Hormonal Treatment of Men with Nonobstructive Azoospermia: What Does the Evidence Suggest?
Abstract
1. Introduction
2. Hormonal Control of Spermatogenesis
3. Relationship between Serum Hormones Levels and Sperm Retrieval
4. Hormonal Treatment before Micro-TESE
5. Unmet Needs and Future Directions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| 17OHP | 17 hydroxyprogesterone |
| AI | aromatase inhibitors |
| AR | androgen receptor |
| ARE | androgen response elements |
| ARKO | AR knock out animals |
| cAMP | cyclic adenosine monophosphate |
| CC | clomiphene citrate |
| CI | confidence interval |
| CREB | cAMP response element-binding protein |
| EGF | epithelial growth factor |
| FSH | follicle-stimulating hormone |
| FSHKO | FSH knock out animals |
| FSHR | FSH receptor |
| FSHRKO | FSHR knock out animals |
| GNRH | gonadotropin-releasing hormone |
| HCG | human chorionic gonadotropin |
| HYPO | hypospermatogenesis |
| INSL3 | insulin-like factor 3 |
| ITT | intratesticular testosterone |
| KS | Klinefelter syndrome |
| LH | luteinizing hormone |
| LHR | LH receptor |
| LuRKO | LHR knock out animals |
| MA | maturation arrest |
| MAP kinase | mitogen-activated protein kinase |
| Micro-TESE | microdissection testicular sperm extraction |
| NOA | nonobstructive azoospermia |
| OR | odds ratio |
| SCARKO | Sertoli cell AR knock out animals |
| SCO | Sertoli-cell only syndrome |
| SERM | selective estrogen receptors modulators |
| SRF | sperm retrieval failure |
| SRR | sperm retrieval rate |
| SSR | successful sperm retrieval |
| STAR | steroidogenic acute regulatory protein |
| T | testosterone |
References
- Esteves, S.C. Clinical management of infertile men with nonobstructive azoospermia. Asian J. Androl. 2015, 17, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Bernie, A.M.; Mata, D.A.; Ramasamy, R.; Schlegel, P.N. Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: A systematic review and meta-analysis. Fertil. Steril. 2015, 104, 1099–1103. [Google Scholar] [CrossRef] [PubMed]
- Tapanainen, J.S.; Aittomäki, K.; Min, J.; Vaskivuo, T.; Huhtaniemi, I.T. Men homozygous for an inactivating mutation of the follicle-stimulating hormone (FSH) receptor gene present variable suppression of spermatogenesis and fertility. Nat. Genet. 1997, 15, 205–206. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Mao, J.; Cui, M.; Liu, Z.; Wang, X.; Xiong, S.; Nie, M.; Wu, X. Novel FSHβ mutation in a male patient with isolated FSH deficiency and infertility. Eur. J. Med Genet. 2017, 60, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Rannikko, A.; Pakarinen, P.; Manna, P.R.; Beau, I.; Misrahi, M.; Aittomäki, K. Functional characterization of the human FSH receptor with an inactivating Ala189Val mutation. Mol. Hum. Reprod. 2002, 8, 311–317. [Google Scholar] [CrossRef]
- Siegel, E.T.; Kim, H.G.; Nishimoto, H.K.; Layman, L.C. The molecular basis of impaired follicle-stimulating hormone action: Evidence from human mutations and mouse models. Reprod. Sci. 2013, 20, 211–233. [Google Scholar] [CrossRef]
- Abel, M.H.; Baker, P.J.; Charlton, H.M.; Monteiro, A.; Verhoeven, G.; De Gendt, K.; Guillou, F.; O’Shaughnessy, P.J. Spermatogenesis and sertoli cell activity in mice lacking sertoli cell receptors for follicle-stimulating hormone and androgen. Endocrinology 2008, 149, 3279–3285. [Google Scholar] [CrossRef]
- McLachlan, R.I.; Wreford, N.G.; de Kretser, D.M.; Robertson, D.M. The effects of recombinant follicle-stimulating hormone on the restoration of spermatogenesis in the gonadotropin-releasing hormone-immunized adult rat. Endocrinology 1995, 136, 4035–4043. [Google Scholar] [CrossRef]
- Ruwanpura, S.M.; McLachlan, R.I.; Meachem, S.J. Hormonal regulation of male germ cell development. J. Endocrinol. 2010, 205, 117–131. [Google Scholar] [CrossRef]
- Allan, C.M.; Garcia, A.; Spaliviero, J.; Zhang, F.P.; Jimenez, M.; Huhtaniemi, I.; Handelsman, D.J. Complete Sertoli cell proliferation induced by follicle-stimulating hormone (FSH) independently of luteinizing hormone activity: Evidence from genetic models of isolated FSH action. Endocrinology 2004, 145, 1587–1593. [Google Scholar] [CrossRef]
- Dwyer, A.A.; Sykiotis, G.P.; Hayes, F.J.; Boepple, P.A.; Lee, H.; Loughin, K.R.; Dym, M.; Sluss, P.M.; Crowley, W.F.; Pitteloud, N. Trial of recombinant follicle-stimulating hormone pretreatment for GnRH-induced fertility in patients with congenital hypogonadotropic hypogonadism. J. Clin. Endocrinol. Metab. 2013, 98, E1790–E1795. [Google Scholar] [CrossRef] [PubMed]
- Larose, H.; Kent, T.; Ma, Q.; Shami, A.N.; Harerimana, N.; Li, J.Z.; Hammoud, S.S.; Handel, M.A. Regulation of meiotic progression by Sertoli-cell androgen signaling. Mol. Biol. Cell 2020, 31, 2841–2862. [Google Scholar] [CrossRef] [PubMed]
- Oduwole, O.O.; Peltoketo, H.; Poliandri, A.; Vengadabady, L.; Chrusciel, M.; Doroszko, M.; Samanta, L.; Owen, L.; Keevil, B.; Rahman, N.A.; et al. Constitutively active follicle-stimulating hormone receptor enables androgen-independent spermatogenesis. J. Clin. Invest. 2018, 128, 1787–1792. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.B.; Walker, W.H. Hormone signaling in the testis. In Knobil and Neil’s Physiology of Reproduction, 4th ed.; Academic Press: Cambridge, MA, USA, 2015; pp. 637–690. [Google Scholar]
- Toocheck, C.; Clister, T.; Shupe, J.; Crum, C.; Ravindranathan, P.; Lee, T.K.; Ahn, J.M.; Raj, G.V.; Sukhwani, M.; Orwig, K.E.; et al. Mouse spermatogenesis requires classical and nonclassical testosterone signaling. Biol. Reprod. 2016, 94, 11. [Google Scholar] [CrossRef]
- Zhang, F.P.; Pakarainen, T.; Poutanen, M.; Toppari, J.; Huhtaniemi, I. The low gonadotropin-independent constitutive production of testicular testosterone is sufficient to maintain spermatogenesis. Proc. Natl. Acad. Sci. USA 2003, 100, 13692–13697. [Google Scholar] [CrossRef]
- Oduwole, O.O.; Vydra, N.; Wood, N.E.; Samanta, L.; Owen, L.; Keevil, B.; Donaldson, M.; Naresh, K.; Huhtaniemi, I.T. Overlapping dose responses of spermatogenic and extragonadal testosterone actions jeopardize the principle of hormonal male contraception. FASEB J. 2014, 28, 2566–2576. [Google Scholar] [CrossRef]
- Goto, T.; Hirabayashi, M.; Watanabe, Y.; Sanbo, M.; Tomita, K.; Inoue, N.; Tsukamura, H.; Uenoyama, Y. Testosterone supplementation rescues spermatogenesis and in vitro fertilizing ability of sperm in Kiss1 knockout mice. Endocrinology 2020, 161, bqaa092. [Google Scholar] [CrossRef]
- Campo, S.; Andreone, L.; Ambao, V.; Urrutia, M.; Calandra, R.S.; Rulli, S.B. Hormonal regulation of follicle-stimulating hormone glycosylation in males. Front. Endocrinol. 2019, 10, 17. [Google Scholar] [CrossRef]
- Campo, S.; Ambao, V.; Creus, S.; Gottlieb, S.; Fernandez Vera, G.; Benencia, H.; Bergadà, C. Carbohydrate complexity and proportions of serum FSH isoforms in the male: Lectin-based studies. Mol. Cell. Endocrinol. 2007, 260–262, 197–204. [Google Scholar] [CrossRef]
- Li, H.; Chen, L.P.; Yang, J.; Li, M.C.; Chen, R.B.; Lan, R.Z.; Wang, S.G.; Liu, J.H.; Wang, T. Predictive value of FSH, testicular volume, and histopathological findings for the sperm retrieval rate of microdissection TESE in nonobstructive azoospermia: A meta-analysis. Asian J. Androl. 2018, 20, 30–36. [Google Scholar]
- Ramasamy, R.; Padilla, W.O.; Osterberg, C.; Srivastava, A.; Reifsnyder, J.E.; Niederberger, C.; Schlegel, P.N. A comparison of models for predicting sperm retrieval before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J. Urol. 2013, 189, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, K.; Ohmi, C.; Shimabukuro, T.; Matsuyama, H. Human chorionic gonadotrophin treatment prior to microdissection testicular sperm extraction in nonobstructive azoospermia. Hum. Reprod. 2012, 27, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Caroppo, E.; Colpi, E.M.; D’Amato, G.; Gazzano, G.; Colpi, G.M. Prediction model for testis histology in men with non-obstructive azoospermia: Evidence for a limited predictive role of serum follicle-stimulating hormone. J. Assist. Reprod. Genet. 2019, 36, 2575–2582. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, R.; Lin, K.; Gosden, L.V.; Rosenwaks, Z.; Palermo, G.D.; Schlegel, P.N. High serum FSH levels in men with nonobstructive azoospermia does not affect success of microdissection testicular sperm extraction. Fertil. Steril. 2009, 92, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Bernie, A.M.; Shah, K.; Halpern, J.A.; Scovell, J.; Ramasamy, R.; Robinson, B.; Schlegel, P.N. Outcomes of microdissection testicular sperm extraction in men with nonobstructive azoospermia due to maturation arrest. Fertil. Steril. 2015, 104, 569–573. [Google Scholar] [CrossRef]
- Themmen, A.P.; Blok, L.J.; Post, M.; Baarends, W.M.; Hoogerbrugge, J.W.; Parmentier, M.; Vassart, G.; Grootegoed, J.A. Follitropin receptor down-regulation involves a cAMP-dependent post-transcriptional decrease of receptor mRNA expression. Mol. Cell. Endocrinol. 1991, 78, R7–R13. [Google Scholar] [CrossRef][Green Version]
- Bhaskaran, R.S.; Ascoli, M. The post-endocytotic fate of the gonadotropin receptors is an important determinant of the desensitization of gonadotropin responses. J. Mol. Endocrinol. 2005, 34, 447–457. [Google Scholar] [CrossRef]
- Okada, H.; Dobashi, M.; Yamazaki, T.; Hara, I.; Fujisawa, M.; Arakawa, S.; Kamidono, S. Conventional versus microdissection testicular sperm extraction for nonobstructive azoospermia. J. Urol. 2002, 168, 1063–1067. [Google Scholar] [CrossRef]
- Tsujimura, A.; Matsumiya, K.; Miyagawa, Y.; Takao, S.; Fujita, K.; Koga, M.; Takeyama, M.; Fujioka, H.; Okuyama, A. Prediction of successful outcome of microdissection testicular sperm extraction in men with idiopathic nonobstructive azoospermia. J. Urol. 2004, 172, 1944–1947. [Google Scholar] [CrossRef]
- Tusjiimura, A.; Miyagawa, Y.; Takao, T.; Fujita, K.; Komori, K.; Matsuoka, Y.; Takada, S.; Koga, M.; Takeyama, M.; Fujioka, H.; et al. Impact of age, follicle stimulating hormone and Johnsen’s score on successful sperm retrieval by microdissection testicular sperm extraction. Reprod. Med. Biol. 2005, 4, 53–57. [Google Scholar]
- Ravizzini, P.; Carizza, C.; Abdelmassih, V.; Abdelmassih, S.; Azevedo, M.; Abdelmassih, R. Microdissection testicular sperm extraction and IVF-ICSI outcome in nonobstructive azoospermia. Andrologia 2008, 40, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Ghalayini, I.F.; Al-Ghazo, M.A.; Hani, O.B.; Al-Azab, R.; Bani-Hani, I.; Zayed, F.; Haddad, Y. Clinical comparison of conventional testicular sperm extraction and microdissection techniques for non-obstructive azoospermia. J. Clin. Med. Res. 2011, 3, 124–131. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Reifsnyder, J.E.; Ramasamy, R.; Husseini, J.; Schlegel, P.N. Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J. Urol. 2012, 188, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Cetinkaya, M.; Onem, K.; Zorba, O.U.; Ozkara, H.; Alici, B. Evaluation of microdissection testicular sperm extraction results in patients with non-obstructive azoospermia: Independent predictive factors and best cutoff values for sperm retrieval. Urol. J. 2015, 12, 2436–2443. [Google Scholar] [PubMed]
- Enatsu, N.; Miyake, H.; Chiba, K.; Fujisawa, M. Predictive factors of successful sperm retrieval on microdissection testicular sperm extraction in Japanese men. Reprod. Med. Biol. 2015, 15, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Althakafi, S.A.; Mustafa, O.M.; Seyam, R.M.; Al-Hathal, N.; Kattan, S. Serum testosterone levels and other determinants of sperm retrieval in microdissection testicular sperm extraction. Transl. Androl. Urol. 2017, 6, 282–287. [Google Scholar] [CrossRef]
- Caroppo, E.; Colpi, E.M.; Gazzano, G.; Vaccalluzzo, L.; Piatti, E.; D’Amato, G.; Colpi, G.M. The seminiferous tubule caliber pattern as evaluated at high magnification during microdissection testicular sperm extraction predicts sperm retrieval in patients with non-obstructive azoospermia. Andrology 2019, 7, 8–14. [Google Scholar] [CrossRef]
- Kizilkan, Y.; Toksoz, S.; Turunc, T.; Ozkardes, H. Parameters predicting sperm retrieval rates during microscopic testicular sperm extraction in nonobstructive azoospermia. Andrologia 2019, 51, e13441. [Google Scholar] [CrossRef]
- Mehmood, S.; Aldaweesh, S.; Junejo, N.N.; Altaweel, W.M.; Kattan, S.A.; Alhathal, N. Microdissection testicular sperm extraction: Overall results and impact of preoperative testosterone level on sperm retrieval rate in patients with nonobstructive azoospermia. Urol. Ann. 2019, 11, 287–293. [Google Scholar] [CrossRef]
- Çayan, S.; Orhan, İ.; Altay, B.; Aşcı, R.; Akbay, E.; Ayas, B.; Yaman, Ö. Fertility outcomes and predictors for successful sperm retrieval and pregnancy in 327 azoospermic men with a history of cryptorchidism who underwent microdissection testicular sperm extraction. Andrology 2020. [Google Scholar] [CrossRef]
- Zhang, H.; Xi, Q.; Zhang, X.; Zhang, H.; Jiang, Y.; Liu, R.; Yu, Y. Prediction of microdissection testicular sperm extraction outcome in men with idiopathic nonobstruction azoospermia. Medicine 2020, 99, e19934. [Google Scholar] [CrossRef] [PubMed]
- Guo, F.; Fang, A.; Fan, Y.; Fu, X.; Lan, Y.; Liu, M.; Cao, S.; An, G. Role of treatment with human chorionic gonadotropin and clinical parameters on testicular sperm recovery with microdissection testicular sperm extraction and intracytoplasmic sperm injection outcomes in 184 Klinefelter syndrome patients. Fertil. Steril. 2020, 114, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, R.; Ricci, J.A.; Palermo, G.D.; Gosden, L.V.; Rosenwaks, Z.; Schlegel, P.N. Successful fertility treatment for Klinefelter’s syndrome. J. Urol. 2009, 182, 1108–1113. [Google Scholar] [CrossRef]
- Huhtaniemi, I.; Nikula, H.; Rannikko, S. Pituitary-testicular function of prostatic cancer patients during treatment with a gonadotropin-releasing hormone agonist analog. I. Circulating hormone levels. J. Androl. 1987, 8, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Amory, J.K.; Coviello, A.D.; Page, S.T.; Anawalt, B.D.; Matsumoto, A.M.; Bremner, W.J. Serum 17-hydroxyprogesterone strongly correlates with intratesticular testosterone in gonadotropin-suppressed normal men receiving various dosages of human chorionic gonadotropin. Fertil. Steril. 2008, 89, 380–386. [Google Scholar] [CrossRef]
- Lima, T.F.N.; Patel, P.; Blachman-Braun, R.; Madhusoodanan, V.; Ramasamy, R. Serum 17-hydroxyprogesterone is a potential biomarker for evaluating intratesticular testosterone. J. Urol. 2020, 204, 551–556. [Google Scholar] [CrossRef]
- Bay, K.; Matthiesson, K.; McLachlan, R.; Andersson, A.M. The effects of gonadotropin suppression and selective replacement on insulin-like factor 3 secretion in normal adult men. J. Clin. Endocrinol. Metab. 2006, 91, 1108–1111. [Google Scholar] [CrossRef][Green Version]
- Roth, M.Y.; Lin, K.; Bay, K.; Amory, J.K.; Anawalt, B.D.; Matsumoto, A.M.; Marck, B.T.; Bremner, W.J.; Page, S.T. Serum insulin-like factor 3 is highly correlated with intratesticular testosterone in normal men with acute, experimental gonadotropin deficiency stimulated with low-dose human chorionic gonadotropin: A randomized, controlled trial. Fertil. Steril. 2013, 99, 132–139. [Google Scholar] [CrossRef]
- Levalle, O.A.; Zylbersztein, C.; Aszpis, S.; Mariani, V.; Ponzio, R.; Aranda, C.; Guitelman, A.; Scaglia, H.E. Serum luteinizing hormone pulsatility and intratesticular testosterone and oestradiol concentrations in idiopathic infertile men with high and normal follicle stimulating hormone serum concentrations. Hum. Reprod. 1994, 9, 781–787. [Google Scholar] [CrossRef]
- Shinjo, E.; Shiraishi, K.; Matsuyama, H. The effect of human chorionic gonadotropin-based hormonal therapy on intratesticular testosterone levels and spermatogonial DNA synthesis in men with nonobstructive azoospermia. Andrology 2013, 1, 929–935. [Google Scholar] [CrossRef]
- Bar-Shira Maymon, B.; Yogev, L.; Yavetz, H.; Lifschitz-Mercer, B.; Schreiber, L.; Kleiman, S.E.; Botchan, A.; Hauser, R.; Paz, G. Spermatogonial proliferation patterns in men with azoospermia of different etiologies. Fertil. Steril. 2003, 80, 1175–1180. [Google Scholar] [CrossRef]
- Kato, Y.; Shiraishi, K.; Matsuyama, H. Expression of testicular androgen receptor in non-obstructive azoospermia and its change after hormonal therapy. Andrology 2014, 2, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Blok, L.J.; Mackenbach, P.; Trapman, J.; Themmen, A.P.; Brinkmann, A.O.; Grootegoed, J.A. Follicle-stimulating hormone regulates androgen receptor mRNA in Sertoli cells. Mol. Cell. Endocrinol. 1989, 63, 267–271. [Google Scholar] [CrossRef]
- Aydos, K.; Unlü, C.; Demirel, L.C.; Evirgen, O.; Tolunay, O. The effect of pure FSH administration in non-obstructive azoospermic men on testicular sperm retrieval. Eur. J. Obstet. Gynecol. Reprod. Biol. 2003, 108, 54–58. [Google Scholar] [CrossRef]
- Hussein, A.; Ozgok, Y.; Ross, L.; Niederberger, C. Clomiphene administration for cases of nonobstructive azoospermia: A multicenter study. J. Androl. 2005, 26, 787–791. [Google Scholar] [CrossRef]
- Hussein, A.; Ozgok, Y.; Ross, L.; Rao, P.; Niederberger, C. Optimization of spermatogenesis-regulating hormones in patients with nonobstructive azoospermia and its impact on sperm retrieval: A multicentre study. BJU Int. 2013, 111, E110–E114. [Google Scholar] [CrossRef]
- Amer, M.K.; Ahmed, A.R.; Abdel Hamid, A.A.; Gamal El Din, S.F. Can spermatozoa be retrieved in non-obstructive azoospermic patients with high FSH level? A retrospective cohort study. Andrologia 2019, 51, e13176. [Google Scholar] [CrossRef]
- Amer, M.K.; Ahmed, H.E.H.; Gamal El Din, S.F.; Fawzy Megawer, A.; Ahmed, A.R. Evaluation of neoadjuvant gonadotropin administration with downregulation by testosterone prior to second time microsurgical testicular sperm extraction: A prospective case-control study. Urologia 2020, 87, 185–190. [Google Scholar] [CrossRef]
- Schlegel, P.N.; Sigman, M.; Collura, B.; De Jonge, C.J.; Eisenberg, M.L.; Lamb, D.J.; Mulhall, J.P.; Niederberger, C.; Sandlow, J.I.; Sokol, R.Z.; et al. Diagnosis and treatment of infertility in men: AUA/ASRM guideline. Part II. Fertil. Steril. 2020, 115, 62–69. [Google Scholar] [CrossRef]
- Colpi, G.M.; Caroppo, E. Re: Predictors of surgical sperm retrieval in non-obstructive azoospermia: Summary of current literature. Int. Urol. Nephrol. 2020, 52, 2039–2041. [Google Scholar] [CrossRef]
- Luján, S.; Caroppo, E.; Niederberger, C.; Arce, J.C.; Sadler-Riggleman, I.; Beck, D.; Nilsson, E.; Skinner, M.K. Sperm DNA methylation epimutation biomarkers for male infertility and FSH therapeutic responsiveness. Sci. Rep. 2019, 9, 16786. [Google Scholar] [CrossRef] [PubMed]
| Study | Patients Characteristics | KS | Subnormal T Levels | Main Results | Hormonal Treatment |
|---|---|---|---|---|---|
| [29] | 74 patients SRR 44.4% | Yes (11/74; 14.8%) | Not shown | No relationship was found between serum T levels and SSR. Data about T serum level in patients with SSR and SRF are not provided | NS |
| [30] | 100 patients SRR 41% | No | Not shown | T was significantly higher in men with SSR than in those with SRF (410 ± 170 vs. 320 ± 110 ng/dL. p = 0.0036). On multivariate logistic regression. T was predictive of SSR (OR 1.57; 95% CI 1.02–2.42; p = 0.042). Patients with SRF had also significantly higher FSH level and smaller testis size compared to those with SSR | NS |
| [31] | 100 patients SRR 41% | No | Not shown | T predicted SSR at univariate logistic analysis (p = 0.0008) but not at multivariate logistic analysis. Data about T serum level in patients with SSR and SRF are not provided | NS |
| [32] | 56 patients with previous failed TESA/TESE SRR 57% | Yes (1/56; 1.7%) | 13 patients (23%) with T < 280 ng/dL | T was significantly higher in patients with SSR (32) compared to those with SRF (24) (458.3 ± 254.2 vs. 378.5 ± 257.3; p = 0.021). | NS |
| [33] | 65 patients. SRR 56.9% | No | Not shown | T levels did not affect SSR (OR 1.06; 95% CI 0.84–1.33; p = 0.64). Data about T serum level in patients with SSR and SRF are not provided | NS |
| [34] | 736 patients SRR 54.4% | Yes (88/736; 12%) | 348 patients (47%) had low T levels (<300 ng/dL) before hormonal treatment. Post-treatment T levels are not provided | SRR was 52% of patients with low T vs. 56% of patients with normal T (p = 0.29). No difference in terms of SSR in patients with low basal T who did or did not receive hormonal treatment post-treatment T levels are not displayed. | Yes (307/348 patients with low basal T levels) |
| [35] | 191 patients SRR 54.5% | Yes (7/191; 3%) | Not shown | Testosterone level was significantly higher in men with SSR compared to those with SRF (468 ± 263 vs. 367 ± 258; p = 0.023). The testosterone serum cut-off-level of 400 ng/mL significantly predicted SSR with a sensitivity of 55.2 and a specificity of 60%. AUC 0.648 | NS |
| [36] | 329 patients SRR 29.5% | Yes (65/329; 19.7%) | Not shown | T levels did not differ among men with SSR (97) and SRF (232) (420 ± 180 vs. 430 ± 190 ng/dL; p = 0.42) | NS |
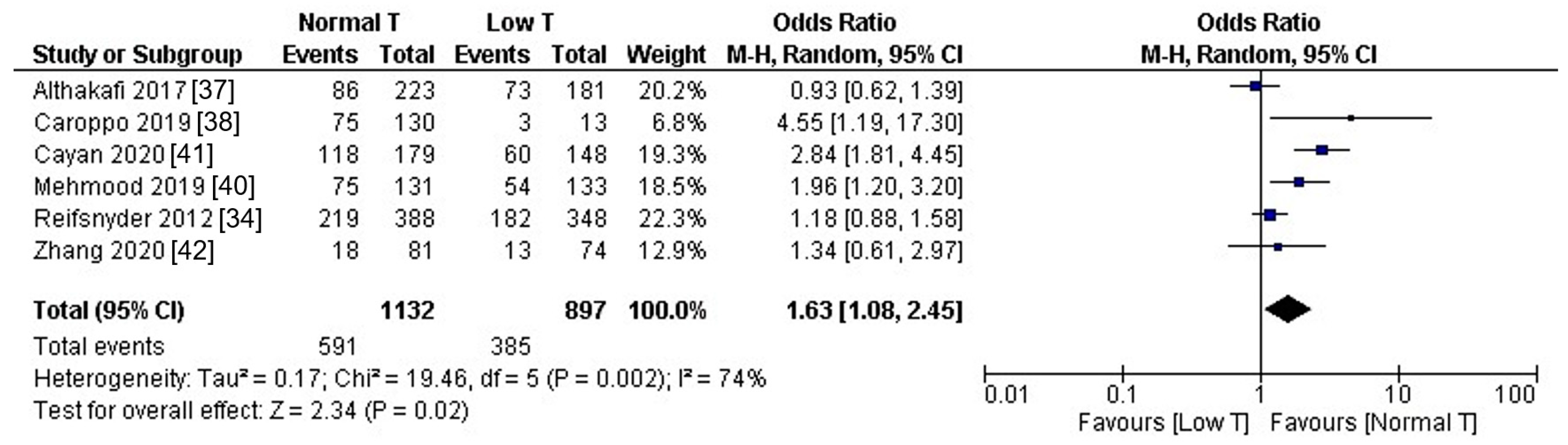
| [37] | 421 patients SSR 39.4% | Yes (13/431; 3%) | 181 patients (43%) had low T (≤9.9 nmol/L). | SRR did not differ in patients with low T (40.3%) compared to those with normal T (38.6%) (p = 0.718); Mean serum T was 11.51 ± 7.40 nmol/L in patients with SSR and 11.67 ± 6.42 nmol/L in patients with SRF SRR did not differ between patients with normal T vs. untreated low T (42%. p = 0.526) and normal vs. pretreated low T normalized with hormonal treatment (36%; p = 0.736) | Yes (50/421) |
| [38] | 143 patients SRR 55.2% | Yes (6/143; 4.1%) | 13 patients (9%) had low T (300 ng/dL) | Testosterone serum level was significantly lower in patients with SRF compared to those with SSR (380 vs. 422 ng/dL; p = 0.007). Sperm retrieval was 23% in patients with low T and 58% in those with normal T (p = 0.014). However. T was not predictive of SSR in multivariate logistic analysis. | No |
| [39] | 860 patients SSR 45.8% | Yes (312/860; 36.2%) | Not shown | Testosterone level was predictive of SSR in univariate but not in multivariate logistic regression | Yes (54/860) |
| [40] | 264 patients 89 (33.9%) had previous surgery SRR 48.86% | NS | 133 with low T (<10 nmol/L = 288 ng/dL) | SSR was 40.6 in low T vs. 57.25 in normal T (p = 0.0068) | No |
| [41] | 327 patients with history of cryptorchidism SSR 52.6% | No | 148 (45.2%) patients had low T (<300 ng/dL) | SSR was 40.5% in low T and 65.9% in normal T (p < 0.0001). | No |
| [42] | 155 patients with idiopathic NOA SSR 20% | No | 74 patients (48%) had T < 9.9 nmol/L. | SSR was 17.6 in low T and 22.2 in normal T (p = NS) | NS |
| Study | Patients Characteristics | Treatment | Results |
|---|---|---|---|
| [55] | 108 men. 16 with SCO. 36 with focal SCO. 19 with MA. 37 with HYPO. All had serum FSH level below 8 mIU/mL | 63 men received FSH 75 IU 3 times/week. 45 received no treatment | SSR 64% (40/63) in FSH treated and 33% (15/45) in controls (p < 0.01) SCO 2/7 (28% controls) vs. 4/9 (44% treated) p = NS FSCO 4/16 (25%) vs. 13/20 (65% treated) (p < 0.01) MA 3/8 (37%) vs. 5/11 (45% treated) p = NS HYPO 6/14 (42%) vs. 18/23 (78% treated) p < 0.05 |
| [56] | 42 men with MA (42.9%) and HYPO (57.1%) | CC 25–75 mg/day to achieve T 600–800 ng/dL (study target) | 27/42 (64.3%) had sperm in the ejaculate; SSR 100% (15/15) |
| [34] | 348 out of 736 patients had subnormal T. 307 out of 348 received hormonal therapy. 41 (12%) received no treatment | 348 (47%) with low T (<300) and 388 with normal T (>300). 307 out of 348 (88%) were treated with hormonal therapy. 41 (12%) were not treated. | SSR in 52% of patients with low T and in 56% of patients with normal T. SSR 51% in treated vs. 61% in untreated |
| [23] | 48 men with failed micro-TESE | 28 hCG/hCG plus FSH if FSH levels decreased during treatment. 20 received no treatment. T did not differ among groups | Sperm retrieval 21% (treatment) vs. 0 (no treatment). |
| [57] | 608 men | 496 received CC, then hCG, and, eventually, hMG according to their response to CC, while 112 received no treatment. Target T level = 600–800 ng/dL | 10.9% of patients had sperm in the ejaculate; SSR was 57% in treated and 33% in controls |
| [51] | 20 men with failed micro-TESE | hCG followed by FSH if serum FSH < 2 | SSR 3/20 (15%). T did not differ among patients with SSR and SRF Spermatogonial PCNA expression increased in patients receiving FSH Patients with SSR had significantly lower basal ITT compared to those with SRF. Post-treatment ITT increased in all patients |
| [53] | 22 men with failed micro-TESE | All received hCG 5000 3 times a week; 12 patients received also FSH 150 thrice/week since FSH level dropped below 2 | SSR 4/22 (18%). A significant increase in the AR index was observed in 12 patients receiving FSH + hCG. AR index was significantly higher in men with SSR compared to SRF. T levels did not correlate with AR index |
| [58] | 1395 patients evaluated by different surgeons | SSR 450/1395 (32.2%) Hormonal therapy (CC or hCG or HMG or FSH or T or AI combination of drugs) in 426 patients | SSR was 27.6% (118/426) in treated vs. 31.7% (308/969) in untreated. No data about T levels in treated vs. untreated. |
| [59] | 40 men with failed micro-TESE. | 20 received testosterone for 1 month. then FSH plus testosterone, while 20 received no treatment | SSR in salvage micro-TESE was 10% in treated vs. 0 in controls. No data about T levels in treated vs. untreated. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caroppo, E.; Colpi, G.M. Hormonal Treatment of Men with Nonobstructive Azoospermia: What Does the Evidence Suggest? J. Clin. Med. 2021, 10, 387. https://doi.org/10.3390/jcm10030387
Caroppo E, Colpi GM. Hormonal Treatment of Men with Nonobstructive Azoospermia: What Does the Evidence Suggest? Journal of Clinical Medicine. 2021; 10(3):387. https://doi.org/10.3390/jcm10030387
Chicago/Turabian StyleCaroppo, Ettore, and Giovanni M. Colpi. 2021. "Hormonal Treatment of Men with Nonobstructive Azoospermia: What Does the Evidence Suggest?" Journal of Clinical Medicine 10, no. 3: 387. https://doi.org/10.3390/jcm10030387
APA StyleCaroppo, E., & Colpi, G. M. (2021). Hormonal Treatment of Men with Nonobstructive Azoospermia: What Does the Evidence Suggest? Journal of Clinical Medicine, 10(3), 387. https://doi.org/10.3390/jcm10030387






