Sex Differences in Chronic Thromboembolic Pulmonary Hypertension. Treatment Options over Time in a National Referral Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Biomarkers, Functional Tests, and Hemodynamic Variables
2.3. Medical Therapies and Interventions
2.4. Classification of Disease
2.5. Outcomes
2.6. Statistical Analysis
3. Results
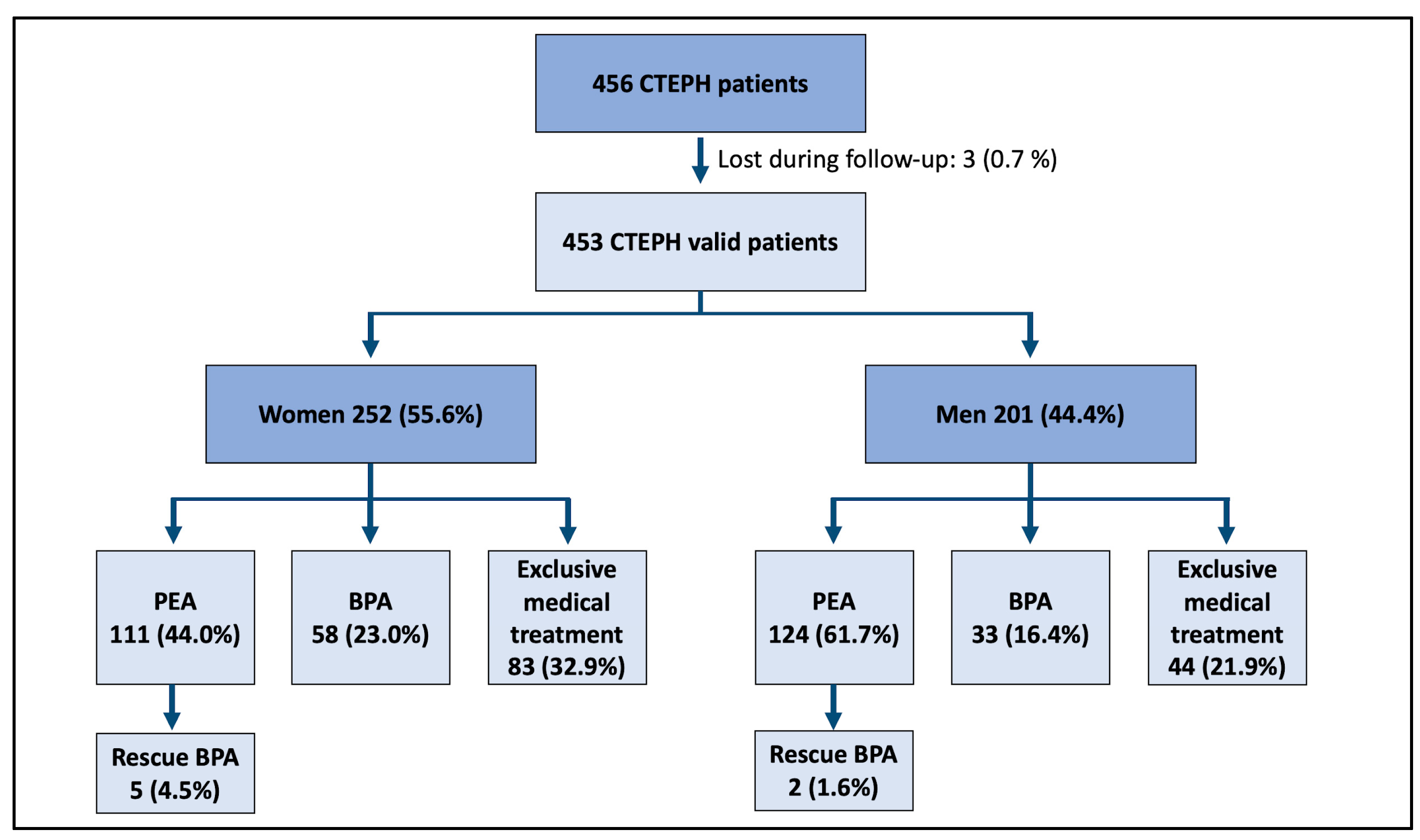
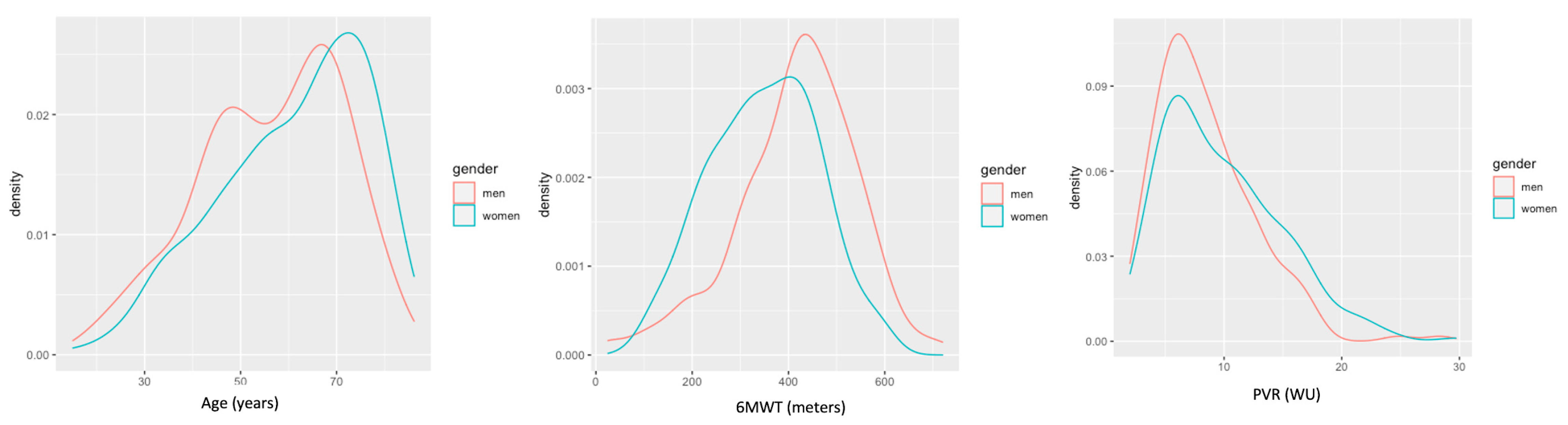
3.1. Study Population. A Global Gender Perspective in CTEPH
3.2. Sex Differences in Treatment Groups and Disease Distribution
3.3. Therapeutic Trends
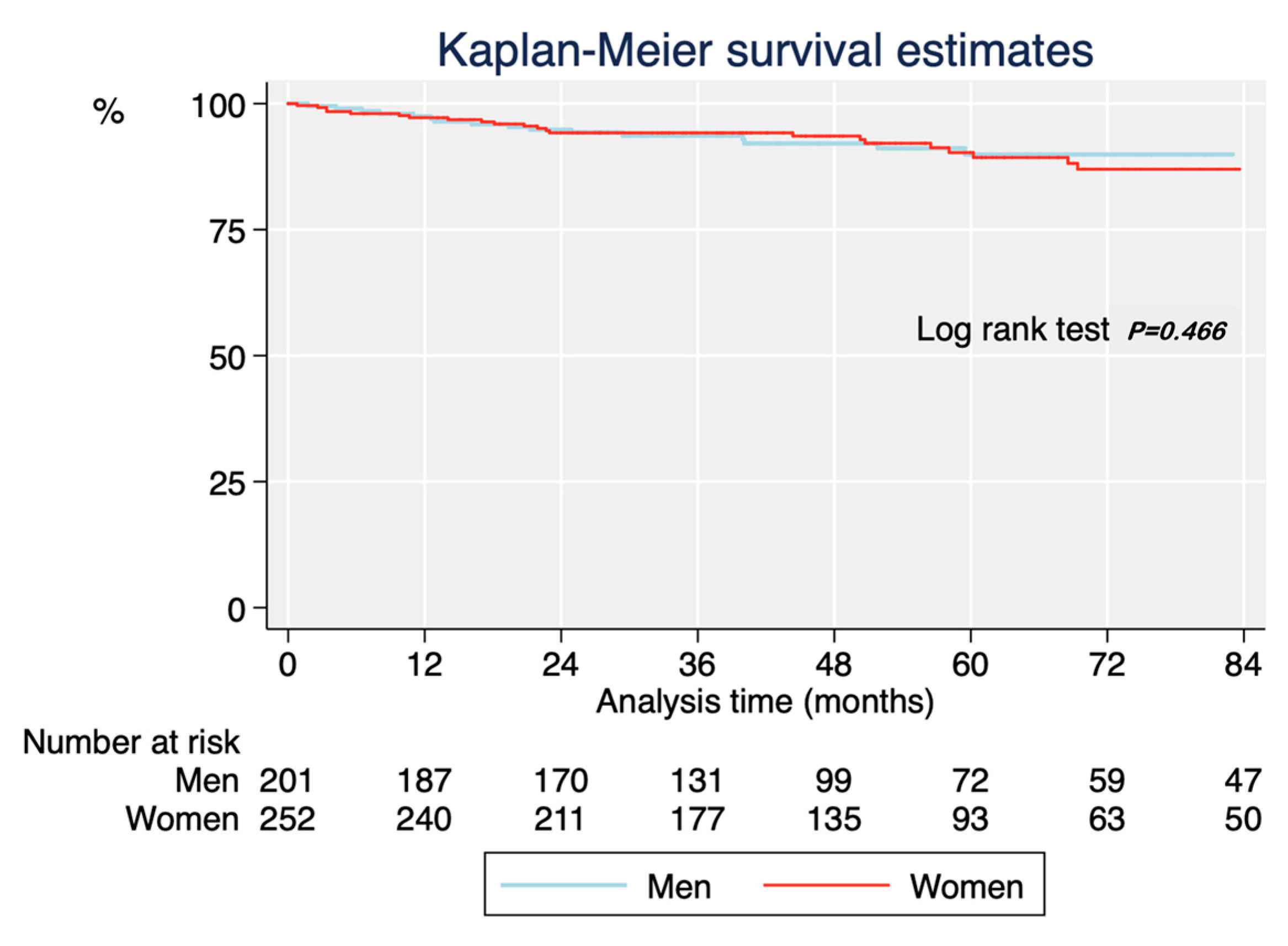
3.4. Prognosis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moser, K.M.; Auger, W.R.; Fedullo, P.F. Chronic major-vessel thromboembolic pulmonary hypertension. Circulation 1990, 81, 1735–1743. [Google Scholar] [CrossRef] [Green Version]
- Kim, N.H.; Delcroix, M.; Jais, X.; Madani, M.M.; Matsubara, H.; Mayer, E.; Ogo, T.; Tapson, V.F.; Ghofrani, H.A.; Jenkins, D.P. Chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2019, 53, 1801915. [Google Scholar] [CrossRef]
- Riedel, M.; Stanek, V.; Widimsky, J.; Prerovsky, I. Longterm follow-up of patients with pulmonary thromboembolism. Late prognosis and evolution of hemodynamic and respiratory data. Chest 1982, 81, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.P.; Madani, M.; Mayer, E.; Kerr, K.; Kim, N.; Klepetko, W.; Morsolini, M.; Dartevelle, P. Surgical treatment of chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2013, 41, 735–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taniguchi, Y.; Miyagawa, K.; Nakayama, K.; Kinutani, H.; Shinke, T.; Okada, K.; Okita, Y.; Hirata, K.-I.; Emoto, N. Balloon pulmonary angioplasty: An additional treatment option to improve the prognosis of patients with chronic thromboembolic pulmonary hypertension. EuroIntervention 2014, 10, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Velázquez, M.; Albarrán, A.; Hernández, I.; López-Gude, M.J.; Sarnago, F.; Martín, R.; Arribas, F.; Escribano, P. Balloon Pulmonary Angioplasty for Inoperable Patients With Chronic Thromboembolic Pulmonary Hypertension. Observational Study in a Referral Unit. Revista Española de Cardiología 2019, 72, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Skoro-Sajer, N.; Bonderman, D.; Wiesbauer, F.; Harja, E.; Jakowitsch, J.; Klepetko, W.; Kneussl, M.P.; Lang, I.M. Treprostinil for severe inoperable chronic thromboembolic pulmonary hypertension. J. Thromb. Haemost. 2007, 5, 483–489. [Google Scholar] [CrossRef]
- Cabrol, S.; Souza, R.; Jais, X.; Fadel, E.; Ali, R.H.S.; Humbert, M.; Dartevelle, P.; Simonneau, G.; Sitbon, O. Intravenous Epoprostenol in Inoperable Chronic Thromboembolic Pulmonary Hypertension. J. Heart Lung Transplant. 2007, 26, 357–362. [Google Scholar] [CrossRef]
- Ghofrani, H.-A.; Simonneau, G.; D’Armini, A.M.; Fedullo, P.; Howard, L.S.; Jais, X.; Jenkins, D.P.; Jing, Z.-C.; Madani, M.M.; Martin, N.; et al. Macitentan for the treatment of inoperable chronic thromboembolic pulmonary hypertension (MERIT-1): Results from the multicentre, phase 2, randomised, double-blind, placebo-controlled study. Lancet Respir. Med. 2017, 5, 785–794. [Google Scholar] [CrossRef]
- Jaïs, X.; D’Armini, A.M.; Jansa, P.; Torbicki, A.; Delcroix, M.; Ghofrani, H.A.; Hoeper, M.M.; Lang, I.M.; Mayer, E.; Pepke-Zaba, J.; et al. Bosentan for Treatment of Inoperable Chronic Thromboembolic Pulmonary Hypertension: BENEFiT (Bosentan Effects in iNopErable Forms of chronIc Thromboembolic pulmonary hypertension), a Randomized, Placebo-Controlled Trial. J. Am. Coll. Cardiol. 2008, 52, 2127–2134. [Google Scholar] [CrossRef] [PubMed]
- Pepke-Zaba, J.; Jansa, P.; Kim, N.H.; Naeije, R.; Simonneau, G. Chronic thromboembolic pulmonary hypertension: Role of medical therapy. Eur. Respir. J. 2013, 41, 985–990. [Google Scholar] [CrossRef] [Green Version]
- Barco, S.; Klok, F.A.; Konstantinides, S.V.; Dartevelle, P.; Fadel, E.; Jenkins, D.; Kim, N.H.; Madani, M.; Matsubara, H.; Mayer, E.; et al. Sex-specific differences in chronic thromboembolic pulmonary hypertension. Results from the European CTEPH registry. J. Thromb. Haemost. 2020, 18, 151–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escribano-Subias, P.; Blanco, I.; López-Meseguer, M.; Lopez-Guarch, C.J.; Roman, A.; Morales, P.; Castillo-Palma, M.J.; Segovia, J.; Gómez-Sanchez, M.A.; Barberà, J.A. Survival in pulmonary hypertension in Spain: Insights from the Spanish registry. Eur. Respir. J. 2012, 40, 596–603. [Google Scholar] [CrossRef]
- Galiè, N.; Humbert, M.; Vachiery, J.-L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endor. Eur. Heart. J. 2016, 37, 67–119. [Google Scholar] [CrossRef] [PubMed]
- Madani, M.; Mayer, E.; Fadel, E.; Jenkins, D.P. Pulmonary Endarterectomy. Patient Selection, Technical Challenges, and Outcomes. Ann. Am. Thorac. Soc. 2016, 13, S240–S247. [Google Scholar] [CrossRef]
- Rodriguez Chaverri, A.; Revilla Ostolaza, Y.; Lopez-Gude, M.J.; Velazquez, M.T.; Ponz de Antonio, I.; Alonso Charterina, S.; Albarran Gonzalez-Trevilla, A.; Perez Nunez, M.; Perez Vela, J.L.; Morales Ruiz, R.; et al. Feasibility of a Noninvasive Operability Assessment in Chronic Thromboembolic Pulmonary Hypertension under Real-World Practice. Diagnostics 2020, 10, 855. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Farber, H.W.; Ghofrani, H.A.; Benza, R.L.; Busse, D.; Meier, C.; Hoeper, M.M. Risk assessment in pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2019, 53, 1802004. [Google Scholar] [CrossRef]
- Tobita, K.; Goda, A.; Nishida, Y.; Takeuchi, K.; Kikuchi, H.; Inami, T.; Kohno, T.; Yamada, S.; Soejima, K.; Satoh, T. Factors contributing to exercise capacity in chronic thromboembolic pulmonary hypertension with near-normal hemodynamics. J. Heart Lung Transplant. 2021, 40, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Syddall, H.; Cooper, C.; Martin, F.; Briggs, R.; Sayer, A.A. Is grip strength a useful single marker of frailty? Age Ageing 2003, 32, 650–656. [Google Scholar] [CrossRef] [Green Version]
- Manders, E.; Bonta, P.I.; Kloek, J.J.; Symersky, P.; Bogaard, H.-J.; Hooijman, P.E.; Jasper, J.R.; Malik, F.I.; Stienen, G.J.M.; Vonk-Noordegraaf, A.; et al. Reduced force of diaphragm muscle fibers in patients with chronic thromboembolic pulmonary hypertension. Am. J. Physiol. Cell. Mol. Physiol. 2016, 311, L20–L28. [Google Scholar] [CrossRef] [Green Version]
- Farooqi, M.A.M.; Killian, K.; Satia, I. The impact of muscle strength on exercise capacity and symptoms. ERJ. Open Res. 2020, 6, 89–2020. [Google Scholar] [CrossRef]
- Vaes, B.; Depoortere, D.; Van Pottelbergh, G.; Matheï, C.; Neto, J.; Degryse, J. Association between traditional cardiovascular risk factors and mortality in the oldest old: Untangling the role of frailty. BMC Geriatr. 2017, 17, 234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerr, K.M.; Elliott, C.G.; Chin, K.; Benza, R.L.; Channick, R.N.; Davis, R.D.; He, F.; LaCroix, A.; Madani, M.M.; McLaughlin; et al. Results From the United States Chronic Thromboembolic Pulmonary Hypertension Registry: Enrollment Characteristics and 1-Year Follow-up. Chest 2021. Article in Press. [Google Scholar] [CrossRef] [PubMed]
- Quadery, S.R.; Swift, A.J.; Billings, C.G.; Thompson, A.A.; Elliot, C.A.; Hurdman, J.; Charalampopoulos, A.; Sabroe, I.; Armstrong, I.J.; Hamilton, N.; et al. The impact of patient choice on survival in chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2018, 52, 1800589. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Jenkins, M.; Glaser, D. Gender differences in risk assessment: Why do women take fewer risks than men? Judgm. Decis. Mak. 2006, 1, 48–63. [Google Scholar]
- Martin, Y.N.; Pabelick, C.M. Sex differences in the pulmonary circulation: Implications for pulmonary hypertension. Am. J. Physiol. Circ. Physiol. 2014, 306, H1253–H1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barco, S.; Klok, F.A.; Mahé, I.; Marchena, P.J.; Ballaz, A.; Rubio, C.M.; Adarraga, M.D.; Mastroiacovo, D.; Konstantinides, S.V.; Monreal, M.; et al. Impact of sex, age, and risk factors for venous thromboembolism on the initial presentation of first isolated symptomatic acute deep vein thrombosis. Thromb. Res. 2019, 173, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Scheres, L.J.J.; Brekelmans, M.P.A.; Beenen, L.F.M.; Büller, H.R.; Cannegieter, S.C.; Middeldorp, S. Sex-specific differences in the presenting location of a first venous thromboembolism. J. Thromb. Haemost. 2017, 15, 1344–1350. [Google Scholar] [CrossRef] [Green Version]
- Robert-Ebadi, H.; Le Gal, G.; Carrier, M.; Couturaud, F.; Perrier, A.; Bounameaux, H.; Righini, M. Differences in clinical presentation of pulmonary embolism in women and men. J. Thromb. Haemost. 2010, 8, 693–698. [Google Scholar] [CrossRef]
- Hobohm, L.; Keller, K.; Münzel, T.; Konstantinides, S.V.; Lankeit, M. Time trends of pulmonary endarterectomy in patients with chronic thromboembolic pulmonary hypertension. Pulm. Circ. 2021, 11, 20458940211008069. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Matsuoka, Y.; Onishi, H.; Yanaka, K.; Emoto, N.; Nakai, H.; Okada, K.; Hirata, K. The role of balloon pulmonary angioplasty and pulmonary endarterectomy: Is chronic thromboembolic pulmonary hypertension still a life-threatening disease? Int. J. Cardiol. 2021, 326, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef] [Green Version]
- Benza, R.L.; Gomberg-Maitland, M.; Miller, D.; Frost, A.; Frantz, R.; Foreman, A.J.; Badesch, D.B.; McGoon, M.D. The REVEAL Registry Risk Score Calculator in Patients Newly Diagnosed With Pulmonary Arterial Hypertension. Chest 2012, 141, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Stouffer, G.A.; Kucharska-Newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Porterfield, D.; Blankstein, R.; Rosamond, W.D.; Bhatt, D.L.; et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation. 2019, 139, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Mehran, R.; Vogel, B.; Ortega, R.; Cooney, R.; Horton, R. The Lancet Commission on women and cardiovascular disease: Time for a shift in women’s health. Lancet 2019, 393, 967–968. [Google Scholar] [CrossRef]
- Chen, T.; Yuan, P.; Liu, J. Gender difference of survival in Chinese patients with inoperable chronic thromboembolic pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2018, 197, A6335. [Google Scholar]
- Shigeta, A.; Tanabe, N.; Shimizu, H.; Hoshino, S.; Maruoka, M.; Sakao, S.; Tada, Y.; Kasahara, Y.; Takiguchi, Y.; Tatsumi, K.; et al. Gender Differences in Chronic Thromboembolic Pulmonary Hypertension in Japan. Circ. J. 2008, 72, 2069–2074. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Santos, P.; Velázquez-Martín, M.T.; Barberá, J.A.; Pérez, C.F.; López-Meseguer, M.; López-Reyes, R.; Martínez-Meñaca, A.; Lara-Padrón, A.; Domingo-Morera, J.A.; Blanco, I.; et al. Chronic thromboembolic pulmonary hypertension in Spain: A decade of change. Revista Española de Cardiología (Engl. Ed.) 2021, 74, 384–392. [Google Scholar] [CrossRef]


| CTEPH Patient Characteristics at Diagnosis by Type of Procedure and Sex (n = 453). | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PEA | BPA | MT | ||||||||||
| n (%N) | Women | Men | p Value | n (%N) | Women | Men | p Value | n (%N) | Women | Men | p Value | |
| Number of patients—(n/%) | 235 (100.0) | 111 (44.1) | 124 (61.7) | <0.001 | 91 (100.0) | 58 (41.1) | 33 (42.9) | 0.805 | 127 (100.0) | 83 (32.9) | 44 (21.9) | 0.009 |
| Age—years (median—IQr) | 235 (100.0) | 53.5 (41.2–66.2) | 55.8 (45.5–65.7) | 0.672 | 91 (100.0) | 66.2 (56.3–74.5) | 57.4 (40.6–72.0) | 0.033 | 127 (100.0) | 71.7 (59.6–71.7) | 66.0 (50.7–73.4) | 0.013 |
| Arterial hypertension (n/%) | 235 (100.0) | 36 (32.4) | 48 (38.7) | 0.316 | 91 (100.0) | 31 (53.5) | 10 (30.3) | 0.033 | 127 (100.0) | 40 (48.2) | 19 (43.2) | 0.590 |
| Diabetes (n/%) | 235 (100.0) | 12 (10.8) | 9 (7.3) | 0.341 | 91 (100.0) | 10 (17.2) | 1 (3.0) | 0.046 | 127 (100.0) | 13 (15.7) | 5 (11.4) | 0.509 |
| Dyslipidemia (n/%) | 235 (100.0) | 25 (22.5) | 25 (20.2) | 0.659 | 91 (100.0) | 14 (24.1) | 7 (21.2) | 0.750 | 127 (100.0) | 36 (43.4) | 10 (22.7) | 0.021 |
| BMI (median—IQr) | 231 (98.3) | 29.4 (23.4–31.4) | 27.2 (24.4–30.1) | 0.417 | 74 (81.3) | 28.2 (26.0–32.0) | 26.8 (23.5–30.5) | 0.114 | 102 (80.3) | 28.0 (24.2–31.0) | 29.0 (26.0–31.0) | 0.240 |
| Coronary artery disease (n/%) | 235 (100.0) | 5 (4.5) | 9 (7.3) | 0.373 | 91 (100.0) | 1 (1.7) | 2 (6.1) | 0.265 | 127 (100.0) | 4 (4.8) | 4 (9.1) | 0.346 |
| Functional class—NYHA (n/%)III-IV | 218 (92.8) | 77 (74.8) | 77 (67.0) | 0.207 | 90 (98.9) | 37 (63.8) | 15 (46.9) | 0.120 | 127 (100.0) | 50 (60.2) | 17 (38.6) | 0.020 |
| Six-minute walking test—meters (mean ± SD) | 159 (67.7) | 366.2 ± 12.7 | 425.6 ± 14.6 | 0.003 | 87 (95.6) | 335.4 ± 15.2 | 423.3 ± 20.5 | 0.001 | 117 (92.1) | 340.9 ± 12.3 | 388.3 ± 19.3 | 0.034 |
| Nt-proBNP—mg/dL (median—IQr) | 149 (63.4) | 643.5 (289.0–2012.0) | 478.0 (86.0–1912.0) | 0.275 | 89 (97.8) | 633.0 (175.0–2079.0) | 702.5 (244.5–1369.5) | 0.949 | 110 (86.6) | 290.5 (126.5–1823.5) | 262.0 (105.0–1087.0) | 0.375 |
| FEV1—% predicted (mean ± SD) | 137 (58.3) | 82.5 ± 1.7 | 78.7 ± 1.8 | 0.126 | 72 (79.1) | 89.6 ± 2.4 | 80.7 ± 3.8 | 0.044 | 105 (82.7) | 91.5 ± 2.5 | 84.4 ± 2.9 | 0.074 |
| FVC—% predicted (mean ± SD) | 133 (56.6) | 89.0 (73.0–99.0) | 86.5 (76.0–96.0) | 0.693 | 81 (89.0) | 95.0 (74.0–105.0) | 84.2 (74.0–98.0) | 0.206 | 103 (81.1) | 93.0 (80.0–110.0) | 90.7 (83.0–100.5) | 0.349 |
| PE history (n/%) | 235 (100.0) | 91 (82.0) | 102 (82.3) | 0.956 | 91 (100.0) | 42 (72.4) | 21 (63.6) | 0.383 | 127 (100.0) | 65 (78.3) | 36 (81.8) | 0.641 |
| Hypercoagulability (n/%) | 182 (77.4) | 57 (60.6) | 53 (60.2) | 0.955 | 86 (94.5) | 18 (32.7) | 11 (35.5) | 0.795 | 118 (92.9) | 33 (41.8) | 16 (41.0) | 0.938 |
| Unadjusted, Stratified by Sex and Adjusted Univariate Cox Regression Analysis for Mortality | |||||
|---|---|---|---|---|---|
| Crude HR (CI 95%) | p Value | Stratified by Sex (CI 95%) | p Value | Adjusted * (CI 95%) | |
| Sex (women vs. men) | 1.26 (0.68–2.35) | 0.467 | 0.98 (0.52–1.87) | ||
| Age (Per 10-year increment) | 1.43 (1.13–1.81) | 0.003 | Men 1.33 (0.91–1.93) Women 1.52 (1.12–2.06) | 0.138 0.007 | 1.02 (0.99–1.04) |
| BMI—Kg/m2 (By increments of 10 Kg/m2) | 1.03 (0.96–1.10) | 0.458 | Men: 1.14 (1.02–1.27) Women: 0.97 (0.88–1.06) | 0.024 0.491 | 1.01 (0.94–1.09) |
| Systemic hypertension | 1.75 (0.96–3.21) | 0.070 | Men: 1.34 (0.50–3.59) Women: 2.13 (0.97–4.64) | 0.566 0.058 | 1.38 (0.73–2.59) |
| Diabetes mellitus | 1.84 (0.82–4.17) | 0.078 | Men: 0.77 (0.10–5.84) Women: 2.50 (0.99–6.29) | 0.802 0.052 | 1.59 (0.70–3.63) |
| Dyslipidemia | 1.18 (0.60–2.30 | 0.637 | Men: 0.1 (0.1-inf) Women: 2.24 (1.03–4.87) | 1.000 0.041 | 0.80 (0.40–1.62) |
| Smoking habits | 1.00 (0.53–1.90) | 0.995 | Men: 0.65 (0.24–1.80) Women: 1.46 (0.63–3.36) | 0.410 0.376 | 1.27 (0.64–2.52) |
| Cancer history | 1.27 (0.56–2.86) | 0.566 | Men: 1.43 (0.41–5.02) Women: 1.15 (0.39–3.33) | 0.576 0.802 | 1.16 (0.51–2.63) |
| Coronary artery disease | 1.69 (0.60–4.74) | 0.318 | Men: 1.66 (0.38–7.30) Women: 1.70 (0.40–7.21) | 0.503 0.473 | 1.46 (0.52–4.13) |
| 6MWT—meters (by increments of 30 m) | 0.74 (0.62–0.89) | 0.002 | Men: 0.86 (0.60–1.23) Women: 0.64 (0.50–0.83) | 0.417 0.001 | 0.70 (0.56–0.87) |
| NtproBNP—mg/dL (by increments of 1000) | 1.23 (1.14–1.23) | <0.001 | Men: 1.21 (1.04–1.42) Women: 1.21 (1.11–1.32) | 0.017 <0.001 | 1.23 (1.14–1.33) |
| WHO III-IV (reference WHO FC I-II) | 1.69 (0.83–3.45) | 0.149 | Men: 1.24 (0.42–3.64) Women: 2.18 (0.82–5.79) | 0.310 0.117 | 2.55 (1.22–5.36) |
| PVR—WU (by increments of 1 mmHg) | 1.04 (0.99–1.11) | 0.144 | Men: 1.01 (0.90–1.13) Women: 1.05 (0.98–1.13) | 0.907 0.160 | 1.08 (1.02–1.14) |
| CI—L/min/m2 (by increments of 1 l/m/m2) | 0.75 (0.46–1.25) | 0.271 | Men: 0.93 (0.40–2.16) Women: 0.67 (0.36–1.26) | 0.864 0.217 | 0.62 (0.37–1.03) |
| mPAP—mmHg (by increments of 10 mmHg) | 1.19 (0.91–1.55) | 0.202 | Men: 1.32 (0.85–2.04) Women:1.12 (0.80–1.57) | 0.215 0.496 | 1.46 (1.11–1.91) |
| RAP—mmHg (by increments of 1 mmHg) | 1.06 (1.01–1.11) | 0.044 | Men: 1.05 (0.96–1.14) Women: 1.05 (0.99–1.13) | 0.266 0.121 | 1.09 (1.03–1.15) |
| Type of treatment received (in reference to PEA)—BPA —Medical therapy | 1.20 (0.37–3.82) 6.23 (3.02–12.85) | 0.763 <0.001 | Men: 1.67 (0.32–8.65) Women: 0.90 (0.17–4.65) Men: 5.53 (1.85–16.54) Women: 6.66 (2.47–17.93) | 0.542 0.900 0.002 <0.001 | 1.39 (0.41–4.71) 4.91 (2.22–10.85) |
| Period of time (2014–2019 Vs 2007–2013) | 0.48 (0.25–0.91) | 0.024 | Men: 0.65 (0.24–1.77) Women: 0.38 (0.16–0.87) | 0.398 0.023 | 0.58 (0.29–1.16) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz-Utrilla, A.; Cristo-Ropero, M.J.; Calderón-Flores, M.; Velázquez, M.; López-Gude, M.J.; Revilla Ostolaza, Y.; Pérez Vela, J.L.; de la Cruz-Bértolo, J.; Bueno, H.; Arribas Ynsaurriaga, F.; et al. Sex Differences in Chronic Thromboembolic Pulmonary Hypertension. Treatment Options over Time in a National Referral Center. J. Clin. Med. 2021, 10, 4251. https://doi.org/10.3390/jcm10184251
Cruz-Utrilla A, Cristo-Ropero MJ, Calderón-Flores M, Velázquez M, López-Gude MJ, Revilla Ostolaza Y, Pérez Vela JL, de la Cruz-Bértolo J, Bueno H, Arribas Ynsaurriaga F, et al. Sex Differences in Chronic Thromboembolic Pulmonary Hypertension. Treatment Options over Time in a National Referral Center. Journal of Clinical Medicine. 2021; 10(18):4251. https://doi.org/10.3390/jcm10184251
Chicago/Turabian StyleCruz-Utrilla, Alejandro, María José Cristo-Ropero, Miguel Calderón-Flores, Maite Velázquez, María Jesús López-Gude, Yolanda Revilla Ostolaza, José Luis Pérez Vela, Javier de la Cruz-Bértolo, Héctor Bueno, Fernando Arribas Ynsaurriaga, and et al. 2021. "Sex Differences in Chronic Thromboembolic Pulmonary Hypertension. Treatment Options over Time in a National Referral Center" Journal of Clinical Medicine 10, no. 18: 4251. https://doi.org/10.3390/jcm10184251
APA StyleCruz-Utrilla, A., Cristo-Ropero, M. J., Calderón-Flores, M., Velázquez, M., López-Gude, M. J., Revilla Ostolaza, Y., Pérez Vela, J. L., de la Cruz-Bértolo, J., Bueno, H., Arribas Ynsaurriaga, F., Cortina, J. M., & Escribano-Subias, P. (2021). Sex Differences in Chronic Thromboembolic Pulmonary Hypertension. Treatment Options over Time in a National Referral Center. Journal of Clinical Medicine, 10(18), 4251. https://doi.org/10.3390/jcm10184251






