Assessing Problematic Social Media Use in Adolescents by Parental Ratings: Development and Validation of the Social Media Disorder Scale for Parents (SMDS-P)
Abstract
1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Problematic Social Media Use (PSMU)
2.2.2. Adolescent Usage Time, Emotional Dysregulation, and Academic Functioning
2.3. Statistical Analysis
2.3.1. Data Cleansing
2.3.2. Factor Structure
2.3.3. Internal Consistency
2.3.4. Criterion Validity
2.3.5. Sensitivity and Specificity
2.3.6. Accordance Rate
3. Results
3.1. Sample Description
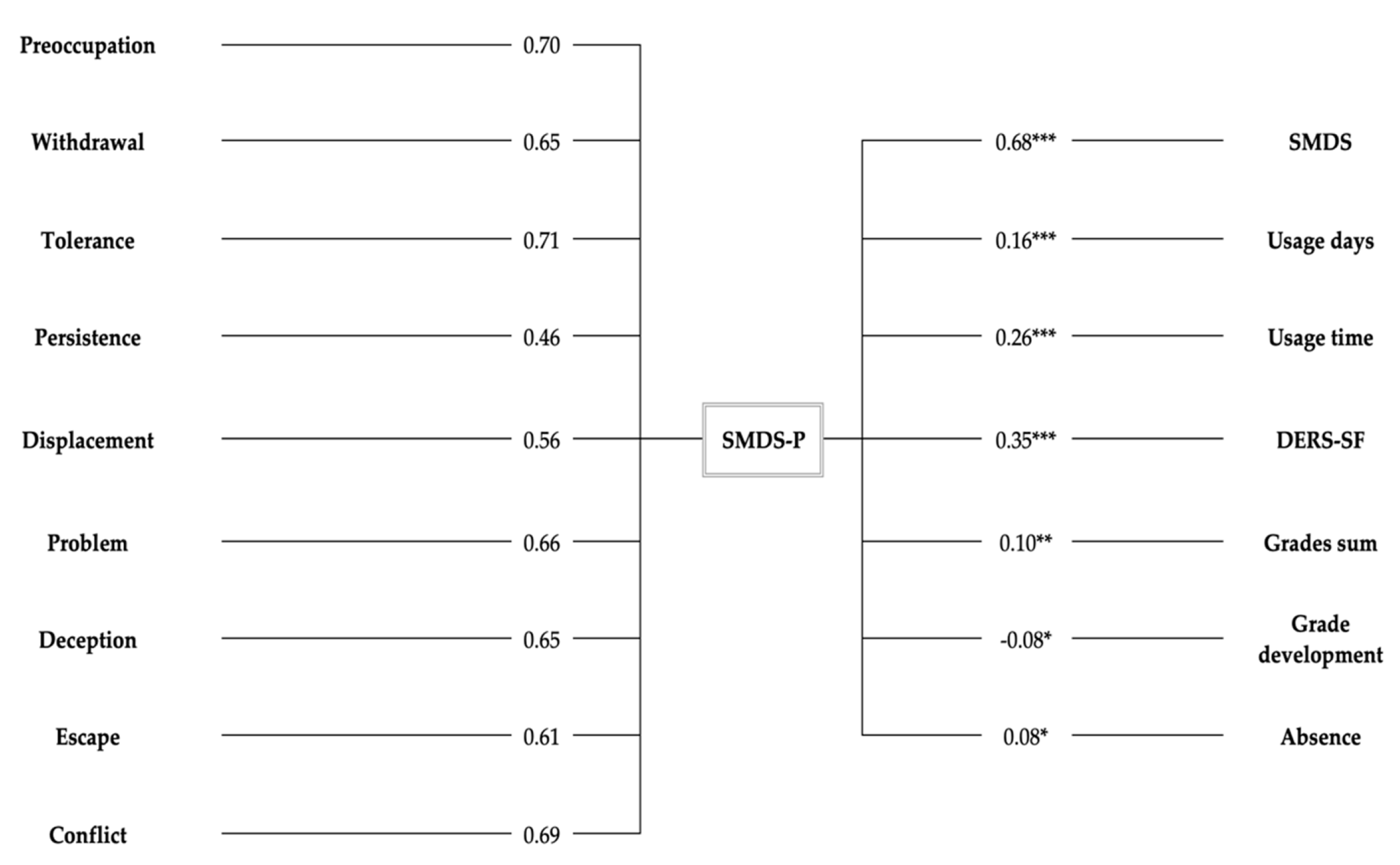
3.2. Factor Structure
3.3. Internal Consistency
3.4. Criterion Validity
3.5. Sensitivity and Specificity
3.6. Accordance Rate
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Paschke, K.; Austermann, M.I.; Simon-Kutscher, K.; Thomasius, R. Adolescent Gaming and Social Media Usage before and during the COVID-19 Pandemic. SUCHT 2021. manuscript accepted for publication. [Google Scholar] [CrossRef]
- Montag, C.; Lachmann, B.; Herrlich, M.; Zweig, K. Addictive Features of Social Media/Messenger Platforms and Freemium Games against the Background of Psychological and Economic Theories. Int. J. Environ. Res. Public Health 2019, 16, 2612. [Google Scholar] [CrossRef]
- Geier, C.F. Adolescent Cognitive Control and Reward Processing: Implications for Risk Taking and Substance Use. Addict. Behav. 2013, 64, 333–342. [Google Scholar] [CrossRef]
- Hussain, Z.; Griffiths, M.D. Problematic Social Networking Site Use and Comorbid Psychiatric Disorders: A Systematic Review of Recent Large-Scale Studies. Front. Psychiatry 2018, 9, 686. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Billieux, J.; Griffiths, M.D.; Kuss, D.J.; Demetrovics, Z.; Mazzoni, E.; Pallesen, S. The Relationship between Addictive Use of Social Media and Video Games and Symptoms of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. Psychol. Addict. Behav. 2016, 30, 252–262. [Google Scholar] [CrossRef]
- Choukas-Bradley, S.; Nesi, J.; Widman, L.; Galla, B.M. The Appearance-Related Social Media Consciousness Scale: Development and Validation with Adolescents. Body Image 2020, 33, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Marino, C.; Gini, G.; Angelini, F.; Vieno, A.; Spada, M.M. Social Norms and E-Motions in Problematic Social Media Use among Adolescents. Addict. Behav. 2020, 11, 100250. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P. Future Directions in Emotion Dysregulation and Youth Psychopathology. J. Clin. Child Adolesc. 2015, 44, 875–896. [Google Scholar] [CrossRef] [PubMed]
- van den Eijnden, R.; Koning, I.; Doornwaard, S.; van Gurp, F.; ter Bogt, T. The Impact of Heavy and Disordered Use of Games and Social Media on Adolescents’ Psychological, Social, and School Functioning. J. Behav. Addict. 2018, 7, 697–706. [Google Scholar] [CrossRef]
- Tsitsika, A.K.; Tzavela, E.C.; Janikian, M.; Ólafsson, K.; Iordache, A.; Schoenmakers, T.M.; Tzavara, C.; Richardson, C. Online Social Networking in Adolescence: Patterns of Use in Six European Countries and Links with Psychosocial Functioning. J. Adolesc. Health 2014, 55, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Sampasa-Kanyinga, H.; Chaput, J.-P.; Hamilton, H.A. Social Media Use, School Connectedness, and Academic Performance Among Adolescents. J. Prim. Prevent. 2019, 40, 189–211. [Google Scholar] [CrossRef] [PubMed]
- van den Eijnden, R.J.J.M.; Lemmens, J.S.; Valkenburg, P.M. The Social Media Disorder Scale. Comput. Hum. Behav. 2016, 61, 478–487. [Google Scholar] [CrossRef]
- Reer, F.; Festl, R.; Quandt, T. Investigating Problematic Social Media and Game Use in a Nationally Representative Sample of Adolescents and Younger Adults. BIT 2020, 1–14. [Google Scholar] [CrossRef]
- Yildiz Durak, H.; Seferoğlu, S.S. Modeling of Variables Related to Problematic Social Media Usage: Social Desirability Tendency Example. Scand. J. Psychol. 2019, 60, 277–288. [Google Scholar] [CrossRef]
- Brand, M.; Rumpf, H.-J.; Demetrovics, Z.; MÜller, A.; Stark, R.; King, D.L.; Goudriaan, A.E.; Mann, K.; Trotzke, P.; Fineberg, N.A.; et al. Which Conditions Should Be Considered as Disorders in the International Classification of Diseases (ICD-11) Designation of “Other Specified Disorders Due to Addictive Behaviors”? J. Behav. Addict. 2020. [Google Scholar] [CrossRef]
- da Veiga, G.F.; Sotero, L.; Pontes, H.M.; Cunha, D.; Portugal, A.; Relvas, A.P. Emerging Adults and Facebook Use: The Validation of the Bergen Facebook Addiction Scale (BFAS). Int. J. Ment. Health Addict. 2019, 17, 279–294. [Google Scholar] [CrossRef]
- Liu, C.; Ma, J. Development and Validation of the Chinese Social Media Addiction Scale. Pers. Individ. Differ. 2018, 134, 55–59. [Google Scholar] [CrossRef]
- Leung, H.; Pakpour, A.H.; Strong, C.; Lin, Y.-C.; Tsai, M.-C.; Griffiths, M.D.; Lin, C.-Y.; Chen, I.-H. Measurement Invariance across Young Adults from Hong Kong and Taiwan among Three Internet-Related Addiction Scales: Bergen Social Media Addiction Scale (BSMAS), Smartphone Application-Based Addiction Scale (SABAS), and Internet Gaming Disorder Scale-Short Form (IGDS-SF9) (Study Part A). Addict. Behav. 2020, 101, 105969. [Google Scholar] [CrossRef]
- Griffiths, M. A ‘Components’ Model of Addiction within a Biopsychosocial Framework. J. Subst. Use 2005, 10, 191–197. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Savci, M.; Ercengiz, M.; Aysan, F. Turkish Adaptation of Social Media Disorder Scale in Adolescents. Arch. Neuropsychiatr. 2017. [Google Scholar] [CrossRef] [PubMed]
- Fung, S. Cross-Cultural Validation of the Social Media Disorder Scale. PRBM 2019, 12, 683–690. [Google Scholar] [CrossRef]
- Boer, M.; van den Eijnden, R.J.J.M.; Boniel-Nissim, M.; Wong, S.-L.; Inchley, J.C.; Badura, P.; Craig, W.M.; Gobina, I.; Kleszczewska, D.; Klanšček, H.J.; et al. Adolescents’ Intense and Problematic Social Media Use and Their Well-Being in 29 Countries. J. Adolesc. Health 2020, 66, S89–S99. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.J.; Cauce, A.M. Predicting DSM-III-R Disorders from the Youth Self-Report: Analysis of Data from a Field Study. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Weil, L.G.; Fleming, S.M.; Dumontheil, I.; Kilford, E.J.; Weil, R.S.; Rees, G.; Dolan, R.J.; Blakemore, S.-J. The Development of Metacognitive Ability in Adolescence. Conscious. Cogn. 2013, 22, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhou, H.; Zhu, H. Working Memory, Executive Function and Impulsivity in Internet-Addictive Disorders: A Comparison with Pathological Gambling. Acta Neuropsychiatr. 2016, 28, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Duque, D.; Baird, J.A.; Posner, M.I. Executive Attention and Metacognitive Regulation. Conscious. Cogn. 2000, 9, 288–307. [Google Scholar] [CrossRef]
- Schneider, W. The Development of Metacognitive Knowledge in Children and Adolescents: Major Trends and Implications for Education. MBE 2008, 2, 114–121. [Google Scholar] [CrossRef]
- Moshagen, M.; Musch, J.; Ostapczuk, M.; Zhao, Z. Brief Report: Reducing Socially Desirable Responses in Epidemiologic Surveys: An Extension of the Randomized-Response Technique. Epidemiology 2010, 21, 379–382. [Google Scholar] [CrossRef]
- Verdejo-García, A.; Pérez-García, M. Substance Abusers’ Self-Awareness of the Neurobehavioral Consequences of Addiction. Psychiatry Res. 2008, 158, 172–180. [Google Scholar] [CrossRef]
- Swadi, H. Validating and Improving the Validity of Self-Reports in Adolescent Substance Misuse Surveys. J. Drug Issues 1990, 20, 473–486. [Google Scholar] [CrossRef]
- Jeong, H.; Yim, H.W.; Lee, S.-Y.; Lee, H.K.; Potenza, M.N.; Kwon, J.-H.; Koo, H.J.; Kweon, Y.-S.; Bhang, S.-Y.; Choi, J.-S. Discordance between Self-Report and Clinical Diagnosis of Internet Gaming Disorder in Adolescents. Sci. Rep. 2018, 8, 10084. [Google Scholar] [CrossRef]
- Larson, R.B. Controlling Social Desirability Bias. Int. J. Mark. Res. 2019, 61, 534–547. [Google Scholar] [CrossRef]
- Wartberg, L.; Zieglmeier, M.; Kammerl, R. Accordance of Adolescent and Parental Ratings of Internet Gaming Disorder and Their Associations with Psychosocial Aspects. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 264–270. [Google Scholar] [CrossRef]
- Vadlin, S.; Åslund, C.; Rehn, M.; Nilsson, K.W. Psychometric Evaluation of the Adolescent and Parent Versions of the Gaming Addiction Identification Test (GAIT). Scand. J. Psychol. 2015, 56, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Wartberg, L.; Kriston, L.; Kegel, K.; Thomasius, R. Adaptation and Psychometric Evaluation of the Young Diagnostic Questionnaire (YDQ) for Parental Assessment of Adolescent Problematic Internet Use. J. Behav. Addict. 2016, 5, 311–317. [Google Scholar] [CrossRef]
- Ok, C.; Lim, J. The Effect of Parental Demographics on Parental Assessment of Adolescent Internet Addiction. IJCBPL 2017, 7, 56–67. [Google Scholar] [CrossRef]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). JCM 2020, 9, 993. [Google Scholar] [CrossRef] [PubMed]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers by Parental Ratings: Development and Validation of the Gaming Disorder Scale for Parents (GADIS-P). J. Behav. Addict. 2021. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994; ISBN 978-0-07-047849-7. [Google Scholar]
- Kaufman, E.A.; Xia, M.; Fosco, G.; Yaptangco, M.; Skidmore, C.R.; Crowell, S.E. The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): Validation and Replication in Adolescent and Adult Samples. J. Psychopathol. Behav. Assess. 2016, 38, 443–455. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Kuhn, M.; Chow, F.; Wickham, H. Rsample: General Resampling Infrastructure. 2019. Available online: https://CRAN.R-project.org/package=rsample (accessed on 11 January 2020).
- Revelle, W. Psych: Procedures for Psychological, Psychometric, and Personality Research; Northwestern University: Evanston, IL, USA, 2018. [Google Scholar]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Kim, S.M.; Han, D.H.; Lee, Y.S.; Renshaw, P.F. Combined Cognitive Behavioral Therapy and Bupropion for the Treatment of Problematic On-Line Game Play in Adolescents with Major Depressive Disorder. Comput. Hum. Behav. 2012, 28, 1954–1959. [Google Scholar] [CrossRef]
- Muthén, B. A General Structural Equation Model with Dichotomous, Ordered Categorical, and Continuous Latent Variable Indicators. Psychometrika 1984, 49, 115–132. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modelling: Guidelines for Determining Model Fit. EJBRM 2008, 6, 53–60. [Google Scholar]
- Watkins, M.W. The Reliability of Multidimensional Neuropsychological Measures: From Alpha to Omega. Clin. Neuropsychol. 2017, 31, 1113–1126. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum Press: New Jersey, NJ, USA, 1988. [Google Scholar]
- Dancey, P.C.; Reidy, J. Statistics without Maths for Psychology, 5th ed.; Prentice Hall: Harlow, UK; New York, NY, USA, 2011; ISBN 978-0-273-72602-9. [Google Scholar]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.-C.; Müller, M. PROC: An Open-Source Package for R and S+ to Analyze and Compare ROC Curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Allgaier, A.-K. Diagnostische Güte von Testverfahren [Accuracy of diagnostic tests]. Psychother. Psychosom. Med. Psychol. 2014, 64, 86–87. [Google Scholar] [CrossRef] [PubMed]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar] [CrossRef]
- Cohen, J. The Effect Size Index: D. Stat. Power Anal. Behav. Sci. 1988, 2, 284–288. [Google Scholar]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Aebi, M.; Kuhn, C.; Banaschewski, T.; Grimmer, Y.; Poustka, L.; Steinhausen, H.-C.; Goodman, R. The Contribution of Parent and Youth Information to Identify Mental Health Disorders or Problems in Adolescents. Child Adolesc. Psychiatry Ment. Health 2017, 11, 23. [Google Scholar] [CrossRef] [PubMed]
- Konrad, K.; Firk, C.; Uhlhaas, P.J. Brain Development during Adolescence: Neuroscientific Insights into This Developmental Period. Dtsch. Arztebl. Int. 2013, 110, 425. [Google Scholar]
- Bányai, F.; Zsila, Á.; Király, O.; Maraz, A.; Elekes, Z.; Griffiths, M.D.; Andreassen, C.S.; Demetrovics, Z. Problematic Social Media Use: Results from a Large-Scale Nationally Representative Adolescent Sample. PLoS ONE 2017, 12, e0169839. [Google Scholar] [CrossRef]
- Chen, G.M. Why Do Women Bloggers Use Social Media? Recreation and Information Motivations Outweigh Engagement Motivations. New Media Soc. 2015, 17, 24–40. [Google Scholar] [CrossRef]
- Demetrovics, Z.; Urban, R.; Nagygyorgy, K.; Farkas, J.; Zilahy, D.; Mervo, B.; Reindl, A.; Agoston, C.; Kertesz, A.; Harmath, E. Why Do You Play? The Development of the Motives for Online Gaming Questionnaire (MOGQ). Behav. Res. Methods 2011, 43, 814–825. [Google Scholar] [CrossRef] [PubMed]
- Wartberg, L.; Kriston, L.; Thomasius, R. Internet Gaming Disorder and Problematic Social Media Use in a Representative Sample of German Adolescents: Prevalence Estimates, Comorbid Depressive Symptoms and Related Psychosocial Aspects. Comput. Hum. Behav. 2020, 103, 31–36. [Google Scholar] [CrossRef]
- Statista. Was Nutzt Du Bei YouTube Täglich Oder Mehrmals pro Woche? Available online: https://de.statista.com/statistik/daten/studie/497921/umfrage/nutzungsverhalten-von-youtube-bei-jugendlichen/ (accessed on 14 January 2021).
- Ng, Z.J.; Huebner, S.E.; Hills, K.J. Life Satisfaction and Academic Performance in Early Adolescents: Evidence for Reciprocal Association. J. Sch. Psychol. 2015, 53, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Scott, H.; Biello, S.M.; Woods, H.C. Social Media Use and Adolescent Sleep Patterns: Cross-Sectional Findings from the UK Millennium Cohort Study. BMJ Open 2019, 9, e031161. [Google Scholar] [CrossRef]
- Dewald, J.F.; Meijer, A.M.; Oort, F.J.; Kerkhof, G.A.; Bögels, S.M. The Influence of Sleep Quality, Sleep Duration and Sleepiness on School Performance in Children and Adolescents: A Meta-Analytic Review. Sleep Med. Rev. 2010, 14, 179–189. [Google Scholar] [CrossRef]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-Regulation Strategies across Psychopathology: A Meta-Analytic Review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Estévez, A.; Jáuregui, P.; Sánchez-Marcos, I.; López-González, H.; Griffiths, M.D. Attachment and Emotion Regulation in Substance Addictions and Behavioral Addictions. J. Behav. Addict. 2017, 6, 534–544. [Google Scholar] [CrossRef]
- Kökönyei, G.; Kocsel, N.; Király, O.; Griffiths, M.D.; Galambos, A.; Magi, A.; Paksi, B.; Demetrovics, Z. The Role of Cognitive Emotion Regulation Strategies in Problem Gaming Among Adolescents: A Nationally Representative Survey Study. Front. Psychiatry 2019, 10, 273. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). 2018. Available online: https://Icd.Who.Int/Browse11/l-m/En (accessed on 12 September 2020).
- Dalvi-Esfahani, M.; Niknafs, A.; Kuss, D.J.; Nilashi, M.; Afrough, S. Social Media Addiction: Applying the DEMATEL Approach. Telemat. Inform. 2019, 43, 101250. [Google Scholar] [CrossRef]
- Stockdale, L.A.; Coyne, S.M. Bored and Online: Reasons for Using Social Media, Problematic Social Networking Site Use, and Behavioral Outcomes across the Transition from Adolescence to Emerging Adulthood. J. Adolesc. 2020, 79, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Statista. Internetzugang in Deutschen Haushalten. Available online: https://de.statista.com/statistik/daten/studie/153257/umfrage/haushalte-mit-internetzugang-in-deutschland-seit-2002/ (accessed on 14 January 2021).
| Item | Criterion | During the Past Year, Has Your Son/Daughter… |
|---|---|---|
| 1 | Preoccupation | regularly found that he/she can’t think of anything else but the moment that he/she will be able to use social media again? |
| 2 | Withdrawal | often felt bad when he/she could not use social media? |
| 3 | Tolerance | regularly felt dissatisfied because he/she wanted to spend more time on social media? |
| 4 | Persistence | tried to spend less time on social media, but failed? |
| 5 | Displacement | regularly neglected other activities (e.g., hobbies, sport) because he/she wanted to use social media? |
| 6 | Problem | regularly had arguments with others because of his/her social media use? |
| 7 | Deception | regularly lied to you, your family, or friends about the amount of time he/she spend on social media? |
| 8 | Escape | often used social media to escape from negative feelings? |
| 9 | Conflict | had serious conflict with you, your partner, his/her brother(s) or sister(s) because of his/her social media use? |
| SDMS-P Item a | Factor Loadings | Communalities | |
|---|---|---|---|
| EFA | CFA | ||
| Item 1 | 0.70 | 0.87 | 0.48 |
| Item 2 | 0.65 | 0.88 | 0.42 |
| Item 3 | 0.71 | 0.81 | 0.50 |
| Item 4 | 0.46 | 0.67 | 0.21 |
| Item 5 | 0.56 | 0.72 | 0.32 |
| Item 6 | 0.66 | 0.73 | 0.44 |
| Item 7 | 0.65 | 0.84 | 0.42 |
| Item 8 | 0.61 | 0.76 | 0.37 |
| Item 9 | 0.69 | 0.83 | 0.48 |
| Variance Proportion b | 0.41 | ||
| SM Usage | Post Hoc Tests | |||
|---|---|---|---|---|
| Variables | Normal | Problematic | (χ2/Scheffé) | Cohen’s d/Cramer’s V |
| Absolute frequency | 782 | 179 | - | - |
| Relative frequency in % (95% CI) | 81.37 [83.84; 78.8] | 18.63 [16.16; 21.09] | - | - |
| Age mean (SE) | 13.45 (0.01) | 12.95 (0.16) | −0.5 ** | 0.21 |
| Female sex in % (95% CI) | 47.95 [44.45; 51.64] | 40.22 [33.04; 47.41] | - | - |
| SMDS-P sum score mean (SE) | 1.13 (0.05) | 6.77 (0.11) | 5.64 *** | 4.02 |
| SMDS sum score mean (SE) | 1.04 (0.06) | 4.31 (0.21) | 3.27 *** | 1.74 |
| Days of social media use per week mean (SE) | 6.01 (0.07) | 6.55 (0.11) | 0.54 *** | 0.3 |
| Minutes of social media use per day mean (SE) | 144.64 (8.6) | 207.33 (11.43) | 62.69 *** | 0.51 |
| DERS sum score mean (SE) | 38.76 (0.42) | 46.98 (0.96) | 8.22 *** | 0.69 |
| Days of absence mean (SE) | 1.67 (0.13) | 2.9 (0.44) | 1.23 *** | 0.3 |
| Grades sum mean (SE) | 6.18 (0.09) | 6.85 (0.2) | 0.67 ** | 0.27 |
| Grades development mean (SE) | 3.24 (0.02) | 3.08 (0.05) | −0.16 ** | 0.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Austermann, M.I.; Thomasius, R.; Paschke, K. Assessing Problematic Social Media Use in Adolescents by Parental Ratings: Development and Validation of the Social Media Disorder Scale for Parents (SMDS-P). J. Clin. Med. 2021, 10, 617. https://doi.org/10.3390/jcm10040617
Austermann MI, Thomasius R, Paschke K. Assessing Problematic Social Media Use in Adolescents by Parental Ratings: Development and Validation of the Social Media Disorder Scale for Parents (SMDS-P). Journal of Clinical Medicine. 2021; 10(4):617. https://doi.org/10.3390/jcm10040617
Chicago/Turabian StyleAustermann, Maria Isabella, Rainer Thomasius, and Kerstin Paschke. 2021. "Assessing Problematic Social Media Use in Adolescents by Parental Ratings: Development and Validation of the Social Media Disorder Scale for Parents (SMDS-P)" Journal of Clinical Medicine 10, no. 4: 617. https://doi.org/10.3390/jcm10040617
APA StyleAustermann, M. I., Thomasius, R., & Paschke, K. (2021). Assessing Problematic Social Media Use in Adolescents by Parental Ratings: Development and Validation of the Social Media Disorder Scale for Parents (SMDS-P). Journal of Clinical Medicine, 10(4), 617. https://doi.org/10.3390/jcm10040617






