Peroral Endoscopic Myotomy in the Management of Zenker’s Diverticulum: A Retrospective Multicenter Study
Abstract
1. Background
2. Materials and Methods
2.1. Z-POEM Procedure
2.2. Study Outcomes
2.3. Statistical Analysis
3. Results
- Mild: two cases of transient and asymptomatic subcutaneous emphysema of the neck
- Moderate: a single case of an extensive subcutaneous and intramuscular emphysema of the neck, chest, and abdomen followed by laryngeal edema requiring prolonged intubation and intensive care unit monitoring. This likely occurred due to erroneous simultaneous CO2 and air insufflation.
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Law, R.; Katzka, D.A.; Baron, T.H. Zenker’s Diverticulum. Clin. Gastroenterol. Hepatol. 2014, 12, 1773–1782. [Google Scholar] [CrossRef] [PubMed]
- Cook, I.J.; Gabb, M.; Panagopoulos, V.; Jamieson, G.G.; Dodds, W.J.; Dent, J.; Shearman, D.J. Pharyngeal (Zenker’s) diverticulum is a disorder of upper esophageal sphincter opening. Gastroenterology 1992, 103, 1229–1235. [Google Scholar] [CrossRef]
- Kothari, T.; Stone, J.; Haber, G. Kothari Haber Scoring System: Zenker’s Diverticulum Myotomy Assessed with the Help of New Scoring System: 30. Am. J. Gastroenterol. 2013, 108, S11–S12. [Google Scholar] [CrossRef]
- Yuan, Y.; Zhao, Y.-F.; Hu, Y.; Chen, L.-Q. Surgical Treatment of Zenker’s Diverticulum. Dig. Surg. 2013, 30, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Ishaq, S.; Hassan, C.; Antonello, A.; Tanner, K.; Bellisario, C.; Battaglia, G.; Anderloni, A.; Correale, L.; Sharma, P.; Baron, T.H.; et al. Flexible endoscopic treatment for Zenker’s diverticulum: A systematic review and meta-analysis. Gastrointest. Endosc. 2016, 83, 1076–1089.e5. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Minami, H.; Kobayashi, Y.; Sato, Y.; Kaga, M.; Suzuki, M.; Satodate, H.; Odaka, N.; Itoh, H.; Kudo, S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010, 42, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.-L.; Chen, W.-F.; Zhang, X.-C.; Cai, M.-Y.; Zhang, Y.-Q.; Hu, J.-W.; He, M.-J.; Yao, L.-Q.; Zhou, P.; Xu, M. Submucosal Tunneling Endoscopic Septum Division: A Novel Technique for Treating Zenker’s Diverticulum. Gastroenterology 2016, 151, 1071–1074. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, O.I.B.; Ichkhanian, Y.; Spadaccini, M.; Vosoughi, K.; Repici, A.; Khashab, M.A. Zenker’s Diverticulum Per-Oral Endoscopic Myotomy Techniques: Changing Paradigms. Gastroenterology 2019, 156, 2134–2135. [Google Scholar] [CrossRef] [PubMed]
- Repici, A.; Spadaccini, M.; Belletrutti, P.J.; Galtieri, P.A.; Fugazza, A.; Anderloni, A.; Carrara, S.; Di Leo, M.; Pellegatta, G.; Cappello, A.; et al. Peroral endoscopic septotomy for short-septum Zenker’s diverticulum. Endoscopy 2020, 52, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Novak, S.; Ujiki, M.; Hernández, Ó.; Desai, P.; Benias, P.; Lee, D.; Chang, K.; Brieau, B.; Barret, M.; et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest. Endosc. 2020, 91, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Maydeo, A.; Patil, G.K.; Dalal, A. Operative technical tricks and 12-month outcomes of diverticular peroral endoscopic myotomy (D-POEM) in patients with symptomatic esophageal diverticula. Endoscopy 2019, 51, 1136–1140. [Google Scholar] [CrossRef] [PubMed]
- Ishaq, S.; Kuwai, T.; Siau, K.; Mulder, C.; Neumann, H. Is Z-POEM for Zenker’s the same as POEM for achalasia? Or we are barking up the wrong tree? Gastrointest. Endosc. 2020, 91, 204–205. [Google Scholar] [CrossRef] [PubMed]
| Symptom | Score |
|---|---|
| Weight loss (over one year) | |
| none | 0 |
| 1–10 lbs (0.45–4.54 kg) | 1 |
| 11–20 lbs (4.99–9.07 kg) | 2 |
| >20 lbs (>9.07 kg) | 3 |
| Dysphagia | |
| none | 0 |
| solids | 1 |
| semi-solids | 2 |
| solid and liquids | 3 |
| Oropharyngeal Symptoms | |
| Regurgitation | |
| none | 0 |
| occasional | 1 |
| daily | 2 |
| Halitosis | |
| none | 0 |
| occasional | 1 |
| daily | 2 |
| Respiratory Symptoms | |
| Cough | |
| none | 0 |
| occasional | 1 |
| daily | 2 |
| Hoarseness | |
| none | 0 |
| occasional | 1 |
| daily | 2 |
| Pneumonia | |
| No | 0 |
| Yes | 2 |
| Characteristic | Value |
|---|---|
| Age, mean ± SD, years | 67.55 ± 10.7 |
| Male gender—n (%) | 14 (63.3%) |
| BMI, median (IQR), kg/m2 | 24.5 (23.9–27.0) |
| Prior endoscopic treatment—n (%) | 2 (9.1%) |
| Size of ZD, median (IQR), mm | 30 (20–40) |
| Presenting symptoms—n (%) | |
| Dysphagia | 22 (100%) |
| Regurgitations | 19 (86.4%) |
| Hoarseness | 14 (63.3%) |
| Cough | 12 (54.5%) |
| Halitosis | 8 (36.4%) |
| Weight loss | 7 (31.8%) |
| Aspirational pneumonia | 3 (13.6%) |
| Outcomes | Value |
|---|---|
| Technical success—n (%) | 22 (100%) |
| Clinical success—n (%) | 20 (90.9%) |
| Procedural time, mean ± SD, min | 48.8 (±19.4) |
| Days of hospitalization, median (IQR) | 2 (2–3) |
Intraprocedural complications—n (%)
| 3 (13.6%) |
Postprocedural adverse events—n (%)
| 3 (13.6%) |
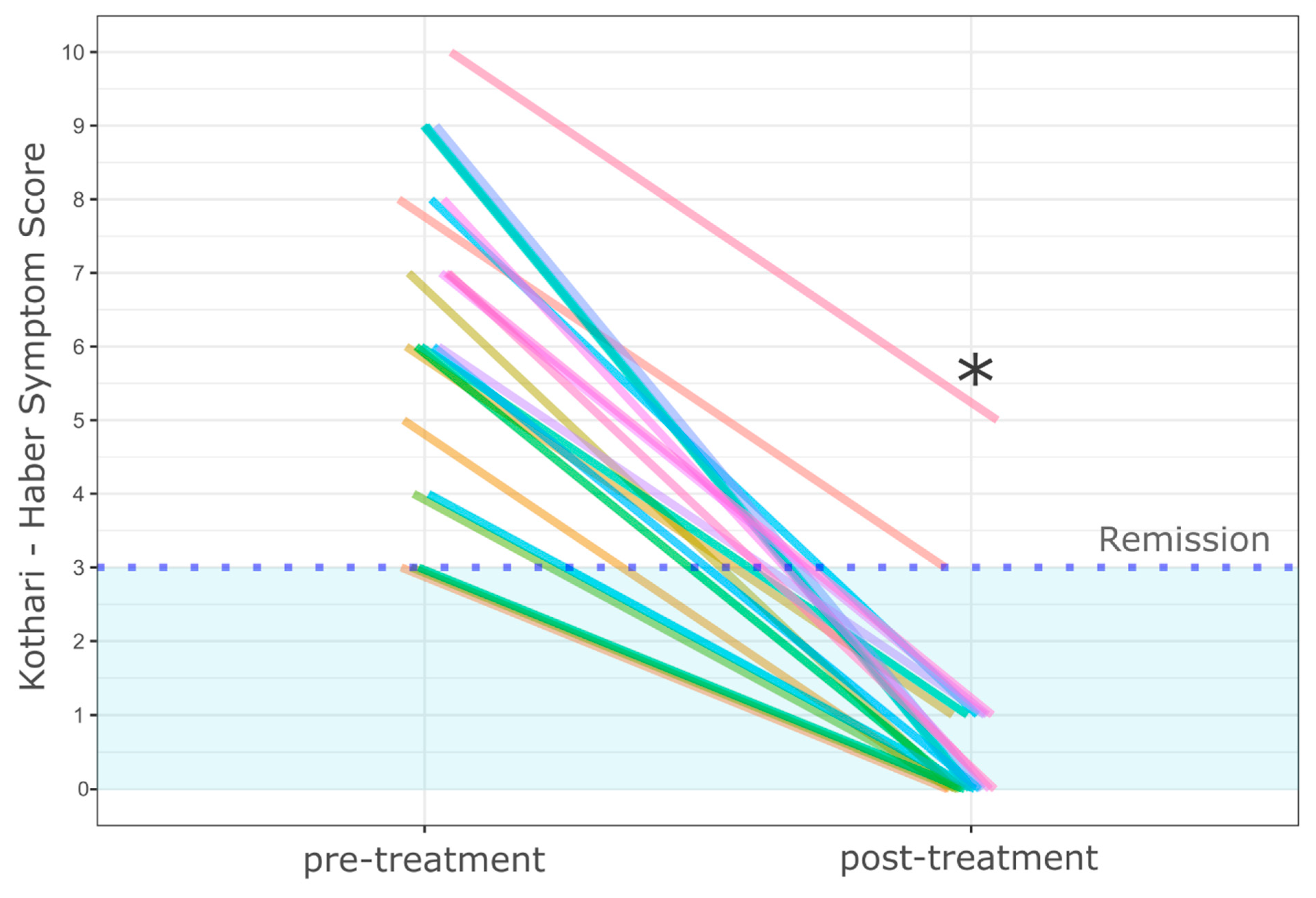
| Pre-procedure Kothari-Haber System Scoring, mean (±SD) | 6.4 (±2.1) |
| Post-procedure Kothari-Haber System Scoring, mean (±SD) | 0.6 (±1.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budnicka, A.; Januszewicz, W.; Białek, A.B.; Spychalski, M.; Reguła, J.; Kaminski, M.F. Peroral Endoscopic Myotomy in the Management of Zenker’s Diverticulum: A Retrospective Multicenter Study. J. Clin. Med. 2021, 10, 187. https://doi.org/10.3390/jcm10020187
Budnicka A, Januszewicz W, Białek AB, Spychalski M, Reguła J, Kaminski MF. Peroral Endoscopic Myotomy in the Management of Zenker’s Diverticulum: A Retrospective Multicenter Study. Journal of Clinical Medicine. 2021; 10(2):187. https://doi.org/10.3390/jcm10020187
Chicago/Turabian StyleBudnicka, Aleksandra, Władysław Januszewicz, Andrzej B. Białek, Michal Spychalski, Jaroslaw Reguła, and Michal F. Kaminski. 2021. "Peroral Endoscopic Myotomy in the Management of Zenker’s Diverticulum: A Retrospective Multicenter Study" Journal of Clinical Medicine 10, no. 2: 187. https://doi.org/10.3390/jcm10020187
APA StyleBudnicka, A., Januszewicz, W., Białek, A. B., Spychalski, M., Reguła, J., & Kaminski, M. F. (2021). Peroral Endoscopic Myotomy in the Management of Zenker’s Diverticulum: A Retrospective Multicenter Study. Journal of Clinical Medicine, 10(2), 187. https://doi.org/10.3390/jcm10020187





