Weight Loss in Patients Waiting for Total Hip Arthroplasty: Fiber-Enriched High Carbohydrate Diet Improves Hip Function and Decreases Pain before Surgery
Abstract
1. Introduction
2. Materials and Methods
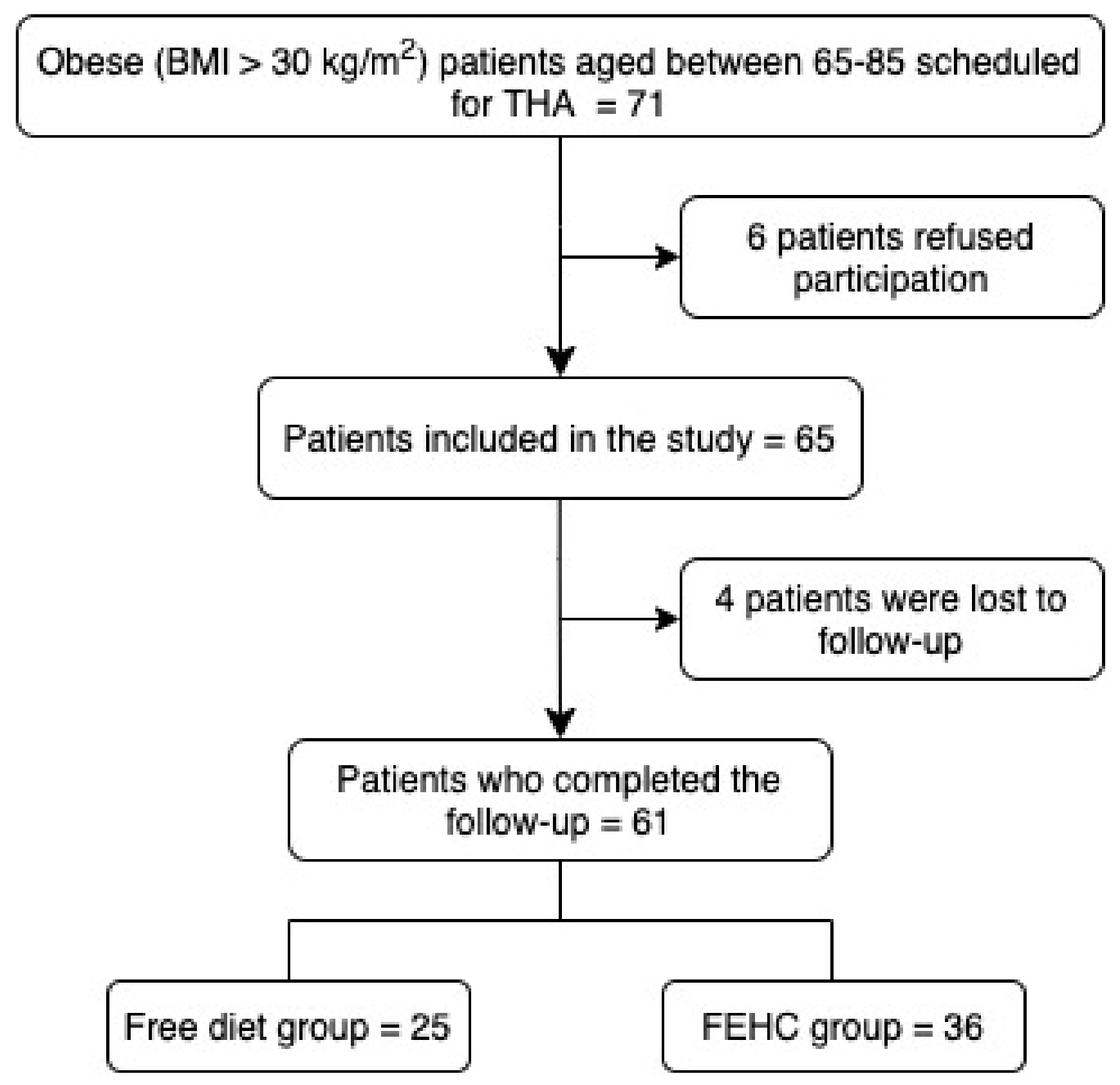
2.1. Patients
2.2. Study Variables and Outcome Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lupoli, R.; Lembo, E.; Saldalamacchia, G.; Avola, C.K.; Angrisani, L.; Capaldo, B. Bariatric surgery and long-term nutritional issues. World J. Diabetes 2017, 8, 464–474. [Google Scholar] [CrossRef]
- Gandhi, R.; Wasserstein, D.; Razak, F.; Davey, J.R.; Mahomed, N.N. BMI independently predicts younger age at hip and knee replacement. Obesity 2010, 18, 2362–2366. [Google Scholar] [CrossRef] [PubMed]
- Inacio, M.C.; Kritz-Silverstein, D.; Paxton, E.W.; Fithian, D.C. Do patients lose weight after joint arthroplasty surgery? A systematic review. Clin. Orthop. Relat Res. 2013, 471, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Kluzek, S.; Newton, J.L.; Arden, N.K. Is osteoarthritis a metabolic disorder? Br. Med. Bull. 2015, 115, 111–121. [Google Scholar] [CrossRef]
- Cannata, F.; Vadala, G.; Ambrosio, L.; Napoli, N.; Papalia, R.; Denaro, V.; Pozzilli, P. Osteoarthritis and type 2 diabetes: From pathogenetic factors to therapeutic intervention. Diabetes Metab. Res. Rev. 2020, 36, e3254. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.C.; Coggon, D. HIP osteoarthritis and work. Best Pract. Res. Clin. Rheumatol. 2015, 29, 462–482. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.D.; McEwan, J.; Adukia, V.; Prabhakar, M. Osteoarthritis and arthroplasty of the hip and knee. Br. J. Hosp. Med. 2018, 79, C54–C59. [Google Scholar] [CrossRef]
- Haverkamp, D.; Klinkenbijl, M.N.; Somford, M.P.; Albers, G.H.; van der Vis, H.M. Obesity in total hip arthroplasty—does it really matter? A meta-analysis. Acta Orthop. 2011, 82, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Huddleston, J.I.; Wang, Y.; Uquillas, C.; Herndon, J.H.; Maloney, W.J. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin. Orthop. Relat Res. 2012, 470, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Morshed, S.; Joseph, T.; Bozic, K.; Ries, M.D. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin. Orthop. Relat Res. 2006, 453, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.W.; Young, D.; Meek, D.R.M.; Patil, S.R. Obesity is associated with higher complication rates in revision total hip arthroplasty. J. Orthop. 2018, 15, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Namba, R.S.; Paxton, L.; Fithian, D.C.; Stone, M.L. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J. Arthroplast. 2005, 20, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.M.; Wood, A.M.; Keenan, A.C.; Brenkel, I.J.; Ballantyne, J.A. Does body mass index affect clinical outcome post-operatively and at five years after primary unilateral total hip replacement performed for osteoarthritis? A multivariate analysis of prospective data. J. Bone Joint Surg. Br. 2011, 93, 1178–1182. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.P.; Sexton, S.A.; Yeung, E.; Walter, W.L.; Walter, W.K.; Zicat, B.A. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J. Bone Joint Surg. Br. 2009, 91, 1296–1300. [Google Scholar] [CrossRef]
- Jones, C.A.; Cox, V.; Jhangri, G.S.; Suarez-Almazor, M.E. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthr. Cartil. 2012, 20, 511–518. [Google Scholar] [CrossRef]
- Lubbeke, A.; Stern, R.; Garavaglia, G.; Zurcher, L.; Hoffmeyer, P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007, 57, 327–334. [Google Scholar] [CrossRef]
- McCalden, R.W.; Charron, K.D.; MacDonald, S.J.; Bourne, R.B.; Naudie, D.D. Does morbid obesity affect the outcome of total hip replacement? An analysis of 3290 THRs. J. Bone Joint Surg. Br. 2011, 93, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Cannata, F.; Vadala, G.; Russo, F.; Papalia, R.; Napoli, N.; Pozzilli, P. Beneficial Effects of Physical Activity in Diabetic Patients. J. Funct. Morphol. Kinesiol. 2020, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Lui, M.; Jones, C.A.; Westby, M.D. Effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to hip and knee arthroplasty surgery: A rapid review. Syst. Rev. 2015, 4, 121. [Google Scholar] [CrossRef]
- Seward, M.W.; Briggs, L.G.; Bain, P.A.; Chen, A.F. Preoperative Nonsurgical Weight Loss Interventions Before Total Hip and Knee Arthroplasty: A Systematic Review. J. Arthroplast. 2021. [Google Scholar] [CrossRef]
- Drost, J.M.; Cook, C.B.; Spangehl, M.J.; Probst, N.E.; Mi, L.; Trentman, T.L. A Plant-Based Dietary Intervention for Preoperative Glucose Optimization in Diabetic Patients Undergoing Total Joint Arthroplasty. Am. J. Lifestyle Med. 2019, 1559827619879073. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Martinez-Gonzalez, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Wylde, V.; Learmonth, I.D.; Cavendish, V.J. The Oxford hip score: The patient’s perspective. Health Qual. Life Outcomes 2005, 3, 66. [Google Scholar] [CrossRef] [PubMed]
- Nilsdotter, A.K.; Lohmander, L.S.; Klassbo, M.; Roos, E.M. Hip disability and osteoarthritis outcome score (HOOS)—Validity and responsiveness in total hip replacement. BMC Musculoskelet. Disord. 2003, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- Wyrwich, K.W.; Bullinger, M.; Aaronson, N.; Hays, R.D.; Patrick, D.L.; Symonds, T. Estimating clinically significant differences in quality of life outcomes. Qual. Life Res. 2005, 14, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Reyes, C.; Leyland, K.M.; Peat, G.; Cooper, C.; Arden, N.K.; Prieto-Alhambra, D. Association Between Overweight and Obesity and Risk of Clinically Diagnosed Knee, Hip, and Hand Osteoarthritis: A Population-Based Cohort Study. Arthritis Rheumatol. 2016, 68, 1869–1875. [Google Scholar] [CrossRef] [PubMed]
- NICE. Joint Replacement (Primary): Hip, Knee and Shoulder. Available online: www.nice.org.uk/guidance/ng157 (accessed on 28 May 2021).
- Smith, T.O.; Aboelmagd, T.; Hing, C.B.; MacGregor, A. Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? Systematic review and meta-analysis. Bone Joint J. 2016, 98-B, 1160–1166. [Google Scholar] [CrossRef]
- Hauner, H. Secretory factors from human adipose tissue and their functional role. Proc. Nutr. Soc. 2005, 64, 163–169. [Google Scholar] [CrossRef]
- Thomas, S.; Browne, H.; Mobasheri, A.; Rayman, M.P. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology 2018, 57, iv61–iv74. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P.; et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef]
- Fernandes, L.; Hagen, K.B.; Bijlsma, J.W.; Andreassen, O.; Christensen, P.; Conaghan, P.G.; Doherty, M.; Geenen, R.; Hammond, A.; Kjeken, I.; et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann. Rheum. Dis. 2013, 72, 1125–1135. [Google Scholar] [CrossRef] [PubMed]
- Slavin, J. Fiber and prebiotics: Mechanisms and health benefits. Nutrients 2013, 5, 1417–1435. [Google Scholar] [CrossRef] [PubMed]
- Howarth, N.C.; Saltzman, E.; Roberts, S.B. Dietary fiber and weight regulation. Nutr. Rev. 2001, 59, 129–139. [Google Scholar] [CrossRef]
- Slavin, J.L. Dietary fiber and body weight. Nutrition 2005, 21, 411–418. [Google Scholar] [CrossRef]
- Clark, M.J.; Slavin, J.L. The effect of fiber on satiety and food intake: A systematic review. J. Am. Coll. Nutr. 2013, 32, 200–211. [Google Scholar] [CrossRef]
- Birketvedt, G.S.; Aaseth, J.; Florholmen, J.R.; Ryttig, K. Long-term effect of fibre supplement and reduced energy intake on body weight and blood lipids in overweight subjects. Acta Med. (Hradec Kralove) 2000, 43, 129–132. [Google Scholar] [CrossRef][Green Version]
- Mueller-Cunningham, W.M.; Quintana, R.; Kasim-Karakas, S.E. An ad libitum, very low-fat diet results in weight loss and changes in nutrient intakes in postmenopausal women. J. Am. Diet. Assoc. 2003, 103, 1600–1606. [Google Scholar] [CrossRef]
- Te Morenga, L.A.; Levers, M.T.; Williams, S.M.; Brown, R.C.; Mann, J. Comparison of high protein and high fiber weight-loss diets in women with risk factors for the metabolic syndrome: A randomized trial. Nutr. J. 2011, 10, 40. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, I.H. Evaluation of a high-fiber diet in hyperlipidemia: A review. J. Am. Coll. Nutr. 1987, 6, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Surampudi, P.; Enkhmaa, B.; Anuurad, E.; Berglund, L. Lipid Lowering with Soluble Dietary Fiber. Curr. Atheroscler. Rep. 2016, 18, 75. [Google Scholar] [CrossRef]
| FEHC Diet (n = 36) Mean (SD) or Median (IQR) or n (%) | Free Diet (n = 25) Mean (SD) or Median (IQR) or n (%) | p | |
|---|---|---|---|
| Age (years) | 74 (7) | 72 (6) | 0.146 |
| Gender (female) | 23 (64) | 13 (52) | 0.431 |
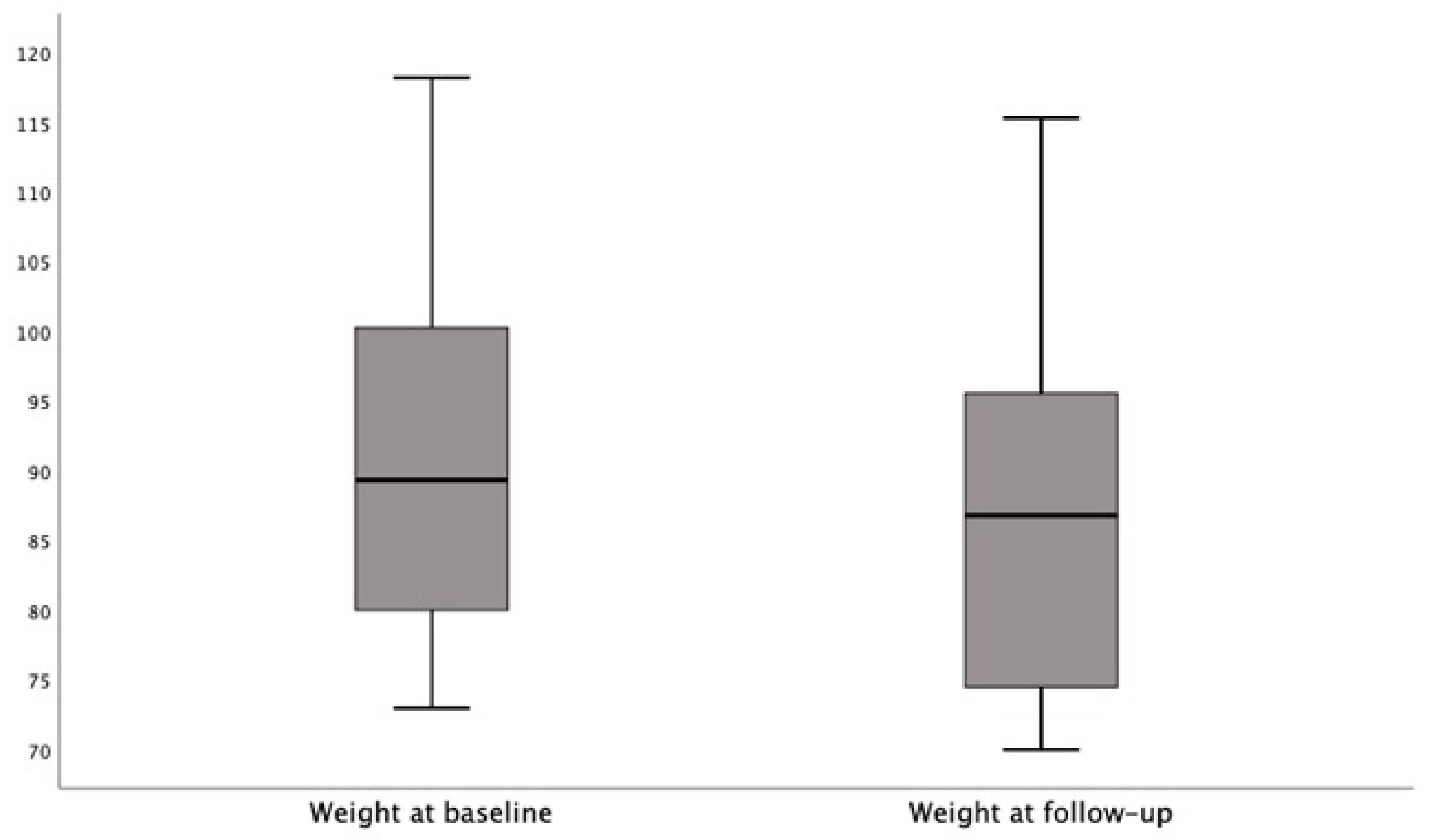
| Weight at baseline (kg) | 89.3 (80.0–100.2) | 91.5(84.0–95.6) | 0.889 |
| Weight at follow-up (kg) | 86.8 (74.5–95.5) | 89.0 (82.6–96.2) | 0.205 |
| BMI at baseline (kg/m2) | 33.4 (31.8–37.5) | 32.3 (30.9–34.3) | 0.070 |
| BMI at follow-up (kg/m2) | 31.7 (30.1–35.1) | 32.0 (30.8–33.8) | 0.832 |
| Total cholesterol at baseline (mg/dL) | 198 (40) | 202 (31) | 0.721 |
| Total cholesterol at follow-up (mg/dL) | 180 (28) | 203 (34) | 0.006 |
| OHS questionnaire baseline | 31 (27–44) | 37 (34–46) | 0.108 |
| OHS questionnaire follow-up | 38 (30–46) | 34 (29–41) | 0.199 |
| HOOS questionnaire baseline | 65 (53–88) | 32 (24–39) | <0.0001 |
| HOOS questionnaire follow-up | 65 (54–91) | 29 (23–31) | <0.0001 |
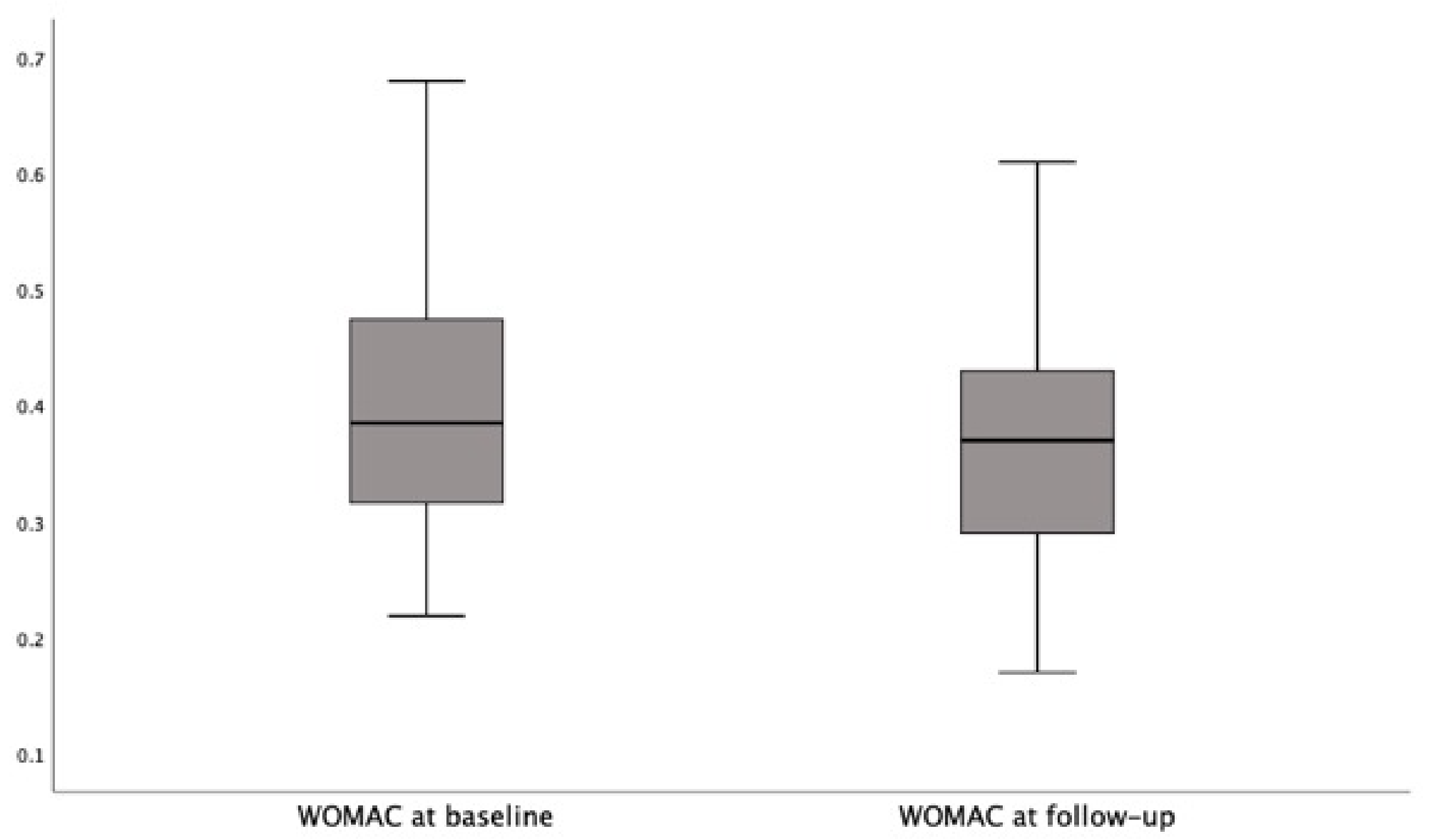
| WOMAC questionnaire baseline | 0.38 (0.32–0.47) | 0.39 (0.33–0.47) | 0.826 |
| WOMAC questionnaire follow-up | 0.37 (0.29–0.43) | 0.43 (0.37–0.49) | 0.005 |
| FEHC Diet (n = 36) | Free Diet (n = 25) | p | |
|---|---|---|---|
| Weight (kg) | −3.7 (−4.4–−2.5) | −0.2 (−1.4–1.7) | <0.0001 |
| BMI (kg/m2) | −1.5 (−2.0–−0.8) | 0.1 (−0.7–1.2) | <0.0001 |
| Total cholesterol (mg/dL) | 18 (7–33) | −9 (−12–−2) | <0.0001 |
| OHS questionnaire | 3 (2–7) | −4 (−10–0) | <0.0001 |
| HOOS questionnaire | 1 (−1–2) | −3 (−4–−2) | <0.0001 |
| WOMAC questionnaire | −0.05 (−0.05–−0.02) | 0.03 (0.02–0.05) | <0.0001 |
| FEHC Diet (n = 36) n (%) | Free Diet (n = 25) n (%) | p | |
|---|---|---|---|
| Weight loss | 35 (97) | 14 (56) | <0.0001 |
| BMI loss | 35 (97) | 14 (56) | <0.0001 |
| Reduced total cholesterol | 32 (89) | 5 (20) | <0.0001 |
| OHS questionnaire | 31 (86) | 6 (24) | <0.0001 |
| HOOS questionnaire | 24 (67) | 3 (12) | <0.0001 |
| WOMAC questionnaire | 18 (50) | 1 (4) | <0.0001 |
| Range of Score | MCID | |
|---|---|---|
| OHS questionnaire | 12–60 | 0.12 |
| HOOS questionnaire | 0–100 | 0.45 |
| WOMAC questionnaire | 0–96 | 0.10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannata, F.; Laudisio, A.; Russo, F.; Ambrosio, L.; Vadalà, G.; Cardinale, M.E.; Bartolomei, C.; Iannone, G.; Napoli, N.; Papalia, R. Weight Loss in Patients Waiting for Total Hip Arthroplasty: Fiber-Enriched High Carbohydrate Diet Improves Hip Function and Decreases Pain before Surgery. J. Clin. Med. 2021, 10, 4203. https://doi.org/10.3390/jcm10184203
Cannata F, Laudisio A, Russo F, Ambrosio L, Vadalà G, Cardinale ME, Bartolomei C, Iannone G, Napoli N, Papalia R. Weight Loss in Patients Waiting for Total Hip Arthroplasty: Fiber-Enriched High Carbohydrate Diet Improves Hip Function and Decreases Pain before Surgery. Journal of Clinical Medicine. 2021; 10(18):4203. https://doi.org/10.3390/jcm10184203
Chicago/Turabian StyleCannata, Francesca, Alice Laudisio, Fabrizio Russo, Luca Ambrosio, Gianluca Vadalà, Marco Edoardo Cardinale, Chiara Bartolomei, Gabriella Iannone, Nicola Napoli, and Rocco Papalia. 2021. "Weight Loss in Patients Waiting for Total Hip Arthroplasty: Fiber-Enriched High Carbohydrate Diet Improves Hip Function and Decreases Pain before Surgery" Journal of Clinical Medicine 10, no. 18: 4203. https://doi.org/10.3390/jcm10184203
APA StyleCannata, F., Laudisio, A., Russo, F., Ambrosio, L., Vadalà, G., Cardinale, M. E., Bartolomei, C., Iannone, G., Napoli, N., & Papalia, R. (2021). Weight Loss in Patients Waiting for Total Hip Arthroplasty: Fiber-Enriched High Carbohydrate Diet Improves Hip Function and Decreases Pain before Surgery. Journal of Clinical Medicine, 10(18), 4203. https://doi.org/10.3390/jcm10184203









