tears in improvement of tear film stability as measured by tear film break-up time (TFBUT) and ocular protection index (OPI). In Proceedings of the Poster Presentation, Tear Film and Ocular Surface Society Meeting, Taormina, Sicily, Italy, 5–8 September 2007. [Google Scholar]
- Ousler, G.; Emory, T.; Welch, D.; Abelson, M. Factors that influence the inter-blink interval (IBI) as measured by the ocular protection index (OPI). Investig. Ophthalmol. Vis. Sci. 2002, 43, 56. [Google Scholar]
- Hagberg, K.W.; Ousler, G., III; Casavant, J.; Welch, D.; Abelson, M. Effect of menopause on the ocular protection index (OPI) in a population of dry eye patients of Ashkenazi Jewish descent. Investig. Ophthalmol. Vis. Sci. 2005, 46, 4470. [Google Scholar]
- Ousler, G.W.; Michaelson, C.; Christensen, M.T. An evaluation of tear film breakup time extension and ocular protection index scores among three marketed lubricant eye drops. Cornea 2007, 26, 949–952. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Utheim, Ø.A.; Xiao, J.; Adil, M.Y.; Stojanovic, A.; Tashbayev, B.; Jensen, J.L.; Utheim, T.P. Meibomian gland features in a Norwegian cohort of patients with primary Sjögren’ s syndrome. PLoS ONE 2017, 12, e0184284. [Google Scholar] [CrossRef]
- Kim, M.; Kim, H.S.; Na, K.-S. Correlation between tear osmolarity and other ocular surface parameters in primary Sjögren’s Syndrome. Korean J. Ophthalmol. 2017, 31, 25–31. [Google Scholar] [CrossRef]
- Mathews, P.M.; Karakus, S.; Agrawal, D.; Hindman, H.B.; Ramulu, P.Y.; Akpek, E.K. Tear osmolarity and correlation with ocular surface parameters in patients with dry eye. Cornea 2017, 36, 1352–1357. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.N.; Graham, A.D.; Lin, M.C. Relationships among tear film stability, osmolarity, and dryness symptoms. Optom. Vis. Sci. 2015, 92, e264. [Google Scholar] [CrossRef] [PubMed]
- Messmer, E.M.; Bulgen, M.; Kampik, A. Hyperosmolarity of the tear film in dry eye syndrome. In Research Projects in Dry Eye Syndrome; Karger Publishers: Basel, Switzerland, 2010; Volume 45, pp. 129–138. [Google Scholar]
- Bunya, V.Y.; Fuerst, N.M.; Pistilli, M.; McCabe, B.E.; Salvo, R.; Macchi, I.; Ying, G.-S.; Massaro-Giordano, M. Variability of tear osmolarity in patients with dry eye. JAMA Ophthalmol. 2015, 133, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Szalai, E.; Berta, A.; Szekanecz, Z.; Szûcs, G.; Módis, L., Jr. Evaluation of tear osmolarity in non-Sjögren and Sjögren syndrome dry eye patients with the TearLab system. J. Cornea 2012, 31, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Baenninger, P.B.; Voegeli, S.; Bachmann, L.M.; Faes, L.; Iselin, K.; Kaufmann, C.; Thiel, M.A. Variability of tear osmolarity measurements with a point-of-care system in healthy subjects—Systematic review. Cornea 2018, 37, 938–945. [Google Scholar] [CrossRef]
- Tashbayev, B.; Utheim, T.P.; Utheim, Ø.A.; Ræder, S.; Jensen, J.L.; Yazdani, M.; Lagali, N.; Vitelli, V.; Dartt, D.A.; Chen, X. Utility of tear osmolarity Measurement in Diagnosis of Dry eye Disease. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef]
- Sullivan, B.D.; Whitmer, D.; Nichols, K.K.; Tomlinson, A.; Foulks, G.N.; Geerling, G.; Pepose, J.S.; Kosheleff, V.; Porreco, A.; Lemp, M.A. An objective approach to dry eye disease severity. J. Investig. Ophthalmol. Vis. Sci. 2010, 51, 6125–6130. [Google Scholar] [CrossRef] [PubMed]
- Lemp, M.A.; Bron, A.J.; Baudouin, C.; del Castillo, J.M.B.; Geffen, D.; Tauber, J.; Foulks, G.N.; Pepose, J.S.; Sullivan, B.D. Tear osmolarity in the diagnosis and management of dry eye disease. Am. J. Ophthalmol. 2011, 151, 792–798.e791. [Google Scholar] [CrossRef]
- Sullivan, B.D.; Crews, L.A.; Messmer, E.M.; Foulks, G.N.; Nichols, K.K.; Baenninger, P.; Geerling, G.; Figueiredo, F.; Lemp, M.A. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: Clinical implications. Acta Ophthalmol. 2014, 92, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Inomata, T.; Iwagami, M.; Hiratsuka, Y.; Fujimoto, K.; Okumura, Y.; Shiang, T.; Murakami, A. Maximum blink interval is associated with tear film breakup time: A new simple, screening test for dry eye disease. Sci. Rep. 2018, 8, 1–6. [Google Scholar]
- Hirosawa, K.; Inomata, T.; Sung, J.; Nakamura, M.; Okumura, Y.; Midorikawa-Inomata, A.; Miura, M.; Fujio, K.; Akasaki, Y.; Fujimoto, K. Diagnostic ability of maximum blink interval together with Japanese version of Ocular Surface Disease Index score for dry eye disease. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Abelson, R.; Lane, K.J.; Angjeli, E.; Johnston, P.; Ousler, G.; Montgomery, D. Measurement of ocular surface protection under natural blink conditions. Clin. Ophthalmol. 2011, 5, 1349. [Google Scholar]
- Grubbs, J.R., Jr.; Tolleson-Rinehart, S.; Huynh, K.; Davis, R.M. A review of quality of life measures in dry eye questionnaires. Cornea 2014, 33, 215. [Google Scholar] [CrossRef]
- Zeev, M.S.-B.; Miller, D.D.; Latkany, R. Diagnosis of dry eye disease and emerging technologies. Clin. Ophthalmol. 2014, 8, 581–590. [Google Scholar] [CrossRef]
- Li, M.; Gong, L.; Chapin, W.J.; Zhu, M. Assessment of vision-related quality of life in dry eye patients. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5722–5727. [Google Scholar] [CrossRef] [PubMed]
- Ünlü, C.; Güney, E.; Akçay, B.İ.S.; Akçalı, G.; Erdoğan, G.; Bayramlar, H. Comparison of ocular-surface disease index questionnaire, tearfilm break-up time, and Schirmer tests for the evaluation of the tearfilm in computer users with and without dry-eye symptomatology. Clin. Ophthalmol. (Auckland, NZ) 2012, 6, 1303–1306. [Google Scholar] [CrossRef]
- Rossi, G.C.M.; Tinelli, C.; Pasinetti, G.M.; Milano, G.; Bianchi, P.E. Dry eye syndrome-related quality of life in glaucoma patients. Eur. J. Ophthalmol. 2009, 19, 572–579. [Google Scholar] [CrossRef]
- Portello, J.K.; Rosenfield, M.; Bababekova, Y.; Estrada, J.M.; Leon, A. Computer-related visual symptoms in office workers. Ophthalmic Physiol. Opt. 2012, 32, 375–382. [Google Scholar] [CrossRef]
- García-Catalán, M.; Jerez-Olivera, E.; Benítez-Del-Castillo-Sánchez, J. Dry eye and quality of life. Arch. Soc. Esp. Oftalmol. 2009, 84, 451–458. [Google Scholar]
- Onwubiko, S.N.; Eze, B.I.; Udeh, N.N.; Onwasigwe, E.N.; Umeh, R.E. Dry eye disease: Concordance between the diagnostic tests in african eyes. Eye Cont. Lens 2016, 42, 395–400. [Google Scholar] [CrossRef]
- Fenga, C.; Aragona, P.; Di Nola, C.; Spinella, R. Comparison of ocular surface disease index and tear osmolarity as markers of ocular surface dysfunction in video terminal display workers. Am. J. Ophthalmol. 2014, 158, 41–48.e42. [Google Scholar] [CrossRef]
- Yeotikar, N.S.; Zhu, H.; Markoulli, M.; Nichols, K.K.; Naduvilath, T.; Papas, E.B. Functional and morphologic changes of meibomian glands in an asymptomatic adult population functional and morphologic changes of meibomian glands. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3996–4007. [Google Scholar] [CrossRef]
- Wood, S.D.; Mian, S.I. Diagnostic tools for dry eye disease. J. Eu Ophthal. Rev. 2016, 10, 101–107. [Google Scholar] [CrossRef]
- Sullivan, D.A. Sex and sex steroid influences on dry eye syndrome. In Dry Eye and Ocular Surface Disorders; CRC Press: Boca Raton, FL, USA, 2004; pp. 177–202. [Google Scholar]
- Han, S.B.; Hyon, J.Y.; Woo, S.J.; Lee, J.J.; Kim, T.H.; Kim, K.W. Prevalence of dry eye disease in an elderly Korean population. Arch. Ophthal. 2011, 129, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Jie, Y.; Xu, L.; Wu, Y.; Jonas, J.B. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye 2009, 23, 688–693. [Google Scholar] [CrossRef]
- Moss, S.E.; Klein, R.; Klein, B.E. Incidence of dry eye in an older population. Arch. Ophthal. 2004, 122, 369–373. [Google Scholar] [CrossRef]
- Uchino, M.; Nishiwaki, Y.; Michikawa, T.; Shirakawa, K.; Kuwahara, E.; Yamada, M.; Dogru, M.; Schaumberg, D.A.; Kawakita, T.; Takebayashi, T. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology 2011, 118, 2361–2367. [Google Scholar] [CrossRef]
- Tang, K.; Lu, S.-Y.; Ma, D.-L.; Leung, C.-H.; Lee, S.-S.; Lin, S.-W.; D. Wang, H.-M. A Review on Common Ingredients of Periocular Cosmetics and Their Hazards. Curr. Org. Chem. 2015, 19, 30–38. [Google Scholar] [CrossRef]
- Wang, M.T.; Craig, J.P. Investigating the effect of eye cosmetics on the tear film: Current insights. Clin. Optom. 2018, 10, 33. [Google Scholar] [CrossRef]
- Ng, A.; Evans, K.; North, R.V.; Jones, L.; Purslow, C. Impact of eye cosmetics on the eye, adnexa, and ocular surface. Eye Cont. Lens 2016, 42, 211–220. [Google Scholar] [CrossRef]
| Number of Subjects | |||||
|---|---|---|---|---|---|
| Test * | Total | Female | Male | Missing Sex | Adjusted p-Value ** |
| OSDI | 1977 | 1436 | 538 | 3 | 0.00192 |
| Osm | 835 | 633 | 201 | 1 | <0.001 |
| TFBUT | 1959 | 1423 | 533 | 3 | <0.001 |
| BI | 1971 | 1433 | 535 | 3 | 0.00827 |
| OPI | 1971 | 1433 | 535 | 3 | 0.214 |
| ST | 1942 | 1408 | 532 | 2 | 0.990 |
| OSS | 1959 | 1424 | 532 | 3 | <0.001 |
| ME | 1873 | 1348 | 523 | 2 | 1.927 |
| MQ | 1871 | 1343 | 526 | 2 | 1.752 |
| MGD | 1881 | 1353 | 526 | 2 | 5.925 |
| Number of Subjects | ||||
|---|---|---|---|---|
| Age Group | Total | Female | Male | Adjusted p-Value * |
| 0–19 | 28 | 11 | 17 | <0.001 |
| 20–39 | 451 | 272 | 179 | <0.001 |
| 40–59 | 783 | 599 | 184 | 0.0107 |
| 60–79 | 679 | 520 | 159 | 0.0258 |
| 80–99 | 78 | 64 | 14 | 0.3775 |
| Total | 2061 ** | 1496 | 565 | |
| Cut-Off Value: 2 | Cut-Off Value: 5 | Cut-Off Value: 10 | Cut-Off Value: 15 | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | ||||||||
| n | 824 | 1111 | 1502 | 433 | 1820 | 115 | 1894 | 41 |
| Percent | 42.58% | 57.42% | 77.62% | 22.38% | 94.06% | 5.94% | 97.88% | 2.12% |
| Cut-Off Value: 2 | Cut-Off Value: 5 | Cut-Off Value: 10 | Cut-Off Value: 15 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test * | ||||||||||||
| OSDI | (0–100) 778 | (0–100) 1004 | <0.001 | (0–100) 1392 | (0–100) 390 | 0.00336 | (0–100) 1678 | (0–82) 104 | <0.001 | (0–100) 1748 | (0–78.6) 34 | 0.0583 |
| Osm | (276–395) 364 | (275–398) 469 | 0.0123 | (275–398) 663 | (280–386) 170 | 0.124 | (275–398) 798 | (280–369) 35 | 0.139 | (275–398) 820 | (283–358) 13 | 0.737 |
| BI | (0.8–60) 753 | (1–60) 921 | <0.001 | (0.8–60) 1311 | (1–60) 363 | <0.001 | (0.8–60) 1580 | (1–30) 94 | <0.001 | (0.8–60) 1641 | (1–15) 33 | <0.001 |
| OPI | (0–2) 753 | (0.05–20) 921 | <0.001 | (0–5) 1311 | (0.12–20) 363 | <0.001 | (0–10) 1580 | (0.4–20) 94 | <0.001 | (0–11.82) 1641 | (1.33–20) 33 | <0.001 |
| ST | (0–36) 799 | (0–36) 1057 | <0.001 | (0–36) 1453 | (0–36) 403 | <0.001 | (0–36) 1750 | (1–36) 106 | <0.001 | (0–36) 1820 | (4–36) 36 | 0.00178 |
| OSS | (0–13) 823 | (0–10) 1109 | <0.001 | (0–13) 1500 | (0–9) 432 | <0.001 | (0–13) 1817 | (0–6) 115 | <0.001 | (0–13) 1891 | (0–2) 41 | <0.001 |
| ME | (0–3) 787 | (0–3) 1051 | <0.001 | (0–3) 1428 | (0–3) 410 | <0.001 | (0–3) 1728 | (0–3) 110 | <0.001 | (0–3) 1798 | (0–3) 40 | 0.00733 |
| MQ | (0–24) 779 | (0–24) 1046 | <0.001 | (0–24) 1418 | (0–24) 407 | 0.0022 | (0–24) 1717 | (0–18) 108 | <0.001 | (0–24) 1785 | (0–16) 40 | 0.01795 |
| MGD | (0–1) 794 | (0–1) 1062 | <0.001 | (0–1) 1441 | (0–1) 415 | <0.001 | (0–1) 1744 | (0–1) 112 | <0.001 | (0–1) 1816 | (0–1) 40 | 0.06897 |
| Cut-Off Value: 2 | Cut-Off Value: 5 | Cut-Off Value: 10 | Cut-Off Value: 15 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Test * | |||||||||
| OSDI | F M p * | (0.100) (0–97.9) 0.00197 | (0–100) (0–83.3) 0.0458 | (0–100) (0–97.9) 0.00016 | (0–100) (0–83.3) 0.81 | (0–100) (0–97.9) 0.0004 | (0–75) (0–82) 0.79 | (0–100) (0–97.9) 0.0003 | (2.1–75) (0–78.6) 0.86 |
| Osm | F M p * | (276 –395) (281 –380) 0.00137 | (275–398) (280–366) 0.0233 | (275– 398) (281– 380) 0.0007 | (282– 386) (280– 358) 0.10 | (275– 398) (281– 380) 0.0002 | .6 (284–369) .8 (280–358) 0.23 | (275–398) (280–380) 0.00005 | (289–324) (283–358) 0.83 |
| BI | F M p * | (0.8–60) (1–30) 0.0544 | (1–60) (1–60) 0.046 | (0.8–60) (1–60) 0.0008 | (1–60) (1–60) 0.38 | (0.8–60) (1–60) 0.0022 | (1–15) (1.1–30) 0.87 | (0.8–60) (1–60) 0.0016 | (1–15) (2.1–6) 0.32 |
| OPI | F M p * | (0–2) (0.07–2) 0.0699 | (0.12–20) (.05–12) 0.0465 | (0–5) (.05–4.2) 0.0577 | (0.12– 20) (0.15– 12) 0.198 | (0–9.1) (.05–10) 0.34 | (0.9–20) (0.4–12) 0.51 | (0–10.8) (.05–11.8) 0.11 | (1.3– 20) (3.3– 9.5) 0.14 |
| ST | F M p * | (0–36) (0–36) 0.55 | (0–36) (0–36) 0.13 | (0–36) (0–36) 0.81 | (0–36) (1–36) 0.54 | (0–36) (0–36) 0.25 | (1–36) (1–36) 0.32 | (0–36) (0–36) 0.12 | (4–36) (7–35) 0.91 |
| OSS | F M p * | (0–12) (0–13) 0.0401 | (0–10) (0–10) 0.0072 | (0–12) (0–13) 0.0372 | (0–7) (0–9) 0.0593 | (0–12) (0–13) 0.0017 | (0–6) (0–6) 0.0828 | (0–12) (0–13) 0.0003 | 0 (0–2) (0–2) 0.0869 |
| ME | F M p * | (0–3) (0–3) 0.39 | (0–3) (0–3) 0.15 | (0–3) (0–3) 0.20 | (0–3) (0–3) 0.0162 | (0–3) (0–3) 0.48 | (0–3) (0–3) 0.72 | (0–3) (0–3) 0.27 | (0–3) (0–3) 0.99 |
| MQ | F M p * | (0–24) (0–24) 0.15 | (0–24) (0–24) 0.29 | (0–24) (0–24) 0.0714 | (0–24) (0–22) 0.59 | (0–24) (0–24) 0.0693 | (0–16) (0–18) 0.94 | (0–24) (0–24) 0.13 | (0–12) (0–16) 0.95 |
| MGD | F M p * | (0–1) (0–1) 1 | (0–1) (0–1) 1 | (0–1) (0–1) 0.19 | (0–1) (0–1) 0.40 | (0–1) (0–1) 0.84 | (0–1) (0–1) 0.77 | (0–1) (0–1) 0.6 | (0–1) (0–1) 1 |
| Variable * | Pearson’s r to TFBUT | 95% CI for r | p-Value ** |
|---|---|---|---|
| OSDI | −0.091 | (−0.143, −0.051) | <0.0001 |
| Osm | −0.049 | (−0.116, 0.011) | 0.0527 |
| BI | 0.093 | (0.053, 0.148) | <0.0001 |
| OPI | 0.696 | (0.677, 0.718) | <0.0001 |
| ST | 0.205 | (0.162, 0.249) | <0.0001 |
| OSS | −0.241 | (−0.283, −0.199) | <0.0001 |
| ME | −0.191 | (−0.238, −0.150) | <0.0001 |
| MQ | −0.108 | (−0.155, −0.065) | <0.0001 |
| MGD | −0.134 | (−0.180, −0.091) | <0.0001 |
| OSDI | Osm | BI | OPI | ST | OSS | ME | MQ | MGD | |
|---|---|---|---|---|---|---|---|---|---|
| OSDI | 1 | 0.036 | −0.042 | −0.004 | −0.057 | 0.09 | 0.009 | −0.002 | 0.033 |
| Osm | 0.036 | 1 | −0.066 | −0.003 | −0.061 | 0.082 | −0.045 | −0.035 | −0.031 |
| BI | −0.042 | −0.066 | 1 | −0.189 | 0.015 | −0.079 | −0.11 | −0.028 | −0.038 |
| OPI | −0.004 | −0.003 | −0.189 | 1 | 0.138 | −0.152 | −0.176 | −0.075 | −0.121 |
| ST | −0.057 | −0.061 | 0.015 | 0.138 | 1 | −0.193 | −0.004 | −0.015 | 0.011 |
| OSS | 0.09 | 0.082 | −0.079 | −0.152 | −0.193 | 1 | 0.107 | −0.004 | 0.058 |
| ME | 0.009 | −0.045 | −0.11 | −0.176 | −0.004 | 0.107 | 1 | 0.173 | 0.289 |
| MQ | −0.002 | −0.035 | −0.028 | −0.075 | −0.015 | −0.004 | 0.173 | 1 | 0.259 |
| MGD | 0.033 | −0.031 | −0.038 | −0.121 | 0.011 | 0.058 | 0.289 | 0.259 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yazdani, M.; Fiskådal, J.; Chen, X.; Utheim, Ø.A.; Ræder, S.; Vitelli, V.; Utheim, T.P. Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort. J. Clin. Med. 2021, 10, 884. https://doi.org/10.3390/jcm10040884
Yazdani M, Fiskådal J, Chen X, Utheim ØA, Ræder S, Vitelli V, Utheim TP. Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort. Journal of Clinical Medicine. 2021; 10(4):884. https://doi.org/10.3390/jcm10040884
Chicago/Turabian StyleYazdani, Mazyar, Jørgen Fiskådal, Xiangjun Chen, Øygunn A. Utheim, Sten Ræder, Valeria Vitelli, and Tor P. Utheim. 2021. "Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort" Journal of Clinical Medicine 10, no. 4: 884. https://doi.org/10.3390/jcm10040884
APA StyleYazdani, M., Fiskådal, J., Chen, X., Utheim, Ø. A., Ræder, S., Vitelli, V., & Utheim, T. P. (2021). Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort. Journal of Clinical Medicine, 10(4), 884. https://doi.org/10.3390/jcm10040884






