Educational Differences in Diabetes Mortality among Hispanics in the United States: An Epidemiological Analysis of Vital Statistics Data (1989–2018)
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Population
2.2. Primary Outcome
Amenable Mortality
2.3. Stratifying Variables
2.4. Statistical Analysis
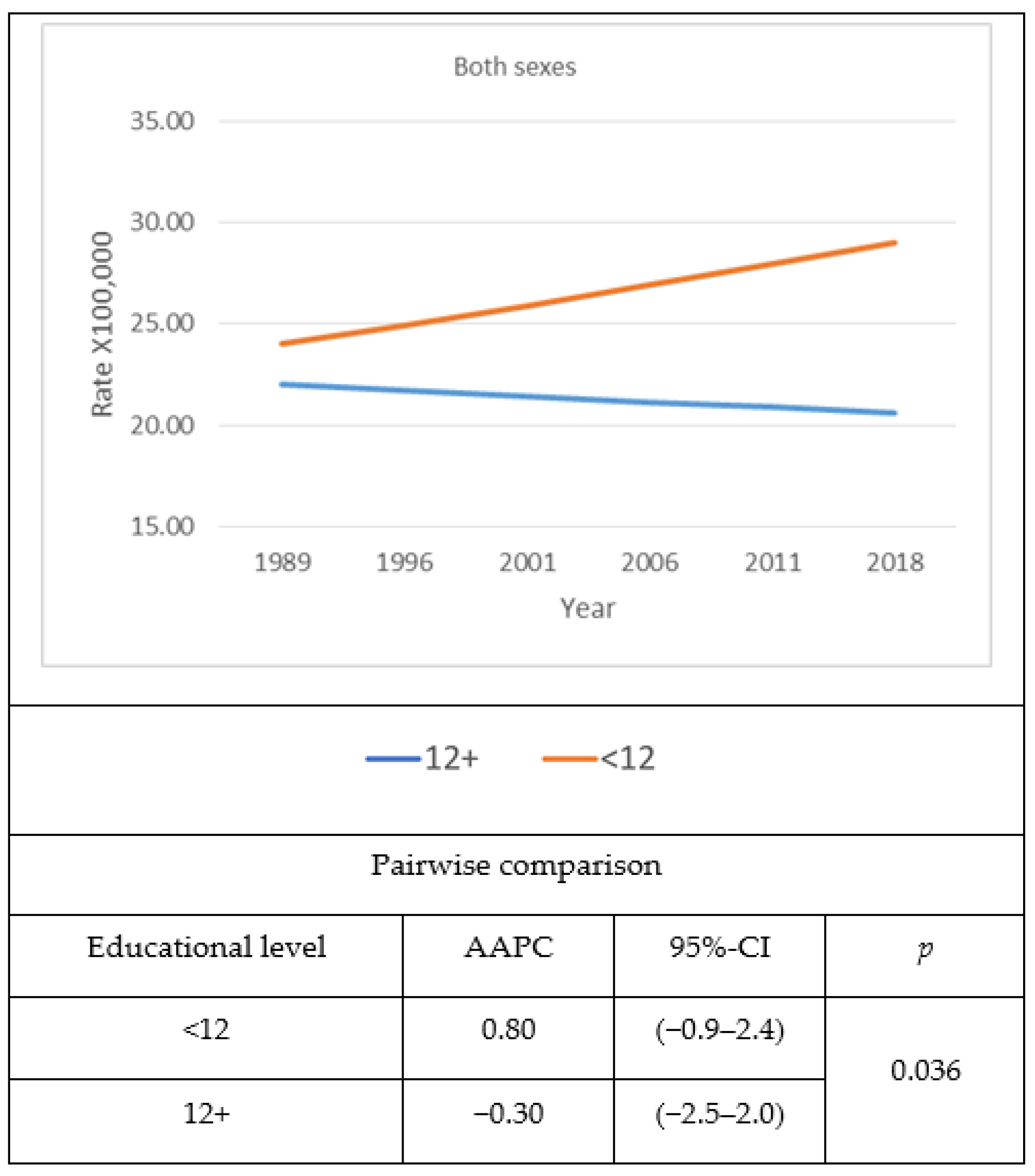
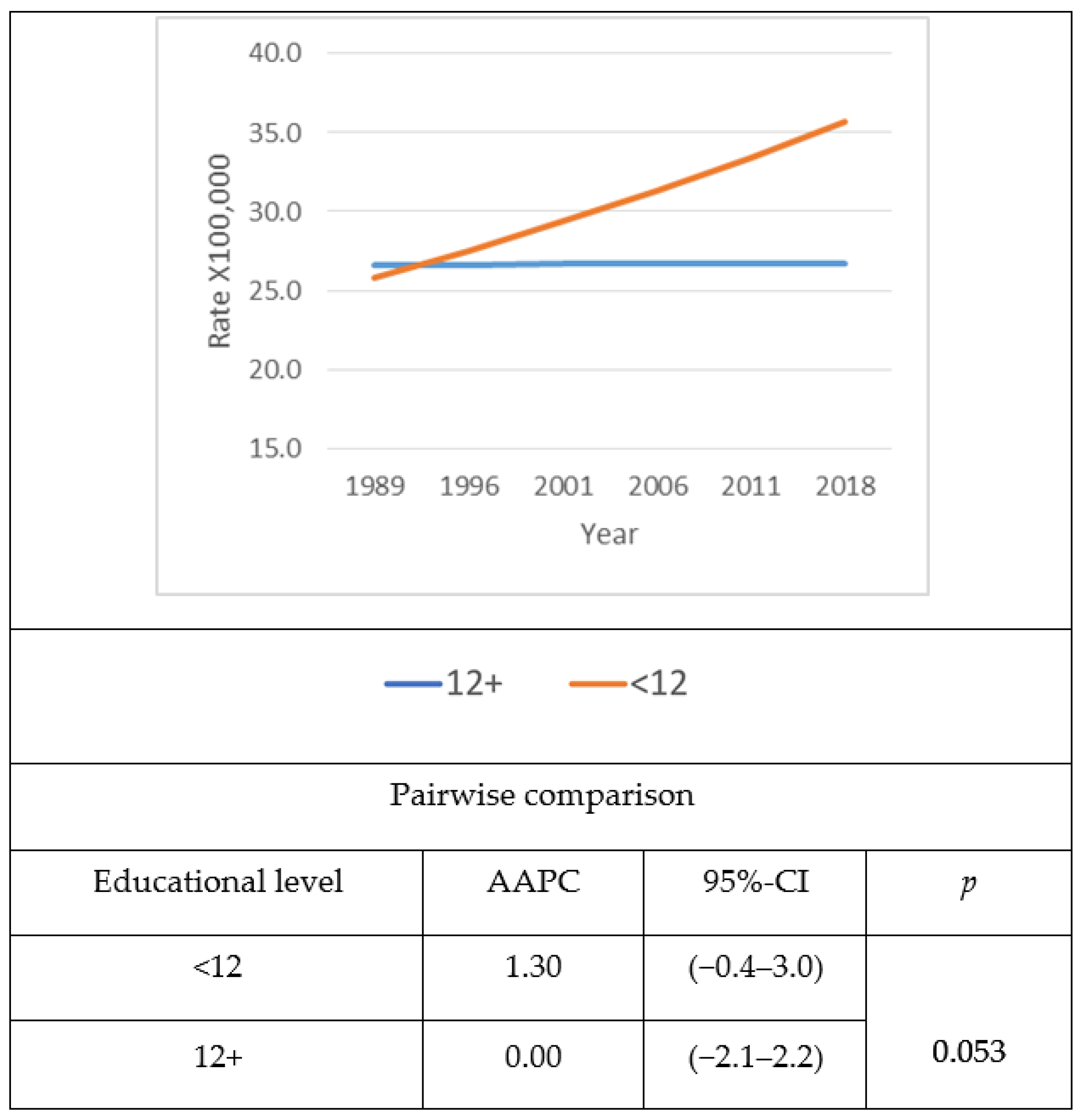
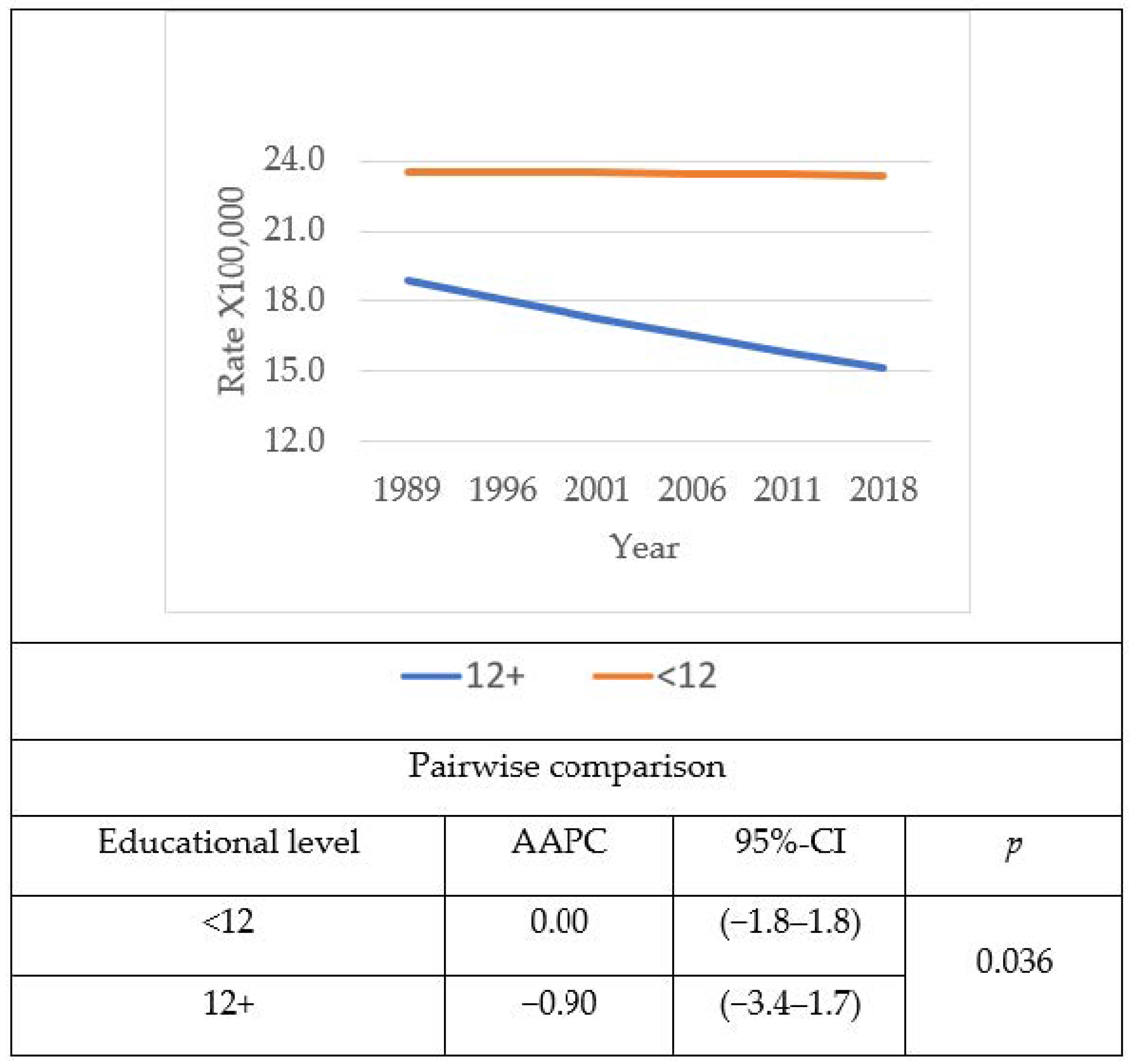
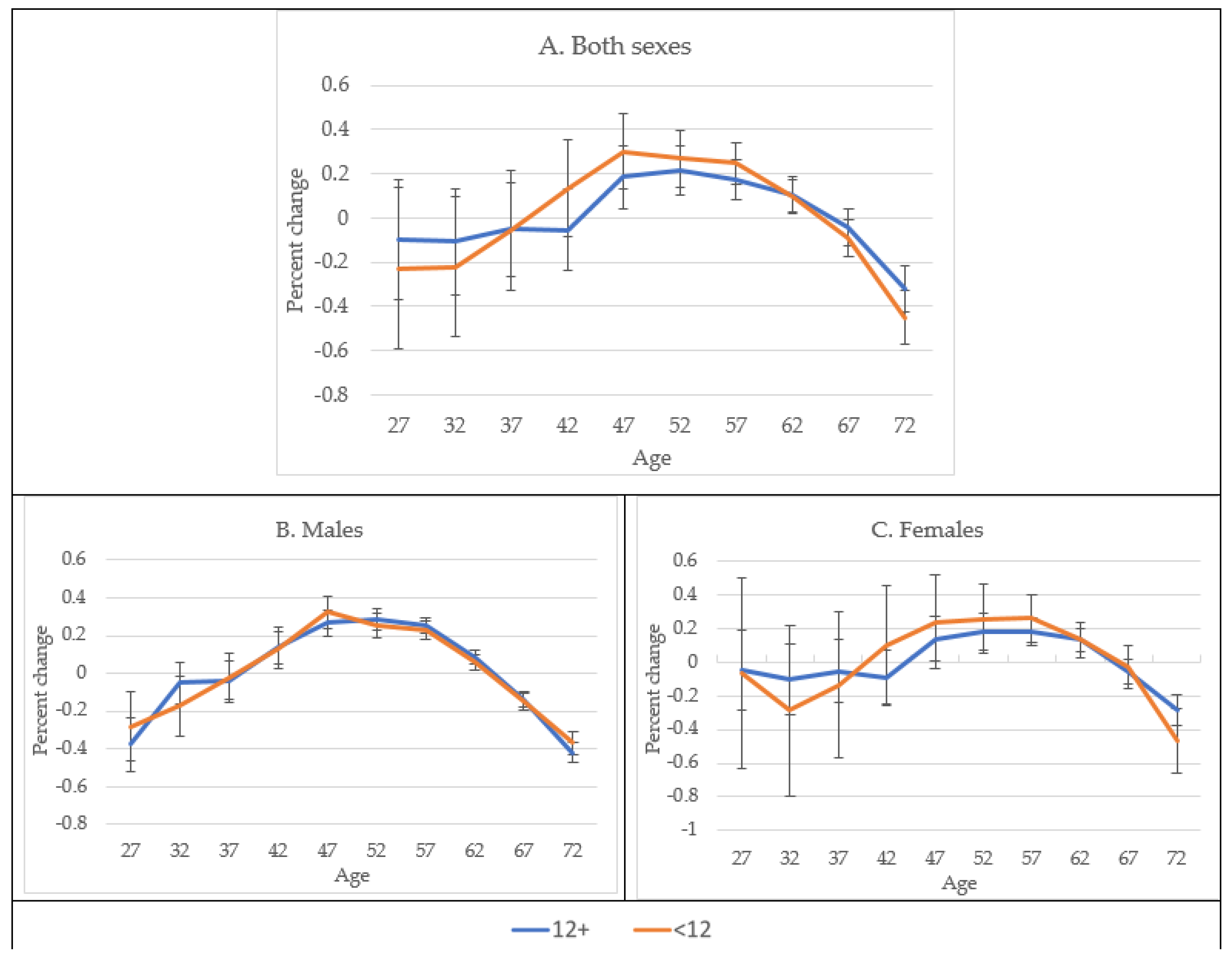
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Name | Abbreviation |
| Non-Hispanic Whites | NHW |
| Non-Hispanic Blacks | NHB |
| United States of America | USA |
| 95% Confidence Intervals | 95%-CI |
| Probability | p |
| Age–Period–Cohort Model | APCM |
| Age–Period–Cohort Web Tool | APCWT |
| Average Annual Percent Change | AAPC |
| Body Mass Index | BMI |
| Centers for Disease Control and Prevention | CDC |
| Relative Risk | RR |
References
- Saeedi, P.; Salpea, P.; Karuranga, S.; Petersohn, I.; Malanda, B.; Gregg, E.W.; Unwin, N.; Wild, S.H.; Williams, R. Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 2020, 162, 108086. [Google Scholar] [CrossRef] [Green Version]
- Gregg, E.W.; Cheng, Y.J.; Srinivasan, M.; Lin, J.; Geiss, L.S.; Albright, A.L.; Imperatore, G. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: An epidemiological analysis of linked national survey and vital statistics data. Lancet 2018, 391, 2430–2440. [Google Scholar] [CrossRef]
- Buscemi, J.; Saiyed, N.; Silva, A.; Ghahramani, F.; Benjamins, M.R. Diabetes mortality across the 30 biggest U.S. cities: Assessing overall trends and racial inequities. Diabetes Res. Clin. Pract. 2021, 173, 108652. [Google Scholar] [CrossRef]
- USA-CDC; Centers for Disease Control and Prevention. National Diabetes Statistics Report; Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services: Atlanta, GA, USA, 2020. Available online: https://www.cdc.gov/diabetes/library/features/diabetes-stat-report.html (accessed on 4 July 2021).
- USA-CDC. Hispanic/Latino Americans and Type 2 Diabetes. Centers for Disease Control and Prevention, Department of Health & Human Services. Available online: https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html#:~:text=Diabetes%20Affects%20Hispanics%2FLatinos%20More,it%20at%20a%20younger%20age (accessed on 4 April 2021).
- Kamody, R.C.; Grilo, C.M.; Vásquez, E.; Udo, T. Diabetes prevalence among diverse Hispanic populations: Considering nativity, ethnic discrimination, acculturation, and BMI. Eating and Weight Disorders-Studies on Anorexia. Bulim. Obes. 2021. [Google Scholar] [CrossRef]
- Steele, E.M.; Khandpur, N.; Sun, Q.; Monteiro, C.A. The impact of acculturation to the US environment on the dietary share of ultra-processed foods among US adults. Prev. Med. 2020, 141, 106261. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Kanaya, A.M.; Araneta, M.R.G.; Saydah, S.H.; Kahn, H.S.; Gregg, E.W. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011–2016. JAMA 2019, 322, 2389–2398. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief 2017, 288, 1–8. [Google Scholar]
- Baraldi, L.G.; Steele, E.M.; Canella, D.S.; Monteiro, C.A. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: Evidence from a nationally representative cross-sectional study. BMJ Open 2018, 83, e020574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonafini, B.A.; Pozzilli, P. Body weight and beauty: The changing face of the ideal female body weight. Obes. Rev. 2011, 12, 62–65. [Google Scholar] [CrossRef]
- Gregg, E.W.; Zhuo, X.; Cheng, Y.J.; Albright, A.L.; Narayan, K.M.V.; Thompson, T.J. Trends in lifetime risk and years of life lost due to diabetes in the USA, 1985–2011: A modelling study. Lancet. Diabetes. Endocrinol. 2014, 2, 867–874. [Google Scholar] [CrossRef]
- Raghavan, S.; Vassy, J.L.; Ho, Y.L.; Song, R.J.; Gagnon, D.R.; Cho, K.; Wilson, P.W.F.; Phillips, L.S. Diabetes Mellitus-Related All-Cause and Cardiovascular Mortality in a National Cohort of Adults. J. Am. Heart Assoc. 2019, 8, e011295. [Google Scholar] [CrossRef] [Green Version]
- Rutstein, D.D.; Berenberg, W.; Chalmers, T.C.; Child, C.G.; Fishman, A.P., 3rd; Perrin, E.B. Measuring the quality of medical care. A clinical method. N. Engl. J. Med. 1976, 294, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Nolte, E.; McKee, C.M. In amenable mortality-deaths avoidable through health care-progress in the US lags that of three European countries. Health Aff. 2012, 31, 2114–2122. [Google Scholar] [CrossRef] [Green Version]
- Nolte, E.; McKee, M. Variations in amenable mortality-Trends in 16 high-income nations. Health Policy 2011, 103, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Nolte, E.; McKee, M. Measuring the health of nations: Analysis of mortality amenable to health care. Br. Med. J. 2003, 327, 1129–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meara, E.R.; Richards, S.; Cutler, D.M. The gap gets bigger: Changes in mortality and life expectancy, by education, 1981–2000. Health Aff. 2008, 27, 350–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masters, R.K.; Link, B.G.; Phelan, J.C. Trends in education gradients of ‘preventable’ mortality: A test of fundamental cause theory. Soc. Sci. Med. 2015, 127, 19–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montez, J.K.; Hummer, R.A.; Hayward, M.D. Educational attainment and adult mortality in the United States: A systematic analysis of functional form. Demography 2012, 49, 315–336. [Google Scholar] [CrossRef] [Green Version]
- Dray-Spira, R.; Gary-Webb, T.L.; Brancati, F.L. Educational disparities in mortality among adults with diabetes in the U.S. Diabetes Care 2010, 33, 1200–1205. [Google Scholar] [CrossRef] [Green Version]
- Goldman, N.; Kimbro, R.T.; Turra, C.M.; Pebley, A.R. Socioeconomic gradients in health for white and Mexican-origin populations. Am. J. Public Health 2006, 96, 2186–2193. [Google Scholar] [CrossRef]
- Mercado, C.; Beckles, G.; Cheng, Y.; Bullard, K.M.; Saydah, S.; Gregg, E.; Imperatore, G. Trends and socioeconomic disparities in all-cause mortality among adults with diagnosed diabetes by race/ethnicity: A population-based cohort study-USA, 1997–2015. BMJ Open 2021, 11, e044158. [Google Scholar] [CrossRef] [PubMed]
- Barcelo, A.; Colugnati, F.; Pastor-Valero, M. The role of education and ethnicity on amenable mortality due to five leading non-communicable diseases among Blacks and Whites in the United States, 1990–2015. J. Glob. Health Rep. 2020, 438, e2020050. [Google Scholar] [CrossRef]
- USA-CDC. Profile: Hispanic/Latino Americans. U.S. Department of Health and Human Services Office of Minority Health. Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64#:~:text=According%20to%20the%202017%20U.S.,the%20largest%20at%2062.3%20percent (accessed on 10 April 2021).
- NBER. National Bureau of Economic Research. Mortality Data-Vital Statistics NCHS’ Multiple Cause of Death Data, 1959–2017. Available online: https://www2.nber.org/data/vital-statistics-mortality-data-multiple-cause-of-death.html (accessed on 5 July 2021).
- USA. United States Census Bureau, Current Population Survey, 2017 Annual Social and Economic Supplement. Available online: https://www.census.gov/data/tables/time-series/demo/educational-attainment/cps-historical-time-series.html (accessed on 17 February 2019).
- USA-CDC. International Classification of Diseases, Ninth Revision (ICD-9). Available online: https://www.cdc.gov/nchs/icd/icd9.html (accessed on 2 July 2021).
- USA-CDC; Center for Disease Control & Prevention/National Center for Health Statistics; US Department of Health & Human Services. Public Use Data Tape Documentation. Multiple Causes of Death for ICD-9 1990–1989; US-CDC: Hyattsville, MD, USA, 1989. [Google Scholar]
- US-CDC. International Classification of Diseases, Tenth Revision (ICD-10). Available online: https://www.cdc.gov/nchs/icd/icd10cm.html (accessed on 2 July 2021).
- Nolte, E.; McKee, C.M. Measuring the health of nations: Updating an earlier analysis. Health Aff. 2008, 27, 58–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, R.G.; Everett, B.G.; Zajacova, A.; Hummer, R.A. Educational degrees and adult mortality risk in the United States. Biodemogr. Soc. Biol. 2010, 56, 80–99. [Google Scholar] [CrossRef] [PubMed]
- Montez, J.K.; Zajacova, A.; Hayward, M.D.; Woolf, S.H.; Chapman, D.; Beckfield, J. Educational Disparities in Adult Mortality Across, U.S. States: How Do They Differ, and Have They Changed Since the Mid-1980s? Demography 2019, 56, 621–644. [Google Scholar] [CrossRef] [PubMed]
- NCI. National Cancer Institute. Joinpoint Regression Program, Version 4.8.0.1-April 2020; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute: Bethesda, MD, USA, 2018. [Google Scholar]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Clegg, L.X.; Hankey, B.F.; Tiwari, R.; Feuer, E.J.; Edwards, B.K. Estimating average annual per cent change in trend analysis. Stat. Med. 2009, 28, 3670–3682. [Google Scholar] [CrossRef] [Green Version]
- Xie, S.H.; Chen, J.; Zhang, B.; Wang, F.; Li, S.S.; Xie, C.H.; Tse, L.; Cheng, J. Time trends and age-period-cohort analyses on incidence rates of thyroid cancer in Shanghai and Hong Kong. BMC Cancer 2014, 14, 975. [Google Scholar] [CrossRef]
- Wasserstein, R.L.; Schirm, A.L.; Lazar, N.A. Moving to a World Beyond “p < 0.05”. Am. Stat. 2019, 73, 1–19. [Google Scholar]
- Rosenberg, P.S.; Anderson, W.F. Age-period-cohort models in cancer surveillance research: Ready for prime time? Cancer Epidemiol. Biomark. Prev. 2011, 20, 1263–1268. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, P.S.; Check, D.P.; Anderson, W.F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomarks Prev. 2014, 23, 2296–2302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krogstad, J.; Noe-Bustamante, L. Key facts about U.S. Latinos for National Hispanic Heritage Month. 10 September 2020. Pew Research Center tabulation 2018 American Community Survey (IPUMS). 2020. Available online: https://www.pewresearch.org/fact-tank/2020/09/10/key-facts-about-u-s-latinos-for-national-hispanic-heritage-month/ (accessed on 19 August 2021).
- Schneiderman, N.; Llabre, M.; Cowie, C.C.; Barnhart, J.; Carnethon, M.; Gallo, L.C.; Giachello, A.L.; Heiss, G.; Kaplan, R.C.; LaVange, L.M.; et al. Prevalence of diabetes among /Latinos from diverse backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care 2014, 37, 2233–2239. [Google Scholar] [CrossRef] [Green Version]
- Gallardo-Rincon, H.; Cantoral, A.; Arrieta, A.; Espinal, C.; Magnus, M.H.; Palacios, C.; Tapia-Conyer, R. Review: Type 2 diabetes in Latin America and the Caribbean: Regional and country comparison on prevalence, trends, costs and expanded prevention. Prim. Care Diabetes 2020, 15, 352–359. [Google Scholar] [CrossRef]
- Kelley, A.T.; Mizokami-Stout, K.; O’Brien, M.J.; Bowen, M.E.; Sussman, J. Hispanic representation in diabetes cardiovascular outcomes trials. BMJ Open Diabetes Res. Care 2019, 7, e000656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, J.; Nichols, G.A.; Qian, L.; Munis, M.A.; Harrison, T.N.; Li, Z.; Wei, R.; Weiss, T.; Rajpathak, S.; Reynolds, K. Prevalence and incidence of microvascular and macrovascular complications over 15 years among patients with incident type 2 diabetes. BMJ Open Diabetes Res. Care 2021, 9, e001847. [Google Scholar] [CrossRef] [PubMed]
- Hummer, R.A.; Hernandez, E.M. Population bulletin: The effect of educational attainment on adult mortality in the United States. Popul. Bull. 2013, 68, 1–20. [Google Scholar] [PubMed]
- Hayward, M.D.; Hummer, R.A.; Sasson, I. Trends and group differences in the association between educational attainment and U.S. adult mortality: Implications for understanding education’s causal influence. Soc. Sci. Med. 2015, 127, 8–18. [Google Scholar] [CrossRef] [Green Version]
- Adler, N.E.; Newman, K. Socioeconomic disparities in health: Pathways and policies. Health Aff. 2002, 21, 60–76. [Google Scholar] [CrossRef]
- Hayward, M.D.; Miles, T.P.; Crimmins, E.M.; Yang, Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am. Sociol. Rev. 2000, 65, 910–930. [Google Scholar] [CrossRef]
- Beckles, G.L.; Chou, C.F. Disparities in the prevalence of diagnosed diabetes—United States, 1999–2002 and 2011–2014. Morb. Mortal. Wkly. Rep. 2016, 65, 1265–1269. [Google Scholar] [CrossRef] [Green Version]



| Education | ||||||
|---|---|---|---|---|---|---|
| Sex/Period | <12 Grade | 12+ Grade | All | |||
| No Deaths | Rate per 100,000 | No Deaths | Rate per 100,000 | No Deaths | Rate per 100,000 | |
| Males | ||||||
| 1989–1993 | 2348 | 18.39 | 1379 | 9.68 | 3727 | 13.80 |
| 1994–1998 | 3734 | 23.02 | 2722 | 13.85 | 6456 | 18.00 |
| 1999–2003 | 4492 | 23.10 | 3721 | 14.51 | 8213 | 18.21 |
| 2004–2008 | 5049 | 21.29 | 4682 | 13.57 | 9731 | 16.71 |
| 2009–2013 | 5177 | 21.29 | 5939 | 14.00 | 11,116 | 16.66 |
| 2014–2018 | 6269 | 32.18 | 8394 | 20.70 | 14,663 | 24.43 |
| Females | ||||||
| 1989–1993 | 2887 | 22.39 | 1084 | 7.48 | 3971 | 14.50 |
| 1994–1998 | 4317 | 24.79 | 2183 | 10.86 | 6500 | 17.33 |
| 1999–2003 | 4791 | 26.16 | 2849 | 10.83 | 7640 | 17.13 |
| 2004–2008 | 4594 | 22.38 | 3233 | 9.48 | 7827 | 14.33 |
| 2009–1013 | 4288 | 20.17 | 3686 | 8.62 | 7974 | 12.46 |
| 2014–2018 | 4671 | 26.49 | 5269 | 12.48 | 9940 | 16.61 |
| Both | ||||||
| 1989–1993 | 5235 | 20.4 | 2463 | 8.57 | 7698 | 14.15 |
| 1994–1998 | 8051 | 23.93 | 4905 | 12.34 | 12,956 | 17.66 |
| 1999–2003 | 9283 | 24.58 | 6570 | 12.65 | 15,853 | 17.67 |
| 2004–2008 | 9643 | 21.80 | 7915 | 11.54 | 17,558 | 15.56 |
| 2009–1013 | 9465 | 20.77 | 9625 | 11.30 | 19,090 | 14.60 |
| 2014–2018 | 10,940 | 29.47 | 13,663 | 16.51 | 24,603 | 20.52 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barcelo, A.; Valdivia, A.; Sabag, A.; Rey-Lopez, J.P.; Galil, A.G.d.S.; Colugnati, F.A.B.; Pastor-Valero, M. Educational Differences in Diabetes Mortality among Hispanics in the United States: An Epidemiological Analysis of Vital Statistics Data (1989–2018). J. Clin. Med. 2021, 10, 4498. https://doi.org/10.3390/jcm10194498
Barcelo A, Valdivia A, Sabag A, Rey-Lopez JP, Galil AGdS, Colugnati FAB, Pastor-Valero M. Educational Differences in Diabetes Mortality among Hispanics in the United States: An Epidemiological Analysis of Vital Statistics Data (1989–2018). Journal of Clinical Medicine. 2021; 10(19):4498. https://doi.org/10.3390/jcm10194498
Chicago/Turabian StyleBarcelo, Alberto, Alfredo Valdivia, Angelo Sabag, Juan Pablo Rey-Lopez, Arise Garcia de Siqueira Galil, Fernando A.B. Colugnati, and María Pastor-Valero. 2021. "Educational Differences in Diabetes Mortality among Hispanics in the United States: An Epidemiological Analysis of Vital Statistics Data (1989–2018)" Journal of Clinical Medicine 10, no. 19: 4498. https://doi.org/10.3390/jcm10194498
APA StyleBarcelo, A., Valdivia, A., Sabag, A., Rey-Lopez, J. P., Galil, A. G. d. S., Colugnati, F. A. B., & Pastor-Valero, M. (2021). Educational Differences in Diabetes Mortality among Hispanics in the United States: An Epidemiological Analysis of Vital Statistics Data (1989–2018). Journal of Clinical Medicine, 10(19), 4498. https://doi.org/10.3390/jcm10194498






