Trends in Hospital Admissions and Death Causes in Patients with Systemic Lupus Erythematosus: Spanish National Registry
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Hospital Admissions
3.3. Deaths
3.4. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lisnevskaia, L.; Murphy, G.; Isenberg, D. Systemic lupus erythematosus. Lancet 2014, 384, 1878–1888. [Google Scholar] [CrossRef]
- Kaul, A.; Gordon, C.; Crow, M.K.; Touma, Z.; Urowitz, M.B.; van Vollenhoven, R.; Ruiz-Irastorza, G.; Hughes, G. Systemic lupus erythematosus. Nat. Rev. Dis. Primers 2016, 2, 16039. [Google Scholar] [CrossRef]
- Cervera, R.; Khamashta, M.A.; Font, J.; Sebastiani, G.D.; Gil, A.; Lavilla, P.; Mejía, J.C.; Aydintug, A.O.; Chwalinska-Sadowska, H.; de Ramón, E.; et al. European Working Party on Systemic Lupus Erythematosus. Morbidity and mortality in systemic lupus erythematosus during a 10-year period: A comparison of early and late manifestations in a cohort of 1000 patients. Medicine 2003, 82, 299–308. [Google Scholar] [CrossRef]
- Bernatsky, S.; Boivin, J.F.; Joseph, L.; Manzi, S.; Ginzler, E.; Gladman, D.D.; Urowitz, M.; Fortin, P.R.; Petri, M.; Barr, S.; et al. Mortality in systemic lupus erythematosus. Arthritis Rheumatol. 2006, 54, 2550–2557. [Google Scholar] [CrossRef] [PubMed]
- Yen, E.Y.; Singh, R.R. Brief Report: Lupus-An Unrecognized Leading Cause of Death in Young Females: A Population-Based Study Using Nationwide Death Certificates, 2000–2015. Arthritis Rheumatol. 2018, 70, 1251–1255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanouriakis, A.; Kostopoulou, M.; Alunno, A.; Aringer, M.; Bajema, I.; Boletis, J.N.; Cervera, R.; Doria, A.; Gordon, C.; Govoni, M.; et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 736–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnaud, L.; Tektonidou, M.G. Long-term outcomes in systemic lupus erythematosus: Trends over time and major contributors. Rheumatology 2020, 59, v29–v38. [Google Scholar] [CrossRef] [PubMed]
- Fors Nieves, C.E.; Izmirly, P.M. Mortality in Systemic Lupus Erythematosus: An Updated Review. Curr. Rheumatol. Rep. 2016, 18, 21. [Google Scholar] [CrossRef] [PubMed]
- Ingvarsson, R.F.; Landgren, A.J.; Bengtsson, A.A.; Jönsen, A. Good survival rates in systemic lupus erythematosus in southern Sweden, while the mortality rate remains increased compared with the population. Lupus 2019, 28, 1488–1494. [Google Scholar] [CrossRef] [PubMed]
- Yurkovich, M.; Vostretsova, K.; Chen, W.; Aviña-Zubieta, J.A. Overall and cause-specific mortality in patients with systemic lupus erythematosus: A meta-analysis of observational studies. Arthritis Care Res. 2014, 66, 608–616. [Google Scholar] [CrossRef]
- Tselios, K.; Gladman, D.D.; Sheane, B.J.; Su, J.; Urowitz, M. All-cause, cause-specific and age-specific standardised mortality ratios of patients with systemic lupus erythematosus in Ontario, Canada over 43 years (1971–2013). Ann. Rheum. Dis. 2019, 7, 802–806. [Google Scholar] [CrossRef]
- Singh, R.R.; Yen, E.Y. SLE mortality remains disproportionately high, despite improvements over the last decade. Lupus 2018, 27, 1577–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, E.Y.; Shaheen, M.; Woo, J.M.P.; Mercer, N.; Li, N.; McCurdy, D.K.; Karlamangla, A.; Singh, R.R. 46-Year Trends in Systemic Lupus Erythematosus Mortality in the United States, 1968 to 2013: A Nationwide Population-Based Study. Ann. Intern. Med. 2017, 167, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Goss, L.B.; Ortiz, J.R.; Okamura, D.M.; Hayward, K.; Goss, C.H. Significant Reductions in Mortality in Hospitalized Patients with Systemic Lupus Erythematosus in Washington State from 2003 to 2011. PLoS ONE 2015, 10, e0128920. [Google Scholar] [CrossRef]
- Urowitz, M.B.; Gladman, D.D.; Tom, B.D.; Ibañez, D.; Farewell, V.T. Changing patterns in mortality and disease outcomes for patients with systemic lupus erythematosus. J. Rheumatol. 2008, 35, 2152–2158. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Choi, S.J.; Ji, J.D.; Song, G.G. Overall and cause-specific mortality in systemic lupus erythematosus: An updated meta-analysis. Lupus 2016, 25, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Dhillon, N.; Pope, J. All-cause hospitalizations in systemic lupus erythematosus from a large Canadian referral centre. Rheumatology 2013, 52, 905–909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosa, G.P.D.; Ortega, M.F.; Teixeira, A.; Espinosa, G.; Cervera, R. Causes and factors related to hospitalizations in patients with systemic lupus erythematosus: Analysis of a 20-year period (1995–2015) from a single referral centre in Catalonia. Lupus 2019, 28, 1158–1166. [Google Scholar] [CrossRef]
- Anastasiou, C.; Dulai, O.; Baskaran, A.; Proudfoot, J.; Verhaegen, S.; Kalunian, K. Immunosuppressant use and hospitalisations in adult patients with systemic lupus erythematosus admitted to a tertiary academic medical centre. Lupus Sci. Med. 2018, 5, e000249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, O.; Markov ADrob, Y.; Maslakov, I.; Tishler, M.; Amit-Vazina, M. All-cause hospitalizations in systemic lupus erythematosus from a single medical center in Israel. Rheumatol. Int. 2018, 38, 1841–1846. [Google Scholar] [CrossRef]
- Liang, H.; Pan, H.F.; Tao, J.H.; Ye, D.Q. Causes and Factors Associated with Frequent Hospitalization in Chinese Patients with Systemic Lupus Erythematosus: An Ambispective Cohort Study. Med. Sci. Monit. 2019, 25, 8061–8068. [Google Scholar] [CrossRef] [PubMed]
- Dzifa, D.; Boima, V.; Yorke, E.; Yawson, A.; Ganu, V.; Mate-Kole, C. Predictors and outcome of systemic lupus erythematosus (SLE) admission rates in a large teaching hospital in sub-Saharan Africa. Lupus 2018, 27, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Busch, R.W.; Kay, S.D.; Voss, A. Hospitalizations among Danish SLE patients: A prospective study on incidence, causes of admission and risk factors in a population-based cohort. Lupus 2018, 27, 165–171. [Google Scholar] [CrossRef] [Green Version]
- Selvananda, S.; Chong, Y.Y.; Thundyil, R.J. Disease activity and damage in hospitalized lupus patients: A Sabah perspective. Lupus 2020, 29, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Gu, K.; Gladman, D.D.; Su, J.; Urowitz, M.B. Hospitalizations in Patients with Systemic Lupus Erythematosus in an Academic Health Science Center. J. Rheumatol. 2017, 44, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, E. Hospitalization and mortality of patients with systemic lupus erythematosus. J. Rheumatol. 2006, 33, 1770–1774. [Google Scholar]
- Rees, F.; Doherty, M.; Grainge, M.; Davenport, G.; Lanyon, P.; Zhang, W. The incidence and prevalence of systemic lupus erythematosus in the UK, 1999–2012. Ann. Rheum. Dis. 2016, 75, 136–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piga, M.; Casula, L.; Perra, D.; Sanna, S.; Floris, A.; Antonelli, A.; Cauli, A.; Mathieu, A. Population-based analysis of hospitalizations in a West-European region revealed major changes in hospital utilization for patients with systemic lupus erythematosus over the period 2001–2012. Lupus 2016, 25, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, C.; Trupin, L.; Glidden, D.V.; Li, J.; Gianfrancesco, M.; Shiboski, S.; Schmajuk, G.; Yazdany, J. Mortality among Hospitalized Individuals with Systemic Lupus Erythematosus in the United States between 2006 and 2016. Arthritis Care Res. 2020. [Google Scholar] [CrossRef]
- Anver, H.; Dubey, S.; Fox, J. Changing trends in mortality in systemic lupus erythematosus? An analysis of SLE inpatient mortality at University Hospital Coventry and Warwickshire NHS Trust from 2007 to 2016. Rheumatol. Int. 2019, 39, 2069–2075. [Google Scholar] [CrossRef] [PubMed]
- Jakes, R.W.; Bae, S.C.; Louthrenoo, W.; Mok, C.C.; Navarra, S.V.; Kwon, N.W. Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: Prevalence, incidence, clinical features, and mortality. Arthritis Care Res. 2012, 64, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Fei, Y.; Shi, X.; Gan, F.; Li, X.; Zhang, W.; Li, M.; Hou, Y.; Zhang, X.; Zhao, Y.; Zeng, X.; et al. Death causes and pathogens analysis of systemic lupus erythematosus during the past 26 years. Clin. Rheumatol. 2014, 33, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Zhen, J.; Ling-Yun, S.; Yao-Hong, Z.; Xiang-Dang, W.; Jie-Ping, P.; Miao-Jia, Z.; Juan, T.; Yu, Z.; Kui-Lin, T.; Jing, L.; et al. Death-related factors of systemic lupus erythematosus patients associated with the course of disease in Chinese populations: Multicenter and retrospective study of 1958 inpatients. Rheumatol. Int. 2013, 33, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Vizcaya, A.; Isenberg, D. Analysis of trends and causes of death in SLE patients over a 40-years period in a cohort of patients in the United Kingdom. Lupus 2021, 30, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Cleveland, J.D. Hospitalized Infections in Lupus: A Nationwide Study of Types of Infections, Time Trends, Health Care Utilization, and In-Hospital Mortality. Arthritis Rheumatol. 2021, 73, 617–630. [Google Scholar] [CrossRef]
- Symmons, D.P.; Gabriel, S.E. Epidemiology of CVD in rheumatic disease, with a focus on RA and SLE. Nat. Rev. Rheumatol. 2011, 7, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Borchers, A.T.; Keen, C.L.; Shoenfeld, Y.; Gershwin, M.E. Surviving the butterfly and the wolf: Mortality trends in systemic lupus erythematosus. Autoimmun. Rev. 2004, 3, 423–453. [Google Scholar] [CrossRef] [PubMed]
- Urowitz, M.B.; Ibañez, D.; Gladman, D.D. Atherosclerotic vascular events in a single large lupus cohort: Prevalence and risk factors. J. Rheumatol. 2007, 34, 70–75. [Google Scholar] [PubMed]
- Danza, A.; Ruiz-Irastorza, G. Infection risk in systemic lupus erythematosus patients: Susceptibility factors and preventive strategies. Lupus 2013, 22, 1286–1294. [Google Scholar] [CrossRef]
- Ladouceur, A.; Clarke, A.E.; Ramsey-Goldman, R.; Bernatsky, S. Malignancies in systemic lupus erythematosus: An update. Curr. Opin. Rheumatol. 2019, 31, 678–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernatsky, S.; Ramsey-Goldman, R.; Labrecque, J.; Joseph, L.; Boivin, J.F.; Petri, M.; Zoma, A.; Manzi, S.; Urowitz, M.B.; Gladman, D.; et al. Cancer risk in systemic lupus: An updated international multi-centre cohort study. J. Autoimmun. 2013, 42, 130–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreiber, R.D.; Old, L.J.; Smyth, M.J. Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science 2011, 331, 1565–1570. [Google Scholar] [CrossRef] [Green Version]
- Vial, T.; Descotes, J. Immunosuppressive drugs and cancer. Toxicology 2003, 185, 229–240. [Google Scholar] [CrossRef]
- Alonso, M.D.; Llorca, J.; Martinez-Vazquez, F.; Miranda-Filloy, J.A.; Diaz de Teran, T.; Dierssen, T.; Rodriguez, T.R.V.; Gomez-Acebo, I.; Blanco, R.; Gonzalez-Gay, M.A. Systemic lupus erythematosus in northwestern Spain: A 20-year epidemiologic study. Medicine 2011, 90, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Ugarte, A.; Danza, A.; Ruiz-Irastorza, G. Glucocorticoids and antimalarials in systemic lupus erythematosus: An update and future directions. Curr. Opin. Rheumatol. 2018, 30, 482–489. [Google Scholar] [CrossRef]
- Ruiz-Arruza, I.; Lozano, J.; Cabezas-Rodriguez, I.; Medina, J.-A.; Ugarte, A.; Erdozain, J.-G.; Ruiz-Irastorza, G. Restrictive Use of Oral Glucocorticoids in Systemic Lupus Erythematosus and Prevention of Damage Without Worsening Long-Term Disease Control: An Observational Study. Arthritis Care Res. 2018, 70, 582–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Overall | 1997–2000 | 2001–2005 | 2006–2010 | 2011–2015 | |
| Patients (n) | 43,432 | 8304 | 12,348 | 15,051 | 17,257 |
| Gender female (%, CI) | 83.3 (83.1–83.6) | 82.8 (82.2–83.4) | 83 (82.5–83.5) | 83.4 (83–83.9) | 83 (82.6–83.4) |
| Age (years) (Mean, SD) | 46.5 (18.7) | 41.1 (18.1) | 44 (18.3) * | 46.6 (18.5) * | 51 (18.3) * T |
| Admissions (n) | 99,859 | 15,807 | 24,204 | 27,781 | 31,977 |
| Average stay (days) (Mean, SD) | 9.1 (13.1) | 9.4 (12.7) | 9.5 (14.2) | 9.3 (12.8) | 8.5 (12.6) * T |
| Readmission rate (%, CI) | 17.6 (17.4–17.8) | 18.3 (17.7–18.9) | 18.6 (18.1–19.1) | 17.7 (17.3–18.2) * | 16.4 (16–16.8) * T |
| Deaths (n, %) | 2786 (6.41) | 351 (4.22) | 659 (5.34) | 798 (5.30) * | 978 (5.67) * T |
| Mortality rate per admission (%, CI) | 2.79 (2.7–2.9) | 2.22 (2.0–2.46) | 2.72 (2.52–2.94) * | 2.86 (2.67–3.07) | 3.06 (2.87–3.25) T |
| Overall | 1997–2000 | 2001–2005 | 2006–2010 | 2011–2015 | |
| Active SLE | |||||
| Admissions n (%) | 31,539 (31.6) | 7440 (47.1) | 9354 (38.7) * | 8088 (29) * | 6657 (20.8) * T |
| Age (years) (Mean, SD) | 37.6 (16.5) ** | 35.9 (16.3) | 37.1 (16.3) | 37.9 (16.5) | 40 (16.8) T |
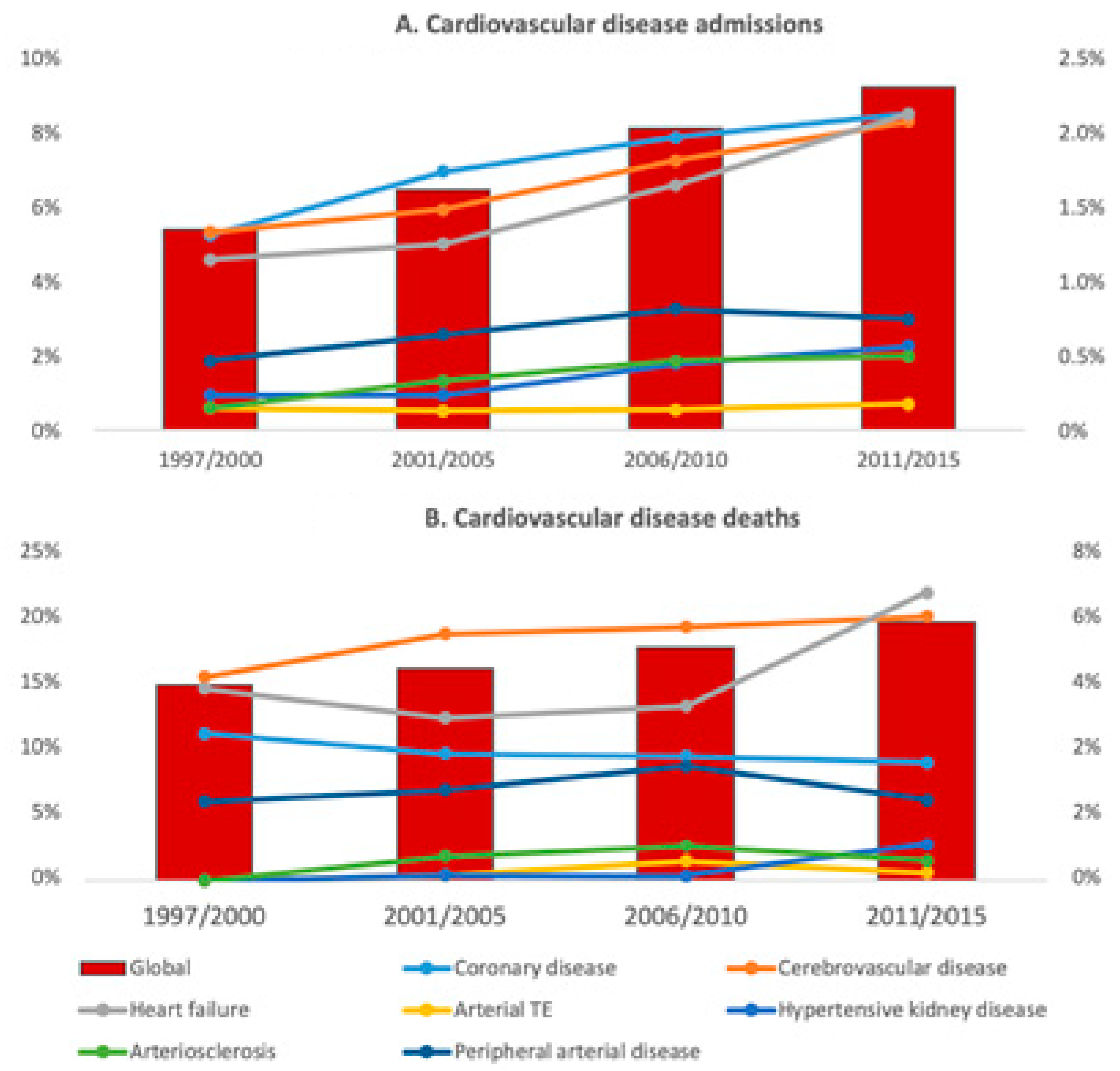
| Cardiovascular disease | |||||
| Admissions n (%) | 7065 (7.1) | 789 (5) | 1448 (6) * | 2096 (7.5) * | 2736 (8.6) * T) |
| Age (years) (Mean, SD) | 59.5 (16.9) | 55.5 (17.6) | 57.1 (16.6) | 59.6 (16.7) | 61.6 (16.6) T |
| Infection | |||||
| Admissions n (%) | 10,865 (10.9) | 1292 (8.2) | 2295 (9.5) * | 3137 (11.3) * | 4141 (13) * T |
| Age (years) (Mean, SD) | 52.1 (19) | 47.9 (18.8) | 49.7 (18.9) | 50.8 (19.1) | 55.6 (18.4) T |
| Neoplasm | |||||
| Admissions n (%) | 4182 (4.2) | 386 (2.4) | 785 (3.2) * | 1238 (4.4) * | 1773 (5.5) * T |
| Age (years) (Mean, SD) | 56.5 (14.3) | 54.8 (14.4) | 55.8 (14.9) | 55.3 (14.2) | 57.9 (13.9) T |
| Venous thrombo-embolic disease | |||||
| Admissions n (%) | 1069 (1.1) | 174 (1.1) | 277 (1.1) | 268 (1) | 350 (1.1) |
| Age (years) (Mean, SD) | 50.1 (19.0) | 45.1 (18) | 47.9 (18.4) | 51 (18.9) | 53.6 (19.3) T |
| Overall | 1997–2000 | 2001–2005 | 2006–2010 | 2011–2015 | |
|---|---|---|---|---|---|
| Active SLE | |||||
| Deaths (n, % of all deaths) | 363 (13) | 85 (24.2) | 119 (18.1) * | 96 (12) * | 63 (6.4) * T |
| Mortality rate (%) | 1.2 | 1.1 | 1.3 | 1.2 | 0.9 |
| Age (years) (Mean, SD) | 54.5 (19.7) ** | 53.5 (19.9) | 52.3 (19.6) | 55.7 (18.9) | 58.5(20.5) |
| Cardiovascular disease | |||||
| Deaths (n, % of all deaths) | 515 (18.5) | 54 (15.4) | 110 (16.7) | 146 (18.3) | 199 (20.4) T |
| Mortality rate (%) | 7.3 | 6.8 | 7.6 | 7 | 7.3 |
| Age (years) (Mean, SD) | 67 (16.6) | 60 (19.5) | 63.5 (16.9) | 66.9 (16) | 71 (14.8) T |
| Infection | |||||
| Deaths (n, % of all deaths) | 522 (18.7) | 50 (14.3) | 116 (17.6) | 150 (18.8) | 206 (21.1) T |
| Mortality rate (%) | 4.8 | 3.9 | 5.1 | 4.8 | 5 |
| Age (years) (Mean, SD) | 64.5 (17.4) | 62.5 (18.6) | 62.5 (18.3) | 61.9 (18.2) | 68 (15.4) T |
| Neoplasm | |||||
| Deaths (n, % of all deaths) | 327 (11.7) | 26 (7.4) | 66 (10) | 100 (12.5) | 135 (13.8) T |
| Mortality rate (%) | 7.8 | 6.7 | 8.4 | 8.1 | 7.6 |
| Age (years) (Mean, SD) | 63.6 (13.6) | 63 (11.7) | 67.1 (12.6) | 61.6 (14.6) | 63.6 (13.4) |
| Venous thrombo-embolic disease | |||||
| Deaths (n, % of all deaths) | 40 (1.4) | 4 (1.1) | 13 (2) | 7 (0.9) | 16 (1.6) |
| Mortality rate (%) | 3.7 | 2.3 | 4.7 | 2.6 | 4.6 |
| Age (years) (Mean, SD) | 62.3 (16.1) | 54.8 (5.8) | 59.5 (17.8) | 68 (16.5) | 68.9 (15.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Torres, V.; Tarín, C.; Ruiz-Irastorza, G.; Castejón, R.; Gutiérrez-Rojas, Á.; Royuela, A.; Durán-del Campo, P.; Mellor-Pita, S.; Tutor, P.; Rosado, S.; et al. Trends in Hospital Admissions and Death Causes in Patients with Systemic Lupus Erythematosus: Spanish National Registry. J. Clin. Med. 2021, 10, 5749. https://doi.org/10.3390/jcm10245749
Moreno-Torres V, Tarín C, Ruiz-Irastorza G, Castejón R, Gutiérrez-Rojas Á, Royuela A, Durán-del Campo P, Mellor-Pita S, Tutor P, Rosado S, et al. Trends in Hospital Admissions and Death Causes in Patients with Systemic Lupus Erythematosus: Spanish National Registry. Journal of Clinical Medicine. 2021; 10(24):5749. https://doi.org/10.3390/jcm10245749
Chicago/Turabian StyleMoreno-Torres, Víctor, Carlos Tarín, Guillermo Ruiz-Irastorza, Raquel Castejón, Ángela Gutiérrez-Rojas, Ana Royuela, Pedro Durán-del Campo, Susana Mellor-Pita, Pablo Tutor, Silvia Rosado, and et al. 2021. "Trends in Hospital Admissions and Death Causes in Patients with Systemic Lupus Erythematosus: Spanish National Registry" Journal of Clinical Medicine 10, no. 24: 5749. https://doi.org/10.3390/jcm10245749
APA StyleMoreno-Torres, V., Tarín, C., Ruiz-Irastorza, G., Castejón, R., Gutiérrez-Rojas, Á., Royuela, A., Durán-del Campo, P., Mellor-Pita, S., Tutor, P., Rosado, S., Sánchez, E., Martínez-Urbistondo, M., de Mendoza, C., Yebra, M., & Vargas, J.-A. (2021). Trends in Hospital Admissions and Death Causes in Patients with Systemic Lupus Erythematosus: Spanish National Registry. Journal of Clinical Medicine, 10(24), 5749. https://doi.org/10.3390/jcm10245749






