Recent Advances in the Treatment of Spasticity: Extracorporeal Shock Wave Therapy
Abstract
1. Introduction
2. Effects on Neuromuscular Tissues
2.1. Inducing NO Production
2.2. Reducing Motor Neuron Excitability
2.3. Dysfunction in Neuromuscular Transmission
2.4. Affecting Rheological Properties
3. Radial vs. Focused ESWT
4. Site and Duration of Application
5. Adverse Effect
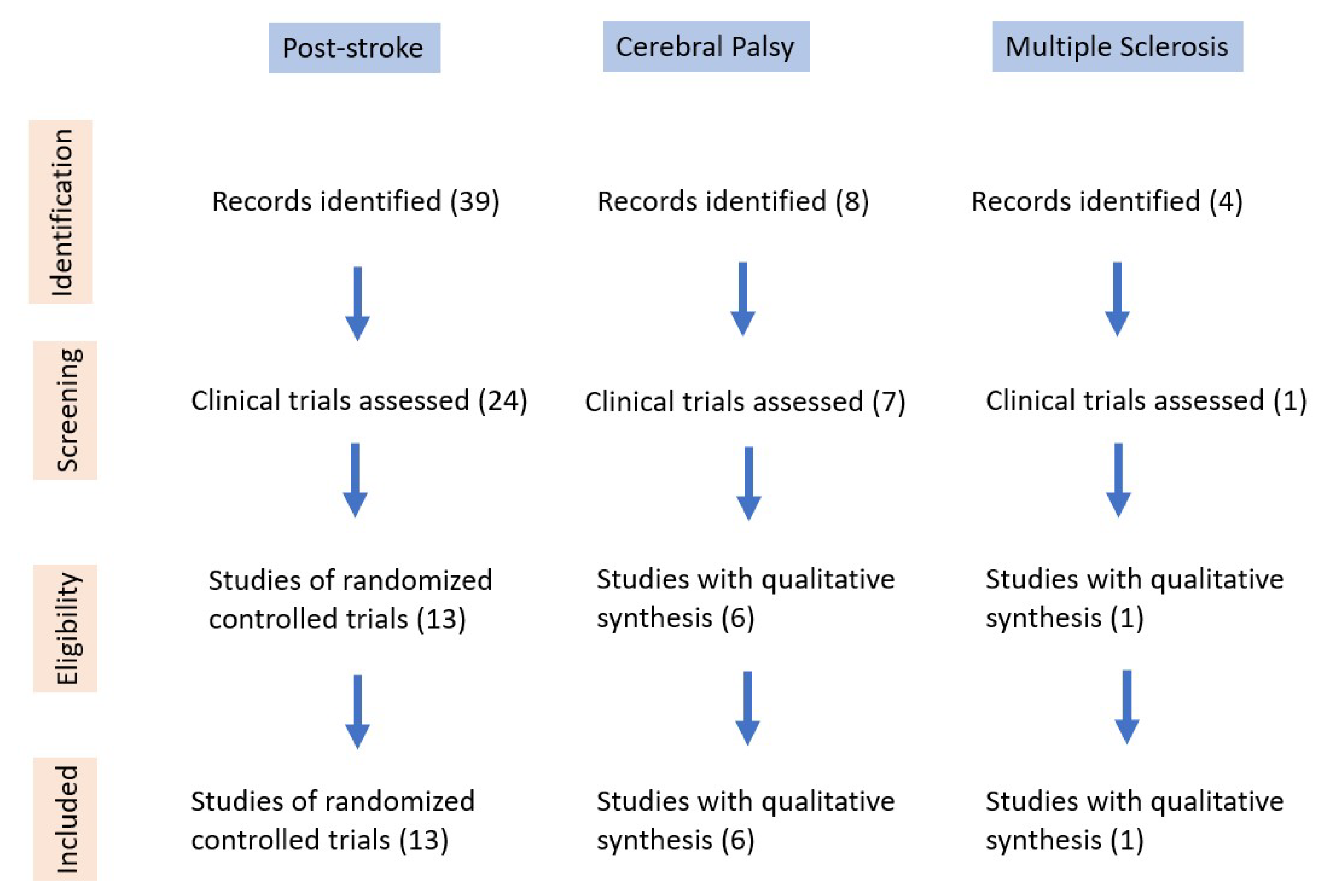
6. Effect of ESWT in Different Clinical Conditions
6.1. Post-Stroke Upper Limb Spasticity
6.1.1. Intensity, Frequency, and Dosage
6.1.2. Clinical Assessment
6.1.3. Functional Assessment
6.1.4. Other Assessments
6.2. Post-Stroke Lower Limb Spasticity
6.2.1. Intensity, Frequency, and Dosage
6.2.2. Clinical Assessment
6.2.3. Functional Assessment
6.2.4. Other Assessments
6.3. Spasticity in CP Patients
6.3.1. Intensity, Frequency, and Dosage
6.3.2. Clinical Assessment
6.4. Spasticity in Multiple Sclerosis
6.5. Botulinum Toxin Injections and EWST
6.5.1. ESWT vs. BTX
6.5.2. ESWT and BTX
7. Limitation
8. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mukherjee, A.; Chakravarty, A. Spasticity mechanisms—For the clinician. Front. Neurol. 2010, 1, 149. [Google Scholar] [CrossRef] [PubMed]
- Bensmail, D.; Wissel, J.; Laffont, I.; Simon, O.; Scheschonka, A.; Flatau-Baqué, B.; Dressler, D.; Simpson, D.M. Efficacy of incobotulinumtoxinA for the treatment of adult lower-limb post-stroke spasticity, including pes equinovarus. Ann. Phys. Rehabil. Med. 2021, 64, 101376. [Google Scholar] [CrossRef] [PubMed]
- Sunnerhagen, K.S.; Opheim, A.; Alt Murphy, M. Onset, time course and prediction of spasticity after stroke or traumatic brain injury. Ann. Phys. Rehabil. Med. 2019, 62, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-H.; Ho, Y.-C.; Hsiao, M.-Y.; Chen, W.-S.; Wang, T.-G. Evaluation of Post-Stroke Spastic Muscle Stiffness Using Shear Wave Ultrasound Elastography. Ultrasound Med. Biol. 2017, 43, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Hobart, J.C.; Riazi, A.; Thompson, A.J.; Styles, I.M.; Ingram, W.; Vickery, P.J.; Warner, M.; Fox, P.J.; Zajicek, J.P. Getting the measure of spasticity in multiple sclerosis: The Multiple Sclerosis Spasticity Scale (MSSS-88). Brain 2006, 129, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Pulgar, S.; Bains, S.; Gooch, J.; Chambers, H.; Noritz, G.H.; Wright, E.; Sawhney, T.G.; Pyenson, B.; Ferro, C. Prevalence, Patterns, and Cost of Care for Children with Cerebral Palsy Enrolled in Medicaid Managed Care. J. Manag. Care Spec. Pharm. 2019, 25, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Abogunrin, S.; Kurth, H.; Dinet, J. Epidemiological, humanistic, and economic burden of illness of lower limb spasticity in adults: A systematic review. Neuropsychiatr. Dis. Treat. 2014, 10, 111–122. [Google Scholar] [CrossRef]
- Khan, F.; Amatya, B.; Bensmail, D.; Yelnik, A. Non-pharmacological interventions for spasticity in adults: An overview of systematic reviews. Ann. Phys. Rehabil. Med. 2019, 62, 265–273. [Google Scholar] [CrossRef]
- Dymarek, R.; Ptaszkowski, K.; Słupska, L.; Halski, T.; Taradaj, J.; Rosińczuk, J. Effects of extracorporeal shock wave on upper and lower limb spasticity in post-stroke patients: A narrative review. Top. Stroke Rehabil. 2016, 23, 293–303. [Google Scholar] [CrossRef]
- Opara, J.; Taradaj, J.; Walewicz, K.; Rosińczuk, J.; Dymarek, R. The Current State of Knowledge on the Clinical and Methodological Aspects of Extracorporeal Shock Waves Therapy in the Management of Post-Stroke Spasticity-Overview of 20 Years of Experiences. J. Clin. Med. 2021, 10, 261. [Google Scholar] [CrossRef]
- Dymarek, R.; Ptaszkowski, K.; Ptaszkowska, L.; Kowal, M.; Sopel, M.; Taradaj, J.; Rosińczuk, J. Shock Waves as a Treatment Modality for Spasticity Reduction and Recovery Improvement in Post-Stroke Adults—Current Evidence and Qualitative Systematic Review. Clin. Interv. Aging. 2020, 15, 9–28. [Google Scholar] [CrossRef]
- Wang, C.J.; Wang, F.S.; Yang, K.D.; Weng, L.H.; Hsu, C.C.; Huang, C.S.; Yang, L.C. Shock wave therapy induces neovascularization at the tendon-bone junction. A study in rabbits. J. Orthop. Res. 2003, 21, 984–989. [Google Scholar] [CrossRef]
- Mariotto, S.; Cavalieri, E.; Amelio, E.; Ciampa, A.R.; de Prati, A.C.; Marlinghaus, E.; Russo, S.; Suzuki, H. Extracorporeal shock waves: From lithotripsy to anti-inflammatory action by NO production. Nitric Oxide 2005, 12, 89–96. [Google Scholar] [CrossRef]
- Xiang, J.; Wang, W.; Jiang, W.; Qian, Q. Effects of extracorporeal shock wave therapy on spasticity in post-stroke patients: A systematic review and meta-analysis of randomized controlled trials. J. Rehabil. Med. 2018, 50, 852–859. [Google Scholar] [CrossRef]
- Moon, S.W.; Kim, J.H.; Jung, M.J.; Son, S.; Lee, J.H.; Shin, H.; Lee, E.S.; Yoon, C.H.; Oh, M.K. The effect of extracorporeal shock wave therapy on lower limb spasticity in subacute stroke patients. Ann. Rehabil. Med. 2013, 37, 461–470. [Google Scholar] [CrossRef]
- Kenmoku, T.; Ochiai, N.; Ohtori, S.; Saisu, T.; Sasho, T.; Nakagawa, K.; Iwakura, N.; Miyagi, M.; Ishikawa, T.; Tatsuoka, H.; et al. Degeneration and recovery of the neuromuscular junction after application of extracorporeal shock wave therapy. J. Orthop. Res. 2012, 30, 1660–1665. [Google Scholar] [CrossRef]
- Manganotti, P.; Amelio, E. Long-term effect of shock wave therapy on upper limb hypertonia in patients affected by stroke. Stroke 2005, 36, 1967–1971. [Google Scholar] [CrossRef]
- Blottner, D.; Lück, G. Just in time and place: NOS/NO system assembly in neuromuscular junction formation. Microsc. Res. Tech. 2001, 55, 171–180. [Google Scholar] [CrossRef]
- Hasuk, B.; Min, L.J.; Hwan, L.K. The Effects of Extracorporeal Shock Wave Therapy on Spasticity in Chronic Stroke Patients. Ann. Rehabil. Med. 2010, 34, 663–669. [Google Scholar]
- Leone, J.A.; Kukulka, C.G. Effects of tendon pressure on alpha motoneuron excitability in patients with stroke. Phys. Ther. 1988, 68, 475–480. [Google Scholar] [CrossRef]
- Leng, Y.; Lo, W.L.A.; Hu, C.; Bian, R.; Xu, Z.; Shan, X.; Huang, D.; Li, L. The Effects of Extracorporeal Shock Wave Therapy on Spastic Muscle of the Wrist Joint in Stroke Survivors: Evidence from Neuromechanical Analysis. Front. Neurosci. 2021, 14, 580762. [Google Scholar] [CrossRef]
- Manganotti, P.; Amelio, E.; Guerra, C. Shock wave over hand muscles: A neurophysiological study on peripheral conduction nerves in normal subjects. Muscl. Lig. Tendons J. 2012, 2, 104–107. [Google Scholar]
- Dymarek, R.; Taradaj, J.; Rosińczuk, J. Extracorporeal Shock Wave Stimulation as Alternative Treatment Modality for Wrist and Fingers Spasticity in Poststroke Patients: A Prospective, Open-Label, Preliminary Clinical Trial. Evid.-Based Complement. Altern. Med. 2016, 2016, 4648101. [Google Scholar] [CrossRef]
- Foldager, C.B.; Kearney, C.; Spector, M. Clinical application of extracorporeal shock wave therapy in orthopedics: Focused versus unfocused shock waves. Ultrasound Med. Biol. 2012, 38, 1673–1680. [Google Scholar] [CrossRef]
- Wu, Y.T.; Chang, C.N.; Chen, Y.M.; Hu, G.C. Comparison of the effect of focused and radial extracorporeal shock waves on spastic equinus in patients with stroke: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 518–525. [Google Scholar] [CrossRef]
- Yoon, S.H.; Shin, M.K.; Choi, E.J.; Kang, H.J. Effective Site for the Application of Extracorporeal Shock-Wave Therapy on Spasticity in Chronic Stroke: Muscle Belly or Myotendinous Junction. Ann. Rehabil. Med. 2017, 41, 547–555. [Google Scholar] [CrossRef]
- Li, G.; Yuan, W.; Liu, G.; Qiao, L.; Zhang, Y.; Wang, Y.; Wang, W.; Zhao, M.; Wang, Y.; Wang, J. Effects of radial extracorporeal shockwave therapy on spasticity of upper-limb agonist/antagonist muscles in patients affected by stroke: A randomized, single-blind clinical trial. Age Ageing 2020, 49, 246–252. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, S.N.; Lee, I.S.; Jung, H.; Lee, K.S.; Koh, S.E. Effects of Extracorporeal Shock Wave Therapy on Spasticity in Patients after Brain Injury: A Meta-analysis. J. Phys. Ther. Sci. 2014, 26, 1641–1647. [Google Scholar] [CrossRef]
- Guo, P.; Gao, F.; Zhao, T.; Sun, W.; Wang, B.; Li, Z. Positive Effects of Extracorporeal Shock Wave Therapy on Spasticity in Poststroke Patients: A Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2017, 26, 2470–2476. [Google Scholar] [CrossRef]
- Oh, J.H.; Park, H.D.; Han, S.H.; Shim, G.Y.; Choi, K.Y. Duration of Treatment Effect of Extracorporeal Shock Wave on Spasticity and Subgroup-Analysis According to Number of Shocks and Application Site: A Meta-Analysis. Ann. Rehabil. Med. 2019, 43, 163–177. [Google Scholar] [CrossRef]
- Cifu, D.X. Braddom’s Physical Medicine and Rehabilitation, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Radinmehr, H.; Nakhostin Ansari, N.; Naghdi, S.; Olyaei, G.; Tabatabaei, A. Effects of one session radial extracorporeal shockwave therapy on post-stroke plantarflexor spasticity: A single-blind clinical trial. Disabil. Rehabil. 2017, 39, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Santamato, A.; Micello, M.F.; Panza, F.; Fortunato, F.; Logroscino, G.; Picelli, A.; Manganotti, P.; Smania, N.; Fiore, P.; Ranieri, M. Extracorporeal shock wave therapy for the treatment of poststroke plantar-flexor muscles spasticity: A prospective open-label study. Top. Stroke Rehabil. 2014, 21 (Suppl. 1), S17–S24. [Google Scholar] [CrossRef] [PubMed]
- Santamato, A.; Notarnicola, A.; Panza, F.; Ranieri, M.; Micello, M.F.; Manganotti, P.; Moretti, B.; Fortunato, F.; Filoni, S.; Fiore, P. SBOTE study: Extracorporeal shock wave therapy versus electrical stimulation after botulinum toxin type a injection for post-stroke spasticity-a prospective randomized trial. Ultrasound Med. Biol. 2013, 39, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Dymarek, R.; Taradaj, J.; Rosińczuk, J. The Effect of Radial Extracorporeal Shock Wave Stimulation on Upper Limb Spasticity in Chronic Stroke Patients: A Single-Blind, Randomized, Placebo-Controlled Study. Ultrasound Med. Biol. 2016, 42, 1862–1875. [Google Scholar] [CrossRef]
- Li, T.Y.; Chang, C.Y.; Chou, Y.C.; Chen, L.C.; Chu, H.Y.; Chiang, S.L.; Chang, S.T.; Wu, Y.T. Effect of Radial Shock Wave Therapy on Spasticity of the Upper Limb in Patients with Chronic Stroke: A Prospective, Randomized, Single Blind, Controlled Trial. Medicine 2016, 95, e3544. [Google Scholar] [CrossRef]
- Wu, Y.T.; Yu, H.K.; Chen, L.R.; Chang, C.N.; Chen, Y.M.; Hu, G.C. Extracorporeal Shock Waves Versus Botulinum Toxin Type A in the Treatment of Poststroke Upper Limb Spasticity: A Randomized Noninferiority Trial. Arch. Phys. Med. Rehabil. 2018, 99, 2143–2150. [Google Scholar] [CrossRef]
- Park, S.K.; Yang, D.J.; Uhm, Y.H.; Yoon, J.H.; Kim, J.H. Effects of extracorporeal shock wave therapy on upper extremity muscle tone in chronic stroke patients. J. Phys. Ther. Sci. 2018, 30, 361–364. [Google Scholar] [CrossRef][Green Version]
- Taheri, P.; Vahdatpour, B.; Mellat, M.; Ashtari, F.; Akbari, M. Effect of Extracorporeal Shock Wave Therapy on Lower Limb Spasticity in Stroke Patients. Arch. Iran. Med. 2017, 20, 338–343. [Google Scholar]
- Lee, C.H.; Lee, S.H.; Yoo, J.I.; Lee, S.U. Ultrasonographic Evaluation for the Effect of Extracorporeal Shock Wave Therapy on Gastrocnemius Muscle Spasticity in Patients with Chronic Stroke. PM R 2019, 11, 363–371. [Google Scholar] [CrossRef]
- Radinmehr, H.; Ansari, N.N.; Naghdi, S.; Tabatabaei, A.; Moghimi, E. Comparison of Therapeutic Ultrasound and Radial Shock Wave Therapy in the Treatment of Plantar Flexor Spasticity After Stroke: A Prospective, Single-blind, Randomized Clinical. Trial. J. Stroke Cerebrovasc. Dis. 2019, 28, 1546–1554. [Google Scholar] [CrossRef]
- Yoldaş Aslan, Ş.; Kutlay, S.; Düsünceli Atman, E.; Elhan, A.H.; Gök, H.; Küçükdeveci, A.A. Does extracorporeal shock wave therapy decrease spasticity of ankle plantar flexor muscles in patients with stroke: A randomized controlled trial. Clin. Rehabil 2021, 35, 1442–1453. [Google Scholar] [CrossRef]
- Amelio, E.; Manganotti, P. Effect of shock wave stimulation on hypertonic plantar flexor muscles in patients with cerebral palsy: A placebo-controlled study. J. Rehabil. Med. 2010, 42, 339–343. [Google Scholar] [CrossRef]
- Vidal, X.; Morral, A.; Costa, L.; Tur, M. Radial extracorporeal shock wave therapy (rESWT) in the treatment of spasticity in cerebral palsy: A randomized, placebo-controlled clinical trial. Neuro Rehabil. 2011, 29, 413–419. [Google Scholar] [CrossRef]
- Gonkova, M.I.; Ilieva, E.M.; Ferriero, G.; Chavdarov, I. Effect of radial shock wave therapy on muscle spasticity in children with cerebral palsy. Int. J. Rehabil. Res. 2013, 36, 284–290. [Google Scholar] [CrossRef]
- Wang, T.; Du, L.; Shan, L.; Dong, H.; Feng, J.; Kiessling, M.C.; Angstman, N.B.; Schmitz, C.; Jia, F. A Prospective Case-Control Study of Radial Extracorporeal Shock Wave Therapy for Spastic Plantar Flexor Muscles in Very Young Children with Cerebral Palsy. Medicine 2016, 95, e3649. [Google Scholar] [CrossRef]
- Lin, Y.; Wang, G.; Wang, B. Rehabilitation treatment of spastic cerebral palsy with radial extracorporeal shock wave therapy and rehabilitation therapy. Medicine 2018, 97, e13828. [Google Scholar] [CrossRef]
- Park, D.S.; Kwon, D.R.; Park, G.Y.; Lee, M.Y. Therapeutic Effect of Extracorporeal Shock Wave Therapy According to Treatment Session on Gastrocnemius Muscle Spasticity in Children with Spastic Cerebral Palsy: A Pilot Study. Ann. Rehabil. Med. 2015, 39, 914–921. [Google Scholar] [CrossRef]
- Vidal, X.; Martí-Fàbregas, J.; Canet, O.; Roqué, M.; Morral, A.; Tur, M.; Schmitz, C.; Sitjà-Rabert, M. Efficacy of radial extracorporeal shock wave therapy compared with botulinum toxin type A injection in treatment of lower extremity spasticity in subjects with cerebral palsy: A randomized, controlled, cross-over study. J. Rehabil. Med. 2020, 52, jrm00076. [Google Scholar] [CrossRef]
- Marinelli, L.; Mori, L.; Solaro, C.; Uccelli, A.; Pelosin, E.; Currà, A.; Molfetta, L.; Abbruzzese, G.; Trompetto, C. Effect of radial shock wave therapy on pain and muscle hypertonia: A double-blind study in patients with multiple sclerosis. Mult. Scler. 2015, 21, 622–629. [Google Scholar] [CrossRef]
- Rossetto, O.; Pirazzini, M.; Montecucco, C. Botulinum neurotoxins: Genetic, structural and mechanistic insights. Nat. Rev. Microbiol. 2014, 12, 535–549. [Google Scholar] [CrossRef]
- Weise, D.; Weise, C.M.; Naumann, M. Central Effects of Botulinum Neurotoxin-Evidence from Human Studies. Toxins 2019, 11, 21. [Google Scholar] [CrossRef]
- Picelli, A.; Santamato, A.; Chemello, E.; Cinone, N.; Cisari, C.; Gandolfi, M.; Ranieri, M.; Smania, N.; Baricich, A. Adjuvant treatments associated with botulinum toxin injection for managing spasticity: An overview of the literature. Ann. Phys. Rehabil. Med. 2019, 62, 291–296. [Google Scholar] [CrossRef]

| Author, Year, Country | Design | Grouping | Follow Up | Parameter | Safety |
|---|---|---|---|---|---|
| Santamato 2013, Italy [34] | RCT | BTX with ES (n = 16) BTX with fESWT (n = 16) | 15, 30 and 90 days | MAS (+), SFS (+) VAS (+) | No adverse effect |
| Dymarek 2016, Poland [35] | RCT | Active rESWT (n = 30) Placebo rESWT (n = 30) | Immediately, 1 h, 24 h | MAS (+), sEMG (+) IRT (+) | No adverse effect |
| Li 2016, Taiwan [36] | RCT | Three rESWT sessions (n = 20) Single rESWT session (n = 20) Sham rESWT (n = 20) | Immediately, 1 wk, 4 wks, 8 wks, 12 wks, 16 wks | MAS (+) FMA (+) | NM |
| Yoon 2016, South Korea [26] | RCT | Control group (n = 26) Belly group (n = 26) Junction group (n = 28) | 1 wk after each session(total of four evaluations) | MAS (+) MTS (+) | NM |
| Wu 2018, Taiwan [37] | RCT | ESWT (n = 21) BTX (n = 21) | 1 wk, 4 wks, 8 wks | MAS (+), MTS (+) PROM (+), FMA (+) | No adverse effect |
| Park 2018, South Korea [38] | RCT | ESWT (n = 15) Sham-ESWT (n = 15) | NM | MyotonPRO (+) | NM |
| Li 2020, China [27] | RCT | Control (n = 25) Agonist (n = 27) Antagonist (n = 30) | 24 h, 4 wks | MAS (+); MTS (+) VAS (+), FMA (−) Swelling scale (−) | NM |
| Leng 2021, China [21] | RCT | ESWT (n = 14) Control (n = 13) | Immediately, 1 wk | NeuroFlexor (+) Myotonometer (+) Electrical impedance myography (+) MAS (+), FMA (−) | NM |
| Author | Type of ESWT | Site of Treatment | Number, Interval of Sessions | Pulses (N) | Frequency (Hz) | Pressure (Bars) | EFD (mJ/mm2) |
|---|---|---|---|---|---|---|---|
| Santamato [34] | Focused | FDS | 5, once every day | 2000 | 4 | 1.5 | 0.1 |
| Dymarek [35] | Radial | FCR, FCU, interosseous muscles | 1 | FCU/FCR: 1000 Intrinsic muscles: 3200 | NM | 1.5 | 0.03 |
| Li [36] | Radial | FCR, FCU, intrinsic muscles | Group A: 3 sessions, once every week Group B: 1 session | FCR, FCU: 1500 Intrinsic muscles: 4000 | 5 | 3–3.5 | NM |
| Yoon [26] | Radial | Elbow flexor, biceps, brachialis | 3, once every week | 1500 | 5 | NM | 0.068–0.093 |
| Wu [37] | NM | FCR, FCU, biceps | 3, once every week | 3000 pulses (1000 on each muscle) | 5 | 3.5 | NM |
| Park [38] | NM | Forearm flexors, interosseous muscles | 16, two times a week, total of eight weeks | Forearm flexors: 1500 Interosseous muscles: 3200 (800 each) | NM | NM | 0.03 |
| Li [27] | Radial | Agonist: biceps, brachialis, Pronator teres Antagonist: triceps | 5, 4-day intervals | 6000 | 18 | 1.2–1.4 | 0.06–0.07 |
| Leng [21] | Radial | FCR | 1 | 1500 | 4 | 1.5 | 0.038 |
| Author, Year, Country | Design | Grouping | Follow-Up | Parameter | Safety |
|---|---|---|---|---|---|
| Yoon 2016, Korea [26] | RCT | Control (n = 26) Belly (n = 26) Junction (28) | 1 wk after each session (total of 4 evaluations) | MAS (+) MTS (+) | NM |
| Taheri 2017, Iran [39] | RCT | ESWT (n = 13) Control (n = 12) | 1 wk, 3 wks, 12 wks | MAS (+); VAS (+); PROM (+) 3-m walk duration (+); LEFS (+) Clonus score (−) | NM |
| Wu 2018, Taiwan [25] | RCT | fESWT (n = 15) rESWT (n = 16) | 1 wk, 4 wks, 8 wks | MAS (+); Tardieu Scale (+) Ankle PROM (+) Dynamic foot contact area (+) 10-m walk test (−) | No adverse effect |
| Lee 2018, Korea [40] | RCT | ESWT (n = 9) Control (n = 9) | 30 min, 1 wk, 4 wks | MAS (+); PROM (−) FMA (+) US measures (+) | NM |
| Radinmehr 2019, Iran [41] | RCT | US (n = 16) rESWT (n = 16) | Immediately, 1 h | H-reflex tests (−) MAS (+); PPFT (+) AROM (+); PROM (+) TUG (clinically not significant) | NM |
| Aslan 2021, Turkey [42] | RCT | rESWT (17) Sham (17) Control (17) | Immediately, 4 wks | MAS (+) Tardieu Scale (+) Elastography (+) | Mild pain (2) |
| Author | Type of ESWT | Site of Treatment | Number, Interval of Sessions | Pulses (N) | Frequency (Hz) | Pressure (Bars) | EFD (mJ/mm2) |
|---|---|---|---|---|---|---|---|
| Yoon [26] | Radial | Knee flexors, semitendinosus muscles | 3, once every week | 1500 | 5 | NM | 0.068–0.093 |
| Taheri [39] | NM | GN | 3, once every week | 1500 | 4 | NM | 0.1 |
| Wu [25] | Focused Radial | GN and soleus | 3, once every week | 3000 (1500 per muscle) | 5 | rESWT: 2 | fESWT: 0.10 |
| Lee [40] | NM | GN | 1 | 2000 | 4 | NM | 0.1 |
| Radinmehr [41] | Radial | GN | 1 | 2000 | 5 | 1 | 0.340 |
| Aslan [42] | Radial | Ankle flexor | 4, twice per week | 1500 | 10 | 2 | NM |
| Author, Year, Country | Design | Subjects/Grouping | Follow-up | Parameter | Safety |
|---|---|---|---|---|---|
| Amelio 2010, Italy [43] | Prospective, placebo-controlled study | n = 12 | Immediately after placebo, immediately after ESST, 1 wk, 4 wks, 12 wks | MAS (+) PROM (+) Pedobarometric assessment (+) | NM |
| Vidal 2011, Spain [44] | Placebo-controlled clinical trial | n = 15 | 1 mo, 2 mos, 3 mos | MAS (+) ROM (+) | NM |
| Gonkova 2013, Italy [45] | Observational study | n = 25 | 2 wks, 4 wks | MAS (+), PROM (+) Baropodometric measurements (+) | NM |
| Wang 2016, China [46] | Case-control study | rESWT (n = 34) Control (n = 32) | 1 mo, 3 mos | MAS (+) PROM (+) GMFM-88 (−) | No adverse effect |
| Lin 2018, China [47] | RCT | rESWT (n = 43) Control (n = 39) | 2 wks, 1 mo | GMFM (+), MAS (+) Plantar area and pressure (+) | NM |
| Park 2018, Korea [48] | RCT (a pilot study) | 1 ESWT (n = 6) 3 ESWT (n = 6) | Immediately after the first and third ESWT, 4 wks | MAS (+) PROM (+) Sonoelastography (+) | No adverse effect |
| Vidal 2020, Germany [49] | RCT, cross-over study * | BTX-A (n = 33) rESWT (n = 35) | 3 wks, 2 mos, 3 mos | Tardieu scale, with goniometer (+) | NM |
| Author | Type of ESWT | Site of Treatment | Number, Interval of Sessions | Pulses (N) | Frequency (Hz) | Pressure (Bars) | EFD (mJ/mm2) |
|---|---|---|---|---|---|---|---|
| Amelio [43] | NM | GN and soleus | 1, one placebo session, followed 6 wks later by one active session | 1500 per muscle | NM | NM | 0.030 |
| Vidal [44] | Radial | Biceps brachii, wrist flexors, hip adductors, GN, soleus, and hamstrings | 3, once every week | 2000 per muscle | 8 | 2 | 0.10 |
| Gonkova [45] | Radial | GN and soleus muscle | 1, one placebo session, 1 active session 4 wks later | 1500 per muscle | 5 | 1.5 | NM |
| Wang [46] | Radial | plantar flexor, GN | 12, one ESWT session per week for 3 months, | 1500 permuscle | 8 | 0.6 | 0.03 |
| Lin [47] | Radial | Hamstring | 4, once a week | 2000 | 10 | 2 | NM |
| Park [48] | NM | GN | 1 or 3 sessions, once a week | 1500 | 4 | NM | 0.030 |
| Vidal [49] | Radial | GN and soleus muscle | 3, one session per week | 2000 | 8 | 2.2–2.4 | 0.10–0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, E.; Lew, H.L.; Özçakar, L.; Wu, C.-H. Recent Advances in the Treatment of Spasticity: Extracorporeal Shock Wave Therapy. J. Clin. Med. 2021, 10, 4723. https://doi.org/10.3390/jcm10204723
Yang E, Lew HL, Özçakar L, Wu C-H. Recent Advances in the Treatment of Spasticity: Extracorporeal Shock Wave Therapy. Journal of Clinical Medicine. 2021; 10(20):4723. https://doi.org/10.3390/jcm10204723
Chicago/Turabian StyleYang, En, Henry L. Lew, Levent Özçakar, and Chueh-Hung Wu. 2021. "Recent Advances in the Treatment of Spasticity: Extracorporeal Shock Wave Therapy" Journal of Clinical Medicine 10, no. 20: 4723. https://doi.org/10.3390/jcm10204723
APA StyleYang, E., Lew, H. L., Özçakar, L., & Wu, C.-H. (2021). Recent Advances in the Treatment of Spasticity: Extracorporeal Shock Wave Therapy. Journal of Clinical Medicine, 10(20), 4723. https://doi.org/10.3390/jcm10204723







