Pseudothrombocytopenia—A Review on Causes, Occurrence and Clinical Implications
Abstract
1. Introduction
- (i)
- (ii)
- (iii)
- (iv)
- Fluorescence platelet counting can be effective in correcting spurious low PC [14];
- (v)
- (vi)
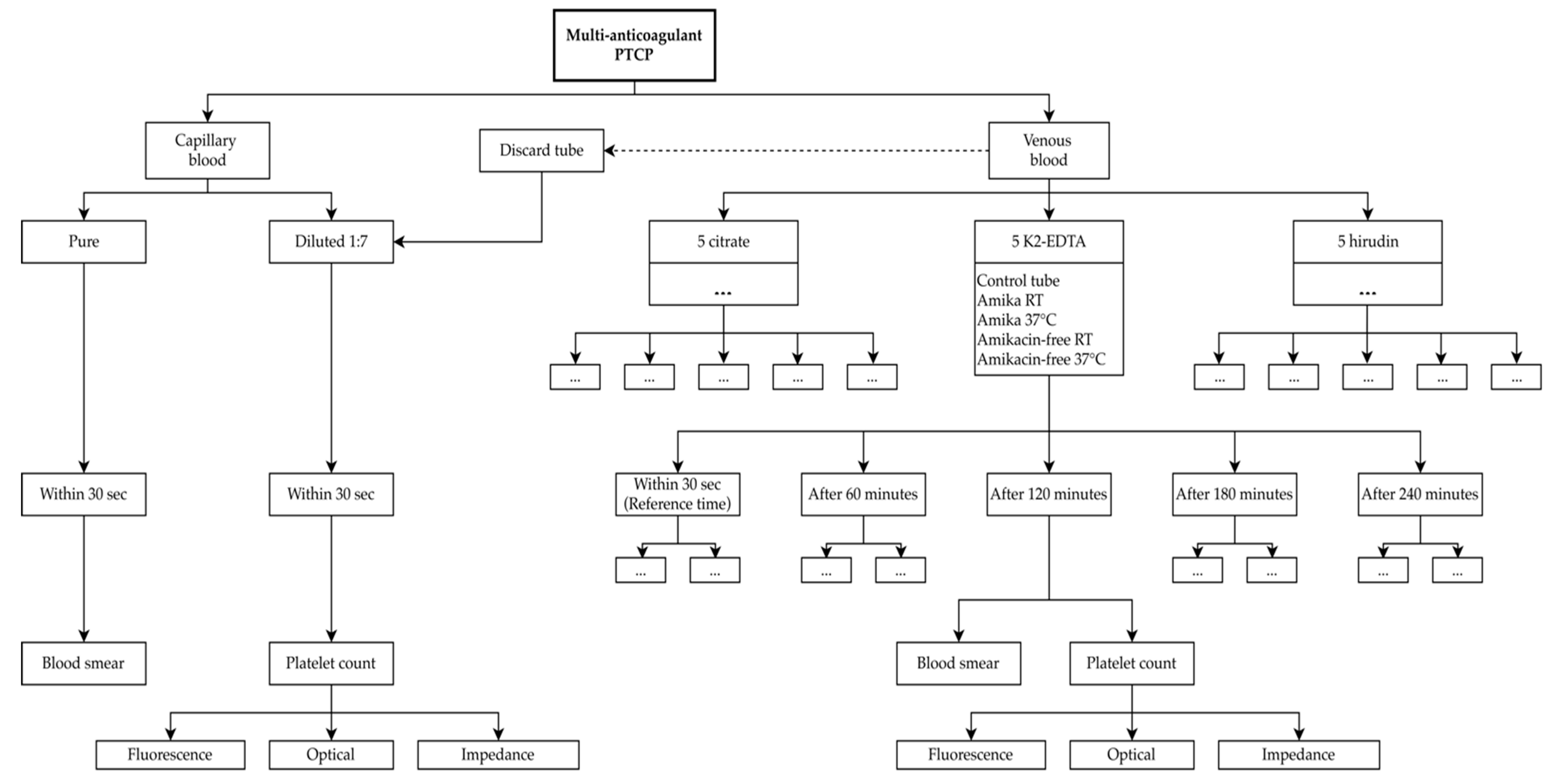
2. Case Study
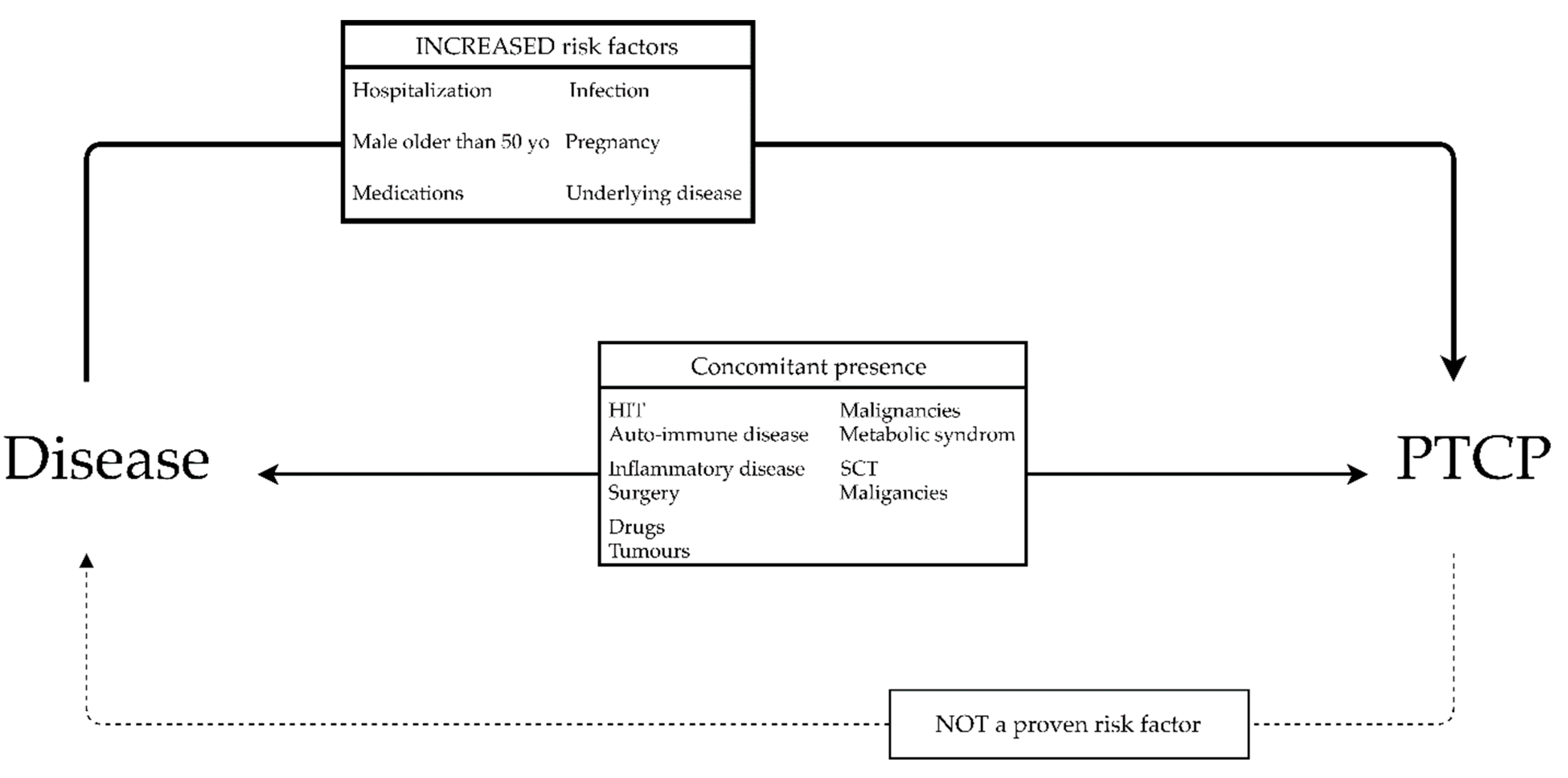
3. Mechanisms, Prevalence and Risk Factors
3.1. Mechanisms
3.2. Prevalence
3.3. Clinical Risk Factors
4. Pre-Analytical and Analytical Influencing Factors
4.1. Collection
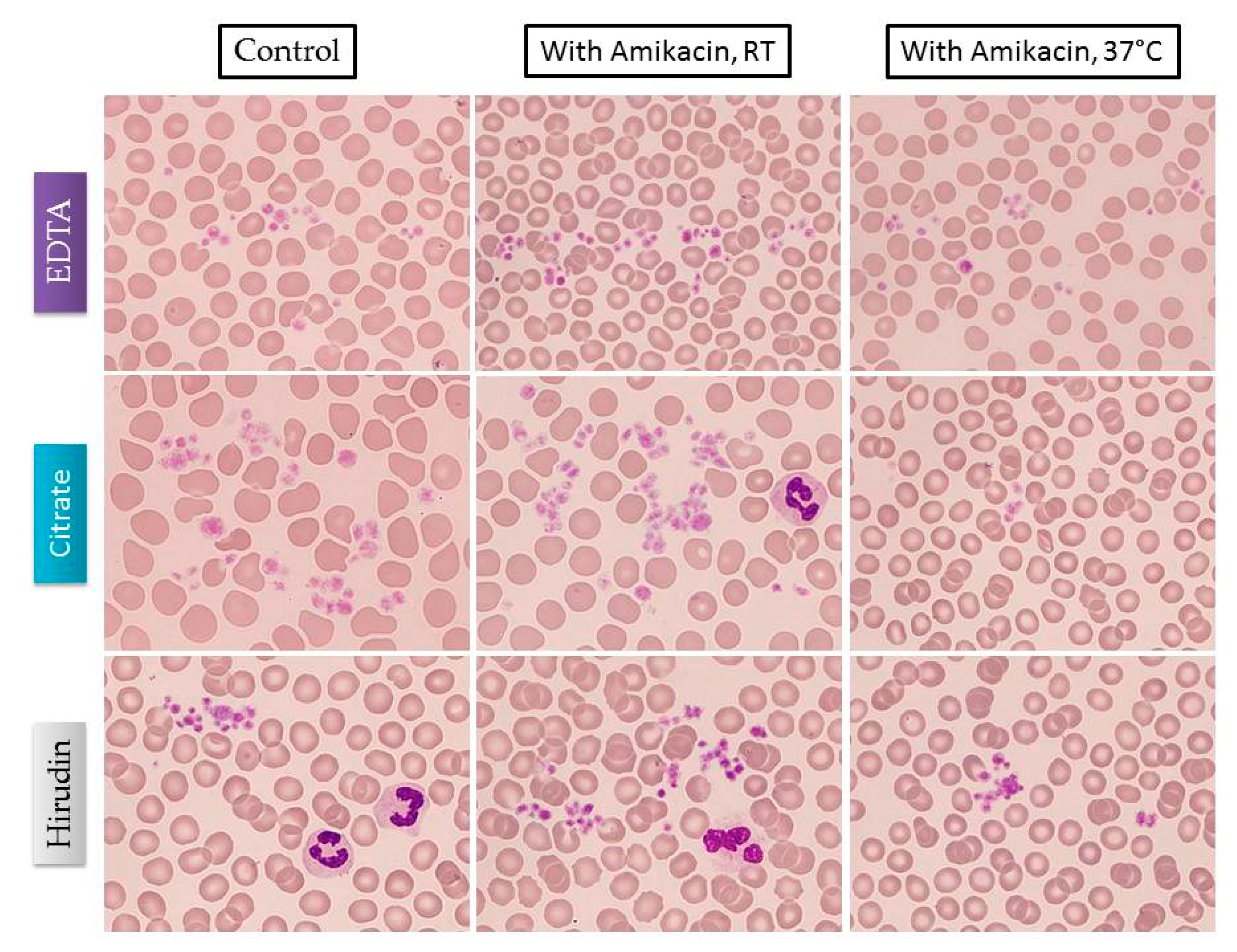
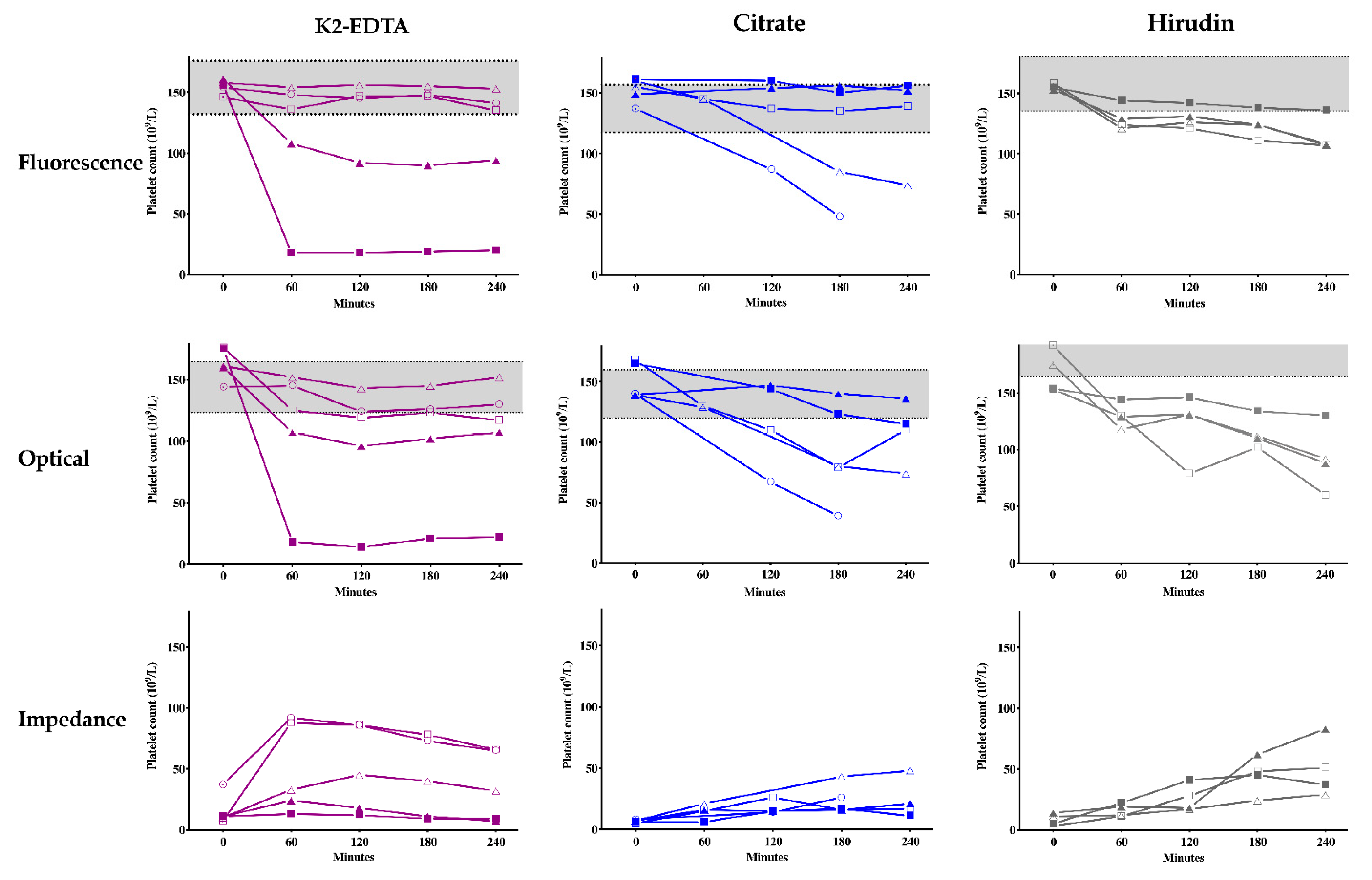
4.2. Aminoglycosides and Other Compounds
4.3. Temperature
4.4. Time
4.5. Analytical Techniques
4.6. Alternative Anticoagulants
5. Clinical Implications
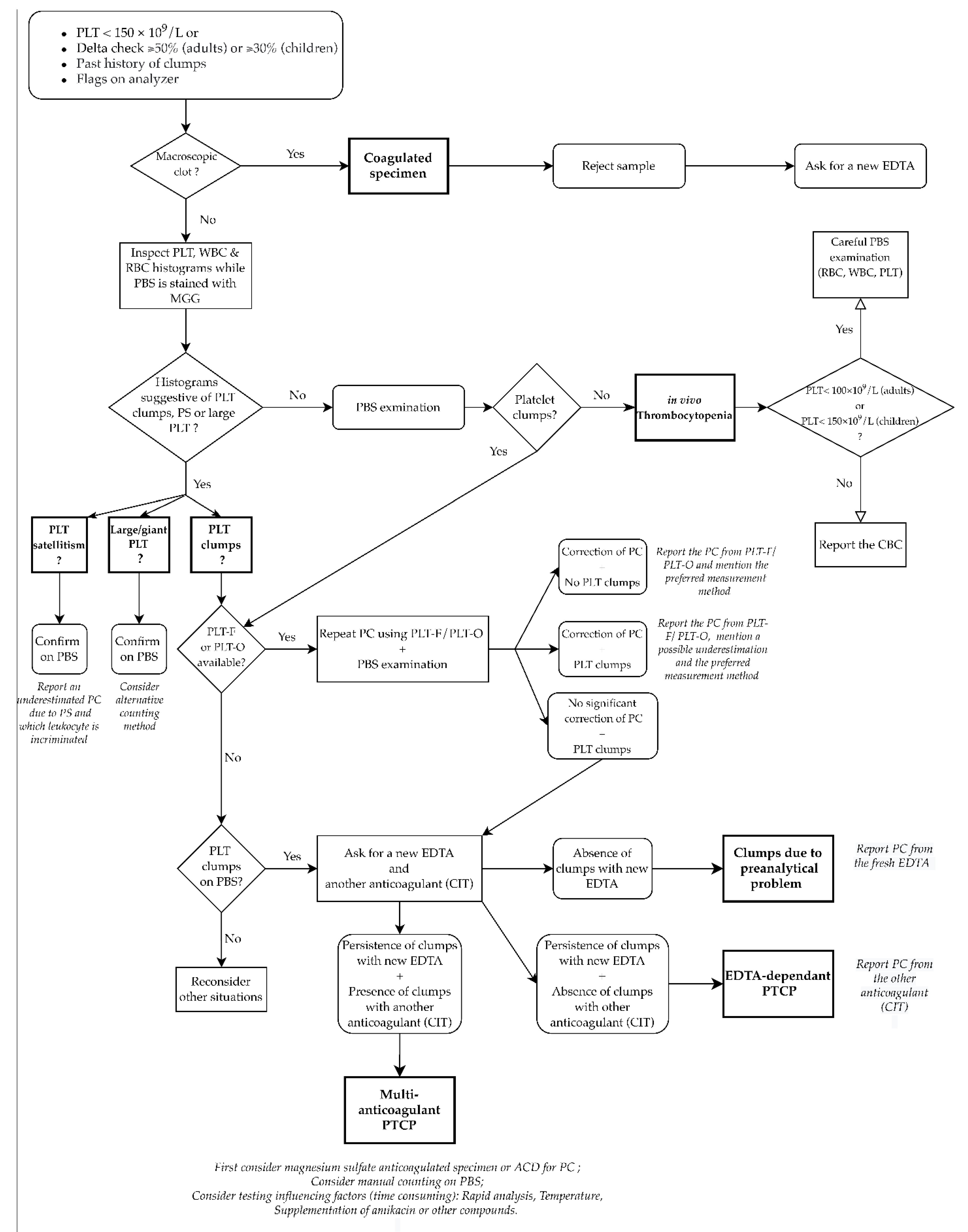
6. Management in the Laboratory and Practical Flowchart
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gowland, E.; Kay, H.E.M.; Spillman, J.C.; Williamson, J.R. Agglutination of platelets by a serum factor in the presence of EDTA. J. Clin. Pathol. 1969, 22, 460–464. [Google Scholar] [CrossRef]
- Li, H.; Wang, B.; Ning, L.; Luo, Y.; Xiang, S. Transient appearance of EDTA dependent pseudothrombocytopenia in a patient with 2019 novel coronavirus pneumonia. Platelets 2020, 31, 825–826. [Google Scholar] [CrossRef]
- Kuhlman, P.; Patrick, J.; Goodman, M. Pan-Pseudothrombocytopenia in COVID-19: A Harbinger for Lethal Arterial Thrombosis? Fed. Pract. 2020, 37, 354–368. [Google Scholar] [CrossRef]
- Baccini, V.; Geneviève, F.; Jacqmin, H.; Chatelain, B.; Girard, S.; Wuilleme, S.; Vedrenne, A.; Guiheneuf, E.; Toussaint-Hacquard, M.; Everaere, F.; et al. Platelet Counting: Ugly Traps and Good Advice. Proposals from the French-Speaking Cellular Hematology Group (GFHC). J. Clin. Med. 2020, 9, 808. [Google Scholar] [CrossRef]
- Chae, H.; Kim, M.; Lim, J.; Oh, E.-J.; Kim, Y.; Han, K. Novel method to dissociate platelet clumps in EDTA-dependent pseudothrombocytopenia based on the pathophysiological mechanism. Clin. Chem. Lab. Med. 2012, 50, 1387–1391. [Google Scholar] [CrossRef]
- Froom, P.; Barak, M. Prevalence and course of pseudothrombocytopenia in outpatients. Clin. Chem. Lab. Med. 2011, 49, 111–114. [Google Scholar] [CrossRef]
- Zandecki, M.; Genevieve, F.; Gerard, J.; Godon, A. Spurious counts and spurious results on haematology analysers: A review. Part I: Platelets. Clin. Lab. Haematol. 2007, 29, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, F.; Varga, M.; Pataki, Z.; Rigo, E. Pseudothrombocytopenia with multiple anticoagulant sample collection tubes. Interv. Med. Appl. Sci. 2016, 8, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Bokaei, P.B.; Grabovsky, D.; Shehata, N.; Wang, C. Impact of Amikacin on Pseudothrombocytopenia. Acta Haematol. 2017, 137, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Schuff-Werner, P.; Mansour, J.; Gropp, A. Pseudo-thrombocytopenia (PTCP). A challenge in the daily laboratory routine? LaboratoriumsMedizin 2020, 44, 295–304. [Google Scholar] [CrossRef]
- Ozcelik, F.; Oztosun, M.; Arslan, E.; Serdar, M.A.; Kurt, I.; Yiginer, O.; Kayadibi, H. A Useful Method for the Detection of Ethylenediaminetetraacetic Acid- and Cold Agglutinin-Dependent Pseudothrombocytopenia. Am. J. Med. Sci. 2012, 344, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Plebani, M. EDTA-dependent pseudothrombocytopenia: Further insights and recommendations for prevention of a clinically threatening artifact. Clin. Chem. Lab. Med. 2012, 50, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Luo, Y.; Yao, S.; Yan, M.; Li, J.; Ouyang, W.; Kuang, M. Discovery and Correction of Spurious Low Platelet Counts due to EDTA-Dependent Pseudothrombocytopenia: In Vitro Blood Anticoagulants Associated Pseudothrombocytopenia. J. Clin. Lab. Anal. 2015, 29, 419–426. [Google Scholar] [CrossRef]
- Bao, Y.; Wang, J.; Wang, A.; Bian, J.; Jin, Y. Correction of spurious low platelet counts by optical fluorescence platelet counting of BC-6800 hematology analyzer in EDTA-dependent pseudo thrombocytopenia patients. Transl. Cancer Res. 2020, 9, 166–172. [Google Scholar] [CrossRef]
- Tan, G.C.; Stalling, M.; Dennis, G.; Nunez, M.; Kahwash, S.B. Pseudothrombocytopenia due to Platelet Clumping: A Case Report and Brief Review of the Literature. Case Rep. Hematol. 2016, 2016, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Robertson, W.O. Drug-Imprint Coding. JAMA J. Am. Med. Assoc. 1974, 229, 766. [Google Scholar] [CrossRef]
- Mannuß, S.; Schuff-Werner, P.; Dreißiger, K.; Kohlschein, P. Magnesium Sulfate as an Alternative In Vitro Anticoagulant for the Measurement of Platelet Parameters? Am. J. Clin. Pathol. 2016, 145, 806–814. [Google Scholar] [CrossRef]
- Lombarts, A.J.P.F.; de Kieviet, W. Recognition and Prevention of Pseudothrombocytopenia and Concomitant Pseudoleukocytosis. Am. J. Clin. Pathol. 1988, 89, 634–639. [Google Scholar] [CrossRef]
- Robier, C.; Neubauer, M.; Sternad, H.; Rainer, F. Hirudin-induced pseudothrombocytopenia in a patient with EDTA-dependent platelet aggregation: Report of a new laboratory artefact. Int. J. Lab. Hematol. 2009, 32, 452–453. [Google Scholar] [CrossRef]
- Nagler, M.; Keller, P.; Siegrist, D.; Alberio, L. A case of EDTA-dependent pseudothrombocytopenia: Simple recognition of an underdiagnosed and misleading phenomenon. BMC Clin. Pathol. 2014, 14, 19. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Collection of Diagnostic Venous Blood Specimens; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2017; ISBN 978-1-56238-812-6. [Google Scholar]
- Notice: Information De L’utilisateur. Available online: bijsluiters.fagg-afmps.be/DownloadLeafletServlet?id=118724 (accessed on 1 December 2020).
- Fraser, C.G. Reference change values. Clin. Chem. Lab. Med. 2012, 50, 807–812. [Google Scholar] [CrossRef]
- Aarsand, A.K.; Fernandez-Calle, P.; Webster, C.; Coskun, A.; Gonzales-Lao, E.; Diaz-Garzon, J. The EFLM Biological Variation Data–Base. Available online: https://biologicalvariation.eu/ (accessed on 1 December 2020).
- Bain, B.J. Blood Cells: A Practical Guide, 5th ed.; Wiley Blackwell: Hoboken, NJ, USA, 2015; ISBN 978-1-118-81729-2. [Google Scholar]
- Wills, T.B.; Wardrop, K.J. Pseudothrombocytopenia Secondary to the Effects of EDTA in a Dog. J. Am. Anim. Hosp. Assoc. 2008, 44, 95–97. [Google Scholar] [CrossRef]
- Riond, B.; Waßmuth, A.K.; Hartnack, S.; Hofmann-Lehmann, R.; Lutz, H. Effective prevention of pseudothrombocytopenia in feline blood samples with the prostaglandin I2 analogue Iloprost. BMC Vet. Res. 2015, 11, 183. [Google Scholar] [CrossRef]
- Erkens, T.; Van den Sande, L.; Witters, J.; Verbraeken, F.; Looszova, A.; Feyen, B. Effect of time and temperature on anticoagulant-dependent pseudothrombocytopenia in Göttingen minipigs. Vet. Clin. Pathol. 2017, 46, 416–421. [Google Scholar] [CrossRef]
- Paltrinieri, S.; Paciletti, V.; Zambarbieri, J. Analytical variability of estimated platelet counts on canine blood smears. Vet. Clin. Pathol. 2018, 47, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Hübers, E.; Bauer, N.; Fey, K.; Moritz, A.; Roscher, K. Thrombopenie beim Pferd. Tierärztl. Prax. Ausg. G Großtiere Nutztiere 2018, 46, 73–79. [Google Scholar] [PubMed]
- Manthorpe, R.; Kofod, B.; Wiik, A.; Saxtrup, O.; Svehag, S.-E. Pseudothrombocytopenia: In Vitro Studies on the Underlying Mechanism. Scand. J. Haematol. 2009, 26, 385–392. [Google Scholar] [CrossRef]
- Pegels, J.G.; Bruynes, E.C.; Engelfriet, C.P.; von dem Borne, A.E. Pseudothrombocytopenia: An immunologic study on platelet antibodies dependent on ethylene diamine tetra-acetate. Blood 1982, 59, 157–161. [Google Scholar] [CrossRef]
- van Vliet, H.H.; Kappers-Klunne, M.C.; Abels, J. Pseudothrombocytopenia: A cold autoantibody against platelet glycoprotein GP IIb. Br. J. Haematol. 1986, 62, 501–511. [Google Scholar] [CrossRef]
- Payne, B.A. EDTA-induced pseudothrombocytopenia. Recognizing a laboratory artifact. Postgrad. Med. 1985, 77, 75–76. [Google Scholar] [CrossRef]
- Bizzaro, N. EDTA-dependent pseudothrombocytopenia: A clinical and epidemiological study of 112 cases, with 10-year follow-up. Am. J. Hematol. 1995, 50, 103–109. [Google Scholar] [CrossRef]
- Casonato, A.; Bertomoro, A.; Pontara, E.; Dannhauser, D.; Lazzaro, A.R.; Girolami, A. EDTA dependent pseudothrombocytopenia caused by antibodies against the cytoadhesive receptor of platelet gpIIB-IIIA. J. Clin. Pathol. 1994, 47, 625–630. [Google Scholar] [CrossRef]
- Bizzaro, N.; Brandalise, M. EDTA-dependent Pseudothrombocytopenia: Association with Antiplatelet and Antiphospholipid Antibodies. Am. J. Clin. Pathol. 1995, 103, 103–107. [Google Scholar] [CrossRef]
- Isik, A.; Balcik, O.S.; Akdeniz, D.; Cipil, H.; Uysal, S.; Kosar, A. Relationship Between Some Clinical Situations, Autoantibodies, and Pseudothrombocytopenia. Clin. Appl. Thromb. 2012, 18, 645–649. [Google Scholar] [CrossRef]
- Bai, M.; Feng, J.; Liang, G. Transient EDTA-Dependent Pseudothrombocytopenia Phenomenon in a Patient with Antiphospholipid Syndrome. Clin. Lab. 2018, 64, 1581–1583. [Google Scholar] [CrossRef]
- Kurata, Y.; Hayashi, S.; Jouzaki, K.; Konishi, I.; Kashiwagi, H.; Tomiyama, Y. Four cases of pseudothrombocytopenia due to platelet cold agglutinins. Rinsho Ketsueki 2006, 47, 781–786. [Google Scholar]
- Balcik, O.S.; Akdeniz, D.; Cipil, H.; Uysal, S.; Isik, A.; Kosar, A. Heparin Platelet Factor 4 Antibody Positivity in Pseudothrombocytopenia. Clin. Appl. Thromb. 2012, 18, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Veenhoven, W.A.; Van Der Schans, G.S.; Huiges, W.; Metting-Scherphuis, H.E.; Halie, M.R.; Nieweg, H.O. Pseudothrombocytopenia Due to Agglutinins. Am. J. Clin. Pathol. 1979, 72, 1005–1008. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Guiu, I.; Martínez-Martinez, I.; Martínez, C.; Navarro-Fernandez, J.; Garcia-Candel, F.; Ferrer-Marín, F.; Vicente, V.; Watson, S.; Andrews, R.; Gardiner, E.; et al. An atypical IgM class platelet cold agglutinin induces GPVI-dependent aggregation of human platelets. Thromb. Haemost. 2015, 114, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Banfi, G.; Salvagno, G.L.; Lippi, G. The role of ethylenediamine tetraacetic acid (EDTA) as in vitro anticoagulant for diagnostic purposes. Clin. Chem. Lab. Med. 2007, 45, 565–576. [Google Scholar] [CrossRef]
- Dabadie, M.; Valli, N.; Jacobin, M.-J.; Laroche-Traineau, J.; Barat, J.-L.; Ducassou, D.; Nurden, A.T.; Clofent-Sanchez, G. Characterisation, cloning and sequencing of a conformation-dependent monoclonal antibody to the α IIb β 3 integrin: Interest for use in thrombus detection. Platelets 2001, 12, 395–405. [Google Scholar] [CrossRef]
- Bowen, R.A.R.; Remaley, A.T. Interferences from blood collection tube components on clinical chemistry assays. Biochem. Medica 2014, 24, 31–44. [Google Scholar] [CrossRef]
- Golański, J.; Pietrucha, T.; Baj, Z.; Greger, J.; Watala, C. A novel approach to inhibit the anticoagulant-induced spontaneous activation of blood platelets - effect of magnesium on platelet release reaction in whole blood. Thromb. Res. 1997, 85, 127–132. [Google Scholar] [CrossRef]
- Onder, O.; Weinstein, A.; Hoyer, L.W. Pseudothrombocytopenia caused by platelet agglutinins that are reactive in blood anticoagulated with chelating agents. Blood 1980, 56, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Chadha, J.; Ameri, A. A Curious Case of Pseudothrombocytopenia due to In Vitro Agglutination. Case Rep. Hematol. 2020, 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Wu, X.; Deng, W.; Li, J.; Luo, W. Amikacin Can Be Added to Blood to Reduce the Fall in Platelet Count. Am. J. Clin. Pathol. 2011, 136, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Nakanishi, K.; Maruta, T.; Takenaka, D.; Hirota, S.; Matsumoto, S.; Saigo, K.; Ohno, Y.; Fujii, M.; Sugimura, K. Anticoagulant-Induced Pseudothrombocytopenia Occurring after Transcatheter Arterial Embolization for Hepatocellular Carcinoma. Jpn. J. Clin. Oncol. 2006, 36, 527–531. [Google Scholar] [CrossRef]
- Albersen, A.; Porcelijn, L.; Schilders, J.; Zuetenhorst, H.; Njo, T.; Hamberg, P. Sunitinib-associated pseudothrombocytopenia induced by IgM antibody. Platelets 2013, 24, 566–570. [Google Scholar] [CrossRef]
- Chiurazzi, F.; Villa, M.R.; Rotoli, B. Transplacental transmission of EDTA-dependent pseudothrombocytopenia. Haematologica 1999, 84, 664. [Google Scholar]
- Korterink, J.J.; Boersma, B.; Schoorl, M.; Porcelijn, L.; Bartels, P.C.M. Pseudothrombocytopenia in a neonate due to mother? Eur. J. Pediatr. 2013, 172, 987–989. [Google Scholar] [CrossRef]
- Ohno, N.; Kobayashi, M.; Hayakawa, S.; Utsunomiya, A.; Karakawa, S. Transient pseudothrombocytopenia in a neonate: Transmission of a maternal EDTA-dependent anticoagulant. Platelets 2012, 23, 399–400. [Google Scholar] [CrossRef]
- Christensen, R.D. Pseudothrombocytopenia in a Preterm Neonate. Pediatrics 2004, 114, 273–275. [Google Scholar] [CrossRef]
- Rajajee, S.; Subbiah, E.; Krishnamurthy, N.; Paranjothi, S.; Lohiya, N. Pseudothrombocytopenia and Usefulness of Platelet Aggregates in Peripheral Smear in the Diagnosis of Scrub Typhus. Indian J. Pediatr. 2019, 86, 93–94. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.K.; Robertson, R.; Nagaoka, G.; Ong, E.; Petz, L.; Stiehm, E.R. Pseudothrombocytopenia in a child with the acquired immunodeficiency syndrome. West. J. Med. 1992, 157, 668–670. [Google Scholar] [PubMed]
- Hsieh, A.T.; Chao, T.Y.; Chen, Y.C. Pseudothrombocytopenia associated with infectious mononucleosis. Arch. Pathol. Lab. Med. 2003, 127, e17–e18. [Google Scholar] [CrossRef]
- Vaidya, P.; Venkataraman, R. Pseudothrombocytopenia in a child with Dengue. Indian J. Pediatr. 2014, 81, 1395–1396. [Google Scholar] [CrossRef] [PubMed]
- Igala, M.; Kouégnigan Rerambiah, L.; Ledaga Lentombo, L.E.; Ifoudji Makao, A.; Nto’o Eyene, S.; Mbiye Cheme, S.W.; Bouyou Akotet, M.; Boguikouma, J.B. Anticoagulant-induced pseudothrombocytopenia after a plasmodium falciparum infection in a five-year-old child. Med. Sante Trop. 2019, 29, 175–177. [Google Scholar]
- Akbayram, S.; Dogan, M.; Akgun, C.; Caksen, H.; Oner, A.F. EDTA-Dependent Pseudothrombocytopenia in a Child. Clin. Appl. Thromb. 2011, 17, 494–496. [Google Scholar] [CrossRef]
- Lopez-Molina, M.; Sorigue, M.; Martinez-Iribarren, A.; Orna Montero, E.; Tejedor Ganduxé, X.; Leis Sestayo, A.; Sala Sanjaume, M.A.; Llopis Díaz, M.-A.; Morales-Indiano, C. Platelet satellitism around lymphocytes: Case report and literature review. Int. J. Lab. Hematol. 2019, 41, e81–e83. [Google Scholar] [CrossRef]
- Bizzaro, N.; Goldschmeding, R. Platelet Satellitism Is Fc Y RIII (CD 16) Receptor-Mediated. Am. J. Clin. Pathol. 1995, 103, 740–744. [Google Scholar] [CrossRef]
- Christopoulos, C.; Mattock, C. Platelet satellitism and ox granule proteins. J. Clin. Pathol. 1991, 44, 788–789. [Google Scholar] [CrossRef]
- Bartels, P.C.M.; Schoorl, M.; Lombarts, A.J.P.F. Screening for EDTA-dependent deviations in platelet counts and abnormalities in platelet distribution histograms in pseudothrombocytopenia. Scand. J. Clin. Lab. Investig. 1997, 57, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Vicari, A.; Banfi, G.; Bonini, P.A. EDTA-dependent pseudothrombocytopaenia: A 12-month epidemiological study. Scand. J. Clin. Lab. Investig. 1988, 48, 537–542. [Google Scholar] [CrossRef]
- García Suárez, J.; Merino, J.L.; Rodríguez, M.; Velasco, A.; Moreno, M.C. [Pseudothrombocytopenia: Incidence, causes and methods of detection]. Sangre 1991, 36, 197–200. [Google Scholar] [PubMed]
- Sakurai, S.; Shiojima, I.; Tanigawa, T.; Nakahara, K. Aminoglycosides prevent and dissociate the aggregation of platelets in patients with EDTA-dependent pseudothrombocytopenia. Br. J. Haematol. 1997, 99, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Fujii, H.; Watada, M.; Yamamoto, K.; Kanoh, T. [Seventeen cases of pseudothrombocytopenia, with special reference to the clinical problems, its pathogenesis and significance (author’s transl)]. Nihon Ketsueki Gakkai Zasshi J. Jpn. Haematol. Soc. 1978, 41, 523–532. [Google Scholar]
- Savage, R.A. Pseudoleukocytosis Due to EDTA-induced Platelet Clumping. Am. J. Clin. Pathol. 1984, 81, 317–322. [Google Scholar] [CrossRef]
- Xiao, Y.; Yu, S.; Xu, Y. The Prevalence and Biochemical Profiles of EDTA-Dependent Pseudothrombocytopenia in a Generally Healthy Population. Acta Haematol. 2015, 134, 177–180. [Google Scholar] [CrossRef]
- Lewinski, U.H.; Cycowitz, Z.; Cohen, A.M.; Gardyn, J.; Mittelman, M. The incidence of pseudothrombocytopenia in automatic blood analyzers. Haematologia 2000, 30, 117–121. [Google Scholar]
- Silvestri, F.; Virgolini, L.; Savignano, C.; Zaja, F.; Velisig, M.; Baccarani, M. Incidence and Diagnosis of EDTA-Dependent Pseudothrombocytopenia in a Consecutive Outpatient Population Referred for Isolated Thrombocytopenia. Vox Sang. 1995, 68, 35–39. [Google Scholar] [CrossRef]
- Tomicic, M.; Vuk, T.; Gulan-Harcet, J. Anticoagulant-induced pseudothrombocytopenia in blood donors: Letter to the Editor. Transfus. Med. 2015, 25, 47–48. [Google Scholar] [CrossRef] [PubMed]
- Maslanka, K.; Marciniak-Bielak, D.; Szczepinski, A. Pseudothrombocytopenia in blood donors. Vox Sang. 2008, 95, 349. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, J.; Holme, S.; Heaton, W.; Campbell, D.; Bowen, M. Pseudothrombocytopenia in plateletpheresis donors. Transfusion 1995, 35, 46–49. [Google Scholar] [CrossRef] [PubMed]
- Lazo-Langner, A.; Piedras, J.; Romero-Lagarza, P.; Lome-Maldonado, C.; Sánchez-Guerrero, J.; López-Karpovitch, X. Platelet satellitism, spurious neutropenia, and cutaneous vasculitis: Casual or causal association?: Case Report: Satellitism and Cutaneous Vasculitis. Am. J. Hematol. 2002, 70, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Choe, W.-H.; Cho, Y.-U.; Chae, J.-D.; Kim, S.-H. Pseudothrombocytopenia or platelet clumping as a possible cause of low platelet count in patients with viral infection: A case series from single institution focusing on hepatitis A virus infection. Int. J. Lab. Hematol. 2013, 35, 70–76. [Google Scholar] [CrossRef]
- Shi, X.; Lin, Z.; He, L.; Li, W.; Mo, L.; Li, Y.; Yang, Z.; Mo, W.-N. Transient appearance of EDTA-dependent pseudothrombocytopenia in a postoperative patient with sepsis: A case report. Medicine 2017, 96, e6330. [Google Scholar] [CrossRef]
- Zimrin, A.B.; Warkentin, T.E. Transient pseudothrombocytopenia associated with immune heparin-induced thrombocytopenia complicated by pulmonary embolism. Thromb. Haemost. 2013, 109, 971–973. [Google Scholar] [CrossRef]
- Martin-Toutain, I.; Settegrana, C.; Ankri, A. High levels of heparin-platelet factor 4 antibodies in patients with pseudothrombocytopenia: Risk of misdiagnosis. J. Thromb. Haemost. 2009, 7, 1416–1418. [Google Scholar] [CrossRef]
- Berkman, N.; Michaeli, Y.; Or, R.; Eldor, A. EDTA-dependent pseudothrombocytopenia: A clinical study of 18 patients and a review of the literature. Am. J. Hematol. 1991, 36, 195–201. [Google Scholar] [CrossRef]
- Matarazzo, M.; Conturso, V.; Di Martino, M.; Chiurazzi, F.; Guida, G.; Morante, R. EDTA-dependent pseudothrombocytopenia in a case of liver cirrhosis. Panminerva Med. 2000, 42, 155–157. [Google Scholar]
- Sahin, C.; Kırlı, I.; Sozen, H.; Canbek, T.D. EDTA-induced pseudothrombocytopenia in association with bladder cancer. BMJ Case Rep. 2014, 2014, bcr2014205130. [Google Scholar] [CrossRef]
- Kim, H.J.; Moh, I.H.; Yoo, H.; Son, S.; Jung, D.H.; Lee, H.G.; Han, D.H.; Park, J.H.; Kim, H.S.; Kim, J.H. Ethylenediaminetetraacetic acid-dependent pseudothrombocytopenia associated with neuroendocrine carcinoma: A case report. Oncol. Lett. 2012, 4, 86–88. [Google Scholar] [CrossRef]
- Dalamangas, C.; Slaughter, T.F. Ethylenediaminetetraacetic Acid-Dependent Pseudothrombocytopenia in a Cardiac Surgical Patient. Anesth. Analg. 1998, 86, 1210–1211. [Google Scholar]
- Wenzel, F.; Lasshofer, R.; Rox, J.; Fischer, J.; Giers, G. Transient appearance of postoperative EDTA-dependent pseudothrombocytopenia in a patient after gastrectomy. Platelets 2011, 22, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.K.; Shah, R.; Petko, M.; Keogh, B.E. Pseudothrombocytopenia in cardiac surgical practice. Interact. Cardiovasc. Thorac. Surg. 2007, 6, 565–566. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Di Francesco, A.; Pasanisi, A.; Tsamesidis, I.; Podda, L.; Fozza, C. Pseudo-thrombocytopenia after autologous stem cell transplantation. Blood Coagul. Fibrinolysis 2019, 30, 66–67. [Google Scholar] [CrossRef] [PubMed]
- Deeren, D.; Van Haute, I. Is pseudothrombocytopenia transmitted from hematopoietic stem cell donor to recipient?: Pseudothrombocytopenia in a Stem Cell Donor. J. Clin. Apher. 2014, 29, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Beyan, C.; Kaptan, K.; Ifran, A. Pseudothrombocytopenia after changing insulin therapy in a case with insulin-dependent diabetes mellitus: A first case report. Am. J. Hematol. 2010, 85, 909–910. [Google Scholar] [CrossRef] [PubMed]
- Sane, D.C.; Damaraju, L.V.; Topol, E.J.; Cabot, C.F.; Mascelli, M.A.; Harrington, R.A.; Simoons, M.L.; Califf, R.M. Occurrence and clinical significance of pseudothrombocytopenia during abciximab therapy. J. Am. Coll. Cardiol. 2000, 36, 75–83. [Google Scholar] [CrossRef]
- Krukowska, K.; Kieszko, R.; Kurek, K.; Chmielewska, I.; Krawczyk, P.; Milanowski, J. An Episode of Pseudothrombocytopenia during Pembrolizumab Therapy in NSCLC Patient. Case Rep. Oncol. Med. 2020, 2020, 1–4. [Google Scholar] [CrossRef]
- Vidranski, V.; Laskaj, R.; Sikiric, D.; Skerk, V. Platelet satellitism in infectious disease? Biochem. Medica 2015, 25, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Kocum, T.H.; Katircibasi, T.M.; Sezgin, A.T.; Atalay, H. An unusual cause of mismanagement in an acute myocardial infarction case: Pseudothrombocytopenia. Am. J. Emerg. Med. 2008, 26, 740.e1–740.e2. [Google Scholar] [CrossRef] [PubMed]
- Bizzaro, N. Platelet Cold Agglutinins and Cardiac Surgery Hypothermia. Am. J. Hematol. 1999, 60, 80–85. [Google Scholar] [CrossRef]
- Greinacher, A.; Selleng, S. How I evaluate and treat thrombocytopenia in the intensive care unit patient. Blood 2016, 128, 3032–3042. [Google Scholar] [CrossRef]
- Ahn, H.L.; Jo, Y.I.; Choi, Y.S.; Lee, J.Y.; Lee, H.W.; Kim, S.R.; Sim, J.; Lee, W.; Jin, C.J. EDTA—dependent Pseudothrombocytopenia Confirmed by Supplementation of Kanamycin; A Case Report. Korean J. Intern. Med. 2002, 17, 65–68. [Google Scholar] [CrossRef]
- Lombarts, A.J.P.F.; Zijlstra, J.J.; Peters, R.H.M.; Thomasson, C.G.; Franck, P.F.H. Accurate Platelet Counting in an Insidious Case of Pseudothrombocytopenia. Clin. Chem. Lab. Med. 1999, 37, 1063–1066. [Google Scholar] [CrossRef]
- Schuff-Werner, P.; Steiner, M.; Fenger, S.; Gross, H.-J.; Bierlich, A.; Dreissiger, K.; Mannuß, S.; Siegert, G.; Bachem, M.; Kohlschein, P. Effective estimation of correct platelet counts in pseudothrombocytopenia using an alternative anticoagulant based on magnesium salt. Br. J. Haematol. 2013, 162, 684–692. [Google Scholar] [CrossRef]
- van der Meer, W.; Allebes, W.; Simon, A.; van Berkel, Y.; de Keijzer, M.H. Pseudothrombocytopenia: A report of a new method to count platelets in a patient with EDTA- and temperature-independent antibodies of the IgM type. Eur. J. Haematol. 2002, 69, 243–247. [Google Scholar] [CrossRef]
- Asma, A.; Anissa, S.; Touhami, K. Aggregation kinetic and temperature optimum of an EDTA-dependent pseudothrombocytopenia. Clin. Chem. Lab. Med. CCLM 2020, 59, e31–e33. [Google Scholar] [CrossRef] [PubMed]
- Salama, A. Autoimmune Thrombocytopenia Complicated by EDTA- and/or Citrate-Dependent Pseudothrombocytopenia. Transfus. Med. Hemother. 2015, 42, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Herb, A.; Maurer, M.; Alamome, I.; Bihl, P.-A.; Ghiura, C.; Hurstel, R. A case report of pseudo grey platelet syndrome with citrate-induced pseudothrombocytopenia: Those artifacts may interfere in the platelet numeration and lead to critical misdiagnosis. Ann. Biol. Clin. 2017, 75, 457–461. [Google Scholar] [CrossRef]
- Védy, S.; Boom, B.; Perez, P.; Schillinger, S.; Ragot, C.; Bakkouch, S.; Puyhardy, J.-M. Automatic platelets numbering with citrate as anticoagulant: Is the result valid? Ann. Biol. Clin. 2011, 69, 453–458. [Google Scholar] [CrossRef]
- Larsen, P.B.; Vikeså, J.; Friis-Hansen, L. EDTA-induced pseudothrombocytosis and citrate-induced platelet agglutination in a patient with Waldenstrom macroglobulinemia. Clin. Case Rep. 2017, 5, 1243–1247. [Google Scholar] [CrossRef]
- Deng, J.; Chen, Y.; Zhang, S.; Li, L.; Shi, Q.; Liu, M.; Yu, X. Mindray SF-Cube technology: An effective way for correcting platelet count in individuals with EDTA dependent pseudo thrombocytopenia. Clin. Chim. Acta 2020, 502, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Guidi, G.; Nicoli, M. Platelet count in EDTA-dependent pseudothrombocytopenia. Eur. J. Haematol. 1996, 56, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Briggs, C.; Harrison, P.; Grant, D.; Staves, J.; Machin, S.J. New quantitative parameters on a recently introduced automated blood cell counter—the XE 2100 TM: Automated blood cell counter quantitative parameters. Clin. Lab. Haematol. 2000, 22, 345–350. [Google Scholar] [CrossRef]
- Sandhaus, L.M.; Osei, E.S.; Agrawal, N.N.; Dillman, C.A.; Meyerson, H.J. Platelet Counting by the Coulter LH 750, Sysmex XE 2100, and Advia 120: A Comparative Analysis Using the RBC/Platelet Ratio Reference Method. Am. J. Clin. Pathol. 2002, 118, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Briggs, C.; Longair, I.; Kumar, P.; Singh, D.; Machin, S.J. Performance evaluation of the Sysmex haematology XN modular system. J. Clin. Pathol. 2012, 65, 1024–1030. [Google Scholar] [CrossRef]
- Kim, H.; Bang, S.; Cho, D.; Kim, H.; Kim, S. Performance evaluation of platelet counting of Abbott Alinity hq and Sysmex XN-9000 automated hematology analyzer compared with international reference method. Int. J. Lab. Hematol. 2020, 13396. [Google Scholar] [CrossRef]
- Sun, Y.; Hu, Z.; Huang, Z.; Chen, H.; Qin, S.; Jianing, Z.; Chen, S.; Qin, X.; Ye, Y.; Wang, C. Compare the accuracy and precision of Coulter LH780, Mindray BC-6000 Plus, and Sysmex XN-9000 with the international reference flow cytometric method in platelet counting. PLoS ONE 2019, 14, e0217298. [Google Scholar] [CrossRef]
- Schoorl, M.; Schoorl, M.; Oomes, J.; van Pelt, J. New Fluorescent Method (PLT-F) on Sysmex XN2000 Hematology Analyzer Achieved Higher Accuracy in Low Platelet Counting. Am. J. Clin. Pathol. 2013, 140, 495–499. [Google Scholar] [CrossRef]
- Park, S.H.; Park, C.-J.; Kim, M.-J.; Han, M.-Y.; Han, S.-H.; Cho, Y.-U.; Jang, S. The New Sysmex XN-2000 Automated Blood Cell Analyzer More Accurately Measures the Absolute Number and the Proportion of Hematopoietic Stem and Progenitor Cells Than XE-2100 When Compared to Flow Cytometric Enumeration of CD34 + Cells. Ann. Lab. Med. 2015, 35, 146–148. [Google Scholar] [CrossRef]
- Hummel, K.; Sachse, M.; Hoffmann, J.J.M.L.; van Dun, L.P.J.M. Comparative evaluation of platelet counts in two hematology analyzers and potential effects on prophylactic platelet transfusion decisions: PLT COUNTS AND TRANSFUSION DECISIONS. Transfusion 2018, 58, 2301–2308. [Google Scholar] [CrossRef]
- International Council for Standardization in Haematology Expert Panel on Cytometry; International Society of Laboratory Hematology Task Force on Platelet Counting. Platelet counting by the RBC/platelet ratio method: A reference method. Am. J. Clin. Pathol. 2001, 115, 460–464. [Google Scholar] [CrossRef]
- Anchinmane, V.T.; Sankhe, S.V. Utility of peripheral blood smear in platelet count estimation. Int. J. Res. Med. Sci. 2019, 7, 434. [Google Scholar] [CrossRef]
- Dumont, P.; Goussot, V.; David, A.; Lizard, S.; Riedinger, J.-M. Identification and validation of a factor of commutability between platelet counts performed on EDTA and citrate. Ann. Biol. Clin. 2017, 75, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Kabutomori, O.; Koh, T.; Amino, N.; Iwatani, Y. “Correct” platelet count in EDTA-dependent pseudothrombocytopenia. Eur. J. Haematol. 2009, 55, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Lippi, U.; Schinella, M.; Nicoli, M.; Modena, N.; Lippi, G. EDTA-induced platelet aggregation can be avoided by a new anticoagulant also suitable for automated complete blood count. Haematologica 1990, 75, 38–41. [Google Scholar]
- Lippi, U.; Schinella, M.; Modena, N.; Nicoli, M.; Lippi, G. Advantages of a New Anticoagulant in Routine Hematology on the Coulter Counter® S-Plus STKR Analyzer. Am. J. Clin. Pathol. 1990, 93, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Granat, F.; Geffrè, A.; Braun, J.-P.; Trumel, C. Comparison of Platelet Clumping and Complete Blood Count Results with Sysmex XT-2000iV in Feline Blood Sampled on EDTA or EDTA plus CTAD (Citrate, Theophylline, Adenosine and Dipyridamole). J. Feline Med. Surg. 2011, 13, 953–958. [Google Scholar] [CrossRef]
- Granat, F.A.; Geffré, A.; Lucarelli, L.A.; Braun, J.-P.D.; Trumel, C.; Bourgès-Abella, N.H. Evaluation of CTAD (citrate–theophylline–adenosine–dipyridamole) as a universal anticoagulant in dogs. J. Vet. Diagn. Invest. 2017, 29, 676–682. [Google Scholar] [CrossRef]
- Yokota, M.; Tatsumi, N.; Tsuda, I.; Nishioka, T.; Takubo, T. CTAD as a universal anticoagulant. J. Autom. Methods Manag. Chem. 2003, 25, 17–20. [Google Scholar] [CrossRef] [PubMed]
- François, D.; Masure, A.; Atallah, N.; Touil, L.; Vasse, M. Underestimation of platelet count on magnesium salt-anticoagulated samples. Clin. Chem. Lab. Med. 2014, 52, e95–e97. [Google Scholar] [CrossRef]
- Kohlschein, P.; Bänsch, D.; Dreißiger, K.; Schuff-Werner, P. Exclusion of thrombocytopenia as a contraindication for invasive radiofrequency ablation in a patient with paroxysmal atrial fibrillation by using magnesium anticoagulation instead of EDTA: Another case of anticoagulant-induced pseudo-thrombocytopenia. Heart Surg. Forum 2015, 18, E90–E92. [Google Scholar] [CrossRef] [PubMed]
- Hardy, M.; Lessire, S.; Kasikci, S.; Baudar, J.; Collard, A.; Dogn, J.-M.; Lecompte, T.; Mullier, F. Effects of Time-Interval since Blood Draw and of Anticoagulation on Platelet Testing (Count, Indices and Impedance Aggregometry): A Systematic Study with Blood from Healthy Volunteers. J. Clin. Med. 2020, 9, 2515. [Google Scholar] [CrossRef] [PubMed]
- Akyol, L.; Onem, S.; Ozgen, M.; Sayarlioglu, M. Ethylenediaminetetraacetic acid-dependent pseudothrombocytopenia in a patient with systemic lupus erythematosus and lupus nephritis. Eur. J. Rheumatol. 2016, 3, 36–37. [Google Scholar] [CrossRef] [PubMed]
- Hultin, M.B.; Sussman, I.I. Postoperative thrombocytopenia in type IIB von Willebrand disease. Am. J. Hematol. 1990, 33, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Creary, S.; Varga, E.A.; Kahwash, S.B. Thrombocytopenia Pitfalls: Misdiagnosing Type 2B von Willebrand Disease as Ethylenediaminetetraacetic Acid−Dependent Pseudothrombocytopenia. J. Pediatr. 2016, 175, 238–238.e1. [Google Scholar] [CrossRef] [PubMed]
- Saba, H.I.; Saba, S.R.; Dent, J.; Ruggeri, Z.M.; Zimmerman, T.S. Type IIB Tampa: A variant of von Willebrand disease with chronic thrombocytopenia, circulating platelet aggregates, and spontaneous platelet aggregation. Blood 1985, 66, 282–286. [Google Scholar] [CrossRef]
- Kratz, A.; Wood, M.J.; Siegel, A.J.; Hiers, J.R.; Van Cott, E.M. Effects of Marathon Running on Platelet Activation Markers: Direct Evidence for In Vivo Platelet Activation. Am. J. Clin. Pathol. 2006, 125, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Lau, L.G.; Chng, W.J.; Liu, T.C. Unnecessary transfusions due to pseudothrombocytopenia: TRANSFUSION MEDICINE ILLUSTRATED. Transfusion 2004, 44, 801. [Google Scholar] [CrossRef] [PubMed]
- Yamada, E.J.; Souto, A.F.P.; Souza, E.D.E.O.D.; Nunes, C.A.; Dias, C.P. Pseudoplaquetopenia em paciente submetida à esplenectomia de baço acessório: Relato de caso. Rev. Bras. Anestesiol. 2008, 58, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, T.; Norberg, B. Thrombocytopenia and pseudothrombocytopenia: A clinical and laboratory problem. Eur. J. Haematol. 1986, 37, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Tardy, B.; Lecompte, T.; Mullier, F.; Vayne, C.; Pouplard, C. Detection of Platelet-Activating Antibodies Associated with Heparin-Induced Thrombocytopenia. J. Clin. Med. 2020, 9, 1226. [Google Scholar] [CrossRef] [PubMed]
| Author (Ref.) | Anticoagulant-Induced Ptcp | Medical Condition | Clinical Implication | Confirmation on Alternative Anticoagulants |
|---|---|---|---|---|
| Akyol et al., 2015 [130] | EDTA | SLE & Lupus nephritis | Unnecessary platelet transfusion | Citrate |
| Kohlschein et al., 2015 [128] | EDTA, Citrate | Paroxysmal atrial fibrillation | Delayed cardiological intervention | Magnesium sulfate |
| Greinacher et al., 2016 [98] | EDTA, Citrate | ACS under GpIIb/IIIa antagonist (Eptifibatide) | Therapeutic management issues and wrongly transferred in ICU | ND |
| Shi et al., 2017 [80] | EDTA | Sepsis | Unnecessary platelet transfusion | Citrate |
| Li et al., 2020 [2] | EDTA | Viral infection (COVID 19) | Unnecessary platelet transfusion | Citrate |
| Kuhlman et al., 2020 [3] | EDTA, Citrate, Heparin | Viral infection (COVID 19) | Associated with an arterial occlusive stent (STEMI) | None |
| Zhong et al., 2020 [49] | EDTA, Citrate, Heparin | Viral infection (gastroenteritis) | Treated with dexamethasone due to misdiagnosis of ITP | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lardinois, B.; Favresse, J.; Chatelain, B.; Lippi, G.; Mullier, F. Pseudothrombocytopenia—A Review on Causes, Occurrence and Clinical Implications. J. Clin. Med. 2021, 10, 594. https://doi.org/10.3390/jcm10040594
Lardinois B, Favresse J, Chatelain B, Lippi G, Mullier F. Pseudothrombocytopenia—A Review on Causes, Occurrence and Clinical Implications. Journal of Clinical Medicine. 2021; 10(4):594. https://doi.org/10.3390/jcm10040594
Chicago/Turabian StyleLardinois, Benjamin, Julien Favresse, Bernard Chatelain, Giuseppe Lippi, and François Mullier. 2021. "Pseudothrombocytopenia—A Review on Causes, Occurrence and Clinical Implications" Journal of Clinical Medicine 10, no. 4: 594. https://doi.org/10.3390/jcm10040594
APA StyleLardinois, B., Favresse, J., Chatelain, B., Lippi, G., & Mullier, F. (2021). Pseudothrombocytopenia—A Review on Causes, Occurrence and Clinical Implications. Journal of Clinical Medicine, 10(4), 594. https://doi.org/10.3390/jcm10040594







