Special Teaching Formats during the COVID-19 Pandemic—A Survey with Implications for a Crisis-Proof Education
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Theoretical Education
2.3. Practical Education
2.4. Final Examination
2.5. Questionnaire
2.6. Statistics
3. Results
3.1. Evaluation of the General Learning Conditions
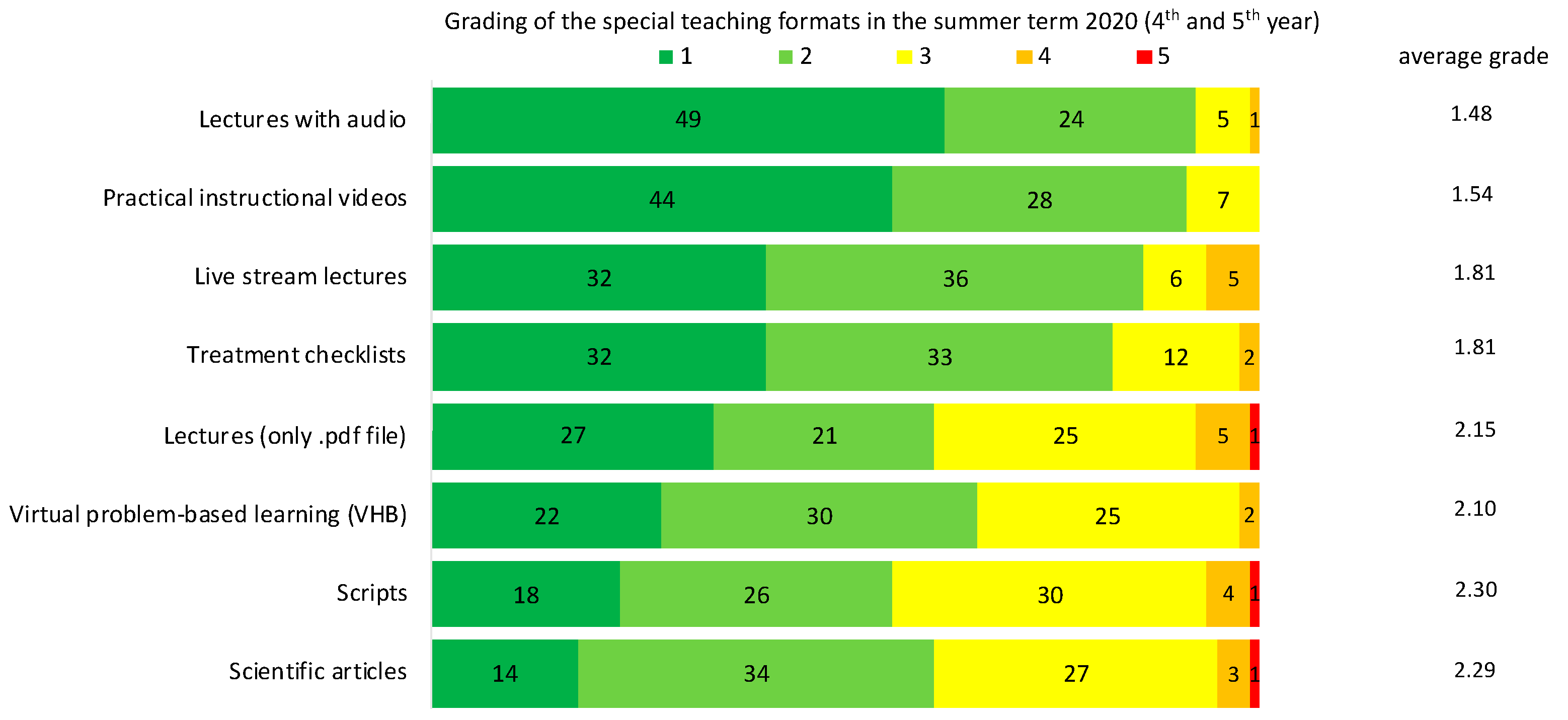
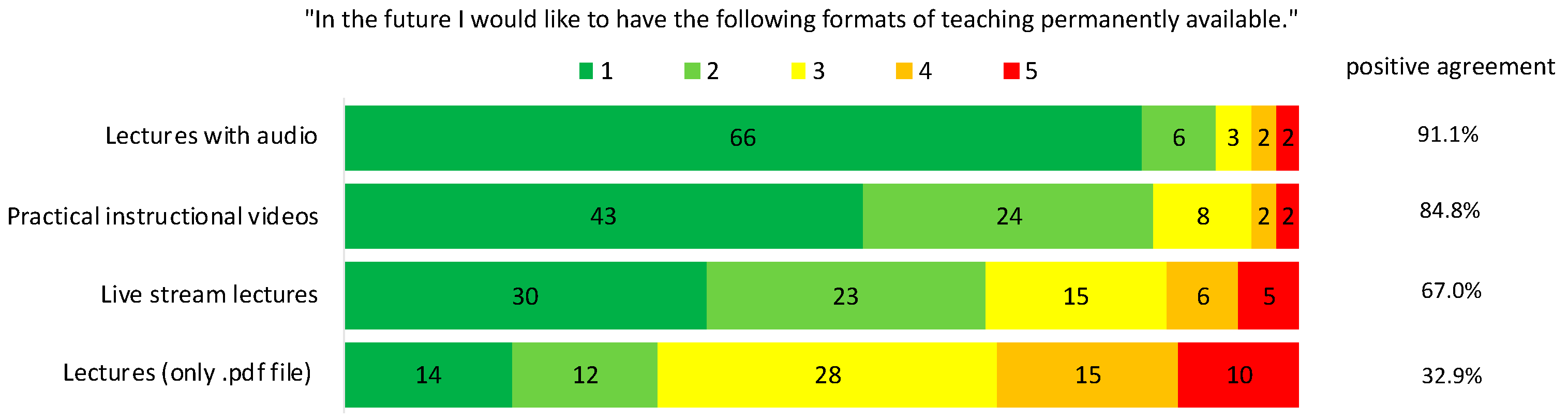
3.2. Evaluation of Theoretical Teaching Formats
3.3. Evaluation of the Practical Training
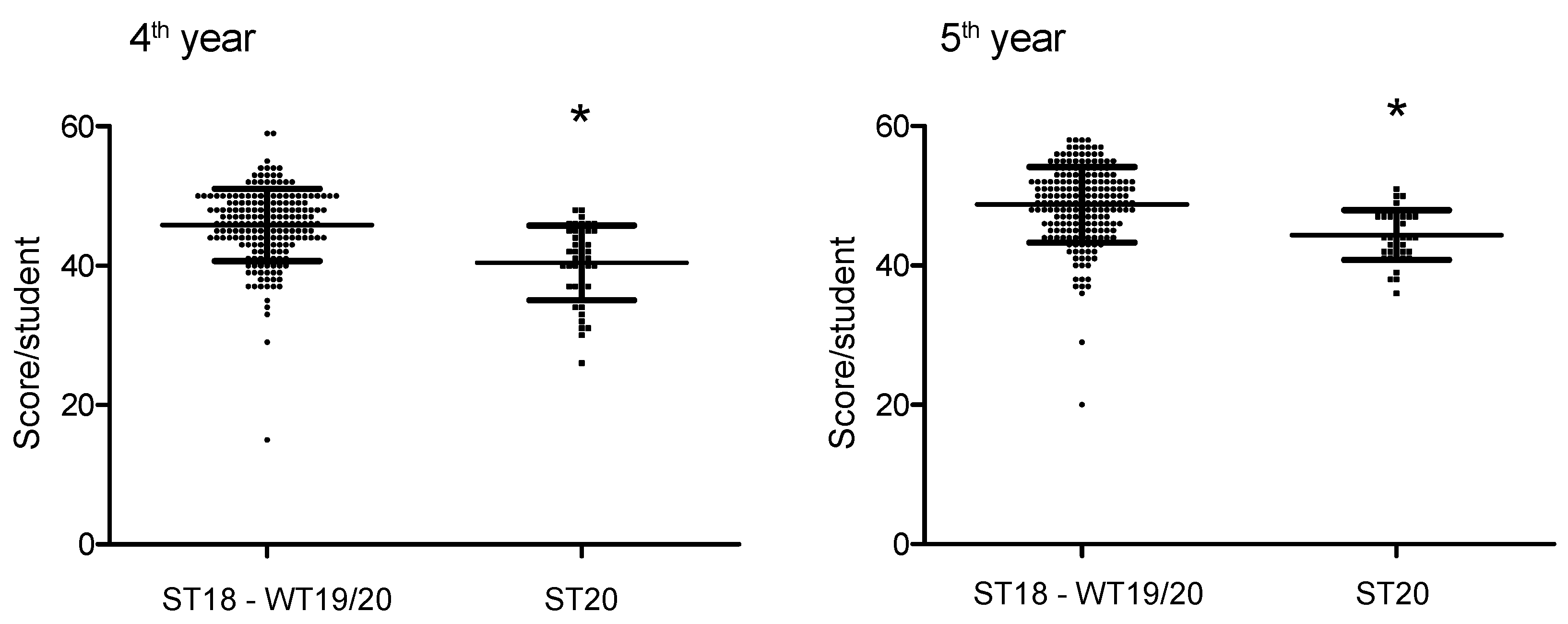
3.4. Final Examination
4. Discussion
4.1. Theoretical Education
4.2. Practical Education
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Europe’s Standing Committee. WHO Declares COVID 19 Outbreak a Pandemic. Available online: https://www.euro.who.int/de/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 13 April 2020).
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walter, E.; von Bronk, L.; Hickel, R.; Huth, K.C. Impact of COVID-19 on Dental Care during a National Lockdown: A Retrospective Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 7963. [Google Scholar] [CrossRef] [PubMed]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Serrano, J.; Roldán, S.; Sanz, M. Is the oral cavity relevant in SARS-CoV-2 pandemic? Clin. Oral Investig. 2020, 24, 2925–2930. [Google Scholar] [CrossRef]
- Diegritz, C.; Manhart, J.; Bücher, K.; Grabein, B.; Schuierer, G.; Kühnisch, J.; Kunzelmann, K.-H.; Hickel, R.; Fotiadou, C. A detailed report on the measures taken in the Department of Conservative Dentistry and Periodontology in Munich at the beginning of the COVID-19 outbreak. Clin. Oral Investig. 2020, 24, 2931–2941. [Google Scholar] [CrossRef]
- Chang, T.-Y.; Hong, G.; Paganelli, C.; Phantumvanit, P.; Chang, W.-J.; Shieh, Y.-S.; Hsu, M.-L. Innovation of dental education during COVID-19 pandemic. J. Dent. Sci. 2020, 16, 15–20. [Google Scholar] [CrossRef]
- Desai, B.K. Clinical implications of the COVID-19 pandemic on dental education. J. Dent. Educ. 2020, 84, 512. [Google Scholar] [CrossRef]
- Iyer, P.; Aziz, K.; Ojcius, D.M. Impact of COVID-19 on dental education in the United States. J. Dent. Educ. 2020, 84, 718–722. [Google Scholar] [CrossRef]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; Krämer, N.; Schulz-Weidner, N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): A cross-sectional study. BMC Med. Educ. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Machado, R.A.; Bonan, P.R.F.; Perez, D.E.d.C.; Martelli JÚnior, H. COVID-19 pandemic and the impact on dental education: Discussing current and future perspectives. Braz. Oral Res. 2020, 34, e083. [Google Scholar] [CrossRef] [PubMed]
- Quinn, B.; Field, J.; Gorter, R.; Akota, I.; Manzanares, M.; Paganelli, C.; Davies, J.; Dixon, J.; Gabor, G.; Amaral Mendes, R. COVID-19: The immediate response of european academic dental institutions and future implications for dental education. Eur. J. Dent. Educ. 2020, 24, 811–814. [Google Scholar] [CrossRef] [PubMed]
- Goob, J.; Erdelt, K.; Güth, J.F.; Liebermann, A. Dental education during the pandemic: Cross-sectional evaluation of four different teaching concepts. J. Dent. Educ. 2021, 85, 1574–1587. [Google Scholar] [CrossRef] [PubMed]
- Varvara, G.; Bernardi, S.; Bianchi, S.; Sinjari, B.; Piattelli, M. Dental Education Challenges during the COVID-19 Pandemic Period in Italy: Undergraduate Student Feedback, Future Perspectives, and the Needs of Teaching Strategies for Professional Development. Healthcare 2021, 9, 454. [Google Scholar] [CrossRef]
- Hattar, S.; AlHadidi, A.; Sawair, F.A.; Abd Alraheam, I.; El-Ma’aita, A.; Wahab, F.K. Impact of COVID-19 pandemic on dental education: Online experience and practice expectations among dental students at the University of Jordan. BMC Med. Educ. 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, K.; El-Kishawi, M.; Moufti, M.A.; Al Kawas, S. Introducing a comprehensive high-stake online exam to final-year dental students during the COVID-19 pandemic and evaluation of its effectiveness. Med. Educ. Online 2020, 25, 1826861. [Google Scholar] [CrossRef] [PubMed]
- Universität Bayern e.V.; Bayerische Universitätenkonferenz. Richtlinien zum Vollzug der Bayerischen Infektionsschutzmaßnahmenverordnung an den Bayerischen Universitäten. Available online: https://www.mathematik-informatik-statistik.uni-muenchen.de/e-mails-corona/corona-update-_30_4_20-21_30_.pdf (accessed on 6 July 2020).
- Ludwig-Maximilians Universität. Ergänzende Regelungen der LMU zu den Richtlinien des Universität Bayern e.V. zum Vollzug der Bayerischen Infektionsschutzmaßnahmenverordnung an den bayerischen Universitäten. Available online: https://www.studium.geowissenschaften.uni-muenchen.de/aktuelles/20-06-30-lmu-ergaenzende-regelungen-infektionsschutz.pdf (accessed on 10 July 2020).
- Al Kawas, S.; Al-Rawi, N.; Talaat, W.; Hamdoon, Z.; Salman, B.; Al Bayatti, S.; Jerjes, W.; Samsudin, A.R. Post COVID-19 lockdown: Measures and practices for dental institutes. BMC Oral Health 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Rohlin, M.; Petersson, K.; Svensäter, G. The Malmö model: A problem-based learning curriculum in undergraduate dental education. Eur. J. Dent. Educ. 1998, 2, 103–114. [Google Scholar] [CrossRef]
- Larsen, T.; Jeppe-Jensen, D. The introduction and perception of an OSCE with an element of self-and peer-assessment. Eur. J. Dent. Educ. 2008, 12, 2–7. [Google Scholar] [CrossRef]
- Bassir, S.H.; Sadr-Eshkevari, P.; Amirikhorheh, S.; Karimbux, N.Y. Problem–Based Learning in Dental Education: A Systematic Review of the Literature. J. Dent. Educ. 2014, 78, 98–109. [Google Scholar] [CrossRef]
- Fischer, M.R.; Bauer, D.; Karin Mohn, N. Finally finished! National competence based catalogues of learning objectives for undergraduate medical education (NKLM) and dental education (NKLZ) ready for trial. GMS Z. Für Med. Ausbild. 2015, 32, Doc35. [Google Scholar]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D printed replicas for endodontic education. Int. Endod. J. 2019, 52, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Gerhard-Szep, S.; Guentsch, A.; Pospiech, P.; Söhnel, A.; Scheutzel, P.; Wassmann, T.; Zahn, T. Assessment formats in dental medicine: An overview. GMS J. Med. Educ. 2016, 33, 6–8. [Google Scholar] [CrossRef]
- Kurtz, S.; Silverman, J. The Calgary—Cambridge Referenced Observation Guides: An aid to defining the curriculum and organizing the teaching in communication training programmes. Med. Educ. 1996, 30, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Kollewe, T.; Sennekamp, M.; Ochsendorf, F. Medizindidaktik; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- McGaghie, W.C.; Issenberg, S.B.; Petrusa, E.R.; Scalese, R.J. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010, 44, 50–63. [Google Scholar] [CrossRef]
- Kurtz, S.; Draper, J.; Silverman, J. Teaching and Learning Communication Skills in Medicine; CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Haladyna, T.M. Developing and Validating Multiple-Choice Test Items; Routledge: New York, NY, USA, 2004. [Google Scholar]
- Bauer, D.; Holzer, M.; Kopp, V.; Fischer, M.R. Pick-N multiple choice-exams: A comparison of scoring algorithms. Adv. Health Sci. Educ. 2011, 16, 211–221. [Google Scholar] [CrossRef] [Green Version]
- Carney, O.; McIntosh, J.; Worth, A. The use of the nominal group technique in research with community nurses. J. Adv. Nurs. 1996, 23, 1024–1029. [Google Scholar] [CrossRef]
- Gallagher, M.; Hares, T.; Spencer, J.; Bradshaw, C.; Webb, I. The nominal group technique: A research tool for general practice? Fam. Pract. 1993, 10, 76–81. [Google Scholar] [CrossRef]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 140, 1–55. [Google Scholar]
- Sullivan, G.M.; Artino, A.R., Jr. Analyzing and interpreting data from Likert-type scales. J. Grad. Med Educ. 2013, 5, 541. [Google Scholar] [CrossRef] [Green Version]
- Mukhtar, K.; Javed, K.; Arooj, M.; Sethi, A. Advantages, Limitations and Recommendations for online learning during COVID-19 pandemic era. Pak. J. Med Sci. 2020, 36, S27. [Google Scholar] [CrossRef]
- Abbasi, S.; Ayoob, T.; Malik, A.; Memon, S.I. Perceptions of students regarding E-learning during Covid-19 at a private medical college. Pak. J. Med Sci. 2020, 36, S57. [Google Scholar] [CrossRef]
- Chen, E.; Kaczmarek, K.; Ohyama, H. Student perceptions of distance learning strategies during COVID-19. J. Dent. Educ. 2020, 85, 1190–1191. [Google Scholar] [CrossRef]
- De Oliveira Araújo, F.J.; de Lima, L.S.A.; Cidade, P.I.M.; Nobre, C.B.; Neto, M.L.R. Impact of Sars-Cov-2 and its reverberation in global higher education and mental health. Psychiatry Res. 2020, 288, 112977. [Google Scholar] [CrossRef]
- Silverman, J.; Kurtz, S.; Draper, J. Skills for Communicating with Patients; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Field, J.; Cowpe, J.; Walmsley, A. The graduating European dentist: A new undergraduate curriculum framework. Eur. J. Dent. Educ. 2017, 21, 2–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cowpe, J.; Plasschaert, A.; Harzer, W.; Vinkka-Puhakka, H.; Walmsley, A.D. Profile and competences for the graduating European dentist–update 2009. Eur. J. Dent. Educ. 2010, 14, 193–202. [Google Scholar] [CrossRef]
- Miller, G.E. The assessment of clinical skills/competence/performance. Acad. Med. 1990, 65, S63–S67. [Google Scholar] [CrossRef] [PubMed]
- Kolb, D.A. Experience as the source of learning and development. Up. Sadle River Prentice Hall 1984, 2, 31–49. [Google Scholar]
- Bundesgesundheitsministerium. Approbationsordnung für Zahnärzte und Zahnärztinnen (ZApprO). 2019. Available online: https://www.buzer.de/ZApprO.htm (accessed on 4 January 2020).

| Teaching Format | Regular Term | Corona Summer Term 2020 | |
|---|---|---|---|
| Theoretical Education | Lectures with audio (n) | None | 41 |
| 33 additionally as .pdf files | |||
| 8 exclusively as lectures with audio | |||
| Live stream lectures (n) | None | 10 | |
| 8 additionally as .pdf files | |||
| 2 exclusively as live stream lectures | |||
| Practical instructional videos (n) | 62 | 64 | |
| Introducing videos (e.g., hygiene briefing) (n) | None | 6 | |
| Treatment checklists (n) | 7 | 7 | |
| Lectures (only .pdf file) (n) | 41 | 43 | |
| 33 additionally as lectures with audio | |||
| 10 exclusively available as .pdf files) | |||
| Virtual problem-based learning (VHB) (n) | 6 | 6 | |
| Scripts (n) | 2 | 2 | |
| Scientific articles/recommended literature (n) | None | 6 | |
| Case presentation (endodontology) (n) | None | 1 | |
| Tutorial periodontology (n) | None | 1 | |
| Practical education | Restorative Dentistry | Regular patient treatment | Phantom head treatment, |
| add on in clinical difficulty (veneers) | |||
| Endodontology | Regular patient treatment | Phantom head treatment, | |
| Problem based Learning (PBL) case presentations, root canal treatment using 3D printed teeth | |||
| Periodontology | Regular patient treatment | Phantom head treatment, | |
| Tutorial (PBL) followed by virtual presentations OSPE including communication training with simulated patients |
| How do you rate your personal learning success with regard to the individual theoretical teaching forms in the summer term 2020? | |||||
| Lectures with audio |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| Live Stream lectures |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| Lectures (only .pdf files) |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| Scripts |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| Scientific articles |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| Virtual problem-based learning (VHB) |  Very good |  Good |  Satisfactory |  Bad |  Very bad |
| In the future I would like to have “Lectures with audio” permanently available |  Fully agree |  Rather agree |  Partially agree |  Disagree |  Disagree at all |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huth, K.C.; von Bronk, L.; Kollmuss, M.; Lindner, S.; Durner, J.; Hickel, R.; Draenert, M.E. Special Teaching Formats during the COVID-19 Pandemic—A Survey with Implications for a Crisis-Proof Education. J. Clin. Med. 2021, 10, 5099. https://doi.org/10.3390/jcm10215099
Huth KC, von Bronk L, Kollmuss M, Lindner S, Durner J, Hickel R, Draenert ME. Special Teaching Formats during the COVID-19 Pandemic—A Survey with Implications for a Crisis-Proof Education. Journal of Clinical Medicine. 2021; 10(21):5099. https://doi.org/10.3390/jcm10215099
Chicago/Turabian StyleHuth, Karin Christine, Leonard von Bronk, Maximilian Kollmuss, Stefanie Lindner, Jürgen Durner, Reinhard Hickel, and Miriam Esther Draenert. 2021. "Special Teaching Formats during the COVID-19 Pandemic—A Survey with Implications for a Crisis-Proof Education" Journal of Clinical Medicine 10, no. 21: 5099. https://doi.org/10.3390/jcm10215099
APA StyleHuth, K. C., von Bronk, L., Kollmuss, M., Lindner, S., Durner, J., Hickel, R., & Draenert, M. E. (2021). Special Teaching Formats during the COVID-19 Pandemic—A Survey with Implications for a Crisis-Proof Education. Journal of Clinical Medicine, 10(21), 5099. https://doi.org/10.3390/jcm10215099






