The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Definitions and Classification
2.2. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. Risk factors and Cardiovascular Diseases
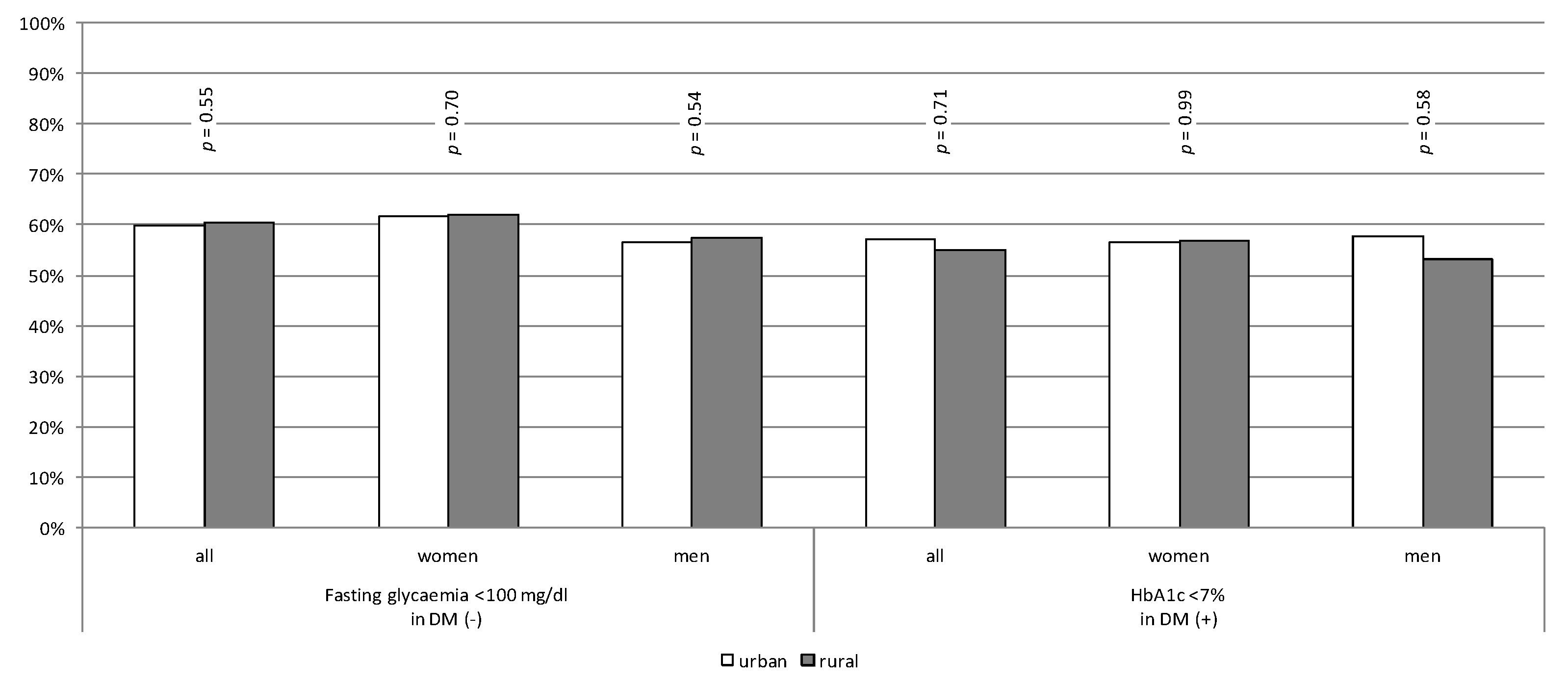
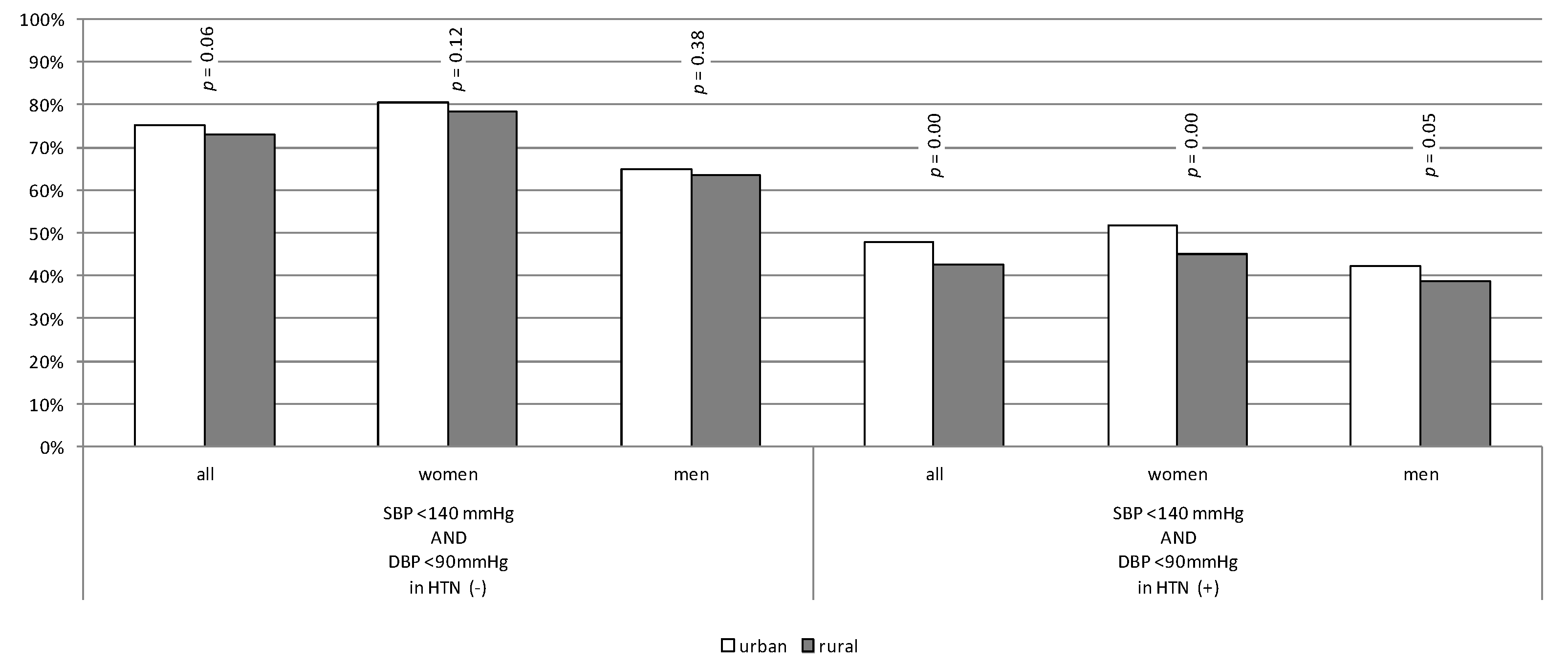
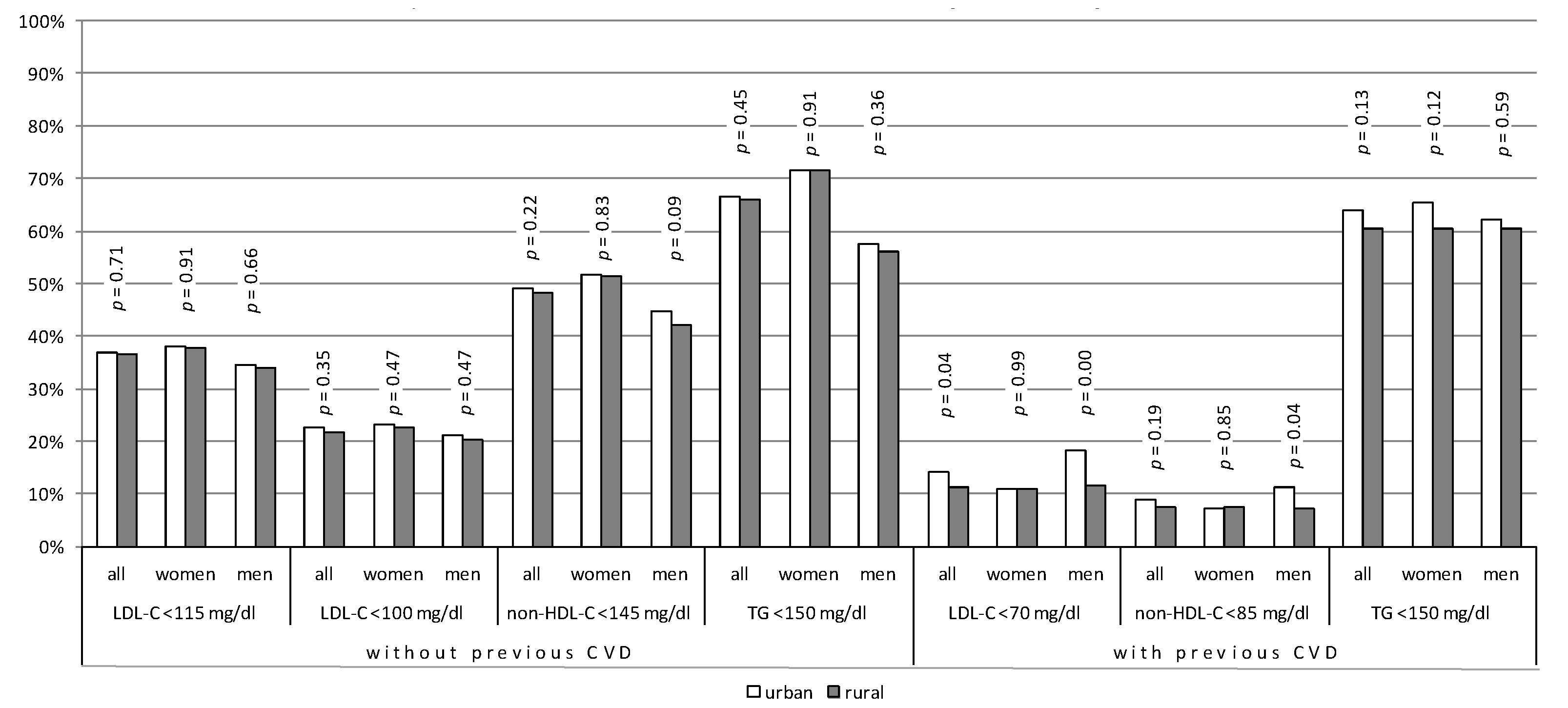
3.3. Achievement of Therapeutic Goals
4. Discussion
4.1. Main Findings
4.2. Comparison with Other Studies
4.3. Interpretation of Study Results
4.4. Implications of Study Results
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartley, D. Rural health disparities, population health, and rural culture. Am. J. Public Health 2004, 94, 1675–1678. [Google Scholar] [CrossRef]
- Bragg, F.; Holmes, M.V.; Iona, A.; Guo, Y.; Du, H.; Chen, Y.; Bian, Z.; Yang, L.; Herrington, W.; Bennett, D.; et al. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA J. Am. Med. Assoc. 2017, 317, 280–289. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [Green Version]
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics 2017; European Heart Network: Brussels, Belgium, 2017. [Google Scholar]
- Jóźwiak, J.J.; Studziński, K.; Tomasik, T.; Windak, A.; Mastej, M.; Catapano, A.L.; Ray, K.K.; Mikhailidis, D.P.; Toth, P.P.; Howard, G.; et al. The prevalence of cardiovascular risk factors and cardiovascular disease among primary care patients in Poland: Results from the LIPIDOGRAM2015 study. Atheroscler. Suppl. 2020, 42, e15–e24. [Google Scholar] [CrossRef] [PubMed]
- Marković, B.B.; Vrdoljak, D.; Kranjčević, K.; Vučak, J.; Kern, J.; Bielen, I.; Lalić, D.I.; Katić, M.; Reiner, Ž. Continental-Mediterranean and rural-urban differences in cardiovascular risk factors in Croatian population. Croat. Med. J. 2011, 52, 566–575. [Google Scholar] [CrossRef] [Green Version]
- Lindroth, M.; Lundqvist, R.; Lilja, M.; Eliasson, M. Cardiovascular risk factors differ between rural and urban Sweden: The 2009 Northern Sweden MONICA cohort. BMC Public Health 2014, 14, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Supiyev, A.; Nurgozhin, T.; Zhumadilov, Z.; Peasey, A.; Hubacek, J.A.; Bobak, M. Prevalence, awareness, treatment and control of dyslipidemia in older persons in urban and rural population in the Astana region, Kazakhstan. BMC Public Health 2017, 17, 651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nuotio, J.; Vähämurto, L.; Pahkala, K.; Magnussen, C.G.; Hutri-Kähönen, N.; Kähönen, M.; Laitinen, T.; Taittonen, L.; Tossavainen, P.; Lehtimäki, T.; et al. CVD risk factors and surrogate markers—Urban-rural differences. Scand. J. Public Health 2020, 48, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Rangarajan, S.; Teo, K.; Islam, S.; Li, W.; Liu, L.; Bo, J.; Lou, Q.; Lu, F.; Liu, T.; et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N. Engl. J. Med. 2014, 371, 818–827. [Google Scholar] [CrossRef]
- Ray, K.K.; Molemans, B.; Schoonen, W.M.; Giovas, P.; Bray, S.; Kiru, G.; Murphy, J.; Banach, M.; De Servi, S.; Gaita, D.; et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: The DA VINCI study. Eur. J. Prev. Cardiol. 2020, 28, 1279–1289. [Google Scholar] [CrossRef] [PubMed]
- Dyrbus, K.; Gasior, M.; Desperak, P.; Nowak, J.; Osadnik, T.; Banach, M. Characteristics of lipid profile and effectiveness of management of dyslipidaemia in patients with acute coronary syndromes—Data from the TERCET registry with 19,287 patients. Pharmacol. Res. 2019, 139, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Jóźwiak, J.; Kasperczyk, S.; Tomasik, T.; Osadnik, T.; Windak, A.; Studziński, K.; Mastej, M.; Catapano, A.; Ray, K.K.; Mikhailidis, D.; et al. Design and rationale of a nationwide screening analysis from the LIPIDOGRAM2015 and LIPIDOGEN2015 studies. Arch. Med. Sci. 2020, 1–13. [Google Scholar] [CrossRef]
- Tykarski, A.; Narkiewicz, K.; Gaciong, Z.; Januszewicz, A.; Litwin, M.; Kostka-Jeziorny, K.; Adamczak, M.; Szczepaniak-Chicheł, L.; Chrostowska, M.; Czarnecka, D.; et al. 2015 guidelines for the management of hypertension. Recommendations of the Polish Society of Hypertension—Short version. Kardiol. Pol. 2015, 73, 676–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reiner, Z.; Catapano, A.L.; De Backer, G.; Graham, I.; Taskinen, M.-R.; Wiklund, O.; Agewall, S.; Alegria, E.; Chapman, M.J.; Durrington, P.; et al. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 2011, 32, 1769–1818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czech, A.; Cypryk, K.; Czupryniak, L.; Gajewska, D.; Grzeszczak, W.; Gumprecht, J.; Idzior-Waluś, B.; Jaosz-Chobot, P.; Kalarus, Z.; Karnafel, W.; et al. Guidelines (PTD) 2015 Guidelines on the management of diabetic patients. A position of Diabetes Poland. Clin. Diabetol. 2015, 4 (Supp. A), 1–79. [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Perk, J.; De Backer, G.; Gohlke, H.; Graham, I.; Reiner, Ž.; Verschuren, M.; Albus, C.; Benlian, P.; Boysen, G.; Cifkova, R.; et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur. Heart J. 2012, 33, 1635–1701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J. Hypertens. 2018, 36, 2284–2309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef] [PubMed]
- Zdrojewski, T.; Rutkowski, M.; Bandosz, P.; Gaciong, Z.; Solnica, B.; Drygas, W.; Wojtyniak, B.; Stokwiszewski, J.; Pencina, M.; Wołkiewicz, E.; et al. Assessment of the prevalence and control of cardiovascular risk factors in Poland—NATPOL 1997, 2002, 2011 studies. In Epidemiology and Prevention of Cardiovascular Diseases; Medycyna Praktyczna: Kraków, Poland, 2015; pp. 57–64. [Google Scholar]
- Doryńska, A.; Polak, M.; Kozela, M.; Szafraniec, K.; Piotrowski, W.; Bielecki, W.; Drygas, W.; Kozakiewicz, K.; Piwoński, J.; Tykarski, A.; et al. Cardiovascular disease (CVD) risk factors in Kraków and in the whole Poland adult population. Results from the WOBASZ study and Polish arm of the HAPIEE project. Przeglad Epidemiologiczny 2015, 69, 79–86, 175–180. [Google Scholar] [PubMed]
- Nowicki, G.J.; Ślusarska, B.; Piasecka, H.; Bartoszek, A.; Kocka, K.; Deluga, A. The status of cardiovascular health in rural and urban areas of janów lubelski district in eastern poland: A population-based study. Int. J. Environ. Res. Public Health 2018, 15, 2388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rywik, S.L.; Davis, C.E.; Pajak, A.; Broda, G.; Folsom, A.R.; Kawalec, E.; Williams, O.D. Poland and U.S. Collaborative study on cardiovascular epidemiology hypertension in the community: Prevalence, awareness, treatment, and control of hypertension in the Pol-MONICA project and the U.S. Atherosclerosis risk in communities study. Ann. Epidemiol. 1998, 8, 3–13. [Google Scholar] [CrossRef]
- Broda, G.; Davis, C.E.; Pajak, A.; Williams, O.D.; Rywik, S.L.; Baczyńska, E.; Folsom, A.R.; Szklo, M. Poland and United States Collaborative Study on Cardiovascular Epidemiology. Arterioscler. Thromb. Vasc. Biol. 1996, 16, 339–349. [Google Scholar] [CrossRef] [PubMed]
| All | Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | p | Urban | Rural | p | Urban | Rural | p | |
| Total n (%) | 7028 (51.21%) | 6696 (48.79%) | 0.11 | 4495 (51.7%) | 4195 (48.3%) | 0.11 | 2533 (50.3%) | 2501 (49.7%) | 0.11 |
| (years) | 57 ± 14 | 56 ± 14 | 0.00 | 57 ± 14 | 55 ± 14 | 0.00 | 56 ± 14 | 56 ± 14 | 0.17 |
| Levels of education n (%) | |||||||||
| Primary | 546 (7.77%) | 1181 (17.64%) | 397 (8.83%) | 796 (18.97%) | 149 (5.88) | 385 (15.39) | |||
| Vocational | 1754 (24.96%) | 2298 (34.32%) | 918 (20.42%) | 1166 (27.79%) | 836 (33.0%) | 1132 (45.26%) | |||
| Secondary | 2811 (40.00%) | 3112 (31.54%) | 1931 (42.96%) | 1448 (34.52%) | 880 (34.74%) | 664 (26.55%) | |||
| High | 1917 (27.28%) | 1105 (16.50%) | 0.00 | 1249 (27.79%) | 785 (18.71%) | 0.00 | 668 (26.37%) | 320 (12.79%) | 0.00 |
| SBP (mmHg) | 132 ± 18 | 133 ± 19 | 0.01 | 130 ± 18 | 131 ± 19 | 0.05 | 136 ± 19 | 135 ± 17 | 0.14 |
| DBP (mmHg) | 80 ± 10 | 81 ± 11 | 0.00 | 79 ± 10 | 80 ± 11 | 0.00 | 83 ± 11 | 82 ± 10 | 0.03 |
| (mg/dL) | 202 ± 44 | 203 ± 45 | 0.21 | 205 ± 44 | 205 ± 43 | 0.92 | 199 ± 47 | 196 ± 44 | 0.02 |
| (mg/dL) | 55 ± 15 | 55 ± 15 | 0.02 | 59 ± 15 | 58 ± 15 | 0.00 | 48 ± 13 | 48 ± 13 | 0.14 |
| (mg/dL) | 128 ± 40 | 130 ± 41 | 0.04 | 129 ± 41 | 130 ± 41 | 0.23 | 129 ± 40 | 126 ± 39 | 0.05 |
| (mg/dL) | 147 ± 42 | 148 ± 43 | 0.03 | 146 ± 42 | 147 ± 41 | 0.24 | 151 ± 45 | 148 ± 42 | 0.04 |
| (mg/dL) | 147 ± 113 | 149 ± 124 | 0.79 | 135 ± 97 | 135 ± 83 | 0.83 | 174 ± 170 | 169 ± 133 | 0.78 |
| (mg/dL) | 104 ± 25 | 103 ± 25 | 0.048 | 102 ± 24 | 102 ± 23 | 0.07 | 106 ± 27 | 106 ± 27 | 0.27 |
| (%) | 5.7 ± 1 | 5.7 ± 1 | 0.61 | 5.7 ± 0.9 | 5.7 ± 0.9 | 0.83 | 5.8 ± 1 | 5.8 ± 1 | 0.39 |
| Hypertension n (%) | 3482 (49.54%) | 3306 (49.37%) | 0.84 | 2152 (47.88%) | 1990 (47.44%) | 0.68 | 1330 (52.51%) | 1316 (52.62%) | 0.94 |
| Diabetes n (%) | 964 (13.72%) | 879 (13.13%) | 0.31 | 534 (11.88%) | 487 (11.61%) | 0.70 | 430 (16.98%) | 392 (15.67%) | 0.21 |
| Dyslipidaemia n (%) | 5917 (84.22%) | 5706 (85.22%) | 0.11 | 3698 (82.27%) | 461 (82.50%) | 0.77 | 2221 (87.68%) | 2245 (89.76%) | 0.02 |
| CVD n (%) | 1014 (14.43%) | 951 (14.20%) | 0.70 | 550 (12.24%) | 459 (10.94%) | 0.06 | 464 (18.32%) | 492 (19.67%) | 0.22 |
| CHD | 921 (13.10%) | 866 (12.93%) | 0.77 | 492 (10.95%) | 415 (9.89%) | 0.11 | 429 (16.94%) | 451 (18.03%) | 0.31 |
| MI | 335 (4.77%) | 290 (4.33%) | 0.22 | 113 (2.51%) | 81 (1.93%) | 0.07 | 222 (8.76%) | 209 (8.36%) | 0.61 |
| Ischaemic stroke | 145 (2.06%) | 123 (1.84%) | 0.34 | 80 (1.78%) | 61 (1.45%) | 0.23 | 65 (2.57%) | 62 (2.48%) | 0.84 |
| Haemorrhagic stroke | 17 (0.24%) | 14 (0.21%) | 0.69 | 8 (0.18%) | 8 (0.19%) | 0.89 | 9 (0.36%) | 6 (0.24%) | 0.45 |
| AF | 343 (4.88%) | 365 (5.45%) | 0.13 | 208 (4.63%) | 202 (4.82%) | 0.68 | 135 (5.33%) | 163 (6.52%) | 0.07 |
| FH | 32 (0.46%) | 41 (0.61%) | 0.21 | 25 (0.56%) | 27 (0.64%) | 0.60 | 7 (0.28%) | 14 (0.56%) | 0.12 |
| Overweight n (%) | 2822 (40.15%) | 2595 (38.75%) | 0.09 | 1623 (36.11%) | 1528 (36.42%) | 0.76 | 1199 (47.34%) | 1067 (42.66%) | 0.00 |
| Obesity n (%) | 2273 (32.34%) | 2513 (37.53%) | 0.00 | 1365 (30.37%) | 1497 (35.69%) | 0.00 | 908 (35.85%) | 1016 (40.62%) | 0.00 |
| Exceeded waist circumference (W ≥ 80 cm; M ≥ 94 cm) n (%) | 5446 (77.49%) | 5401 (80.66%) | 0.00 | 3563 (79.27%) | 3478 (82.91%) | 0.00 | 650 (74.34%) | 578 (76.89%) | 0.04 |
| Abdominal obesity n (%) | 3035 (43.18%) | 3107 (46.40%) | 0.00 | 2292 (50.99%) | 2356 (56.16%) | 0.00 | 743 (29.33%) | 751 (30.03%) | 0.59 |
| Smoking status n (%) | |||||||||
| Never smokers | 3648 (51.91%) | 3742 (55.88%) | 2620 (58.29%) | 2781 (66.29%) | 1028 (40.58%) | 961 (38.42%) | |||
| Current smokers | 1247 (17.74%) | 1056 (15.77%) | 748 (16.64%) | 551 (13.13%) | 499 (19.70%) | 505 (20.19%) | |||
| Ex-smokers | 2133 (30.35%) | 1898 (28.35%) | 0.00 | 1127 (25.07%) | 863 (20.57%) | 0.00 | 1006 (39.72%) | 1035 (41.38%) | 0.29 |
| Lipids | Blood Pressure | Glucose | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Rural | Urban | Rural | |||||||
| Analysed Variables | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| Age | 0.98 (0.98–0.98) | 0.00 | 0.98 (0.98–0.98) | 0.00 | 0.97 (0.97–0.97) | 0.00 | 0.96 (0.96–0.96) | 0.00 | 0.97 (0.97–0.98) | 0.00 | 0.97 (0.97–0.98) | 0.00 |
| Male | 0.83 (0.75–0.91) | 0.00 | 0.71 (0.65–0.79) | 0.00 | 0.57 (0.51–0.63) | 0.00 | 0.60 (0.54–0.67) | 0.00 | 0.80 (0.73–0.88) | 0.00 | 0.80 (0.72–0.88) | 0.00 |
| Levels of education | ||||||||||||
| 0.89 (0.74–1.09) | 0.26 | 0.90 (0.78–1.03) | 0.13 | 1.16 (0.96–1.41) | 0.13 | 1.37 (1.19–1.57) | 0.00 | 1.16 (0.96–1.41) | 0.12 | 1.23 (1.07–1.41) | 0.00 |
| 0.99 (0.83–1.19) | 0.94 | 1.06 (0.92–1.22) | 0.42 | 1.59 (1.32–1.92) | 0.00 | 2.21 (1.91–2.55) | 0.00 | 1.51 (1.25–1.81) | 0.00 | 1.67 (1.44–1.93) | 0.00 |
| 1.24 (1.02–1.50) | 0.03 | 1.39 (1.18–1.64) | 0.00 | 2.68 (2.20–3.26) | 0.00 | 3.56 (2.98–4.24) | 0.00 | 2.04 (1.68–2.47) | 0.00 | 2.19 (1.85–2.60) | 0.00 |
| Hypertension | 0.77 (0.70–0.84) | 0.00 | 0.84 (0.76–0.92) | 0.00 | 0.31 (0.28–0.34) | 0.00 | 0.27 (0.24–0.30) | 0.00 | 0.50 (0.46–0.55) | 0.00 | 0.53 (0.48–0.58) | 0.00 |
| Diabetes | 1.15 (1.00–1.32) | 0.04 | 1.06 (0.92–1.23) | 0.39 | 0.47 (0.41–0.54) | 0.00 | 0.46 (0.40–0.53) | 0.00 | 0.69 (0.60–0.79) | 0.00 | 0.61 (0.53–0.71) | 0.00 |
| Dyslipidaemia | 0.73 (0.66–0.80) | 0.00 | 0.76 (0.69–0.84) | 0.00 | 0.70 (0.64–0.77) | 0.00 | 0.64 (0.58–0.71) | 0.00 | 0.64 (0.58–0.70) | 0.00 | 0.69 (0.63–0.76) | 0.00 |
| CVD | 0.17 (0.14–0.20) | 0.00 | 0.13 (0.11–0.16) | 0.00 | 0.58 (0.51–0.66) | 0.00 | 0.59 (0.51–0.67) | 0.00 | 0.65 (0.57–0.75) | 0.00 | 0.60 (0.52–0.69) | 0.00 |
| Overweight | 0.62 (0.55–0.70) | 0.00 | 0.63 (0.56–0.72) | 0.00 | 0.48 (0.42–0.55) | 0.00 | 0.51 (0.45–0.59) | 0.00 | 0.59 (0.52–0.67) | 0.00 | 0.56 (0.48–0.64) | 0.00 |
| Obesity | 0.59 (0.52–0.67) | 0.00 | 0.60 (0.53–0.69) | 0.00 | 0.28 (0.25–0.32) | 0.00 | 0.28 (0.25–0.32) | 0.00 | 0.38 (0.34–0.44) | 0.00 | 0.33 (0.29–0.38) | 0.00 |
| Exceeded waist circumference (W ≥ 80 cm; M ≥ 94 cm) | 0.63 (0.56–0.71) | 0.00 | 0.64 (0.57–0.72) | 0.00 | 0.43 (0.38–0.49) | 0.00 | 0.39 (0.34–0.44) | 0.00 | 0.45 (0.40–0.51) | 0.00 | 0.45 (0.39–0.51) | 0.00 |
| Abdominal obesity | 0.81 (0.74–0.90) | 0.00 | 0.86 (0.78–0.95) | 0.00 | 0.67 (0.60–0.73) | 0.00 | 0.66 (0.60–0.73) | 0.00 | 0.64 (0.58–0.70) | 0.00 | 0.65 (0.59–0.72) | 0.00 |
| Smoking status | ||||||||||||
| 0.85 (0.76–0.95) | 0.00 | 0.82 (0.74–0.92) | 0.00 | 0.78 (0.70–0.87) | 0.00 | 0.90 (0.80–1.00) | 0.06 | 0.78 (0.70–0.86) | 0.00 | 0.86 (0.77–0.96) | 0.01 |
| 0.80 (0.70–0.91) | 0.00 | 0.79 (0.68–0.90) | 0.00 | 0.99 (0.87–1.13) | 0.90 | 1.02 (0.89–1.18) | 0.73 | 0.85 (0.74–0.97) | 0.01 | 0.95 (0.83–1.10) | 0.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Studziński, K.; Tomasik, T.; Windak, A.; Banach, M.; Wójtowicz, E.; Mastej, M.; Tomaszewski, M.; Mikhailidis, D.P.; Toth, P.P.; Catapano, A.; et al. The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study. J. Clin. Med. 2021, 10, 5656. https://doi.org/10.3390/jcm10235656
Studziński K, Tomasik T, Windak A, Banach M, Wójtowicz E, Mastej M, Tomaszewski M, Mikhailidis DP, Toth PP, Catapano A, et al. The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study. Journal of Clinical Medicine. 2021; 10(23):5656. https://doi.org/10.3390/jcm10235656
Chicago/Turabian StyleStudziński, Krzysztof, Tomasz Tomasik, Adam Windak, Maciej Banach, Ewa Wójtowicz, Mirosław Mastej, Maciej Tomaszewski, Dimitri P. Mikhailidis, Peter P. Toth, Alberico Catapano, and et al. 2021. "The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study" Journal of Clinical Medicine 10, no. 23: 5656. https://doi.org/10.3390/jcm10235656
APA StyleStudziński, K., Tomasik, T., Windak, A., Banach, M., Wójtowicz, E., Mastej, M., Tomaszewski, M., Mikhailidis, D. P., Toth, P. P., Catapano, A., Ray, K. K., Howard, G., Lip, G. Y. H., Charchar, F. J., Sattar, N., Williams, B., MacDonald, T. M., Penson, P. E., Jóźwiak, J. J., & on behalf of the LIPIDOGRAM2015 Investigators. (2021). The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study. Journal of Clinical Medicine, 10(23), 5656. https://doi.org/10.3390/jcm10235656









