Long-Term Outcome in Systemic Lupus Erythematosus; Knowledge from Population-Based Cohorts
Abstract
1. Introduction
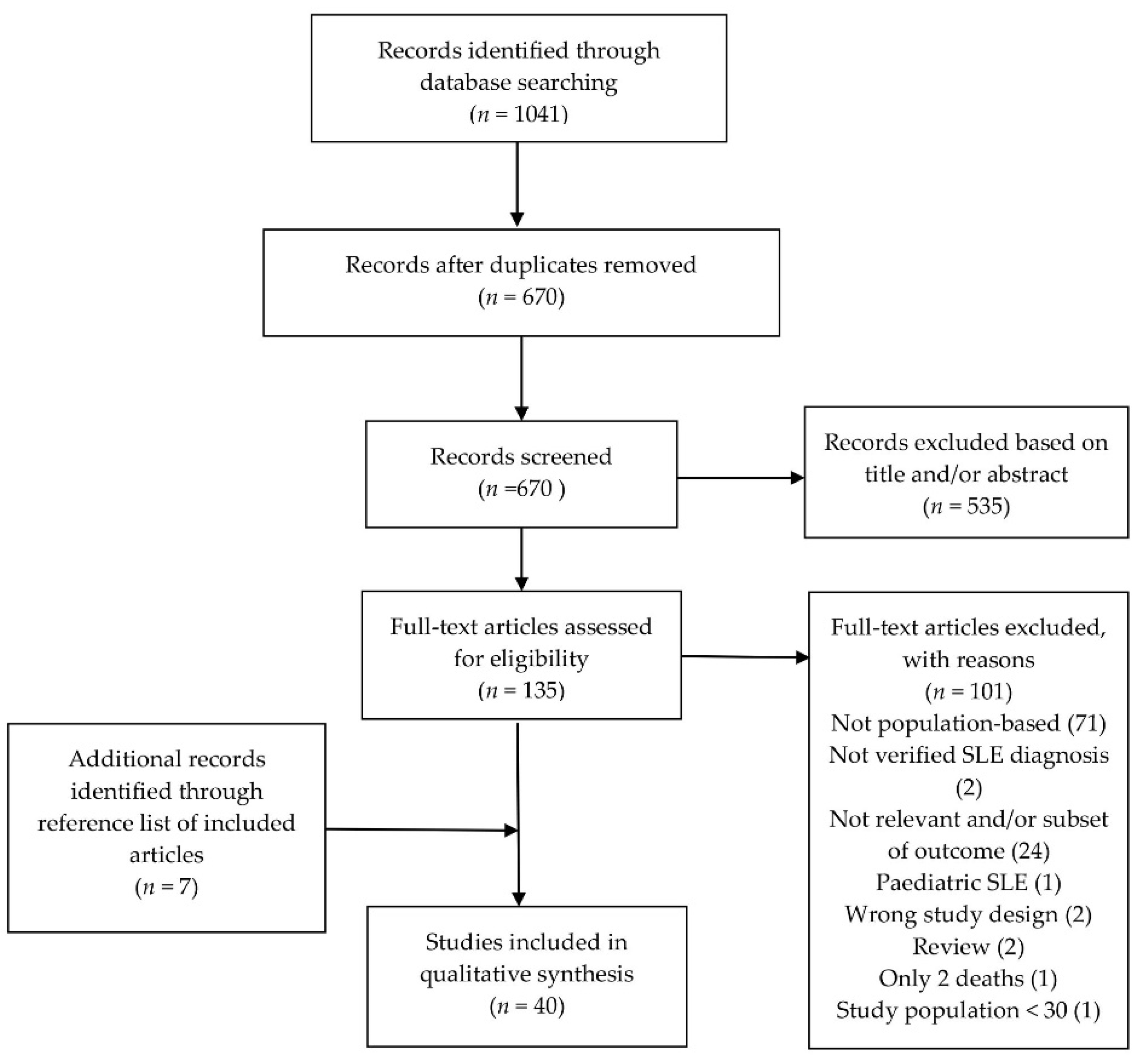
2. Materials and Methods
3. Results
3.1. Standardized Mortality Rate and Survival
3.2. The Main Causes of Death in Systemic Lupus Erythematosus
3.3. End Stage Renal Disase
3.4. Cancer
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rees, F.; Doherty, M.; Grainge, M.; Lanyon, P.; Zhang, W. The worldwide incidence and prevalence of systemic lupus erythematosus: A systematic review of epidemiological studies. Rheumatology 2017, 56, 1945–1961. [Google Scholar] [CrossRef]
- Lerang, K.; Gilboe, I.-M.; Gran, J.T. Differences between rheumatologists and other internists regarding diagnosis and treatment of systemic lupus erythematosus. Rheumatology 2011, 51, 663–669. [Google Scholar] [CrossRef]
- Gergianaki, I.; Fanouriakis, A.; Repa, A.; Tzanakakis, M.; Adamichou, C.; Pompieri, A.; Spirou, G.; Bertsias, A.; Kabouraki, E.; Tzanakis, I.; et al. Epidemiology and burden of systemic lupus erythematosus in a Southern European population: Data from the community-based lupus registry of Crete, Greece. Ann. Rheum. Dis. 2017, 76, 1992–2000. [Google Scholar] [CrossRef]
- Voss, A.; Green, A.; Junker, P. Systemic lupus erythematosus in Denmark: Clinical and epidemiological characterization of a county-based cohort. Scand. J. Rheumatol. 1998, 27, 98–105. [Google Scholar]
- Ingvarsson, R.F.; Bengtsson, A.A.; Jönsen, A. Variations in the epidemiology of systemic lupus erythematosus in southern Sweden. Lupus 2016, 25, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Bayakly, A.R.; Helmick, C.G.; Gordon, C.; Easley, K.; Drenkard, C. The Incidence and Prevalence of Systemic Lupus Erythematosus, 2002–2004: The Georgia Lupus Registry. Arthritis Rheumatol. 2013, 66, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Hochberg, M.C. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997, 40, 1725. [Google Scholar] [CrossRef] [PubMed]
- Voss, A.; Laustrup, H.; Hjelmborg, J.; Junker, P. Survival in systemic lupus erythematosus, 1995–2010. A prospective study in a Danish community. Lupus 2013, 22, 1185–1191. [Google Scholar] [CrossRef]
- Ingvarsson, R.F.; Landgren, A.J.; Bengtsson, A.A.; Jönsen, A. Good survival rates in systemic lupus erythematosus in southern Sweden, while the mortality rate remains increased compared with the population. Lupus 2019, 28, 1488–1494. [Google Scholar] [CrossRef]
- Al-Adhoubi, N.K.; Al-Balushi, F.; Al Salmi, I.; Ali, M.; Al Lawati, T.; Al Lawati, B.S.H.; Abdwani, R.; Al Shamsi, A.; Al Kaabi, J.; Al Mashaani, M.; et al. A multicenter longitudinal study of the prevalence and mortality rate of systemic lupus erythematosus patients in Oman: Oman Lupus Study. Int. J. Rheum. Dis. 2021, 24, 847–854. [Google Scholar] [CrossRef]
- Flower, C.; Hennis, A.J.M.; Hambleton, I.R.; Nicholson, G.D.; Liang, M.H.; the The Barbados National Lupus Registry Group. Systemic lupus erythematosus in an Afro-Caribbean population: Incidence, clinical manifestations and survival in the Barbados national lupus registry. Arthritis Rheum. 2012, 64, 1151–1158. [Google Scholar] [CrossRef]
- Peschken, C.A.; Esdaile, J.M. Systemic lupus erythematosus in North American Indians: A population based study. J. Rheumatol. 2000, 27. [Google Scholar]
- Mok, C.C.; Mak, A.; Chu, W.P.; To, C.H.; Nin Wong, S. Long-term Survival of Southern Chinese Patients With Systemic Lupus Erythematosus. Medicine 2005, 84, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Nossent, J. Systemic lupus erythematosus on the Caribbean island of Curacao: An epidemiological investigation. Ann. Rheum. Dis. 1992, 51, 1197–1201. [Google Scholar] [CrossRef] [PubMed]
- Alamanos, Y.; Voulgari, P.V.; Siozos, C.; Katsimpri, P.; Tsintzos, S.; Dimou, G.; Politi, E.N.; Rapti, A.; Laina, G.; Drosos, A.A. Epidemiology of systemic lupus erythematosus in northwest Greece 1982–2001. J. Rheumatol. 2003, 30, 731–735. [Google Scholar]
- Gudmundsson, S.; Steinsson, K. Systemic lupus erythematosus in Iceland 1975 through 1984. A nationwide epidemiological study in an unselected population. J. Rheumatol. 1990, 17, 1162–1167. [Google Scholar]
- Nossent, H.C. Systemic lupus erythematosus in the Arctic region of Norway. J. Rheumatol. 2001, 28, 539–546. [Google Scholar]
- Eilertsen, G.; Becker-Merok, A.; Nossent, J.C. The Influence of the 1997 Updated Classification Criteria for Systemic Lupus Erythematosus: Epidemiology, Disease Presentation, and Patient Management. J. Rheumatol. 2009, 36, 552–559. [Google Scholar] [CrossRef][Green Version]
- Lerang, K.; Gilboe, I.-M.; Thelle, D.S.; Gran, J.T. Mortality and years of potential life loss in systemic lupus erythematosus: A population-based cohort study. Lupus 2014, 23, 1546–1552. [Google Scholar] [CrossRef]
- Alonso, M.D.; Llorca, J.; Martinez-Vazquez, F.; Miranda-Filloy, J.A.; de Teran, T.D.; Dierssen, T.; Rodriguez, T.R.V.; Gomez-Acebo, I.; Blanco, R.; Gonzalez-Gay, M.A. Systemic Lupus Erythematosus in Northwestern Spain. Medicine 2011, 90, 350–358. [Google Scholar] [CrossRef]
- Ståhl-Hallengren, C.; Jönsen, A.; Nived, O.; Sturfelt, G. Incidence studies of systemic lupus erythematosus in Southern Sweden: Increasing age, decreasing frequency of renal manifestations and good prognosis. J. Rheumatol. 2000, 27, 685–691. [Google Scholar] [PubMed]
- Pamuk, O.N.; Balci, M.A.; Donmez, S.; Tsokos, G.C. The incidence and prevalence of systemic lupus erythematosus in Thrace, 2003–2014: A 12-year epidemiological study. Lupus 2015, 25, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Naleway, A.L.; Davis, M.E.; Greenlee, R.T.; Wilson, D.A.; Mccarty, D.J. Epidemiology of systemic lupus erythematosus in rural Wisconsin. Lupus 2005, 14, 862–866. [Google Scholar] [CrossRef] [PubMed]
- Bartels, C.M.; Buhr, K.A.; Goldberg, J.W.; Bell, C.L.; Visekruna, M.; Nekkanti, S.; Greenlee, R.T. Mortality and Cardiovascular Burden of Systemic Lupus Erythematosus in a US Population-based Cohort. J. Rheumatol. 2014, 41, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Uramoto, K.M.; Michet, C.J., Jr.; Thumboo, J.; Sunku, J.; O’Fallon, W.M.; Gabriel, S.E. Trends in the incidence and mortality of systemic lupus erythematosus, 1950-1992. Arthritis Rheum. 1999, 42, 46–50. [Google Scholar] [CrossRef]
- Jarukitsopa, S.; Hoganson, D.D.; Crowson, C.S.; Sokumbi, O.; Davis, M.D.; Michet, C.J.; Matteson, E.L.; Kremers, H.M.; Chowdhary, V.R. Epidemiology of Systemic Lupus Erythematosus and Cutaneous Lupus Erythematosus in a Predominantly White Population in the United States. Arthritis Rheum. 2014, 67, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, H.; Nived, O.; Sturfelt, G. Outcome in systemic lupus erythematosus: A prospective study of patients from a defined population. Medicine 1989, 68, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Lucero, L.G.; Barbaglia, A.L.; Bellomio, V.I.; Bertolaccini, M.C.; Escobar, M.A.M.; Sueldo, H.R.; Yacuzzi, M.S.; Carrizo, G.A.; Robles, N.; Rengel, S.; et al. Prevalence and incidence of systemic lupus erythematosus in Tucumán, Argentina. Lupus 2020, 29, 1815–1820. [Google Scholar] [CrossRef]
- Jacobsen, S. Mortality and Causes of Death of 513 Danish Patients with Systemic Lupus Erythematosus. Scand. J. Rheumatol. 1999, 28, 75–80. [Google Scholar] [CrossRef]
- Laustrup, H.; Voss, A.; Green, A.; Junker, P. Occurrence of systemic lupus erythematosus in a Danish community: An 8-year prospective study. Scand. J. Rheumatol. 2009, 38, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Helmick, C.G.; Bao, G.; Hootman, J.; Bayakly, R.; Gordon, C.; Drenkard, C. Racial Disparities in Mortality Associated with Systemic Lupus Erythematosus—Fulton and DeKalb Counties, Georgia, 2002–2016. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Mok, C.C.; To, C.H.; Ho, L.Y.; Yu, K.L. Incidence and mortality of systemic lupus erythematosus in a southern Chinese population, 2000-2006. J. Rheumatol. 2008, 35, 1978–1982. [Google Scholar]
- Yeh, K.-W.; Yu, C.-H.; Chan, P.-C.; Horng, J.-T.; Huang, J.-L. Burden of systemic lupus erythematosus in Taiwan: A population-based survey. Rheumatol. Int. 2013, 33, 1805–1811. [Google Scholar] [CrossRef]
- Iseki, K.; Miyasato, F.; Oura, T.; Uehara, H.; Nishime, K.; Fukiyama, K. An Epidemiologic Analysis of End-stage Lupus Nephritis. Am. J. Kidney Dis. 1994, 23, 547–554. [Google Scholar] [CrossRef]
- Jacobsen, S.; Petersen, J.; Ullman, S.; Junker, P.; Voss, A.; Rasmussen, J.M.; Tarp, U.; Poulsen, L.H.; Hansen, G.V.O.; Skaarup, B.; et al. A multicentre study of 513 Danish patients with systemic lupus erythematosus. I. Disease manifestations and analyses of clinical subsets. Clin. Rheumatol. 1998, 17, 468–477. [Google Scholar] [CrossRef]
- Somers, E.C.; Marder, W.; Cagnoli, P.; Lewis, E.E.; Deguire, P.; Gordon, C.; Helmick, C.G.; Wang, L.; Wing, J.J.; Dhar, J.P.; et al. Population-Based Incidence and Prevalence of Systemic Lupus Erythematosus: The Michigan Lupus Epidemiology and Surveillance Program. Arthritis Rheumatol. 2013, 66, 369–378. [Google Scholar] [CrossRef]
- Moe, S.E.R.; Molberg, Ø.; Strøm, E.H.; Lerang, K. Assessing the relative impact of lupus nephritis on mortality in a population-based systemic lupus erythematosus cohort. Lupus 2019, 28, 818–825. [Google Scholar] [CrossRef]
- Yu, K.-H.; Kuo, C.-F.; Chou, I.-J.; Chiou, M.-J.; See, L.-C. Risk of end-stage renal disease in systemic lupus erythematosus patients: A nationwide population-based study. Int. J. Rheum. Dis. 2016, 19, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Plantinga, L.C.; Lim, S.S.; Patzer, R.E.; McClellan, W.M.; Kramer, M.; Klein, M.; Pastan, S.; Gordon, C.; Helmick, C.G.; Drenkard, C. Incidence of End-Stage Renal Disease Among Newly Diagnosed Systemic Lupus Erythematosus Patients: The Georgia Lupus Registry. Arthritis Rheum. 2015, 68, 357–365. [Google Scholar] [CrossRef]
- Nived, O.; Bengtsson, A.; Jönsen, A.; Sturfelt, G.; Olsson, H. Malignancies during follow-up in an epidemiologically defined systemic lupus erythematosus inception cohort in southern Sweden. Lupus 2001, 10, 500–504. [Google Scholar] [CrossRef]
- Lin, C.-H.; Hung, P.-H.; Hu, H.-Y.; Chen, Y.-J.; Guo, H.-R.; Hung, K.-Y. Infection-related hospitalization and risk of end-stage renal disease in patients with systemic lupus erythematosus: A nationwide population-based study. Nephrol. Dial. Transplant. 2016, 32, 1683–1690. [Google Scholar] [CrossRef]
- Lin, W.-H.; Guo, C.-Y.; Wang, W.-M.; Yang, D.-C.; Kuo, T.-H.; Liu, M.-F.; Wang, M.-C. Incidence of progression from newly diagnosed systemic lupus erythematosus to end stage renal disease and all-cause mortality: A nationwide cohort study in Taiwan. Int. J. Rheum. Dis. 2013, 16, 747–753. [Google Scholar] [CrossRef]
- Eilertsen, G.O.; Fismen, S.; Hanssen, T.-A.; Nossent, J.C. Decreased incidence of lupus nephritis in northern Norway is linked to increased use of antihypertensive and anticoagulant therapy. Nephrol. Dial. Transplant. 2010, 26, 620–627. [Google Scholar] [CrossRef][Green Version]
- Ragnarsson, O.; Gröndal, G.; Steinsson, K. Risk of malignancy in an unselected cohort of Icelandic patients with systemic lupus erythematosus. Lupus 2003, 12, 687–691. [Google Scholar] [CrossRef]
- Chen, Y.-J.; Chang, Y.-T.; Wang, C.-B.; Wu, C.-Y. Malignancy in Systemic Lupus Erythematosus: A Nationwide Cohort Study in Taiwan. Am. J. Med. 2010, 123, 1150.e1–1150.e6. [Google Scholar] [CrossRef]
- Borchers, A.T.; Keen, C.L.; Shoenfeld, Y.; Gershwin, M. Surviving the butterfly and the wolf: Mortality trends in systemic lupus erythematosus. Autoimmun. Rev. 2004, 3, 423–453. [Google Scholar] [CrossRef]
- Tektonidou, M.; Lewandowski, L.B.; Hu, J.; Dasgupta, A.; Ward, M.M. Survival in adults and children with systemic lupus erythematosus: A systematic review and Bayesian meta-analysis of studies from 1950 to 2016. Ann. Rheum. Dis. 2017, 76, 2009–2016. [Google Scholar] [CrossRef]
- Schoenfeld, S.R.; Kasturi, S.; Costenbader, K.H. The epidemiology of atherosclerotic cardiovascular disease among patients with SLE: A systematic review. Semin. Arthritis Rheum. 2013, 43, 77–95. [Google Scholar] [CrossRef]
- Lu, X.; Wang, Y.; Zhang, J.; Pu, D.; Hu, N.; Luo, J.; An, Q.; He, L. Patients with systemic lupus erythematosus face a high risk of cardiovascular disease: A systematic review and Meta-analysis. Int. Immunopharmacol. 2021, 94, 107466. [Google Scholar] [CrossRef]
- Urowitz, M.B.; Bookman, A.A.; Koehler, B.E.; Gordon, D.A.; Smythe, H.A.; Ogryzlo, M.A. The bimodal mortality pattern of systemic lupus erythematosus. Am. J. Med. 1976, 60, 221–225. [Google Scholar] [CrossRef]
- Yurkovich, M.; Vostretsova, K.; Chen, W.; Aviña-Zubieta, J.A. Overall and Cause-Specific Mortality in Patients With Systemic Lupus Erythematosus: A Meta-Analysis of Observational Studies. Arthritis Rheum. 2013, 66, 608–616. [Google Scholar] [CrossRef]
- Lee, Y.H.; Choi, S.J.; Ji, J.D.; Song, G.G. Overall and cause-specific mortality in systemic lupus erythematosus: An updated meta-analysis. Lupus 2016, 25, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.J.; Jawad, A.S. The effect of ethnicity and genetic ancestry on the epidemiology, clinical features and outcome of systemic lupus erythematosus. Rheumatology 2016, 56, i67–i77. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.-J.; Wallace, D.; Ishimori, M.; Scofield, R.; Weisman, M. Review: Male systemic lupus erythematosus: A review of sex disparities in this disease. Lupus 2009, 19, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Hanly, J.G.; O’Keeffe, A.G.; Su, L.; Urowitz, M.B.; Romero-Diaz, J.; Gordon, C.; Bae, S.-C.; Bernatsky, S.; Clarke, A.E.; Wallace, D.J.; et al. The frequency and outcome of lupus nephritis: Results from an international inception cohort study. Rheumatology 2015, 55, 252–262. [Google Scholar] [CrossRef]
- Tektonidou, M.; Dasgupta, A.; Ward, M.M. Risk of End-Stage Renal Disease in Patients With Lupus Nephritis, 1971-2015: A Systematic Review and Bayesian Meta-Analysis. Arthritis Rheumatol. 2016, 68, 1432–1441. [Google Scholar] [CrossRef]
- Choi, M.Y.; Flood, K.; Bernatsky, S.; Ramsey-Goldman, R.; Clarke, A.E. A review on SLE and malignancy. Best Pr. Res. Clin. Rheumatol. 2017, 31, 373–396. [Google Scholar] [CrossRef]
- Jørgensen, K.T.; Pedersen, B.V.; Nielsen, N.M.; Jacobsen, S.; Frisch, M. Childbirths and risk of female predominant and other autoimmune diseases in a population-based Danish cohort. J. Autoimmun. 2012, 38, J81–J87. [Google Scholar] [CrossRef]
| Author; Year (Ref.) | Study Location | Study Period * | Ethnicity | Follow-Up Time | SLE Cases, n | Deaths, n | SMR, 95% CI | Survival (Controls)% | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Incident | Total | Incident | Total | Female | Male | 5 Years | 10 Years | 15 Years | 20 Years | |||||
| NORTH AMERICA | |||||||||||||||
| Peschken et al.; 2000 [13] | Canada | 1980–1997 | 177 Caucasian | NA | 257 | 257 | NA | NA | 97 | 95 | 91 | ||||
| 49 NAI | 95 | 83 | 75 | ||||||||||||
| Uramoto et al.; 1999 [26] | MN, USA | 1950–1979 | Mainly Caucasian | 7.2 years (µ) | 79 | 79 | NA | NA | 2.7 (1.7–4.2) | 75 (95) | 50 (92) | ||||
| 1980–1992 | 90 (90) | 71 (90) | |||||||||||||
| Naleway et al.; 2005 [24] | WI, USA | 1991–2001 | Mainly Caucasian | 5.8 years (µ) | 117 | 44 | NA | 8 | 88 | 76 | |||||
| Bartels et al.; 2014 [25] | WI, USA | 1991–2009 | NA | 7.7 years (µ) | 70 | 70 | 87 (90) | 74 (81) | 59 (73) | ||||||
| Jarukitsopa, S et al.; 2015 [27] | MN, USA | 1993–2005 | 80% white | 7.8 years (µ) | 117 | 45 | NA | 6 | 2.6 (1.0–5.6) | 93 | 89 | 64 | |||
| Lim et al.; 2019 [32] | GA, USA | 2002–2016 | 76% black | NA | 1689 | 336 | 401 | 97 | 3.1 (2.8–3.4) | 3.1 (2.8–3.5) | 3.0 (2.3–3.9) | ||||
| Flower et al.; 2012 [12] | Barbados | 2000–2009 | 98% African Caribbean | NA | 183 | 183 | 24 | 24 | 88 | 80 | |||||
| SOUTH AMERICA | |||||||||||||||
| Lucero et al.; 2020 [29] | Argentina | 2005–2012 | 83% Mestizos | NA | 353 | NA | 32 | NA | 96 | 93 | |||||
| Nossent; 1992 [15] | Curaçao | 1980–1990 | All of African descent | NA | 94 | 68 | 25 | NA | 60 | 46 | |||||
| ASIA | |||||||||||||||
| Iseki et al.; 1994 [35] | Japan | 1972–1993 | NA | 4877 PY | 566 | NA | 104 | NA | 89 | 78 | 72 | 69 | |||
| Mok et al.; 2005 [14] | Hong Kong, China | 1991–2003 | All ethnic Chinese | NA | 258 | 258 | 29 | 29 | 92 | 83 | 80 | ||||
| Mok et al.; 2008 [33] | Hong Kong, China | 2000–2006 | Mainly Asian | NA | 442 | NA | 30 | NA | 3.9 ** | 4.0 ** | 9.6 ** | ||||
| Yeh et al.; 2013 [34] | Taiwan | 2003–2008 | NA | NA | 6675 | 6675 | 1611 | 1611 | 11.1 (NA) | ||||||
| Al-Adhoubi et al.; 2021 [11] | Oman | 2006–2020 | NA | NA | 1160 | NA | 54 | NA | 100 | 100 | 99 | ||||
| EUROPE | |||||||||||||||
| Gudmundsson et al.; 1990 [17] | Iceland | 1975–1988 | NA | NA | 76 | 76 | 17 | 17 | 3.4 (2.0–5.4) | 84 | 78 | ||||
| Jacobsen et al., 1999 [30] | Denmark | 1975–1995 | NA | 4185 PY | 513 | NA | 122 | NA | 4.6 (3.8–5.5) | 4.7 (3.9–5.8) | 4.0 (3.8–5.5) | 91 | 76 | 53 | |
| Nossent et al.; 2001 [18] | Norway, north | 1978–1999 | >96% Caucasian | NA | 105 | 83 | 18 | 11 | 92 | 75 | |||||
| Eilertsen et al.; 2009 [19] | Norway, north | 1978–1995 | 98.8% Caucasian | NA | 81 | 81 | 25 | 25 | 2.0 (1.4–2.8) | 2.1 (1.5–3.1) | 1.5 (0.6–3.5) | 91(98) | 81 (96) | ||
| 1996–2007 | 98.3% Caucasian | NA | 58 | 58 | 5 | 5 | 96 (98) | 92 (96) | |||||||
| Lerang et al.; 2014 [20] | Norway, Oslo | 1999–2009 | 84% of European descent | 2665/812 PY | 325 | 129 | 50 | 7 | 3.0 (2–3.8) | 2,7 (2,0–3.7) | 4.6 (2.3–8.1) | 95 (99) | 90 (96) | ||
| Jonsson et al.; 1989 [28] | Sweden, Lund | 1981–1986 | NS | 342 PY | 86 | 38 | 9 | NA | 97 (97) | ||||||
| Ståhl-Hallengren et al.; 2000 [22] | Sweden, Lund | 1981–1991 | NA | NA | 162 | 162 | 17 | 17 | 93 (98) | 83 (96) | |||||
| Ingvarsson et al.; 2019 [10] | Sweden, Lund | 1981–2014 | 98.3% Caucasian | 3053 PY | 174 | 174 | 60 | 60 | 2.5 (1.9–3.3) | 2.7 (2.0–3.6) | 1.9 (1.0–3.4) | 91 (97) | 85 (91) | 73 (86) | 62 (77) |
| Alamanos et al.; 2003 [16] | Greece | 1982–2001 | NA | NA | 178 | 178 | 12 | 12 | 1.3 (NA) | 97 | 90 | ||||
| Alonso et al.; 2011 [21] | Spain | 1987–2006 | NA | 7.8 years (µ) | 150 | 150 | 19 | 19 | 94 (97) | 87 (94) | 80 (89) | ||||
| Laustrup et al.; 2009 [31] | Denmark, Funen | 1995–2003 | 94% Caucasian | 767 PY | 138 | NA | 15 | NA | 1.9 (1.0–3.0) | 1.8 (0.9–3.2) | 2.1 (0.4–6.2) | ||||
| Voss et al.; 2013 [9] | Denmark, Funen | 1995–2010 | 94% Caucasian | 2052 PY | 215 | NA | 38 | NA | 2.3 (1.6–3.2) | 1.9 (1.3–2.9) | 3.2 (1.5–6.3) | 94 | 73 | ||
| Pamuk et al.; 2015 [23] | Turkey | 2003–2014 | NA | 48 months (mdn) | 331 | 331 | 17 | 17 | 95 | 90 | |||||
| Author; Year (Ref.) | Study Location | Study Period * | Follow-Up Time | Deaths/SLE Cases; n/N | Cause of Death, % | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Active SLE | CVD | Infections | PD | Malignancy | Renal Failure | |||||
| NORTH AMERICA | ||||||||||
| Bartels et al.; 2014 [25] | WI, USA | 1991–2009 | 540 patient years | 19/70 | 32% | 16% | 13% | 13% | ||
| Jarukitsopa et al.; 2015 [27] | MN, USA | 1993–2005 | 7.8 years (mean) | 6/45 | 67% | 33% | ||||
| Flower et al.; 2012 [12] | Barbados | 2000–2009 | NA | 24/181 | 42% d | 8% | 46% b | |||
| SOUTH AMERICA | ||||||||||
| Lucero et al.; 2020 [29] | Argentina | 2005–2012 | NA | 32/353 | 44% | |||||
| ASIA | ||||||||||
| Mok et al.; 2005 [14] | China | 1991–2003 | NA | 29/258 | 31% c | 55% | 3% | |||
| Iseki et al.; 1994 [35] | Japan | 1972–1993 | 4877 patient years | 104/566 | 15% | 24% | 12% | |||
| Mok et al.; 2008 [33] | China | 2000–2006 | NA | 30/422 | 6% | 60% | 3% | 7% | ||
| EUROPE | ||||||||||
| Jacobsen et al.; 1999 [30] | Denmark | 1975–1995 | 4185 patient years | 122/513 | 19% | 24% | 20% | 7% | 10% | |
| Voss et al.; 2013 a [9] | Denmark | 1995–2010 | 2052 patient years | 38/214 | 8% | 32% | 8% | 16% | 13% | |
| Gudmundsson et al.; 1990 [17] | Iceland | 1975–1988 | NA | 17/76 | 35% b | 29% | 6% | |||
| Ingvarsson et al.; 2019 a [10] | Sweden | 1981–2014 | 3053 patient years | 60/174 | 7% | 59% | 15% | 5% | 13% | |
| Alamanos et al.; 2003 [16] | Greece | 1982–2001 | NA | 12/178 | 17% | 17% | ||||
| Alonso et al.; 2011 [21] | Spain | 1987–2006 | 7.8 years (mean) | 19/150 | 21% | 21% | 26% | 11% | ||
| Lerang et al.; 2014 [20] | Norway | 1999–2009 | 2665 patient years | 50/325 | 12% | 16% | 6% | 20% | ||
| Pamuk et al.; 2015 [23] | Turkey | 2003–2014 | 48 months (mdn) | 17/331 | 24% | 23% d | 12% | 12% | ||
| Author, Year (Ref.) | Study Location | Study Period * | Follow-Up Time | SLE Cases, n | LN,% | Age, Years | Ethnicity | ESRD Development | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Incident | Total SLE | Incident SLE | LN | |||||||
| NORTH AMERICA | |||||||||||
| Somers et al., 2014 [37] | MI, USA | 2002–2004 | NA | 2129 | 399 | 32 | All | 56% black patients | Total 10.8%; black 15.3%, white 4.5% | ||
| Plantinga et al., 2016 [40] | GA, USA | 2002–2004 | 2603 patient years | 344 | 344 | NA | All | 76.1% black patients | Total 11.1; black 13.8, white 3.3/1000 patient years | ||
| ASIA | |||||||||||
| Iseki et al., 1994 [35] | Japan | 1972–1991 | 4788 patient years | 566 | NA | 49 | All | NA | 9% | ||
| Yu et al., 2016 [39] | Taiwan | 2000–2008 | NA | 1196 | 1196 | NA | All | NA | 6.1/1000 patient years | ||
| Lin et al., 2017 [42] | Taiwan | 2000–2011 | 8.1 years (mean) | 7326 | 7326 | NA | All | NA | 4.3% | ||
| Lin et al., 2013 [43] | Taiwan | 2003–2008 | NA | 4130 | 4130 | NA | All | NA | 2.5% | ||
| EUROPE | |||||||||||
| Jacobsen et al., 1998 [36] | Denmark | 1975–1995 | 8.2 years (mean) | 513 | NA | 42 | All | NA | 5% | ||
| Eilertsen et al., 2011 [44] | Norway | 1978–1995 | NA | 62 | 62 | 32 | ≥16 | 98% Caucasian | 10 years renal survival: 100% | ||
| 1996–2007 | NA | 87 | 87 | 18 | ≥16 | 99% Caucasian | 10 years renal survival 88.5% | ||||
| Jonsson et al., 1989 [28] | Sweden | 1981–1986 | NA | 86 | 38 | 30 | ≥15 | NA | 3.8% | ||
| Gergianaki et al., 2017 [3] | Greece | 1999–2013 | 7.2 years (mean) | 750 | NA | 13 | ≥15 | 97% Greek | 4.4% | ||
| Reppe Moe et al., 2019 [38] | Norway | 1999–2017 | 18.4/10.6 years (mean) | 325 | 129 | 30 | ≥16 | 84% of European descent | 6% | 2,3/1000 patient years | |
| Author; Year (Ref.) | Study Location | Study Period * | Follow-Up Time, Mean | Age, Years | SLE Cases, n | SLE Cases with Malignancies, n | Malignancies O/E Ratio (95% CI) | Subgroups of Malignancy **, O/E Ratio (95% CI)/(p) *** | |
|---|---|---|---|---|---|---|---|---|---|
| Total | Incident | ||||||||
| EUROPE | |||||||||
| Ragnarsson et al.; 2003 [45] | Iceland | 1957–2001 | 12.8 years | All | 238 | NA | 27 | O/E 1.4 (0.9–1.9) | Skin SCC 6.4 (1.3–18.5) Lymphoma 5.5 (0.6–19.6) Lung 1.7 (0.4–5.0) Breast 1.6 (0.7–3.2) Prostate 1.2 (0.0–6.2) |
| Nived et al.; 2001 [41] | Sweden | 1981–1998 | 9.4 years | >15 | 116 | 116 | 11 | SMR 1.2 **** Male 2.2 (0.6–5.7) Female 1.0 (0.4–2.1) | NHL 11.6 (1.4–42) Prostate 6.4 (1.3–18.7) Lung 5.6 (0.7–20.1) |
| ASIA | |||||||||
| Chen et al.; 2010 [46] a | Taiwan | 1996–2007 | 6.1 years | All | 11,763 | 11,763 | 259 | SIR 1.8 (1.7–1.8) | NHL 7.3 (7.0–7.6) Vagina/vulva 4.8 (4.2–5.3) Nasopharynx, siunus, ears 4.2 (3.9–4.5) Leukemia 2.6 (2.5–2.8) Skin 1.7 (1.6–1.8) Breast 1.6 (1.5–1.6) Cervix 1.4 (1.3–1.5) Lung/mediastinum 1.2 (1.2–1.3) Prostate 0.8 (0.7–0.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reppe Moe, S.; Haukeland, H.; Molberg, Ø.; Lerang, K. Long-Term Outcome in Systemic Lupus Erythematosus; Knowledge from Population-Based Cohorts. J. Clin. Med. 2021, 10, 4306. https://doi.org/10.3390/jcm10194306
Reppe Moe S, Haukeland H, Molberg Ø, Lerang K. Long-Term Outcome in Systemic Lupus Erythematosus; Knowledge from Population-Based Cohorts. Journal of Clinical Medicine. 2021; 10(19):4306. https://doi.org/10.3390/jcm10194306
Chicago/Turabian StyleReppe Moe, Sigrid, Hilde Haukeland, Øyvind Molberg, and Karoline Lerang. 2021. "Long-Term Outcome in Systemic Lupus Erythematosus; Knowledge from Population-Based Cohorts" Journal of Clinical Medicine 10, no. 19: 4306. https://doi.org/10.3390/jcm10194306
APA StyleReppe Moe, S., Haukeland, H., Molberg, Ø., & Lerang, K. (2021). Long-Term Outcome in Systemic Lupus Erythematosus; Knowledge from Population-Based Cohorts. Journal of Clinical Medicine, 10(19), 4306. https://doi.org/10.3390/jcm10194306





