The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Swiss HIV Cohort Study and Inclusion Criteria
2.2. Outcomes
2.3. Exposure
2.4. Statistical Analyses
2.5. Sensitivity Analyses
3. Results
3.1. Study Population
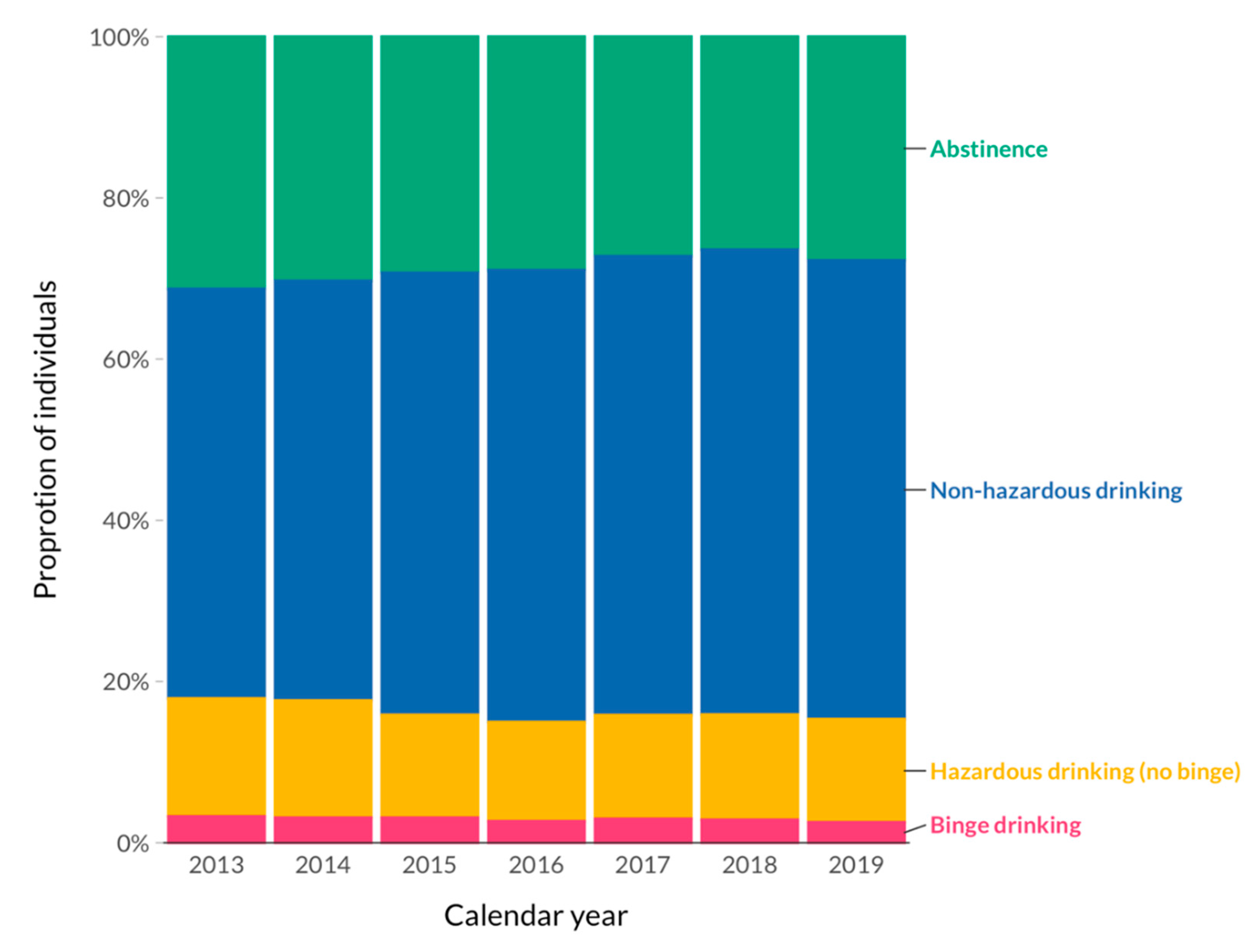
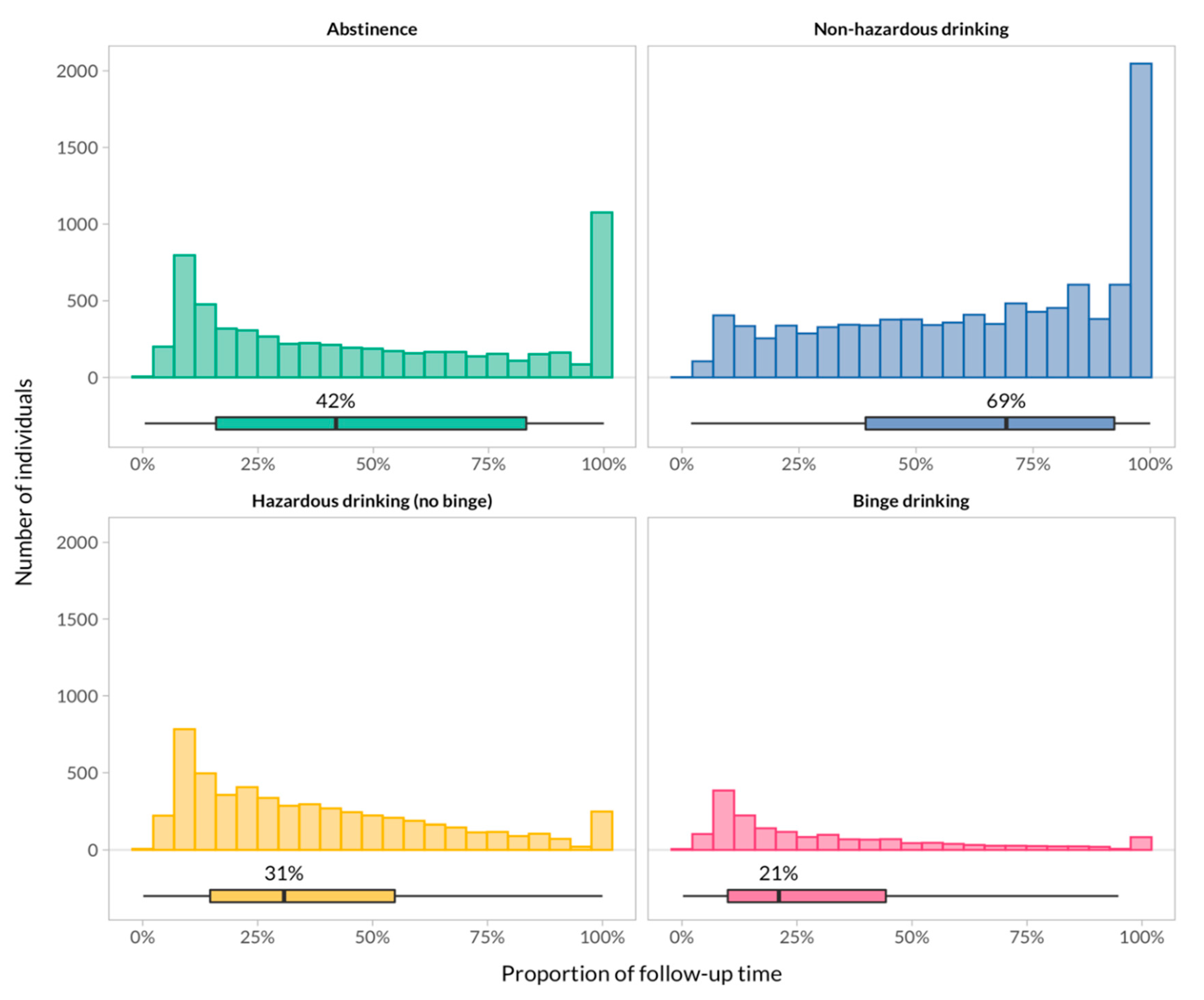
3.2. Alcohol Drinking Patterns
3.3. All-Cause and Liver-Related Deaths
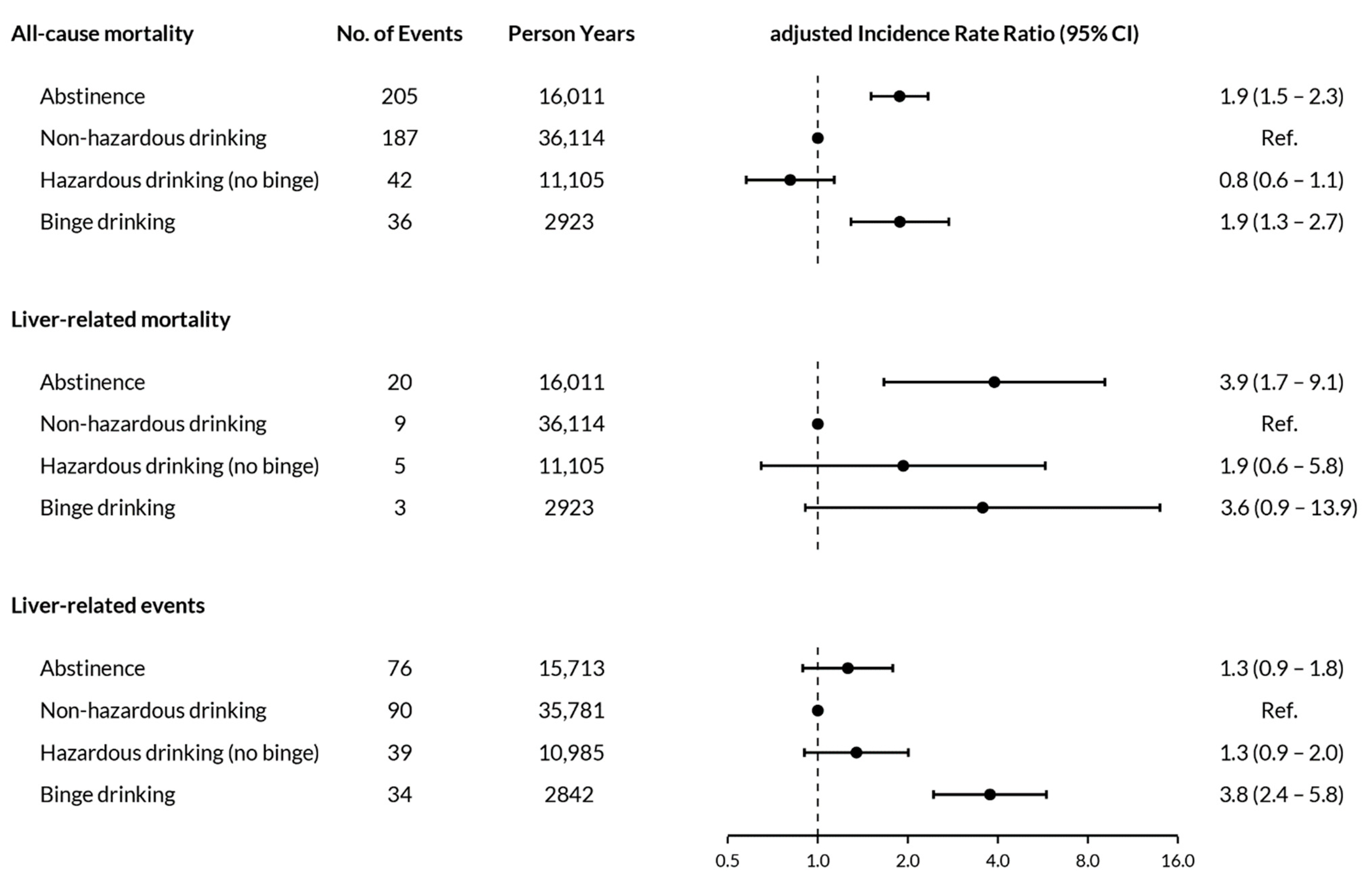
3.4. Liver-Related Events
3.5. Sensitivity Analyses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health. 2018. Available online: https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1 (accessed on 4 November 2020).
- Marmet, S.; Rehm, J.; Gmel, G.; Frick, H.; Gmel, G. Alcohol-attributable mortality in Switzerland in 2011--age-specific causes of death and impact of heavy versus non-heavy drinking. Swiss Med. Wkly. 2014, 144, w13947. [Google Scholar] [CrossRef] [PubMed]
- Sepanlou, S.G.; Safiri, S.; Bisignano, C.; Ikuta, K.S.; Merat, S.; Saberifiroozi, M.; Poustchi, H.; Tsoi, D.; Colombara, D.V.; Abdoli, A.; et al. GBD 2017 Cirrhosis Collaborators The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 245–266. [Google Scholar] [CrossRef]
- Duko, B.; Ayalew, M.; Ayano, G. The prevalence of alcohol use disorders among people living with HIV/AIDS: A systematic review and meta-analysis. Subst. Abuse Treat. Prev. Policy 2019, 14, 52. [Google Scholar] [CrossRef]
- Hasse, B.; Ledergerber, B.; Hirschel, B.; Vernazza, P.; Glass, T.R.; Jeannin, A.; Evison, J.-M.; Elzi, L.; Cavassini, M.; Bernasconi, E.; et al. Frequency and determinants of unprotected sex among HIV-infected persons: The Swiss HIV cohort study. Clin. Infect. Dis. 2010, 51, 1314–1322. [Google Scholar] [CrossRef]
- Chander, G.; Lau, B.; Moore, R.D. Hazardous alcohol use: A risk factor for non-adherence and lack of suppression in HIV infection. J. Acquir. Immune Defic. Syndr. 2006, 43, 411–417. [Google Scholar] [CrossRef]
- Wandeler, G.; Kraus, D.; Fehr, J.; Conen, A.; Calmy, A.; Orasch, C.; Battegay, M.; Schmid, P.; Bernasconi, E.; Furrer, H.; et al. The J-Curve in HIV: Low and Moderate Alcohol Intake Predicts Mortality but Not the Occurrence of Major Cardiovascular Events. J. Acquir. Immune Defic. Syndr. 2016, 71, 302–309. [Google Scholar] [CrossRef]
- Justice, A.C.; McGinnis, K.A.; Tate, J.P.; Braithwaite, R.S.; Bryant, K.J.; Cook, R.L.; Edelman, E.J.; Fiellin, L.E.; Freiberg, M.S.; Gordon, A.J.; et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016, 161, 95–103. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch. Intern. Med. 2006, 166, 2437–2445. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, M.M.; Rehm, J.; Klipstein-Grobusch, K.; Boeing, H.; Schütze, M.; Drogan, D.; Overvad, K.; Tjønneland, A.; Halkjær, J.; Fagherazzi, G.; et al. The association of pattern of lifetime alcohol use and cause of death in the European prospective investigation into cancer and nutrition (EPIC) study. Int. J. Epidemiol. 2013, 42, 1772–1790. [Google Scholar] [CrossRef]
- Xi, B.; Veeranki, S.P.; Zhao, M.; Ma, C.; Yan, Y.; Mi, J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Åberg, F.; Helenius-Hietala, J.; Puukka, P.; Jula, A. Binge drinking and the risk of liver events: A population-based cohort study. Liver Int. 2017, 37, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Conen, A.; Wang, Q.; Glass, T.R.; Fux, C.A.; Thurnheer, M.C.; Orasch, C.; Calmy, A.; Bernasconi, E.; Vernazza, P.; Weber, R.; et al. Association of alcohol consumption and HIV surrogate markers in participants of the swiss HIV cohort study. J. Acquir. Immune Defic. Syndr. 2013, 64, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Carrieri, M.P.; Protopopescu, C.; Raffi, F.; March, L.; Reboud, P.; Spire, B.; Leport, C.; ANRS CO8 APROCO-COPILOTE Study Group. Low alcohol consumption as a predictor of higher CD4+ cell count in HIV-treated patients: A french paradox or a proxy of healthy behaviors? The ANRS APROCO-COPILOTE CO-08 cohort. J. Acquir. Immune Defic. Syndr. 2014, 65, e148–e150. [Google Scholar] [CrossRef] [PubMed]
- Nouaman, M.N.; Vinikoor, M.; Seydi, M.; Ekouevi, D.K.; Coffie, P.A.; Mulenga, L.; Tanon, A.; Egger, M.; Dabis, F.; Jaquet, A.; et al. High prevalence of binge drinking among people living with HIV in four African countries. J. Int. AIDS Soc. 2018, 21, e25202. [Google Scholar] [CrossRef] [PubMed]
- Schoeni-Affolter, F.; Ledergerber, B.; Rickenbach, M.; Rudin, C.; Günthard, H.F.; Telenti, A.; Furrer, H.; Yerly, S.; Francioli, P.; Swiss HIV Cohort Study. Cohort profile: The Swiss HIV Cohort study. Int. J. Epidemiol. 2010, 39, 1179–1189. [Google Scholar] [CrossRef]
- Wai, C.-T.; Greenson, J.K.; Fontana, R.J.; Kalbfleisch, J.D.; Marrero, J.A.; Conjeevaram, H.S.; Lok, A.S.-F. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003, 38, 518–526. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Fuster, D.; Tsui, J.I.; Cheng, D.M.; Quinn, E.K.; Bridden, C.; Nunes, D.; Libman, H.; Saitz, R.; Samet, J.H. Impact of lifetime alcohol use on liver fibrosis in a population of HIV-infected patients with and without hepatitis C coinfection. Alcohol. Clin. Exp. Res. 2013, 37, 1527–1535. [Google Scholar] [CrossRef]
- Kim, H.N.; Crane, H.M.; Rodriguez, C.V.; Van Rompaey, S.; Mayer, K.H.; Christopoulos, K.; Napravnik, S.; Chander, G.; Hutton, H.; McCaul, M.E.; et al. The Role of Current and Historical Alcohol Use in Hepatic Fibrosis among HIV-Infected Individuals. AIDS Behav. 2017, 21, 1878–1884. [Google Scholar] [CrossRef]
- Shanyinde, M.; Girardi, E.; Puoti, M.; De Luca, A.; Sighinolfi, L.; Caterina, U.F.; Caramello, P.; Lampe, F.C.; D’Arminio Monforte, A.; Cozzi-Lepri, A.; et al. Is physician assessment of alcohol consumption useful in predicting risk of severe liver disease among people with HIV and HIV/HCV co-infection? BMC Public Health 2019, 19, 1291. [Google Scholar] [CrossRef]
- Stockwell, T.; Zhao, J.; Panwar, S.; Roemer, A.; Naimi, T.; Chikritzhs, T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J. Stud. Alcohol Drugs 2016, 77, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Aberra, H.; Desalegn, H.; Berhe, N.; Mekasha, B.; Medhin, G.; Gundersen, S.G.; Johannessen, A. The WHO guidelines for chronic hepatitis B fail to detect half of the patients in need of treatment in Ethiopia. J. Hepatol. 2019, 70, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
| Abstinence | Non-Hazardous Drinking | Hazardous Drinking(No Binge) | Binge Drinking | |
|---|---|---|---|---|
| n | 2718 | 6861 | 1814 | 456 |
| Female (%) | 1220 (44.9) | 1697 (24.7) | 287 (15.8) | 60 (13.2) |
| Median age, years (IQR) | 47 (39–53) | 47 (39–53) | 45 (36–52) | 46 (36–52) |
| Caucasian (%) | 1756 (64.6) | 5436 (79.2) | 1529 (84.3) | 376 (82.5) |
| HIV transmission (%) | ||||
| Heterosexual | 1333 (49.0) | 2455 (35.8) | 502 (27.7) | 145 (31.8) |
| PWID | 516 (19.0) | 559 (8.1) | 197 (10.9) | 75 (16.4) |
| MSM | 692 (25.5) | 3483 (50.8) | 1037 (57.2) | 213 (46.7) |
| Other | 177 (6.5) | 364 (5.3) | 78 (4.3) | 23 (5.0) |
| Education (%) | ||||
| No education | 332 (12.2) | 333 (4.9) | 85 (4.7) | 35 (7.7) |
| Basic education | 1658 (61.0) | 3838 (55.9) | 976 (53.8) | 266 (58.3) |
| Higher education | 604 (22.2) | 2528 (36.8) | 722 (39.8) | 145 (31.8) |
| Missing data | 124 (4.6) | 162 (2.4) | 31 (1.7) | 10 (2.2) |
| Median nadir CD4, cells/µL (IQR) | 186 (79–294) | 222 (110–338) | 241 (126–380) | 226 (117–373) |
| History of AIDS defining disease (%) | 744 (27.4) | 1430 (20.8) | 305 (16.8) | 96 (21.1) |
| HBV coinfection (%) | 165 (6.1) | 327 (4.8) | 66 (3.6) | 15 (3.3) |
| HCV coinfection (%) | 372 (13.7) | 525 (7.7) | 158 (8.7) | 61 (13.4) |
| Smoker (%) | 1203 (44.3) | 2975 (43.4) | 1097 (60.5) | 336 (73.7) |
| Unemployed (%) | 1311 (48.2) | 1757 (25.6) | 450 (24.8) | 201 (44.1) |
| Lives with partner (%) | 1139 (41.9) | 3351 (48.8) | 782 (43.1) | 158 (34.6) |
| Any depressive episode (%) | 1186 (43.6) | 2263 (33.0) | 649 (35.8) | 216 (47.4) |
| BMI category (%) | ||||
| Normal | 1377 (50.7) | 3840 (56.0) | 1075 (59.3) | 260 (57.0) |
| Underweight | 205 (7.5) | 274 (4.0) | 77 (4.2) | 27 (5.9) |
| Overweight/obese | 1046 (38.5) | 2624 (38.2) | 633 (34.9) | 158 (34.6) |
| Missing data | 90 (3.3) | 123 (1.8) | 29 (1.6) | 11 (2.4) |
| Median follow-up, years (IQR) | 6.8 (3.8–7.0) | 6.8 (4.6–7.1) | 6.7 (3.3–7.0) | 6.2 (3.1–7.0) |
| All-Cause Deaths | Liver-Related Deaths | Liver-Related Events | ||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Person-Years | n | Rate per 1000 Person-Years (95% CI) | n | Rate per 1000 Person-Years (95% CI) | Person-Years | n | Rate per 1000 Person-Years (95% CI) |
| Overall | 66,153 | 470 | 7.1 (6.5–7.8) | 37 | 0.6 (0.4–0.8) | 65,321 | 239 | 3.7 (3.2–4.2) |
| Calendar year 1 | ||||||||
| 2013 | 8482 | 65 | 7.7 (6.0– 9.8) | 7 | 0.8 (0.4–1.7) | 8459 | 70 | 8.3 (6.5–10.5) |
| 2014 | 9252 | 60 | 6.5 (5.0–8.4) | 8 | 0.9 (0.4–1.7) | 9176 | 44 | 4.8 (3.6–6.4) |
| 2015 | 9526 | 96 | 10.1 (8.3–12.3) | 5 | 0.5 (0.2–1.3) | 9417 | 37 | 3.9 (2.8–5.4) |
| 2016 | 9647 | 69 | 7.2 (5.7–9.1) | 6 | 0.6 (0.3–1.4) | 9510 | 30 | 3.2 (2.2–4.5) |
| 2017 | 9603 | 83 | 8.6 (7.0–10.7) | 6 | 0.6 (0.3–1.4) | 9451 | 28 | 3.0 (2.0–4.3) |
| 2018 | 9660 | 66 | 6.8 (5.4–8.7) | 4 | 0.4 (0.2–1.1) | 9496 | 23 | 2.4 (1.6–3.6) |
| 2019 | 9352 | 30 | 3.2 (2.2–4.6) | 1 | 0.1 (0.0–0.8) | 9194 | 7 | 0.8 (0.4–1.6) |
| 2020 | 592 | 1 | 1.7 (0.2–12.0) | 0 | 0 | 578 | 0 | 0 |
| Transmission risk group | ||||||||
| Heterosexual | 25,289 | 145 | 5.7 (4.9–6.7) | 11 | 0.4 (0.2–0.8) | 25,089 | 63 | 2.5 (4.9–6.7) |
| PWID | 7466 | 138 | 18.5 (15.6–21.9) | 21 | 2.8 (1.8–4.3) | 7098 | 100 | 14.1 (15.6–21.9) |
| MSM | 30,072 | 165 | 5.5 (4.7–6.4) | 5 | 0.2 (0.1–0.4) | 29,839 | 68 | 2.3 (4.7–6.4) |
| Other | 3326 | 22 | 6.6 (4.4–10.0) | 0 | 0 | 3294 | 8 | 2.4 (4.4–10.0) |
| Alcohol drinking pattern | ||||||||
| Abstinence | 16,011 | 205 | 12.8 (11.2–14.7) | 20 | 1.2 (0.8–1.9) | 15,713 | 76 | 4.8 (3.9–6.1) |
| Non-hazardous drinking | 36,114 | 187 | 5.2 (4.5–6.0) | 9 | 0.2 (0.1–0.5) | 35,781 | 90 | 2.5 (2.0–3.1) |
| Hazardous drinking (no binge) | 11,105 | 42 | 3.8 (2.8–5.1) | 5 | 0.5 (0.2–1.1) | 10,985 | 39 | 3.6 (2.6–4.9) |
| Binge drinking | 2923 | 36 | 12.3 (8.9–17.0) | 3 | 1.0 (0.3–3.2) | 2842 | 34 | 12.0 (8.5–16.8) |
| Liver-Related Event | n |
|---|---|
| Cirrhosis (confirmed AST-to-platelet ratio index (APRI-score) above 2) | 140 |
| Cirrhosis (based on liver-biopsy) | 28 |
| Diagnosis of portal hypertension | 20 |
| Hepatocellular carcinoma (HCC) | 20 |
| Bleeding from gastric or esophageal varices | 10 |
| Hepatic encephalopathy (stage III or IV) | 9 |
| Hepatorenal syndrome | 4 |
| Liver transplantation | 3 |
| Spontaneous bacterial peritonitis (with cirrhosis) | 3 |
| Ascites, clinically and confirmed by imaging | 2 |
| Total | 239 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Surial, B.; Bertholet, N.; Daeppen, J.-B.; Darling, K.E.A.; Calmy, A.; Günthard, H.F.; Stöckle, M.; Bernasconi, E.; Schmid, P.; Rauch, A.; et al. The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study. J. Clin. Med. 2021, 10, 295. https://doi.org/10.3390/jcm10020295
Surial B, Bertholet N, Daeppen J-B, Darling KEA, Calmy A, Günthard HF, Stöckle M, Bernasconi E, Schmid P, Rauch A, et al. The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study. Journal of Clinical Medicine. 2021; 10(2):295. https://doi.org/10.3390/jcm10020295
Chicago/Turabian StyleSurial, Bernard, Nicolas Bertholet, Jean-Bernard Daeppen, Katharine E. A. Darling, Alexandra Calmy, Huldrych F. Günthard, Marcel Stöckle, Enos Bernasconi, Patrick Schmid, Andri Rauch, and et al. 2021. "The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study" Journal of Clinical Medicine 10, no. 2: 295. https://doi.org/10.3390/jcm10020295
APA StyleSurial, B., Bertholet, N., Daeppen, J.-B., Darling, K. E. A., Calmy, A., Günthard, H. F., Stöckle, M., Bernasconi, E., Schmid, P., Rauch, A., Furrer, H., Wandeler, G., & The Swiss HIV Cohort Study. (2021). The Impact of Binge Drinking on Mortality and Liver Disease in the Swiss HIV Cohort Study. Journal of Clinical Medicine, 10(2), 295. https://doi.org/10.3390/jcm10020295