Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Participants
2.2. Data Collection
2.3. Statistical Analysis
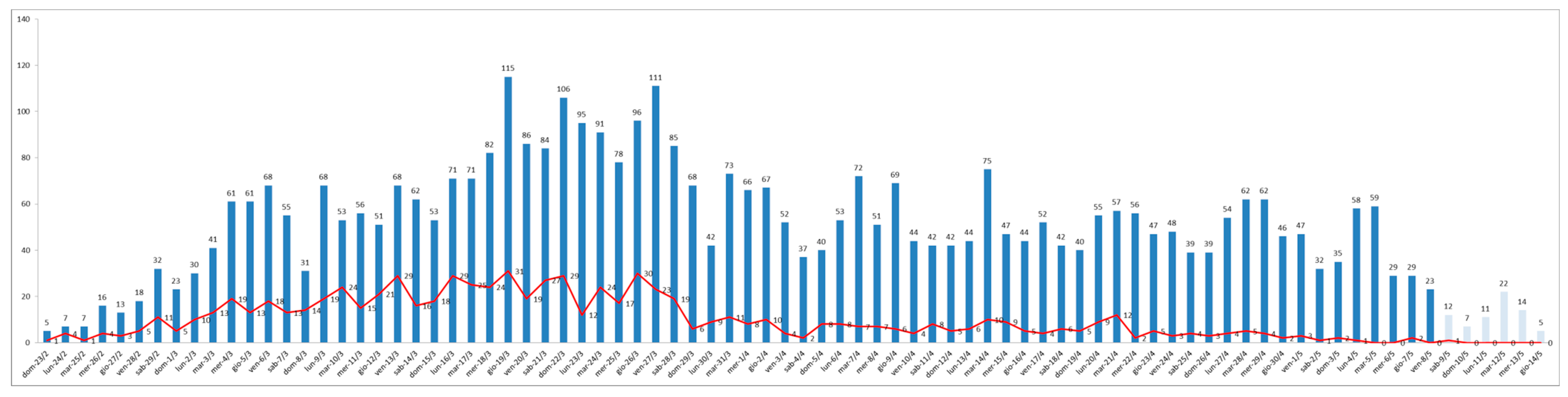
3. Results
4. Discussion
Future Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 4 February 2021).
- Her, M. Repurposing and reshaping of hospitals during the COVID-19 outbreak in South Korea. One Health 2020, 10, 100137. [Google Scholar] [CrossRef] [PubMed]
- Sen-Crowe, B.; Sutherland, M.; McKenney, M.; Elkbuli, A. A Closer Look into Global Hospital Beds Capacity and Resource Shortages During the COVID-19 Pandemic. J. Surg. Res. 2021, 260, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Mégarbane, B.; Bourasset, F.; Scherrmann, J.-M. Is Lockdown Effective in Limiting SARS-CoV-2 Epidemic Progression?—A Cross-Country Comparative Evaluation Using Epidemiokinetic Tools. J. Gen. Intern. Med. 2021, 1–7. [Google Scholar] [CrossRef]
- Kluge, H.H.P.; Wickramasinghe, K.; Rippin, H.L.; Mendes, R.; Peters, D.H.; Kontsevaya, A.; Breda, J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020, 395, 1678–1680. [Google Scholar] [CrossRef]
- Sheldon, T.A.; Wright, J. Twin epidemics of covid-19 and non-communicable disease. BMJ 2020, 369, m2618. [Google Scholar] [CrossRef]
- Palmer, K.; Monaco, A.; Kivipelto, M.; Onder, G.; Maggi, S.; Michel, J.-P.; Prieto, R.; Sykara, G.; Donde, S. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 2020, 32, 1189–1194. [Google Scholar] [CrossRef]
- Reno, C.; Lenzi, J.; Navarra, A.; Barelli, E.; Gori, D.; Lanza, A.; Valentini, R.; Tang, B.; Fantini, M.P. Forecasting COVID-19-Associated Hospitalizations under Different Levels of Social Distancing in Lombardy and Emilia-Romagna, Northern Italy: Results from an Extended SEIR Compartmental Model. J. Clin. Med. 2020, 9, 1492. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Sorbello, M.; El-Boghdadly, K.; Di Giacinto, I.; Cataldo, R.; Esposito, C.; Falcetta, S.; Merli, G.; Cortese, G.; Corso, R.M.; Bressan, F.; et al. The Italian coronavirus disease 2019 outbreak: Recommendations from clinical practice. Anaesthesia 2020, 75, 724–732. [Google Scholar] [CrossRef]
- Pecoraro, F.; Clemente, F.; Luzi, D. The efficiency in the ordinary hospital bed management in Italy: An in-depth analysis of intensive care unit in the areas affected by COVID-19 before the outbreak. PLoS ONE 2020, 15, e0239249. [Google Scholar] [CrossRef] [PubMed]
- Pasin, L.; Sella, N.; Correale, C.; Boscolo, A.; Rosi, P.; Saia, M.; Mantoan, D.; Navalesi, P. Regional COVID-19 Network for Coordination of SARS-CoV-2 outbreak in Veneto, Italy. J. Cardiothorac. Vasc. Anesthesia 2020, 34, 2341–2345. [Google Scholar] [CrossRef]
- OECD Health at a Glance 2019. Available online: http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm (accessed on 4 February 2021).
- Rhodes, A.; Ferdinande, P.; Flaatten, H.; Guidet, B.; Metnitz, P.G.; Moreno, R.P. The variability of critical care bed numbers in Europe. Intensiv. Care Med. 2012, 38, 1647–1653. [Google Scholar] [CrossRef]
- Meschi, T.; Rossi, S.; Volpi, A.; Ferrari, C.; Sverzellati, N.; Brianti, E.; Fabi, M.; Nouvenne, A.; Ticinesi, A. Reorganization of a large academic hospital to face COVID-19 outbreak: The model of Parma, Emilia-Romagna region, Italy. Eur. J. Clin. Investig. 2020, 50, e13250. [Google Scholar] [CrossRef] [PubMed]
- L’ospedale|Azienda Ospedaliero-Universitaria di Parma. Available online: https://www.ao.pr.it/chi-siamo/lospedale/ (accessed on 13 October 2020).
- Schede di Dimissione Ospedaliera—Salute. Available online: https://salute.regione.emilia-romagna.it/siseps/sanita/sdo (accessed on 13 October 2020).
- Pijls, B.G.; Jolani, S.; Atherley, A.; Derckx, R.T.; Dijkstra, J.I.R.; Franssen, G.H.L.; Hendriks, S.; Richters, A.; Venemans-Jellema, A.; Zalpuri, S.; et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open 2021, 11, e044640. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The Impact of the COVID-19 Pandemic on Hospital Admissions in The United States. Health Aff. 2020, 39, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. OUP accepted manuscript. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Metzler, B.; Siostrzonek, P.; Binder, R.K.; Bauer, A.; Reinstadler, S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: The pandemic response causes cardiac collateral damage. Eur. Heart J. 2020, 41, 1852–1853. [Google Scholar] [CrossRef]
- Markus, H.S.; Brainin, M. COVID-19 and stroke—A global World Stroke Organization perspective. Int. J. Stroke 2020, 15, 361–364. [Google Scholar] [CrossRef]
- Ebinger, J.E.; Shah, P.K. Declining Admissions for Acute Cardiovascular Illness: The Covid-19 Paradox. J. Am. Coll. Cardiol. 2020, 76, 289–291. [Google Scholar] [CrossRef]
- Schwarz, V.; Mahfoud, F.; Lauder, L.; Reith, W.; Behnke, S.; Smola, S.; Rissland, J.; Pfuhl, T.; Scheller, B.; Böhm, M.; et al. Decline of emergency admissions for cardiovascular and cerebrovascular events after the outbreak of COVID-19. Clin. Res. Cardiol. 2020, 1–7. [Google Scholar] [CrossRef]
- Baracchini, C.; Pieroni, A.; Viaro, F.; Cianci, V.; Cattelan, A.M.; Tiberio, I.; Munari, M.; Causin, F. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol. Sci. 2020, 41, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- Stöhr, E.; Aksoy, A.; Campbell, M.; Al Zaidi, M.; Öztürk, C.; Vorloeper, J.; Lange, J.; Sugiura, A.; Wilde, N.; Becher, M.U.; et al. Hospital admissions during Covid-19 lock-down in Germany: Differences in discretionary and unavoidable cardiovascular events. PLoS ONE 2020, 15, e0242653. [Google Scholar] [CrossRef]
- Niccoli, G.; Luescher, T.F.; Crea, F. Decreased myocardial infarction admissions during COVID times: What can we learn? Cardiovasc. Res. 2020, 116, e126–e128. [Google Scholar] [CrossRef] [PubMed]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef]
- Curigliano, G. How to Guarantee the Best of Care to Patients with Cancer During the COVID-19 Epidemic: The Italian Experience. Oncology 2020, 25, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Brandes, A.A.; Ardizzoni, A.; Artioli, F.; Cappuzzo, F.; Cavanna, L.; Frassineti, G.L.; Frassoldati, A.; Leonardi, F.; Longo, G.; Maestri, A.; et al. Fighting cancer in coronavirus disease era: Organization of work in medical oncology departments in Emilia Romagna region of Italy. Future Oncol. 2020, 16, 1433–1439. [Google Scholar] [CrossRef]
- Regione Emilia Romagna. COVID 19: Indicazioni Organizzative per le Reti Cliniche Integrate Ospedale-Territorio. Available online: https://salute.regione.emilia-romagna.it/assistenza-ospedaliera/covid-19-indicazioni-organizzative-per-le-reti-cliniche-integrate-ospedale-territorio (accessed on 13 October 2020).
- Baldi, E.; Savastano, S. Fear of Contagion: One of the Most Devious Enemies to Fight During the COVID-19 Pandemic. Disaster Med. Public Health Prep. 2020, 2020, 1–2. [Google Scholar] [CrossRef]
- Temesgen, Z.M.; DeSimone, D.C.; Mahmood, M.; Libertin, C.R.; Palraj, B.R.V.; Berbari, E.F. Health Care After the COVID-19 Pandemic and the Influence of Telemedicine. Mayo Clin. Proc. 2020, 95, S66–S68. [Google Scholar] [CrossRef]
- Omboni, S. Telemedicine During the COVID-19 in Italy: A Missed Opportunity? Telemed. e-Health 2020, 26, 973–975. [Google Scholar] [CrossRef] [PubMed]

| Year 2019 | Year 2020 | p-Value | COVID-19 2020 | Non-COVID-19 2020 | p-Value | |
|---|---|---|---|---|---|---|
| (n = 8656) | (n = 7938) | (n = 4160) | (n = 3778) | |||
| Age | ||||||
| Median (IQR) | 61 (33–78) | 64 (35–79) | <0.001 Ɨ | 73 (59–82) | 39 (11–71) | <0.001 Ɨ |
| Class | ||||||
| 0 | 717 (8.3%) | 831 (10.5%) | <0.001 | 44 (1.1%) | 787 (20.8%) | <0.001 |
| 1–17 | 753 (8.7%) | 356 (4.5%) | <0.001 | 132 (3.2%) | 224 (5.9%) | <0.001 |
| 18–39 | 1171 (13.5%) | 1075 (13.5%) | 0.99 | 180 (4.3%) | 895 (23.7%) | <0.001 |
| 40–64 | 2005 (23.2%) | 1701 (21.4%) | 0.007 | 1040 (25.0%) | 661 (17.5%) | <0.001 |
| 65–80 | 2090 (24.1%) | 1969 (24.8%) | 0.67 | 1337 (32.1%) | 632 (16.7%) | <0.001 |
| 80 + | 1919 (22.2%) | 1940 (24.4%) | <0.001 | 1361 (32.7%) | 579 (15.3%) | <0.001 |
| Sex | ||||||
| F | 4443 (51.3%) | 4023 (50.7%) | 0.41 | 1807 (43.4%) | 2216 (58.7%) | <0.001 |
| M | 4212 (48.7%) | 3915 (49.3%) | 0.41 | 2353 (56.6%) | 1562 (41.3%) | <0.001 |
| Comorbidities | ||||||
| Median (IQR) | 2 (1–4) | 4 (2–6) | <0.001 Ɨ | 4 (3–6) | 2 (1–4) | <0.001 Ɨ |
| Acute NCDs | ||||||
| Acute Myocardial Infarction | 230 (2.7%) | 152 (1.9%) | 0.002 | 73 (1.8%) | 79 (2.1%) | 0.32 |
| Cerebrovascular Disease (Stroke, TIA) | 566 (6.5%) | 331 (4.2%) | <0.001 | 178 (4.3%) | 153 (4.0%) | 0.65 |
| Chronic NCDs | ||||||
| Hypertension | 1420 (16.4%) | 1360 (17.1%) | 0.21 | 993 (23.9%) | 367 (9.7%) | <0.001 |
| Dementia | 409 (4.7%) | 328 (4.1%) | 0.07 | 253 (6.1%) | 75 (2.0%) | <0.001 |
| Chronic Respiratory Disease (COPD, Asthma) | 418 (4.8%) | 334 (4.2%) | 0.6 | 246 (5.9%) | 88 (2.3%) | <0.001 |
| Diabetes | 751 (8.7%) | 684 (8.6%) | 0.9 | 495 (11.9%) | 189 (5%) | <0.001 |
| Cancer | 1152 (13.3%) | 784 (9.9%) | <0.001 | 326 (7.8%) | 458 (12.1%) | <0.001 |
| Urgent surgical procedures | ||||||
| 257(3%) | 160(2%) | <0.001 | 82 (2%) | 78 (2.1%) | 0.8 | |
| Year 2019 | Year 2020 | p-value | COVID-19 2020 | Non-COVID-19 2020 | p-Value | |
|---|---|---|---|---|---|---|
| (n = 8656) | (n = 7938) | (n = 4160) | (n = 3778) | |||
| LOS—days, Mean (SD) | 8.3 (11.8) | 7.6 (10.0) | <0.001 § | 9.9 (10.2) | 5.2 (9.2) | <0.001 § |
| First access to ICU | 333 (3.8%) | 246 (3.1%) | 0.08 | 160 (3.8%) | 86 (2.3%) | <0.001 |
| Access to ICU at least once | 737 (8.5%) | 537 (6.8%) | <0.001 | 342 (8.2%) | 195 (5.2%) | <0.001 |
| LOS—days in ICU, Mean (SD) | 5.2 (8.7) | 7.9 (11.1) | <0.001 § | 9.9 (12.6) | 4.4(5.9) | <0.001 § |
| Deaths | 351 (4.1%) | 966 (12.2%) | <0.001 | 798 (19.2%) | 168 (4.4%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caminiti, C.; Maglietta, G.; Meschi, T.; Ticinesi, A.; Silva, M.; Sverzellati, N. Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. J. Clin. Med. 2021, 10, 880. https://doi.org/10.3390/jcm10040880
Caminiti C, Maglietta G, Meschi T, Ticinesi A, Silva M, Sverzellati N. Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. Journal of Clinical Medicine. 2021; 10(4):880. https://doi.org/10.3390/jcm10040880
Chicago/Turabian StyleCaminiti, Caterina, Giuseppe Maglietta, Tiziana Meschi, Andrea Ticinesi, Mario Silva, and Nicola Sverzellati. 2021. "Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study" Journal of Clinical Medicine 10, no. 4: 880. https://doi.org/10.3390/jcm10040880
APA StyleCaminiti, C., Maglietta, G., Meschi, T., Ticinesi, A., Silva, M., & Sverzellati, N. (2021). Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. Journal of Clinical Medicine, 10(4), 880. https://doi.org/10.3390/jcm10040880






