Gan-Lu-Yin (Kanroin), Traditional Chinese Herbal Extracts, Reduces Osteoclast Differentiation In Vitro and Prevents Alveolar Bone Resorption in Rat Experimental Periodontitis
Abstract
1. Introduction
2. Experimental Section
2.1. Reagents
2.2. Cell Culture and Osteoclastogenesis
2.3. Cell Viability Assay
2.4. Western Blot Analysis
2.5. Animals
2.6. Experimental Periodontitis
2.7. Microcomputed Tomography (µCT) Analysis of Alveolar Bone
2.8. Histological Analysis
2.9. Analysis of Bone Metabolism Marker in Rat Serum
2.10. Analysis of Systemic Bone Volume Fraction and Bone Mineral Density
2.11. Statistical Analysis
3. Results
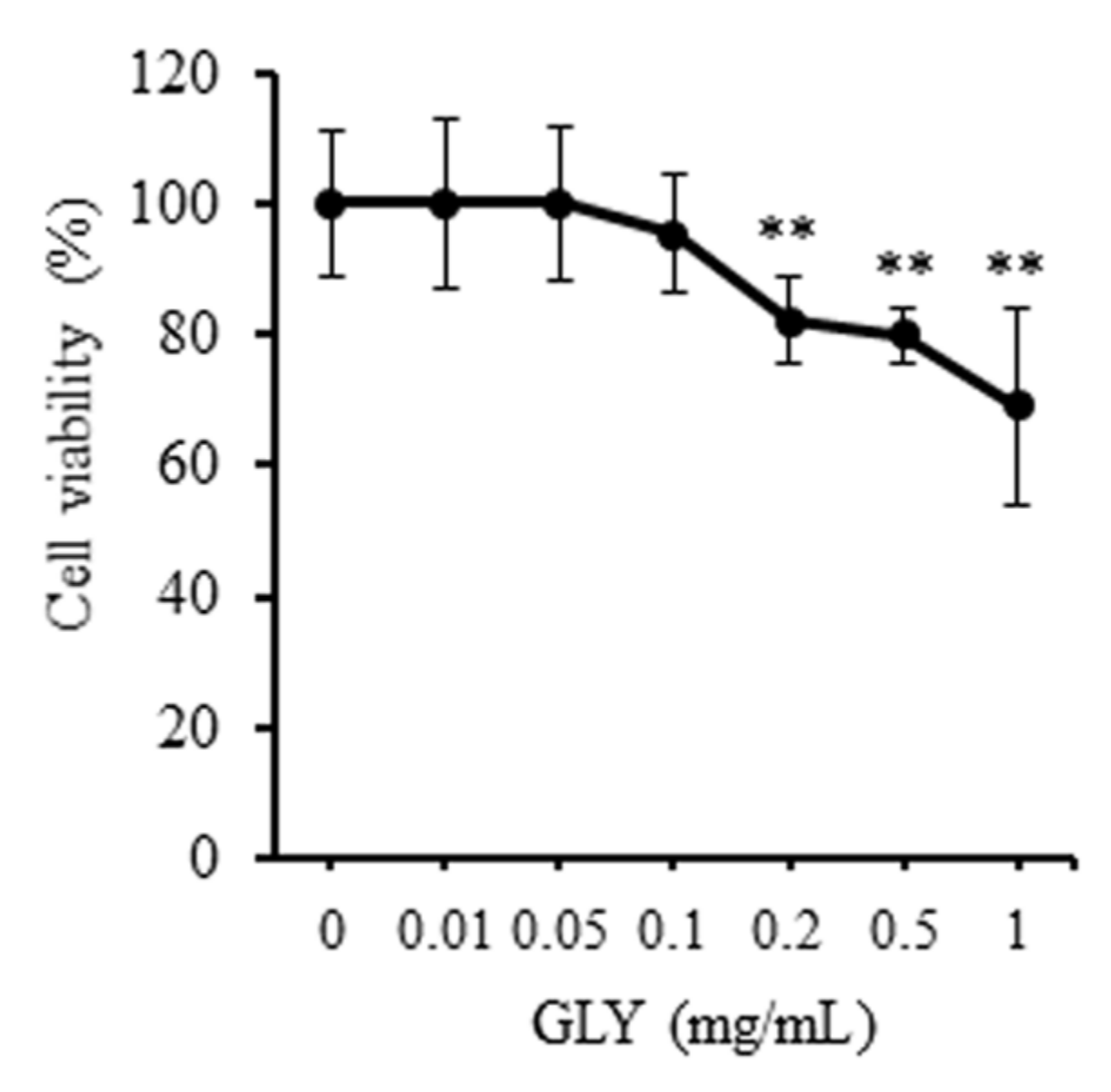
3.1. Effect of GLY Extracts on Cell Proliferation of RAW264.7 Cells
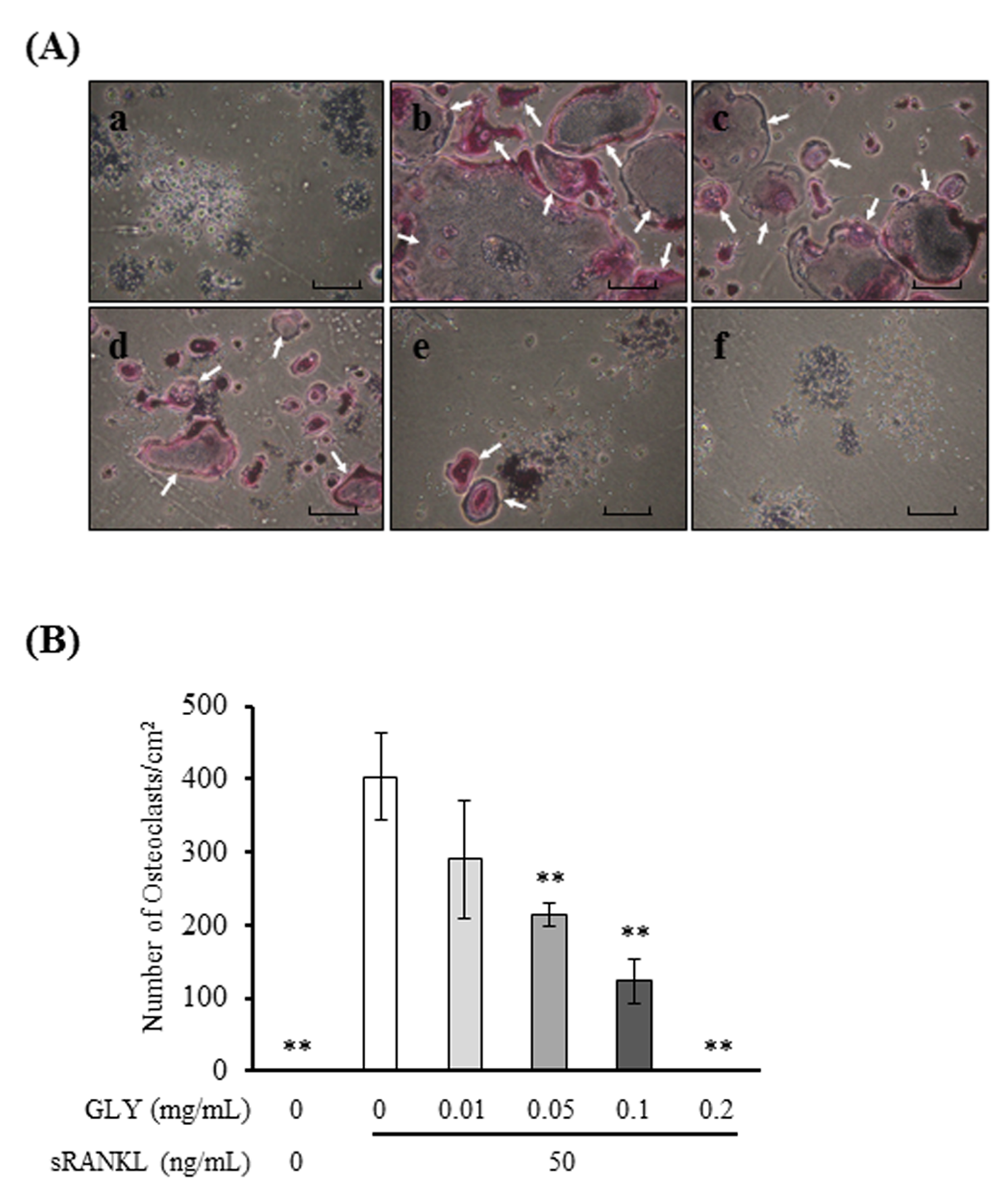
3.2. GLY Extracts Inhibit Osteoclast Differentiation
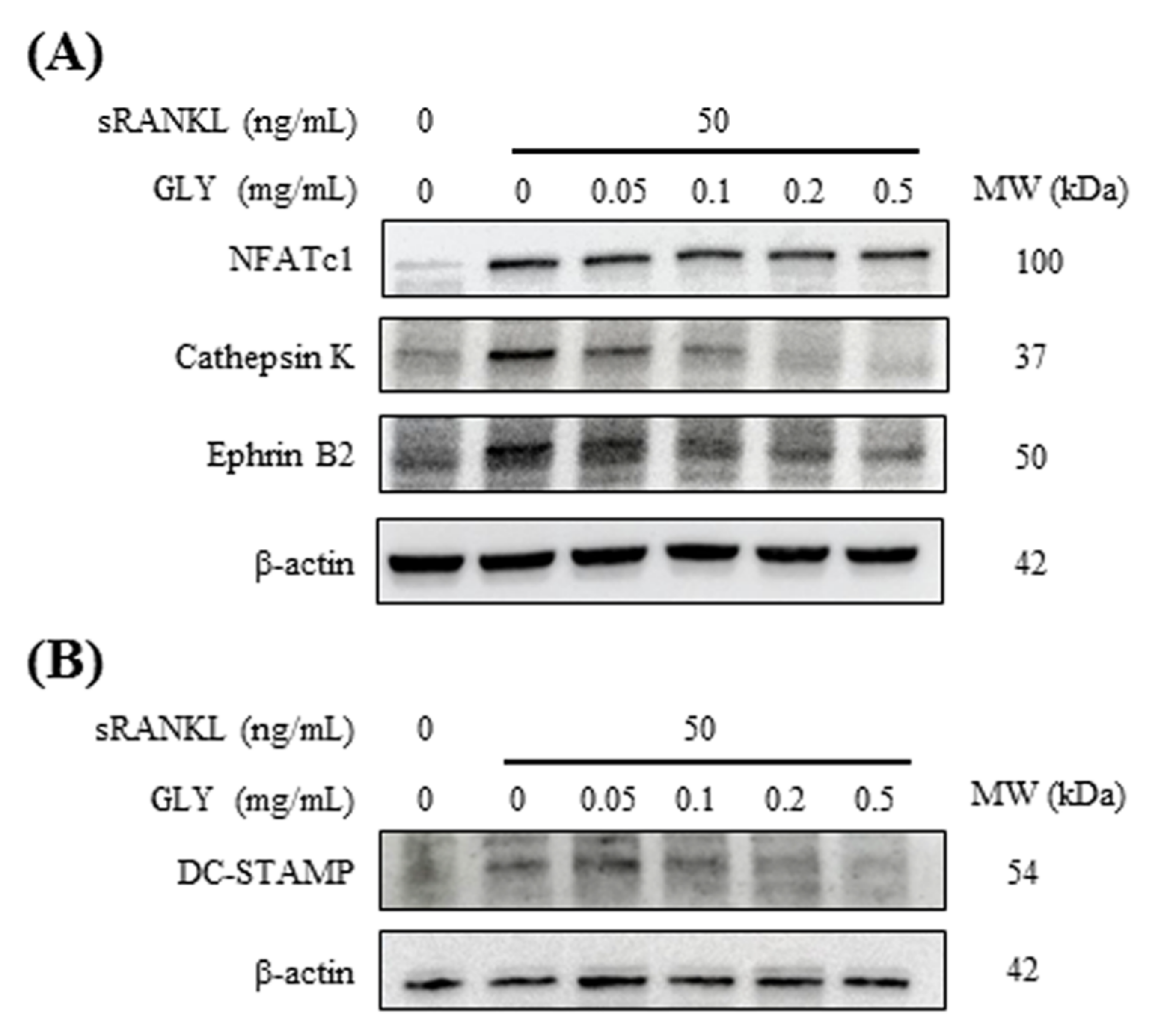
3.3. GLY Extracts Inhibited the Expressions of Osteoclast Markers in RAW264.7 Cells
3.4. GLY Extracts Inhibited Alveolar Bone Resorption in Rat Experimental Periodontitis
3.5. GLY Extracts Inhibited Osteoclast Differentiation in Rat Experimental Periodontitis
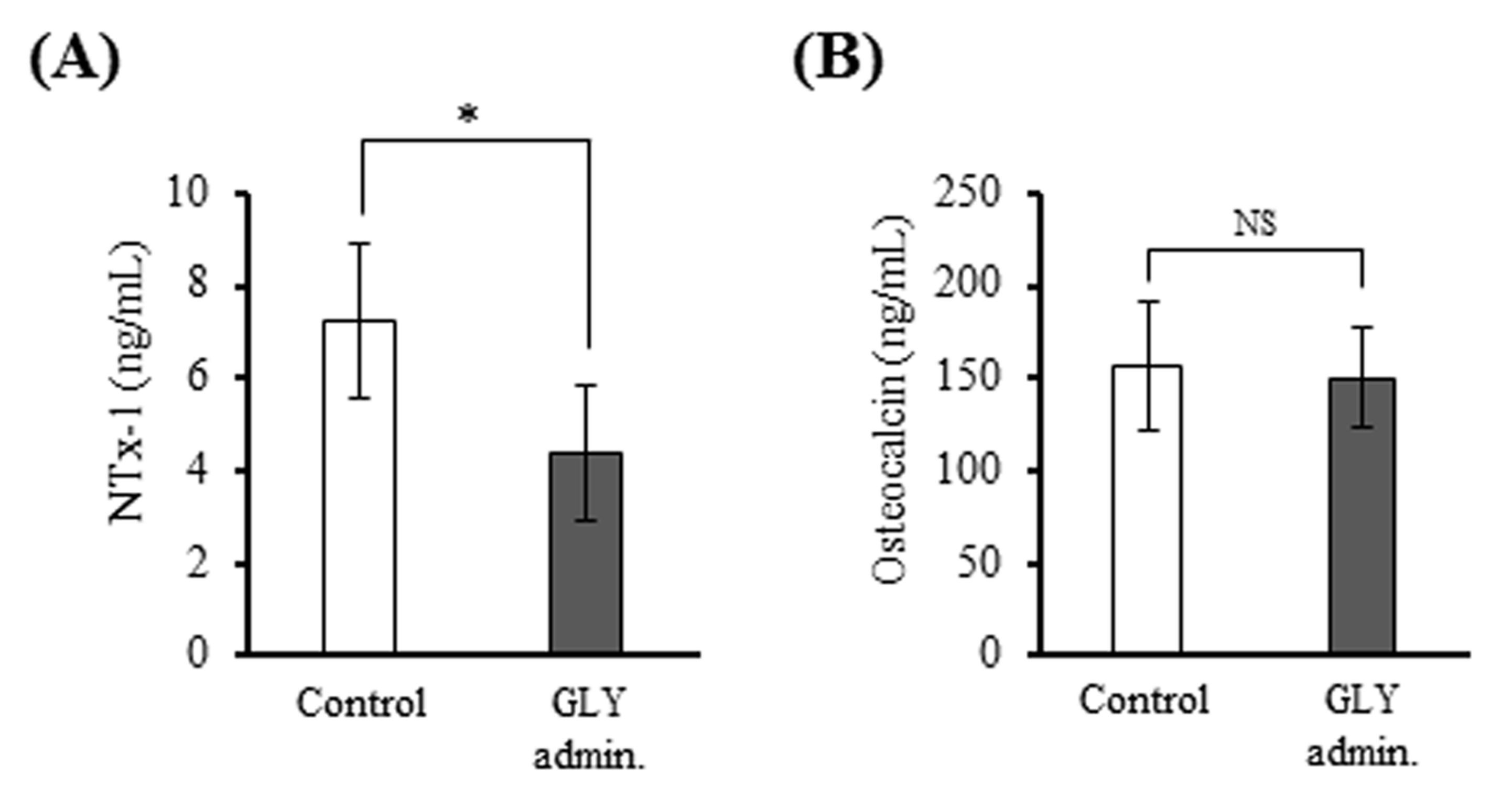
3.6. GLY Extracts Decreased Serum NTx-1 Level in Rat Experimental Periodontitis
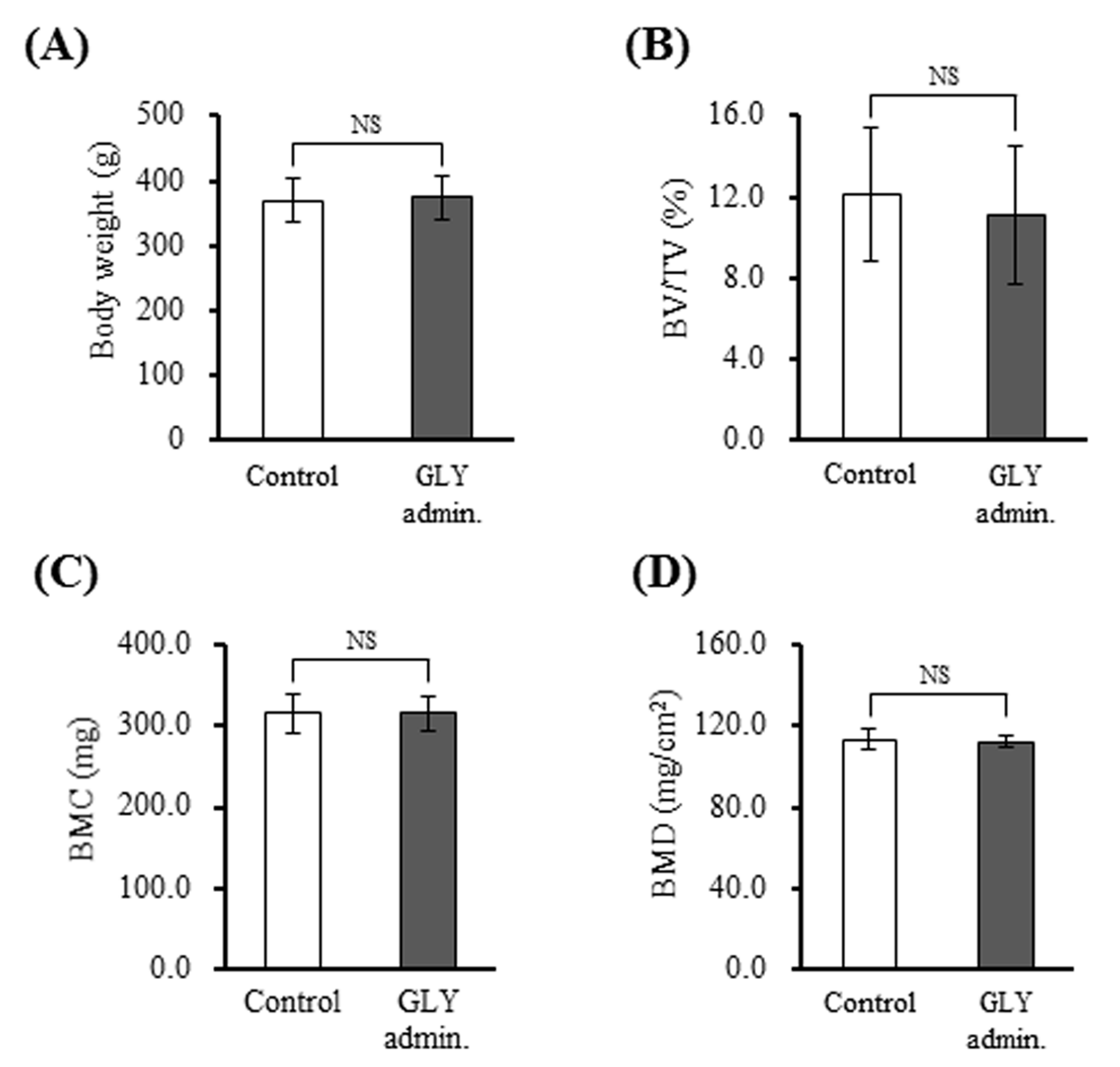
3.7. GLY Extracts Not Affect Bone Structure and Bone Mineral Density in Rat with Experimental Periodontitis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Isola, G.; Polizzi, A.; Alibrandi, A.; Williams, R.C.; Leonardi, R. Independent impact of periodontitis and cardiovascular disease on elevated soluble urokinase-type plasminogen activator receptor (suPAR) levels. J. Periodontol. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Patini, R.; Ferlito, S.; Alibrandi, A.; Palazzo, G. Association among serum and salivary A. actinomycetemcomitans specific immunoglobulin antibodies and periodontitis. BMC Oral Health 2020, 20, 283. [Google Scholar] [CrossRef] [PubMed]
- Bartold, P.M.; Cantley, M.D.; Haynes, D.R. Mechanisms and control of pathologic bone loss in periodontitis. Periodontol. 2000 2010, 53, 55–69. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Jia, Y.; Xiao, Y. Cathepsin K: A therapeutic target for bone diseases. Biochem. Biophys. Res. Commun. 2009, 380, 721–723. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, T. Regulators of osteoclast differentiation and cell-cell fusion. Keio J. Med. 2011, 60, 101–105. [Google Scholar] [CrossRef]
- Zhang, C.; Dou, C.E.; Xu, J.; Dong, S. DC-STAMP, the key fusion-mediating molecule in osteoclastogenesis. J. Cell Physiol. 2014, 229, 1330–1335. [Google Scholar] [CrossRef]
- Yagi, M.; Miyamoto, T.; Toyama, Y.; Suda, T. Role of DC-STAMP in cellular fusion of osteoclasts and macrophage giant cells. J. Bone Miner. Metab. 2006, 24, 355–358. [Google Scholar] [CrossRef]
- Zhao, Q.; Wang, X.; Liu, Y.; He, A.; Jia, R. NFATc1: Functions in osteoclasts. Int. J. Biochem. Cell Biol. 2010, 42, 576–579. [Google Scholar] [CrossRef]
- Seto, H.; Ohba, H.; Tokunaga, K.; Hama, H.; Horibe, M.; Nagata, T. Topical administration of simvastatin recovers alveolar bone loss in rats. J. Periodontal. Res. 2008, 43, 261–267. [Google Scholar] [CrossRef]
- Tokunaga, K.; Seto, H.; Ohba, H.; Mihara, C.; Hama, H.; Horibe, M.; Yoneda, S.; Nagata, T. Topical and intermittent application of parathyroid hormone recovers alveolar bone loss in rat experimental periodontitis. J. Periodontal. Res. 2011, 46, 655–662. [Google Scholar] [CrossRef]
- Wada-Mihara, C.; Seto, H.; Ohba, H.; Tokunaga, K.; Kido, J.I.; Nagata, T.; Naruishi, K. Local administration of calcitonin inhibits alveolar bone loss in an experimental periodontitis in rats. Biomed. Pharmacother. 2018, 97, 765–770. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Hao, D.; Zhang, Q.; Chen, B.; Zhang, R.; Wang, Y.; Yang, H. Natural products for treatment of bone erosive diseases: The effects and mechanisms on inhibiting osteoclastogenesis and bone resorption. Int. Immunopharmacol. 2016, 36, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Martínez, C.C.; Gómez, M.D.; Oh, M.S. Use of traditional herbal medicine as an alternative in dental treatment in Mexican dentistry: A review. Pharmaceutic. Biol. 2017, 55, 1992–1998. [Google Scholar] [CrossRef] [PubMed]
- Safiaghdam, H.; Oveissi, V.; Bahramsoltani, R.; Farzaei, M.H.; Rahimi, R. Medicinal plants for gingivitis: A review of clinical trials. Iran J. Basic Med. Sci. 2018, 21, 978–991. [Google Scholar] [PubMed]
- Yonezawa, T.; Hasegawa, S.; Asai, M.; Ninomiya, T.; Sasaki, T.; Cha, B.Y.; Teruya, T.; Ozawa, H.; Yagasaki, K.; Nagai, K.; et al. Harmine, a β-carboline alkaloid, inhibits osteoclast differentiation and bone resorption in vitro and in vivo. Eur. J. Pharmacol. 2011, 650, 511–518. [Google Scholar] [CrossRef]
- Lee, J.W.; Kobayashi, Y.; Nakamichi, Y.; Udagawa, N.; Takahashi, N.; Im, N.K.; Seo, H.J.; Jeon, W.B.; Yonezawa, T.; Cha, B.Y.; et al. Alisol-B, a novel phyto-steroid, suppresses the RANKL-induced osteoclast formation and prevents bone loss in mice. Biochem. Pharmacol. 2010, 80, 352–361. [Google Scholar] [CrossRef]
- Kim, H.J.; Hong, J.; Jung, J.W.; Kim, T.H.; Kim, J.A.; Kim, Y.H.; Kim, S.Y. Gymnasterkoreayne F inhibits osteoclast formation by suppressing NFATc1 and DC-STAMP expression. Int. Immunopharmacol. 2010, 10, 1440–1447. [Google Scholar] [CrossRef]
- Surathu, N.; Kurumathur, A.V. Traditional therapies in the management of periodontal disease in India and China. Periodontol. 2000 2011, 56, 14–24. [Google Scholar] [CrossRef]
- Veilleux, M.P.; Moriyama, S.; Yoshioka, M.; Hinode, D.; Grenier, D. A review of evidence for a therapeutic application of traditional Japanese Kampo medicine for oral diseases/disorders. Medicines 2018, 5, 35. [Google Scholar] [CrossRef]
- Takeda, O.; Toyama, T.; Watanabe, K.; Sato, T.; Sasaguri, K.; Akimoto, S.; Sato, S.; Kawata, T.; Hamada, N. Ameliorating effects of Juzentaihoto on restraint stress and P. gingivalis-induced alveolar bone loss. Arch. Oral Biol. 2014, 59, 1130–1138. [Google Scholar] [CrossRef]
- Fournier-Larente, J.; Azelmat, J.; Yoshioka, M.; Hinode, D.; Grenier, D. The daiokanzoto (TJ-84) kampo formulation reduces virulence factor gene expression in Porphyromonas gingivalis and possesses anti-inflammatory and anti-protease activities. PLoS ONE 2016, 11, e0148860. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.S.; Wu, C.C.; Lee, H.Z.; Hsieh, W.T.; Tang, F.Y.; Bau, D.T.; Lai, K.C.; Lien, J.C.; Chung, J.G. Suppression of the TNF-alpha level is mediated by Gan-Lu-Yin (traditional Chinese medicine) in human oral cancer cells through the NF-kappa B, AKT, and ERK-dependent pathways. Environ. Toxicol. 2016, 31, 1196–1205. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.C.; Pan, C.H.; Lai, M.T.; Chang, S.J.; Chung, J.G.; Wu, C.H. Gan-Lu-Yin Inhibits Proliferation and Migration of Murine WEHI-3 Leukemia Cells and Tumor Growth in BALB/C Allograft Tumor Model. Evid. Based Compl. Alter. Med. 2013, 2013, 684071. [Google Scholar] [CrossRef] [PubMed]
- Chien, Y.C.; Sheu, M.J.; Wu, C.H.; Lin, W.H.; Chen, Y.Y.; Cheng, P.L.; Cheng, H.C. A Chinese herbal formula “Gan-Lu-Yin” suppresses vascular smooth muscle cell migration by inhibiting matrix metalloproteinase-2/9 through the PI3K/AKT and ERK signaling pathways. BMC Compl. Altern. Med. 2012, 12, 137. [Google Scholar] [CrossRef]
- Pan, C.H.; Hsieh, I.C.; Liu, F.C.; Hsieh, W.T.; Sheu, M.J.; Koizumi, A.; Wu, C.H. Effects of a Chinese herbal health formula, “Gan-Lu-Yin”, on angiogenesis. J. Agric. Food Chem. 2010, 58, 7685–7692. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, X.C.; Bao, X.F.; Hu, M.; Yu, W.X. Effects of Porphyromonas gingivalis lipopolysaccharide on osteoblast-osteoclast bidirectional EphB4-EphrinB2 signaling. Exp. Ther. Med. 2014, 7, 80–84. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Messora, M.R.; Pereira, L.J.; Foureaux, R.; Oliveira, L.F.; Sordi, C.G.; Alves, A.J.; Napimoga, M.H.; Nagata, M.J.; Ervolino, E.; Furlaneto, F.A. Favourable effects of Bacillus subtilis and Bacillus licheniformis on experimental periodontitis in rats. Arch. Oral Biol. 2016, 66, 108–119. [Google Scholar] [CrossRef]
- Seto, H.; Toba, Y.; Takada, Y.; Kawakami, H.; Ohba, H.; Hama, H.; Horibe, M.; Nagata, T. Milk basic protein increases alveolar bone formation in rat experimental periodontitis. J. Periodontal. Res. 2007, 42, 85–89. [Google Scholar] [CrossRef]
- Hashimura, S.; Kido, J.; Matsuda, R.; Yokota, M.; Matsui, H.; Inoue-Fujiwara, M.; Inagaki, Y.; Hidaka, M.; Tanaka, T.; Tsutsumi, T.; et al. A low level of lysophosphatidic acid in human gingival crevicular fluid from patients with periodontitis due to high soluble lysophospholipase activity: Its potential protective role on alveolar bone loss by periodontitis. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2020, 1865, 158698. [Google Scholar] [CrossRef]
- Vargas-Sanchez, P.K.; Moro, M.G.; Santos, F.A.D.; Anbinder, A.L.; Kreich, E.; Moraes, R.M.; Padilha, L.; Kusiak, C.; Scomparin, D.X.; Franco, G.C.N. Agreement, correlation, and kinetics of the alveolar bone-loss measurement methodologies in a ligature-induced periodontitis animal model. J. Appl. Oral Sci. 2017, 25, 490–497. [Google Scholar] [CrossRef]
- De Molon, R.S.; Park, C.H.; Jin, Q.; Sugai, J.; Cirelli, J.A. Characterization of ligature-induced experimental periodontitis. Microsc. Res. Tech. 2018, 81, 1412–1421. [Google Scholar] [CrossRef] [PubMed]
- Lin, I.H.; Lee, M.C.; Chuang, W.C. Application of LC/MS and ICP/MS for establishing the fingerprint spectrum of the traditional Chinese medicinal preparation Gan-Lu-Yin. J. Sep. Sci. 2006, 29, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Li, C.; Du, G.; Cao, Z. Protective effects of baicalin on ligature-induced periodontitis in rats. J. Periodontal. Res. 2008, 43, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Zhu, W.; Wu, Q.; Zhang, Q.; Guo, S.; Liu, T.; Li, S.; Chen, X.; Peng, D.; Ouyang, Z. Glycyrrhizic acid suppresses osteoclast differentiation and postmenopausal osteoporosis by modulating the NF-κB, ERK, and JNK signaling pathways. Eur. J. Pharmacol. 2019, 859, 172550. [Google Scholar] [CrossRef] [PubMed]
- Ang, E.S.; Yang, X.; Chen, H.; Liu, Q.; Zheng, M.H.; Xu, J. Naringin abrogates osteoclastogenesis and bone resorption via the inhibition of RANKL-induced NF-κB and ERK activation. FEBS Lett. 2011, 585, 2755–2762. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.; Bak, E.J.; Kim, M.; Kim, J.M.; Chung, W.Y.; Cha, J.H.; Yoo, Y.J. Wogonin inhibit osteoclast formation induced by lipopolysaccharide. Phytother. Res. 2010, 24, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Eyre, D.R. Bone biomarkers as tools in osteoporosis management. Spine (Phila Pa 1976) 1997, 22, 17S–24S. [Google Scholar] [CrossRef]
- Wen, X.; Yi, L.Z.; Liu, F.; Wei, J.H.; Xue, Y. The role of cathepsin K in oral and maxillofacial disorders. Oral Dis. 2016, 22, 109–115. [Google Scholar] [CrossRef]
- Li, Z.; Chen, C.; Zhu, X.; Li, Y.; Yu, R.; Xu, W. Glycyrrhizin suppresses RANKL-induced osteoclastogenesis and oxidative stress through inhibiting NF-kB and MAPK and activating AMPK/Nrf2. Calcif. Tissue Int. 2018, 103, 324–337. [Google Scholar] [CrossRef]
- Kim, M.H.; Ryu, S.Y.; Bae, M.A.; Choi, J.S.; Min, Y.K.; Kim, S.H. Baicalein inhibits osteoclast differentiation and induces mature osteoclast apoptosis. Food Chem. Toxicol. 2008, 46, 3375–3382. [Google Scholar] [CrossRef]
- Negishi-Koga, T.; Takayanagi, H. Ca2+-NFATc1 signaling is an essential axis of osteoclast differentiation. Immunol. Rev. 2009, 231, 241–256. [Google Scholar] [CrossRef] [PubMed]
- Geng, X.; Yang, L.; Zhang, C.; Qin, H.; Liang, Q. Wogonin inhibits osteoclast differentiation by inhibiting NFATc1 translocation into the nucleus. Exp. Ther. Med. 2015, 10, 1066–1070. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Huang, X.; Zhao, J.; Gu, Z. Preliminary identification of potential PDZ-domain proteins downstream of ephrin B2 during osteoclast differentiation of RAW264.7 cells. Int. J. Mol. Med. 2011, 27, 669–677. [Google Scholar] [PubMed]
- Ikeda, K.; Takeshita, S. Factors and mechanisms involved in the coupling from bone resorption to formation: How osteoclasts talk to osteoblasts. J. Bone Metab. 2014, 21, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Irie, N.; Takada, Y.; Shimoda, K.; Miyamoto, T.; Nishiwaki, T.; Suda, T.; Matsuo, K. Bidirectional ephrinB2-EphB4 signaling controls bone homeostasis. Cell Metab. 2006, 4, 111–121. [Google Scholar] [CrossRef]
- Yang, H.; Wen, Q.; Xue, J.; Ding, Y. Alveolar bone regeneration potential of a traditional Chinese medicine, Bu-Shen-Gu-Chi-Wan, in experimental periodontitis. J. Periodontal. Res. 2014, 49, 382–389. [Google Scholar] [CrossRef]
- Zhou, T.; Chen, D.; Li, Q.; Sun, X.; Song, Y.; Wang, C. Curcumin inhibits inflammatory response and bone loss during experimental periodontitis in rats. Acta Odontol. Scand. 2013, 71, 349–356. [Google Scholar] [CrossRef]
- Luo, W.; Wang, C.Y.; Jin, L. Baicalin downregulates Porphyromonas gingivalis lipopolysaccharide-upregulated IL-6 and IL-8 expression in human oral keratinocytes by negative regulation of TLR signaling. PLoS ONE 2012, 7, e51008. [Google Scholar] [CrossRef]
- Ku, S.K.; Bae, J.S. Baicalin, baicalein and wogonin inhibits high glucose-induced vascular inflammation in vitro and in vivo. BMB Rep. 2015, 48, 519–524. [Google Scholar] [CrossRef]
- Kim, Y.W.; Zhao, R.J.; Park, S.J.; Lee, J.R.; Cho, I.J.; Yang, C.H.; Kim, S.G.; Kim, S.C. Anti-inflammatory effects of liquiritigenin as a consequence of the inhibition of NF-kB-dependent iNOS and proinflammatory cytokines production. Br. J. Pharmacol. 2008, 154, 165–173. [Google Scholar] [CrossRef]
- Liu, L.; Zuo, Z.; Lu, S.; Liu, A.; Liu, X. Naringin attenuates diabetic retinopathy by inhibiting inflammation, oxidative stress and NF-kB activation in vivo and in vitro. Iran J. Basic Med. Sci. 2017, 20, 813–821. [Google Scholar] [PubMed]
- Hienz, S.A.; Paliwal, S.; Ivanovski, S. Mechanisms of Bone Resorption in Periodontitis. J. Immunol. Res. 2015, 2015, 615486. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, S.R.; Padhye, A.M. Future prospects of systemic host modulatory agents in periodontal therapy. Br. Dent. J. 2013, 214, 467–471. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inagaki, Y.; Kido, J.-i.; Nishikawa, Y.; Kido, R.; Sakamoto, E.; Bando, M.; Naruishi, K.; Nagata, T.; Yumoto, H. Gan-Lu-Yin (Kanroin), Traditional Chinese Herbal Extracts, Reduces Osteoclast Differentiation In Vitro and Prevents Alveolar Bone Resorption in Rat Experimental Periodontitis. J. Clin. Med. 2021, 10, 386. https://doi.org/10.3390/jcm10030386
Inagaki Y, Kido J-i, Nishikawa Y, Kido R, Sakamoto E, Bando M, Naruishi K, Nagata T, Yumoto H. Gan-Lu-Yin (Kanroin), Traditional Chinese Herbal Extracts, Reduces Osteoclast Differentiation In Vitro and Prevents Alveolar Bone Resorption in Rat Experimental Periodontitis. Journal of Clinical Medicine. 2021; 10(3):386. https://doi.org/10.3390/jcm10030386
Chicago/Turabian StyleInagaki, Yuji, Jun-ichi Kido, Yasufumi Nishikawa, Rie Kido, Eijiro Sakamoto, Mika Bando, Koji Naruishi, Toshihiko Nagata, and Hiromichi Yumoto. 2021. "Gan-Lu-Yin (Kanroin), Traditional Chinese Herbal Extracts, Reduces Osteoclast Differentiation In Vitro and Prevents Alveolar Bone Resorption in Rat Experimental Periodontitis" Journal of Clinical Medicine 10, no. 3: 386. https://doi.org/10.3390/jcm10030386
APA StyleInagaki, Y., Kido, J.-i., Nishikawa, Y., Kido, R., Sakamoto, E., Bando, M., Naruishi, K., Nagata, T., & Yumoto, H. (2021). Gan-Lu-Yin (Kanroin), Traditional Chinese Herbal Extracts, Reduces Osteoclast Differentiation In Vitro and Prevents Alveolar Bone Resorption in Rat Experimental Periodontitis. Journal of Clinical Medicine, 10(3), 386. https://doi.org/10.3390/jcm10030386




