Safety and Efficacy of Four Different Diagnostic Catheter Curves Dedicated to One-Catheter Technique of Transradial Coronaro-Angiography—Prospective, Randomized Pilot Study. TRACT 1: Trans RAdial CoronaryAngiography Trial 1
Abstract
:1. Introduction
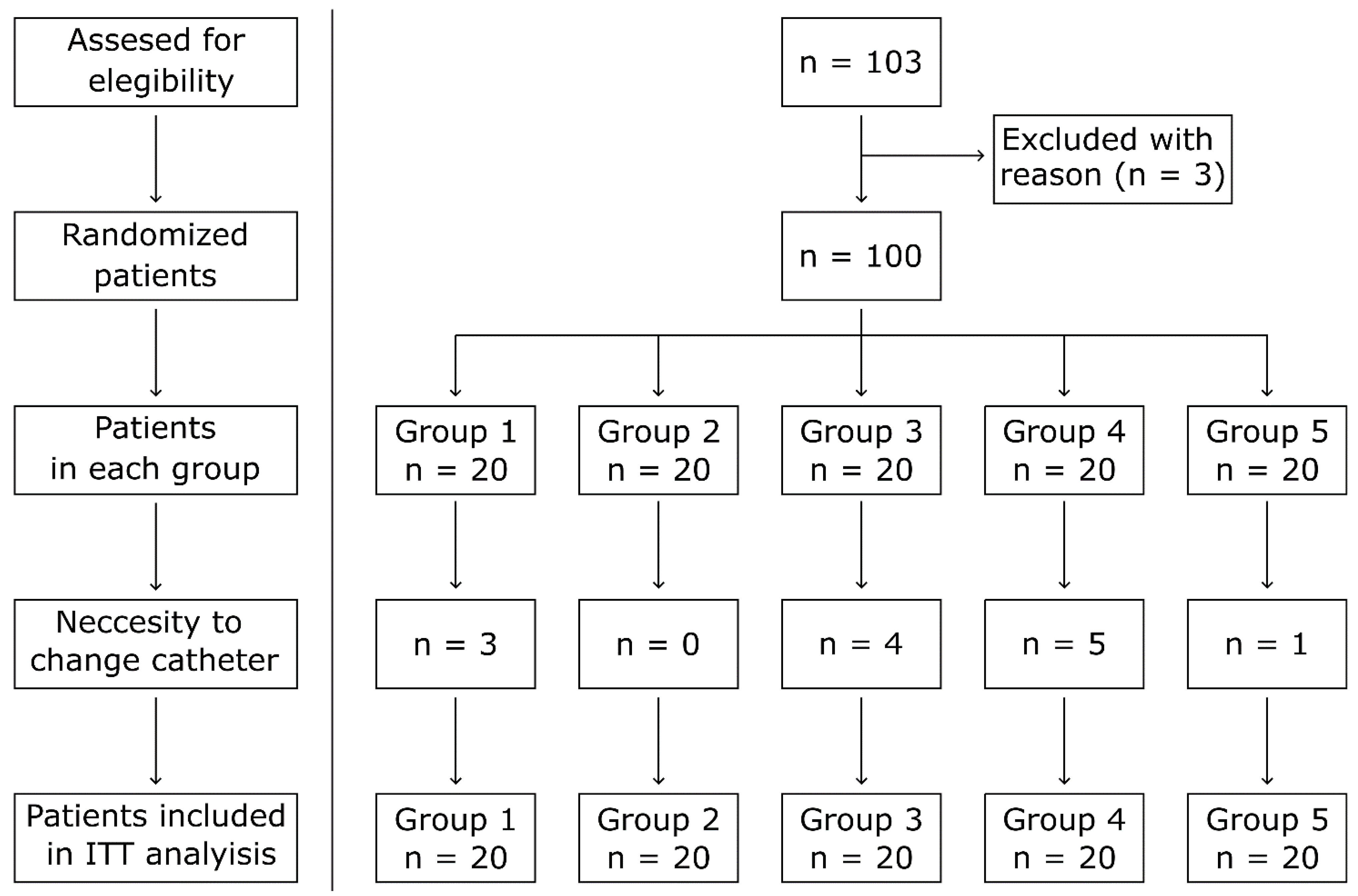
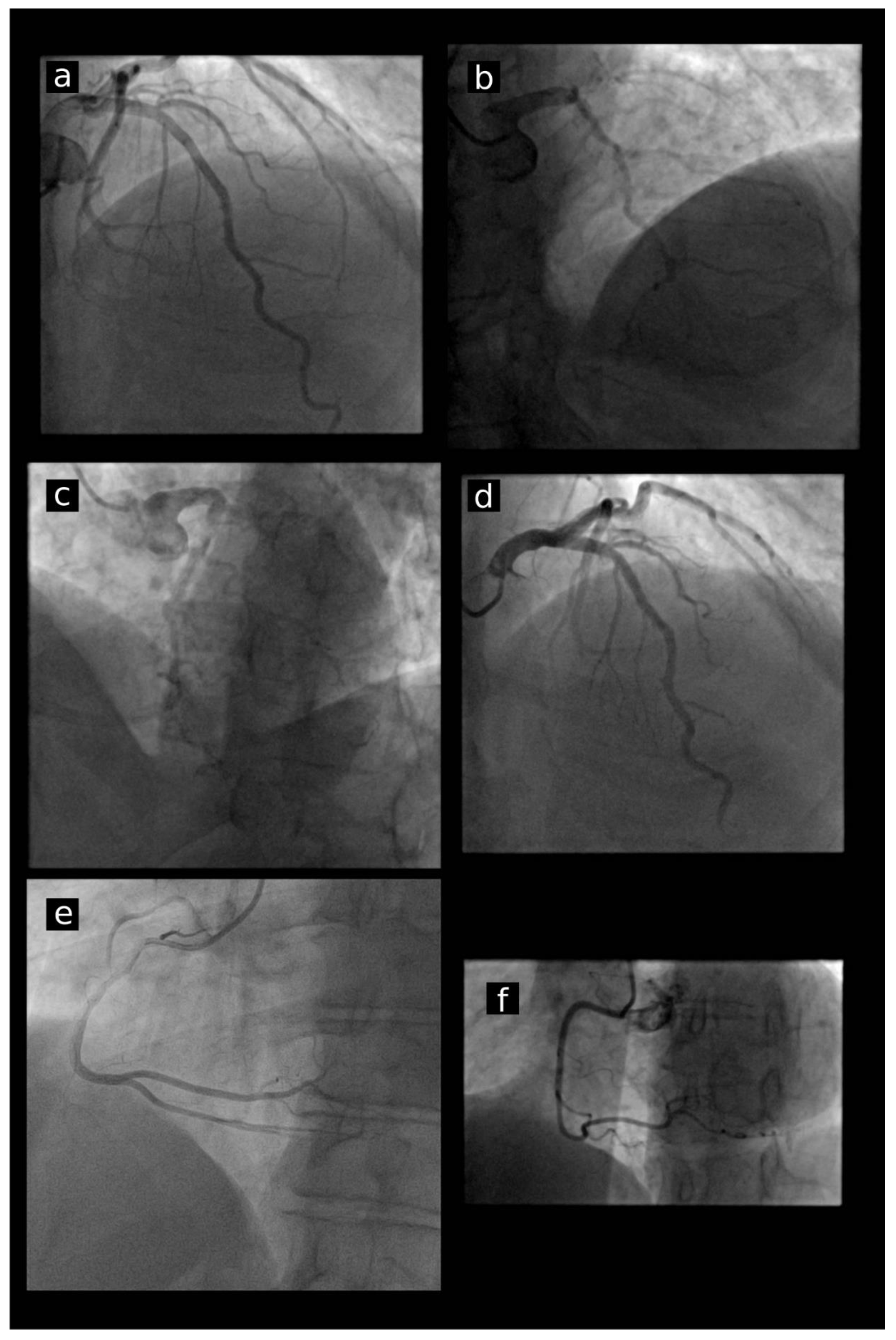
2. Materials and Methods
3. Results
3.1. Baseline Characteristics
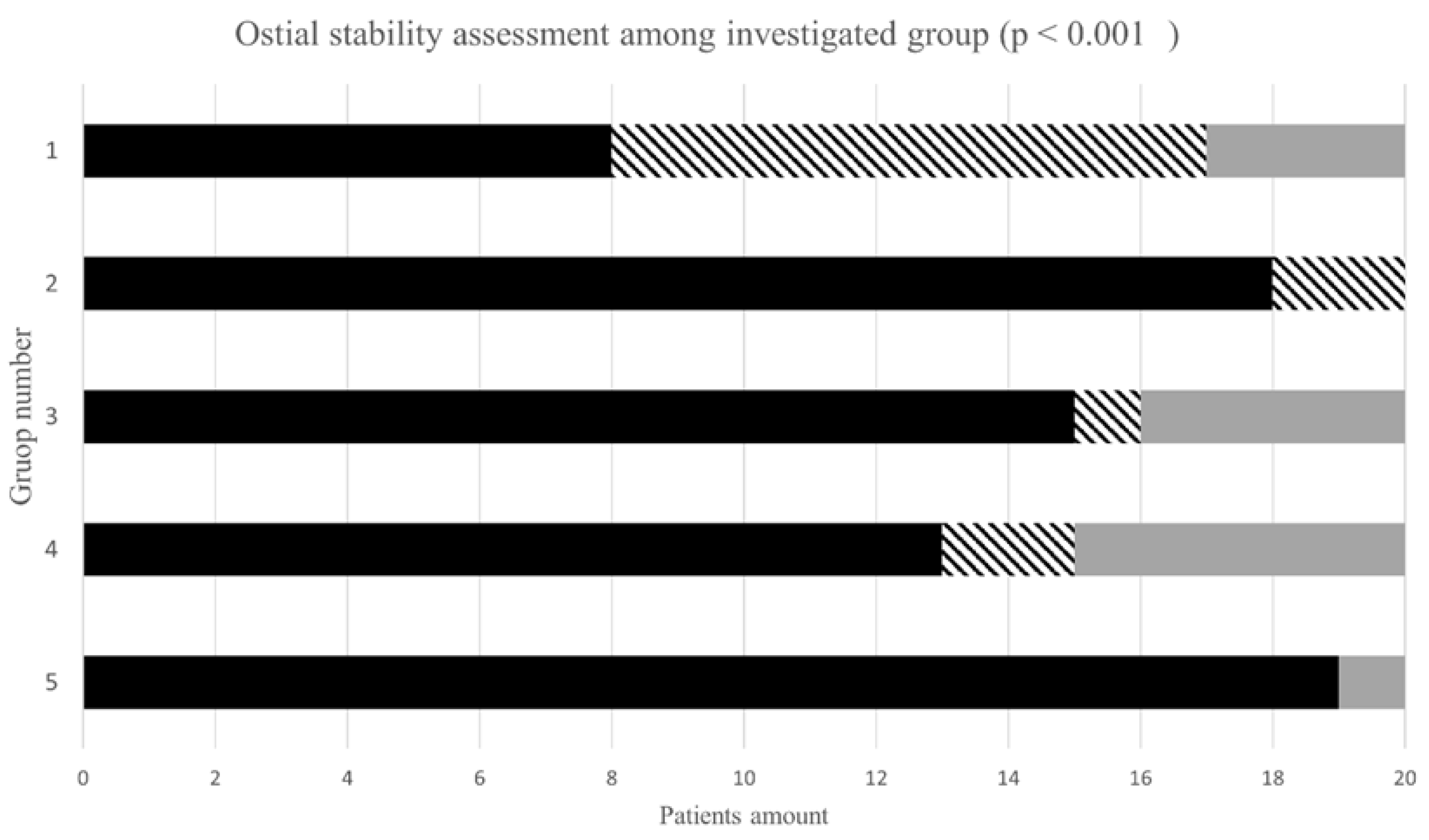
3.2. Ostial Stability and Engagement in Investigated Groups
3.3. Procedural Characteristic
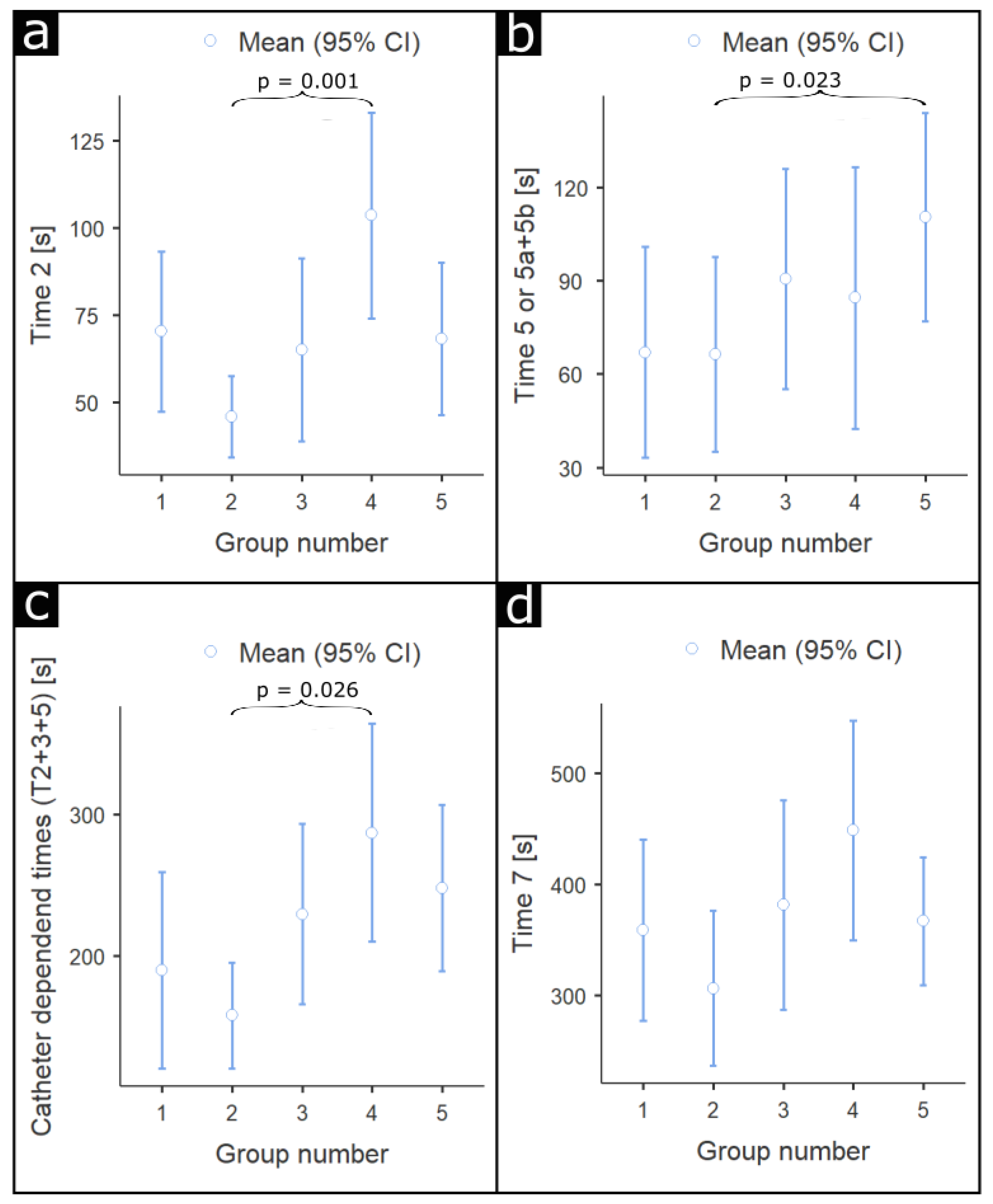
3.4. Duration of Each Procedural Step
3.5. Contrast Volume and Radiation Dose
3.6. Periprocedural Complications
3.7. Treatment Pathway after Diagnostic Catheterization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Dworeck, C.; Redfors, B.; Völz, S.; Haraldsson, I.; Angerås, O.; Råmunddal, T.; Ioanes, D.; Myredal, A.; Odenstedt, J.; Hirlekar, G.; et al. Radial artery access is associated with lower mortality in patients undergoing primary PCI: A report from the SWEDEHEART registry. Eur. Heart J. Acute. Cardiovasc. Care 2020, 9, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Campeau, L. Percutaneous radial artery approach for coronary angiography. Cathet. Cardiovasc. Diagn. 1989, 16, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Kiemeneij, F.; Laarman, G.J. Percutaneous transradial artery approach for coronary Palmaz-Schatz stent implantation. Am. Heart J. 1994, 128, 167–174. [Google Scholar] [CrossRef]
- Mamas, M.A.; Anderson, S.G.; Car, M.; Ratib, K.; Buchan, I.; Sirker, A.; Fraser, D.G.; Hildick-Smith, D.; de Belder, M.; Ludman, F.P. Baseline bleeding risk and arterial access site practice in relation to procedural outcomes following percutaneous coronary intervention. J. Am. Coll. Cardiol. 2014, 64, 1554–1564. [Google Scholar] [CrossRef] [PubMed]
- Mamas, M.A.; Anderson, S.G.; Ratib, K.; Routledge, H.; Neyses, L.; Fraser, D.G.; Buchan, I.; de Belder, M.A.; Ludman, P.; Nolan, J. Arterial access site utilization in cardiogenic shock in the United Kingdom: Is radial access feasible? Am. Heart J. 2014, 167, 900–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, C.J.; El-Shiekh, R.A.; Cohen, D.J.; Blaesing, L.; Burket, M.W.; Basu, A.; Moore, J.A. Effect of transradial access on quality of life and coast of cardiac catheterization: A randomized comparison. Am. Heart J. 1999, 138, 430–436. [Google Scholar] [CrossRef]
- Anderson, S.G.; Ratib, K.; Myint, P.K.; Keavney, B.; Kwok, C.S.; Zaman, A.; Dm, B.B.K.; de Belder, M.A.; Nolan, J.; Mamas, M.A.; et al. Impact of age on access site-related outcomes in 469,983 percutaneous coronary intervention procedures: Insights from the British Cardiovascular Intervention Society. Catheter. Cardiovasc. Interv. 2015, 86, 965–972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldman, D.N.; Swaminathan, R.V.; Kaltenbach, L.A.; Baklanov, D.V.; Kim, L.K.; Wong, S.C.; Minutello, R.M.; Messenger, J.C.; Moussa, I.; Garratt, K.N. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: An updated report from the National Cardiovascular Data Registry ± 2007–2012). Circulation 2013, 127, 2295–2306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartrand, O.F.; Bernat, I. Radial artery occlusion: Still the Achille’s heel of transradial approach or is it? Coron. Artery Dis. 2015, 26, 97–98. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.D.; Hong, J.A.; Lee, B.Y.; Umscheid, C.A.; Bartsch, S.M.; Don, C.W. Systematic Review and Cost–Benefit Analysis of Radial Artery Access for Coronary Angiography and Intervention. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 454–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.-M.; Kim, D.-K.; Kim, O.-I.; Kim, N.-S.; Joo, S.-J.; Lee, J.-W. Novel diagnostic catheter specifically designed for both coronary arteries via the right transradial approach. Int. J. Cardiovasc. Imaging 2005, 22, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Langer, C.; Riehle, J.; Wuttig, H.; Dürrwald, S.; Lange, H.; Samol, A.; Frey, N.; Wiemer, M. Efficacy of a one-catheter concept for transradial coronary angiography. PLoS ONE 2018, 13, e0189899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turan, B.; Erkol, A.; Mutlu, A.; Daşlı, T.; Erden, I. Effectiveness of Left Judkins Catheter as a Single Multipurpose Catheter in Transradial Coronary Angiography From Right Radial Artery: A Randomized Comparison With Conventional Two-Catheter Strategy. J. Interv. Cardiol. 2016, 29, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Chen, O.; Goel, S.; Acholonu, M.; Kulbak, G.; Verma, S.; Travlos, E.; Casazza, R.; Borgen, E.; Malik, B.; Friedman, M.; et al. Comparison of Standard Catheters Versus Radial Artery–Specific Catheter in Patients Who Underwent Coronary Angiography Through Transradial Access. Am. J. Cardiol. 2016, 118, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Xanthopoulou, I.; Stavrou, K.; Davlouros, P.; Tsigkas, G.; Koufou, E.-E.; Almpanis, G.; Koutouzis, M.; Tsiafoutis, I.; Perperis, A.; Moulias, A.; et al. Randomised comparison of JUDkins vs. tiGEr catheter in coronary angiography via the right radial artery: The JUDGE study. EuroIntervention 2018, 13, 1950–1958. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, E.; Brousseau-Provencher, C.; Montminy, S.; Plourde, G.; MacHaalany, J.; Bataille, Y.; Molin, P.; Déry, J.-P.; Barbeau, G.; Roy, L.; et al. Risk Score, Causes, and Clinical Impact of Failure of Transradial Approach for Percutaneous Coronary Interventions. JACC Cardiovasc. Interv. 2013, 6, 1129–1137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De-an, I.A.; Zhou, Y.; Shi, D.; Liu, Y.; Wang, J.; Liu, X.; Wang, Z.; Yang, S.; Ge, H.; Hu, B. Incidence and predictors of radial artery spasm during transradial coronary angi-ography and intervention. Chin. Med. J. 2010, 123, 843–847. [Google Scholar]
- Sanmartin, M.; Esparza, J.; Moxica, J.; Baz, J.A.; Iñiguez-Romo, A. Safety and efficacy of a multipurpose coronary angiography strategy using the transradial technique. J. Invasive Cardiol. 2005, 17, 594–597. [Google Scholar] [PubMed]
- Trilla, M.; Freixa, X.; Regueiro, A.; Fernández-Rodriguez, D.; Brugaletta, S.; Martin-Yuste, V.; Jiménez, M.; Betriu, A.; Sabaté, M.; Masotti, M. Impact of Aging on Radial Spasm during Coronary Catheterization. J. Invasive Cardiol. 2015, 27, E303–E307. [Google Scholar] [PubMed]
| Characteristics | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | p Value |
|---|---|---|---|---|---|---|
| Age (years) | 65.1 ± 7.8 | 63.1 ± 11.3 | 66 ± 10.1 | 68 ± 8.6 | 69.3 ± 9 | 0.28 |
| Weight (kg) | 84.6 ± 16.2 | 78.3 ± 10.1 | 88.5 ± 17.4 | 82.6 ± 20.9 | 77.6 ± 14.3 | 0.22 |
| Height (cm) | 173 ± 9.3 | 170 ± 9.2 | 171 ± 9.3 | 166 ± 9.2 | 168 ± 6.6 | 0.08 |
| BMI (kg/m2) | 28.3 ± 4.5 | 27.1 ± 3.1 | 30 ± 4.7 | 29.8 ± 7 | 27.4 ± 4.6 | 0.39 |
| Men (n (%)) | 15 (75) | 17 (85) | 16 (80) | 12 (60) | 13 (65) | 0.36 |
| Diameter of aorta (mm) | 35.8 ± 4.5 | 33.9 ± 4.0 | 36.1 ± 4.3 | 35.9 ± 6.4 | 35.8 ± 4.8 | 0.48 |
| Left ventricle diameter (mm) | 55.6 ± 9.1 | 50.5 ± 7.1 | 53.8 ± 8.2 | 56.7 ± 8.5 | 51.0 ± 7.9 | 0.07 |
| EF (%) | 43.6 ± 13.0 | 52.8 ± 12.7 | 46.3 ± 12.9 | 42.5 ± 12.0 | 51.8 ± 11.2 | 0.012 a |
| Diabetes (n (%)) | 4 (20) | 3 (15) | 5 (25) | 4 (20) | 6 (30) | 0.82 |
| Hypertension (n (%)) | 14 (70) | 13 (65) | 18 (90) | 15 (75) | 17 (85) | 0.30 |
| PAD (n (%)) | 1 (5) | 2 (10) | 1 (5) | 2 (10) | 3 (15) | 0.78 |
| CKD (n (%)) | 2 (10) | 1 (5) | 3 (15) | 3 (15) | 5 (25) | 0.45 |
| Group | Suboptimal Ostial Stability during Cannulation of LCA and RCA (n) | Necessity of Catheter Change during Cannulation of LCA and RCA (n) |
|---|---|---|
| 1 | LCA: 8 RCA: 1 | LCA: 3 RCA: 0 |
| 2 | LCA: 1 RCA: 1 | LCA: 0 RCA: 0 |
| 3 | LCA: 1 RCA: 1 | LCA: 2 RCA: 2 |
| 4 | LCA: 2 RCA: 1 | LCA: 2 RCA: 3 |
| 5 | LCA: 0 RCA: 0 | LCA: 0 RCA: 1 |
| Amount of Contrast and Radiation | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | p Value |
|---|---|---|---|---|---|---|
| RCA contrast volume (mL) | 15.9 11.3 | 18.1 ± 9.2 | 23.1 ± 18.6 | 26.7 ± 21.3 | 19 ± 10.4 | 0.19 |
| RCA radiation dose (mGy) | 38.1 ± 25.1 | 29.4 ± 23.7 | 47 ± 27.1 | 41 ± 31 | 40.1 ± 36.6 | 0.23 |
| LCA contrast volume (mL) | 36.8 ± 11.3 | 38 ± 18.2 | 39.2 ± 17.5 | 45 ± 20.8 | 38.2 ± 14.4 | 0.71 |
| Total radiation dose (mGy) | 115 ± 71.4 | 67 ± 45.2 | 108 ± 58.5 | 86.9 ± 78.5 | 80.5 ± 40.7 | 0.045 a |
| Total contrast volume (mL) | 60.4 ± 32.1 | 57.4 ± 22.4 | 64.8 ± 31.4 | 71.8 ± 31.6 | 63.3 ± 30.6 | 0.39 |
| Treatment Pathway | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | p Value |
|---|---|---|---|---|---|---|
| OMT ± n ± % | 13 ± 65 | 6 ± 30 | 10 ± 50 | 13 ± 65 | 10 ± 50 | 0.16 |
| PCI ± n ± % | 4 ± 20 | 11 ± 55 | 9 ± 45 | 4 ± 20 | 9 ± 45 | 0.065 |
| CABG ± n ± % | 3 ± 15 | 3 ± 15 | 1 ± 5 | 3 ± 15 | 1 ± 5 | 0.71 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chyrchel, M.; Bartuś, S.; Dziewierz, A.; Legutko, J.; Kleczyński, P.; Januszek, R.; Gallina, T.; Chyrchel, B.; Surdacki, A.; Rzeszutko, Ł. Safety and Efficacy of Four Different Diagnostic Catheter Curves Dedicated to One-Catheter Technique of Transradial Coronaro-Angiography—Prospective, Randomized Pilot Study. TRACT 1: Trans RAdial CoronaryAngiography Trial 1. J. Clin. Med. 2021, 10, 4722. https://doi.org/10.3390/jcm10204722
Chyrchel M, Bartuś S, Dziewierz A, Legutko J, Kleczyński P, Januszek R, Gallina T, Chyrchel B, Surdacki A, Rzeszutko Ł. Safety and Efficacy of Four Different Diagnostic Catheter Curves Dedicated to One-Catheter Technique of Transradial Coronaro-Angiography—Prospective, Randomized Pilot Study. TRACT 1: Trans RAdial CoronaryAngiography Trial 1. Journal of Clinical Medicine. 2021; 10(20):4722. https://doi.org/10.3390/jcm10204722
Chicago/Turabian StyleChyrchel, Michał, Stanisław Bartuś, Artur Dziewierz, Jacek Legutko, Paweł Kleczyński, Rafał Januszek, Tomasz Gallina, Bernadeta Chyrchel, Andrzej Surdacki, and Łukasz Rzeszutko. 2021. "Safety and Efficacy of Four Different Diagnostic Catheter Curves Dedicated to One-Catheter Technique of Transradial Coronaro-Angiography—Prospective, Randomized Pilot Study. TRACT 1: Trans RAdial CoronaryAngiography Trial 1" Journal of Clinical Medicine 10, no. 20: 4722. https://doi.org/10.3390/jcm10204722
APA StyleChyrchel, M., Bartuś, S., Dziewierz, A., Legutko, J., Kleczyński, P., Januszek, R., Gallina, T., Chyrchel, B., Surdacki, A., & Rzeszutko, Ł. (2021). Safety and Efficacy of Four Different Diagnostic Catheter Curves Dedicated to One-Catheter Technique of Transradial Coronaro-Angiography—Prospective, Randomized Pilot Study. TRACT 1: Trans RAdial CoronaryAngiography Trial 1. Journal of Clinical Medicine, 10(20), 4722. https://doi.org/10.3390/jcm10204722








