Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Variable
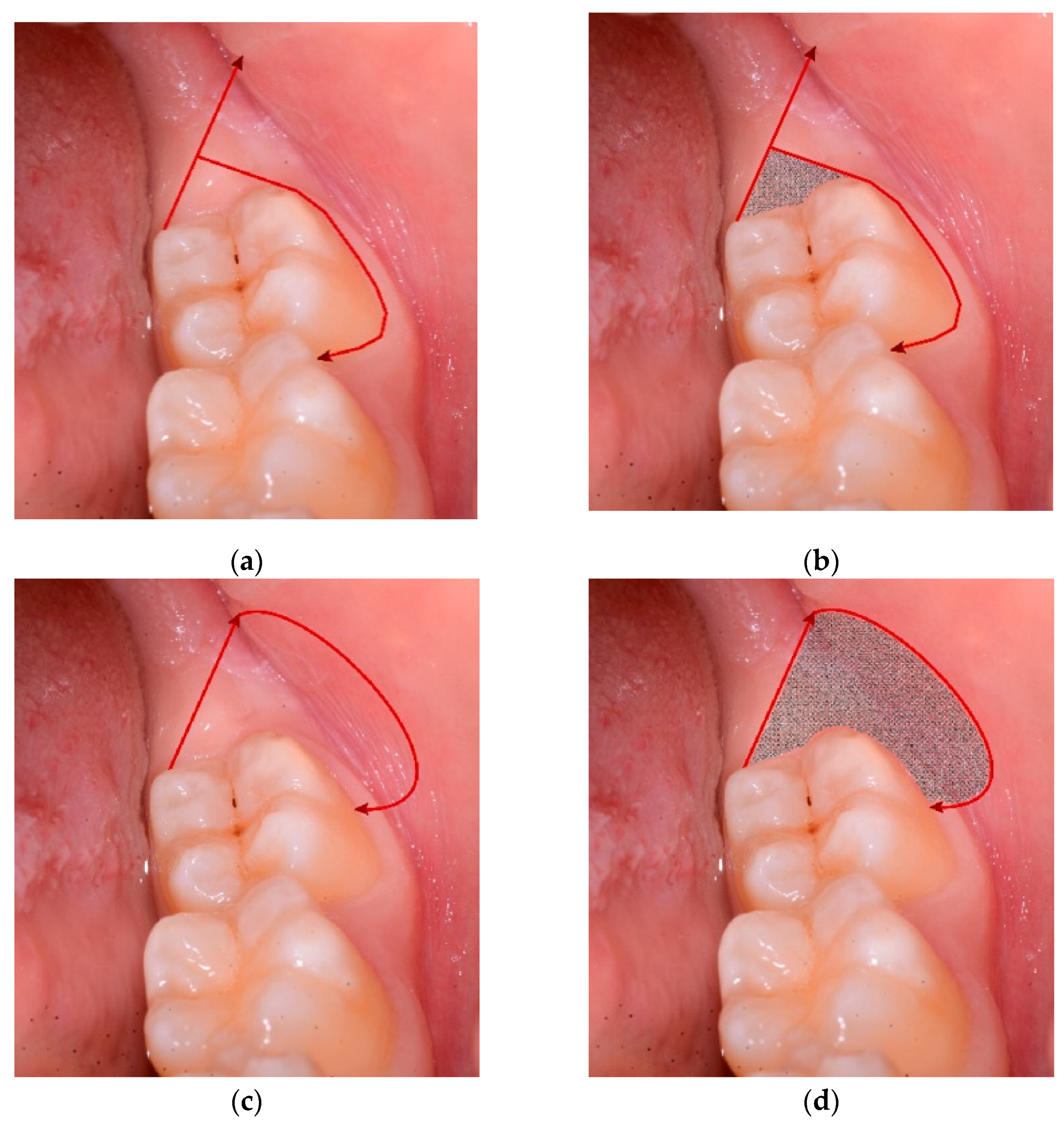
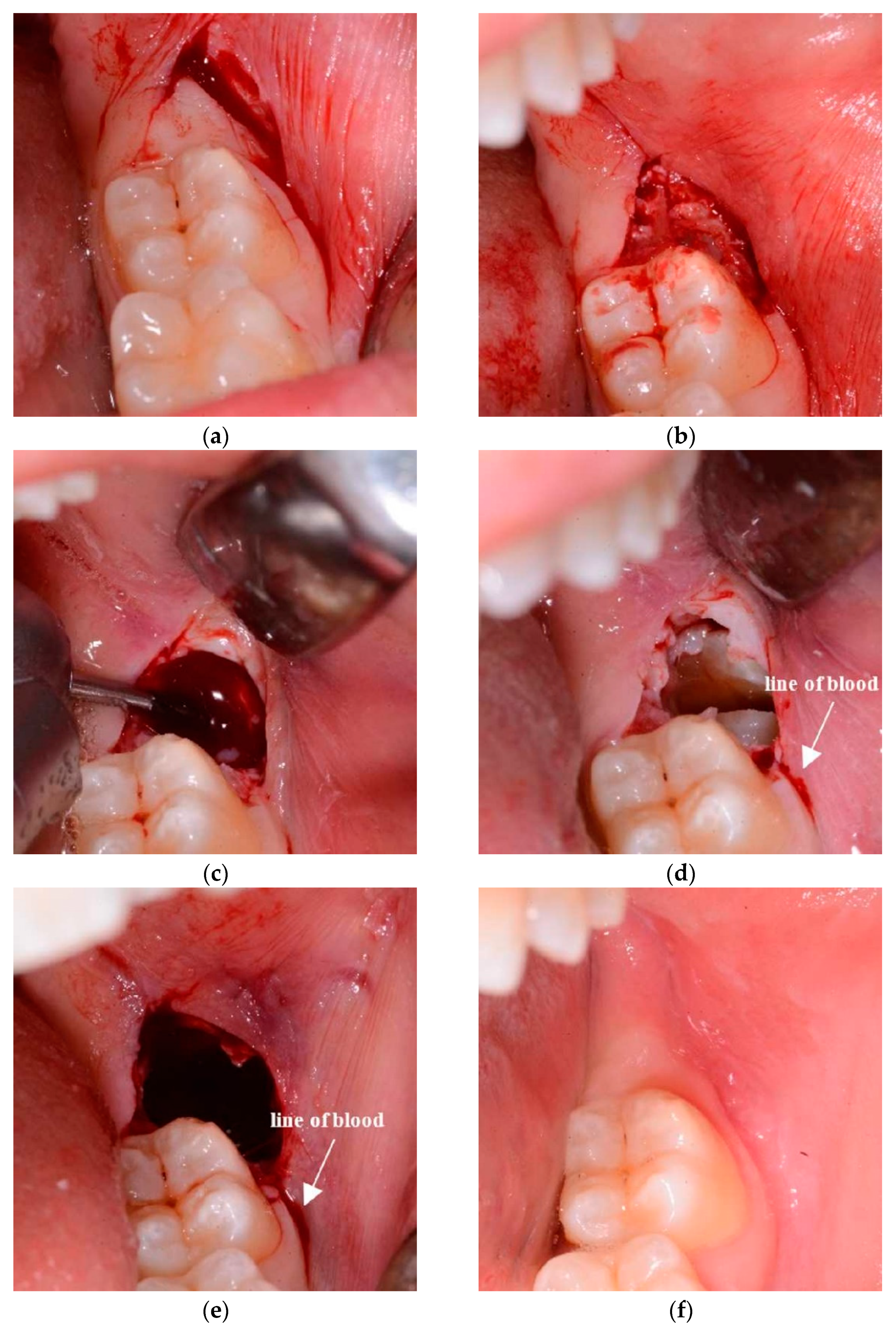
2.2. Surgical Design
2.3. Statistical Analysis
3. Results
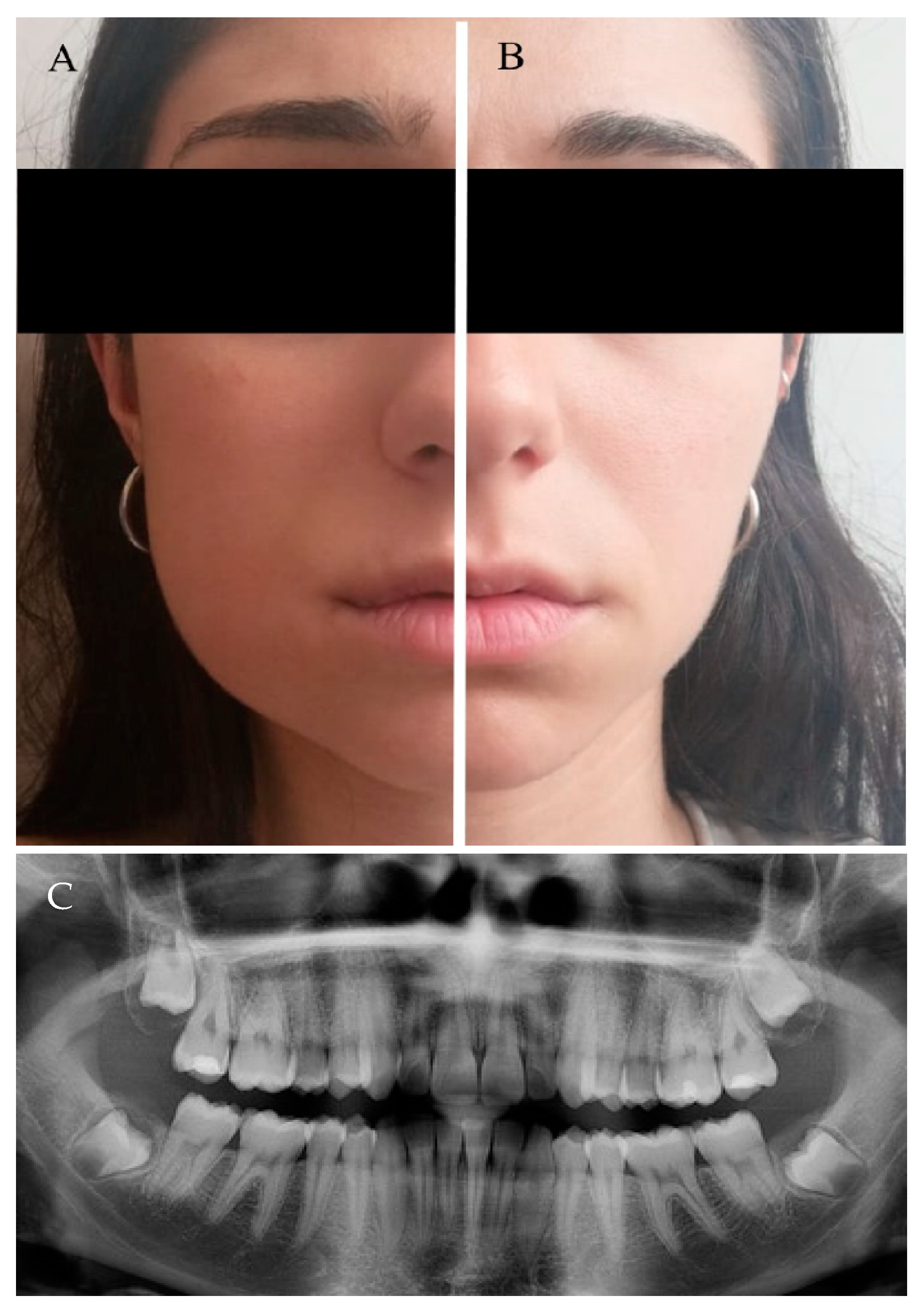
3.1. Patient and Baseline Characteristics
3.2. Clinical Follow-Up and Outcome Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbato, L.; Kalemaj, Z.; Buti, J.; Baccini, M.; La Marca, M.; Duvina, M.; Tonelli, P. Effect of surgical intervention for removal of mandibular third molar on periodontal healing of adjacent mandibular second molar: A systematic review and bayesian network meta-analysis. J. Periodontol. 2016, 87, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Berge, T.I.; Bøe, O.E. Predictor evaluation of postoperative morbidity after surgical removal of mandibular third molars. Acta Odontol. Scand. 1994, 52, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Øyri, H.; Bjørnland, T.; Barkvoll, P.; Jensen, J.L. Mandibular third molar surgery in 396 patients at a Norwegian university clinic: Morbidity recorded after 1 week utilizing an e-infrastructure for clinical research. Acta Odontol. Scand. 2016, 74, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-W.; Lee, C.-T.; Hum, L.; Chuang, S.-K. Effect of flap design on periodontal healing after impacted third molar extraction: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 363–372. [Google Scholar] [CrossRef]
- Khaleelahmed, S.; Alqahtani, N.A.; Desai, F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. J. Oral Maxillofac. Pathol. 2017, 21, 317–318. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Liu, Z.; Shi, Y.; Fang, D.; Li, S.; Zhang, D. A novel orthodontic extraction method for removal of impacted mandibular third molars in close proximity to inferior alveolar nerve. J. Oral. Maxillofac. Surg. 2019, 77, 1575.e1–1575.e6. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, P.; Bailey, E.; Esposito, M.; Furness, S.; Renton, T.F.; Worthington, H.V. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst. Rev. 2014, 29, CD004345. [Google Scholar] [CrossRef]
- Suarez-Cunqueiro, M.M.; Gutwald, R.; Reichman, J.; Otero-Cepeda, X.L.; Schmelzeisen, R. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2003, 95, 403–408. [Google Scholar] [CrossRef]
- Libersa, P.; Roze, D.; Cachart, T.; Libersa, J.-C. Immediate and late mandibular fractures after third molar removal. J. Oral Maxillofac. Surg. 2002, 60, 163–165. [Google Scholar] [CrossRef]
- Schimmel, M.; Müller, F.; Suter, V.; Buser, D. Implants for elderly patients. Periodontology 2000 2016, 73, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Asadollahi, R.; Mohammadi Khah, M.; Yahyazadehfar, N.; Kouhestani, F.; Tehrani, Z.; González-Argote, J.; Alfonso-Sanchez, I. Dental implant placement with flapless and flapped technique: A systematic review. J. Oral Res. 2018, 7, 264–275. [Google Scholar] [CrossRef]
- Anumala, D.; Haritha, M.; Sailaja, S.; Prasuna, E.; Sravanthi, G.; Reddy, N. Effect of flap and flapless implant surgical techniques on soft and hard tissue profile in single-stage dental implants. J. Orofac. Sci. 2019, 11, 11. [Google Scholar] [CrossRef]
- Khojastepour, L.; Khaghaninejad, M.S.; Hasanshahi, R.; Forghani, M.; Ahrari, F. Does the winter or pell and Gregory classification system indicate the apical position of impacted mandibular third molars? J. Oral Maxillofac. Surg. 2019, 77, 2222.e1–2222.e9. [Google Scholar] [CrossRef]
- Monaco, G.; Daprile, G.; Tavernese, L.; Corinaldesi, G.; Marchetti, C. Mandibular third molar removal in young patients: An evaluation of 2 different flap designs. J. Oral Maxillofac. Surg. 2009, 67, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.A.; Horliana, A.C.R.T.; Pannuti, C.M.; Braz-Silva, P.H.; Bispo, C.G.C.; Buscariolo, I.A.; Rocha, R.G.; Tortamano, I.P. Comparative evaluation of anesthetic efficacy of 1.8 mL and 3.6 mL of articaine in irreversible pulpitis of the mandibular molar: A randomized clinical trial. PLoS ONE 2019, 14, e0219536. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, P.E.; Wilson, B.J.; Loga, M.G.; Ariyawardana, A. Effect of submucosal dexamethasone injections in the prevention of postoperative pain, trismus, and oedema associated with mandibular third molar surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2019, 48, 1456–1469. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; De Cicco, L.; Marrone, G. Side effects and complications associated with third molar surgery. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 412–420. [Google Scholar] [CrossRef]
- Peterson, L.J. Antibiotic prophylaxis against wound infections in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 1990, 48, 617–620. [Google Scholar] [CrossRef]
- Longman, L.P.; Martin, M.V. The use of antibiotics in the prevention of post-operative infection: A re-appraisal. Br. Dent. J. 1991, 170, 257–262. [Google Scholar] [CrossRef]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Grossi, G.B.; Maiorana, C.; Garramone, R.A.; Borgonovo, A.; Creminelli, L.; Santoro, F. Assessing postoperative discomfort after third molar surgery: A prospective study. J. Oral Maxillofac. Surg. 2007, 65, 901–917. [Google Scholar] [CrossRef]
- Pogrel, M.A. What Is the effect of timing of removal on the incidence and severity of complications? J. Oral Maxillofac. Surg. 2012, 70, S37–S40. [Google Scholar] [CrossRef]
- Ottria, L.; Luciani, F.; Piva, P.; Alagna, A.; Arcuri, C.; Bartuli, F. The flap recovery on the impacted lower third molar surgery comparing 3 different flap designs: A clinical study. Oral Implant. (Rome) 2017, 10, 270–275. [Google Scholar] [CrossRef]
- Kjølle, G.K.; Bjørnland, T. Low risk of neurosensory dysfunction after mandibular third molar surgery in patients less than 30 years of age. A prospective study following removal of 1220 mandibular third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 411–417. [Google Scholar] [CrossRef]
- Barone, R.; Clauser, C.; Testori, T.; Del Fabbro, M. Self-assessed neurological disturbances after surgical removal of impacted lower third molar: A pragmatic prospective study on 423 surgical extractions in 247 consecutive patients. Clin. Oral Investig. 2019, 23, 3257–3265. [Google Scholar] [CrossRef]
- Gülşen, U.; Şentürk, M.F. Effect of platelet rich fibrin on edema and pain following third molar surgery: A split mouth control study. BMC Oral Heal. 2017, 17, 79. [Google Scholar] [CrossRef]
- Liu, S.; You, Z.; Ma, C.; Wang, Y.; Zhao, H. Effectiveness of drainage in mandibular third molar surgery: A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2018, 76, 1640–1650. [Google Scholar] [CrossRef]
- Damodar, N.D.; Nandakumar, H.; Srinath, N.M. Postoperative recovery after mandibular third molar surgery: A criterion for selection of type of surgical site closure. Gen. Dent. 2013, 61, e9–e13. [Google Scholar]
- Pajarola, G.F.; Sailer, H.F. The surgical removal of the lower wisdom teeth. Is open follow-up care still up-to-date? Schweiz Monatsschr Zahnmed. 1994, 104, 1202–1209. [Google Scholar]
| Variable | TA | FSA | ||
|---|---|---|---|---|
| T0 | T1 | T0 | T1 | |
| AG | 3.4 (0.6) | 3.2 (0.8) | 2.9 (0.8) | 3.3 (0.5) * |
| PPD | 5.4 (1.9) | 3.5 (1.0) | 5.4 (2.1) | 3.6 (1.0) |
| Variable | TA | FSA | ||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T0 | T1 | T2 | |
| OED | 0.0 (0.0) | 0.6 * (0.5) | 1.8 * (1.3) | 0.0 (0.0) | 0.1 (0.3) | 0.1 (0.3) |
| PS | 0.4 (1.2) | 1.3 * (1.2) | 0.8 * (1.3) | 0.3 (0.9) | 0.1 (0.3) | 0.2 (0.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Materni, A.; De Angelis, N.; Di Tullio, N.; Colombo, E.; Benedicenti, S.; Amaroli, A. Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study. J. Clin. Med. 2021, 10, 593. https://doi.org/10.3390/jcm10040593
Materni A, De Angelis N, Di Tullio N, Colombo E, Benedicenti S, Amaroli A. Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study. Journal of Clinical Medicine. 2021; 10(4):593. https://doi.org/10.3390/jcm10040593
Chicago/Turabian StyleMaterni, Alberto, Nicola De Angelis, Nicolò Di Tullio, Esteban Colombo, Stefano Benedicenti, and Andrea Amaroli. 2021. "Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study" Journal of Clinical Medicine 10, no. 4: 593. https://doi.org/10.3390/jcm10040593
APA StyleMaterni, A., De Angelis, N., Di Tullio, N., Colombo, E., Benedicenti, S., & Amaroli, A. (2021). Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study. Journal of Clinical Medicine, 10(4), 593. https://doi.org/10.3390/jcm10040593









