Predicting Outcome in an Intensive Outpatient PTSD Treatment Program Using Daily Measures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
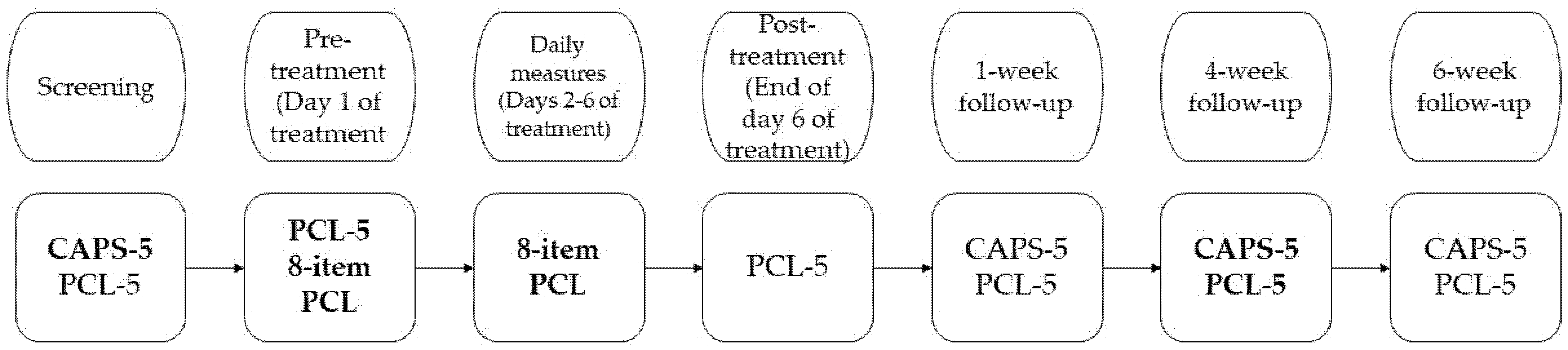
2.2. Procedure
2.3. Treatment
2.4. Measurements
- The Dutch version of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) assesses the frequency and intensity of the 20 DSM-5 PTSD symptoms [40,41]. Severity scores were computed as a sum score of the 20 symptom-specific severity scores, ranging from 0–80. The CAPS-5 was used for evaluating the existence of a PTSD diagnosis and measuring the change in PTSD symptoms. It has adequate validity and reliability [42].
- The Dutch version of the PTSD checklist for DSM-5 (PCL-5) is a 20-item self-report questionnaire intended to measure PTSD symptomatology with scores ranging from 0–80 [43,44]. It was administered to participants to measure the difference in PTSD symptomatology before and after treatment, and shows strong validity and reliability [45].
- An abbreviated 8-item version of the Dutch PCL-5 (from here onwards referred to as the 8-item PCL) was used to monitor the daily PTSD symptoms during treatment. This self-report instrument consists of 8 of the original 20 questions from the PCL-5 with scores ranging from 0–32. The 8-item PCL strongly correlated with the complete PCL-5 and has been recommended for use to monitor treatment progress [46]. For interpretive data on the 8-item PCL, readers are referred to Price et al. [46].
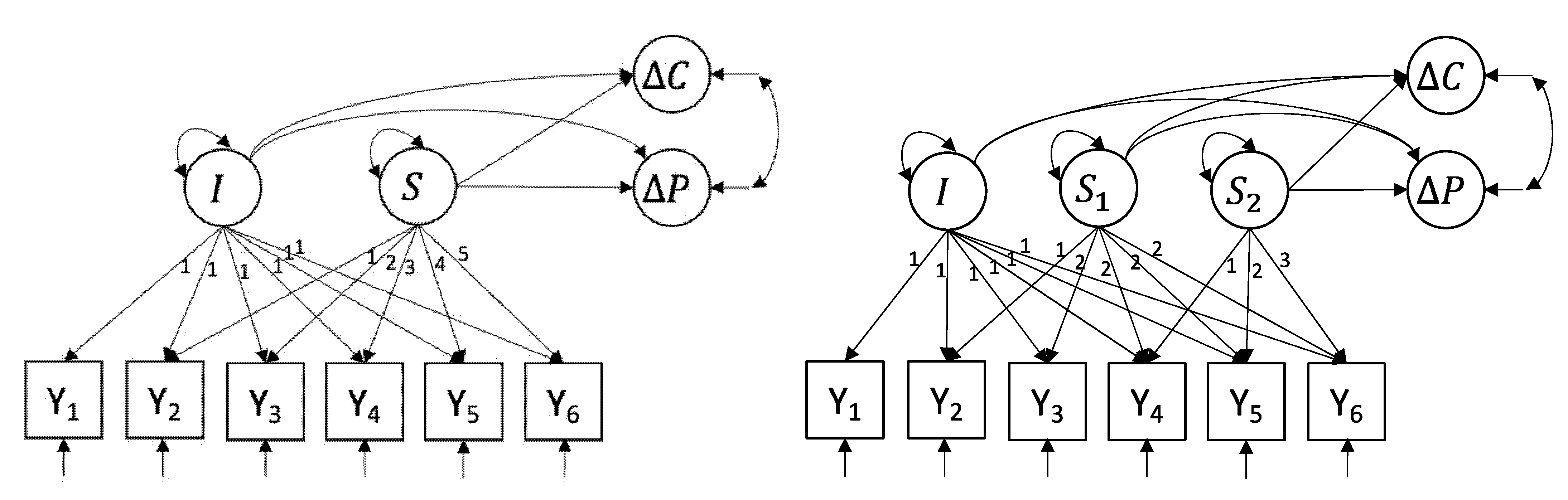
2.5. Data Analysis
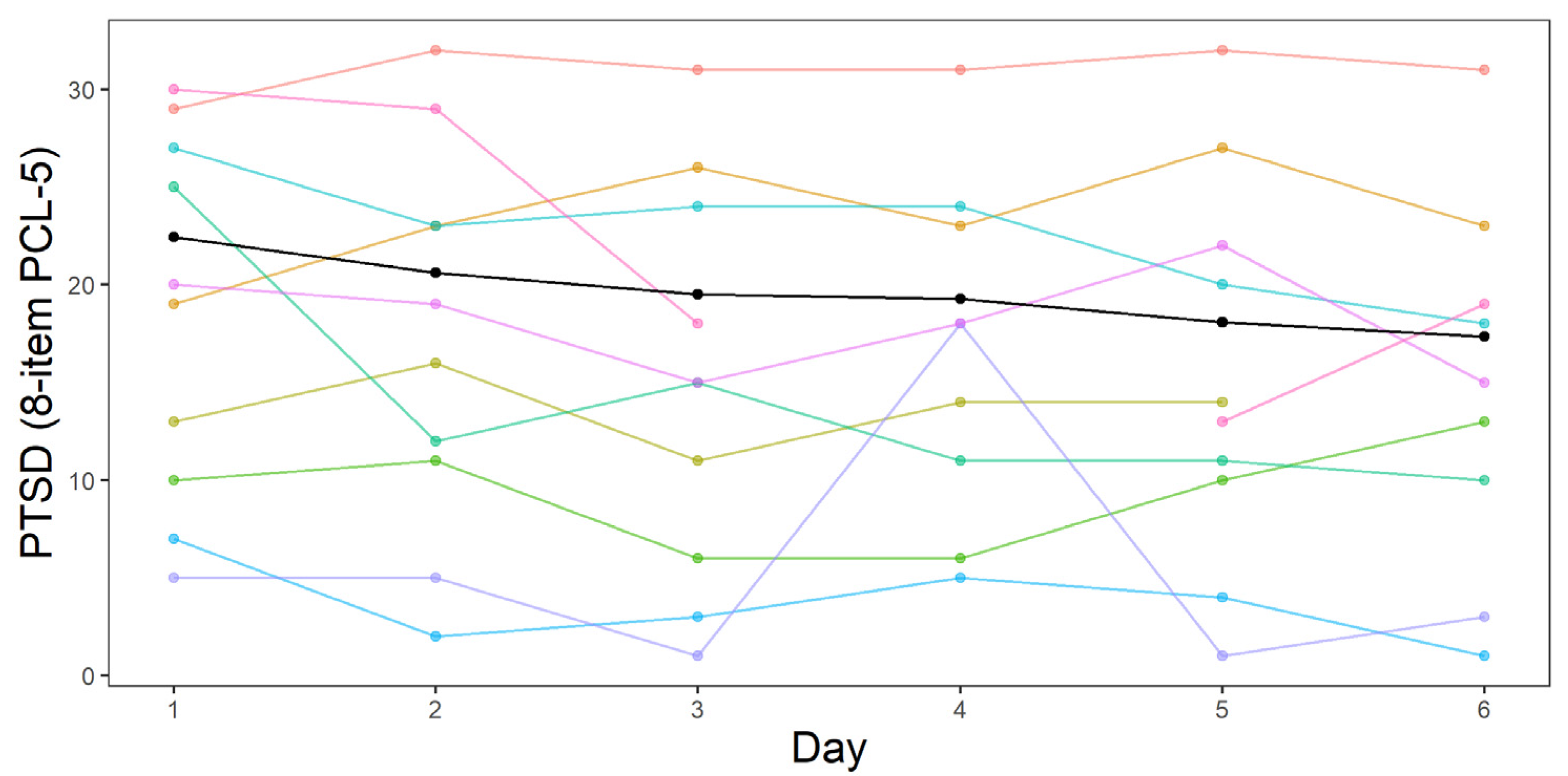
3. Results
3.1. The Linear LGCM (L-LGCM)
3.2. The Piecewise LGCM (P-LGCM)
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Kessler, R.C.; Petukhova, M.; Sampson, N.A.; Zaslavsky, A.M.; Wittchen, H.U. Twelve month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 2012, 21, 169–184. [Google Scholar] [CrossRef]
- De Vries, G.J.; Olff, M. The lifetime prevalence of traumatic events and posttraumatic stress disorder in the Netherlands. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2009, 22, 259–267. [Google Scholar] [CrossRef]
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults; American Psychiatric Association: Washington, DC, USA, 2017; Available online: https://www.apa.org/ptsd-guideline/ptsd.pdf (accessed on 28 May 2021).
- International Society of Traumatic Stress Studies (ISTSS). New ISTSS Prevention and Treatment Guidelines. 2018. Available online: http://www.istss.org/treating-trauma/new-istssguidelines.aspx (accessed on 28 May 2021).
- Lewis, C.; Roberts, N.P.; Andrew, M.; Starling, E.; Bisson, J.I. Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020, 11, 1729633. [Google Scholar] [CrossRef] [Green Version]
- Mavranezouli, I.; Megnin-Viggars, O.; Grey, N.; Bhutani, G.; Leach, J.; Daly, C.; Pilling, S. Cost-effectiveness of psychological treatments for post-traumatic stress disorder in adults. PLoS ONE 2020, 15, e0232245. [Google Scholar] [CrossRef]
- Imel, Z.E.; Laska, K.; Jakupcak, M.; Simpson, T.L. Meta-analysis of dropout in treatments for posttraumatic stress disorder. J. Consult. Clin. Psychol. 2013, 81, 394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schottenbauer, M.A.; Glass, C.R.; Arnkoff, D.B.; Tendick, V.; Gray, S.H. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry: Interpers. Biol. Process. 2008, 71, 134–168. [Google Scholar] [CrossRef] [PubMed]
- Bradley, R.; Greene, J.; Russ, E.; Dutra, L.; Westen, D. A multidimensional meta-analysis of psychotherapy for PTSD. Am. J. Psychiatry 2005, 162, 214–227. [Google Scholar] [CrossRef] [Green Version]
- Ehlers, A.; Clark, D.M.; Dunmore, E.; Jaycox, L.; Meadows, E.; Foa, E.B. Predicting response to exposure treatment in PTSD: The role of mental defeat and alienation. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 1998, 11, 457–471. [Google Scholar] [CrossRef] [PubMed]
- Forbes, D.; Creamer, M.; Hawthorne, G.; Allen, N.; McHugh, T. Comorbidity as a predictor of symptom change after treatment in combat-related posttraumatic stress disorder. J. Nerv. Ment. Dis. 2003, 191, 93–99. [Google Scholar] [CrossRef]
- Tarrier, N.; Sommerfield, C.; Pilgrim, H.; Faragher, B. Factors associated with outcome of cognitive-behavioural treatment of chronic post-traumatic stress disorder. Behav. Res. Ther. 2000, 38, 191–202. [Google Scholar] [CrossRef]
- Van Minnen, A.; Arntz, A.; Keijsers GP, J. Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behav. Res. Ther. 2002, 40, 439–457. [Google Scholar] [CrossRef]
- Karatzias, A.; Power, K.; McGoldrick, T.; Brown, K.; Buchanan, R.; Sharp, D.; Swanson, V. Predicting treatment outcome on three measures for post-traumatic stress disorder. Eur. Arch. Psychiatry Clin. Neurosci. 2007, 257, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Guina, J.; Rossetter, S.R.; DeRhodes, B.J.; Nahhas, R.W.; Welton, R.S. Benzodiazepines for PTSD: A systematic review and meta-analysis. J. Psychiatr. Pract. 2015, 21, 281–303. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, A.; Grey, N.; Wild, J.; Stott, R.; Liness, S.; Deale, A.; Manley, J. Implementation of cognitive therapy for PTSD in routine clinical care: Effectiveness and moderators of outcome in a consecutive sample. Behav. Res. Ther. 2013, 51, 742–752. [Google Scholar] [CrossRef] [Green Version]
- Horvath, A.O.; Symonds, B.D. Relation between working alliance and outcome in psychotherapy: A meta-analysis. J. Couns. Psychol. 1991, 38, 139. [Google Scholar] [CrossRef]
- Martin, D.J.; Garske, J.P.; Davis, M.K. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. J. Consult. Clin. Psychol. 2000, 68, 438. [Google Scholar] [CrossRef]
- Cooper, A.A.; Clifton, E.G.; Feeny, N.C. An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clin. Psychol. Rev. 2017, 56, 106–121. [Google Scholar] [CrossRef]
- Hendriks, L.; de Kleine, R.A.; Broekman, T.G.; Hendriks, G.J.; van Minnen, A. Intensive prolonged exposure therapy for chronic PTSD patients following multipletrauma and multiple treatment attempts. Eur. J. Psychotraumatol. 2018, 9, 1425574. [Google Scholar] [CrossRef] [Green Version]
- Foa, E.B.; Riggs, D.S.; Massie, E.D.; Yarczower, M. The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behav. Ther. 1995, 26, 487–499. [Google Scholar] [CrossRef]
- Jaycox, L.H.; Foa, E.B.; Morral, A.R. Influence of emotional engagement and habituation on exposure therapy for PTSD. J. Consult. Clin. Psychol. 1998, 66, 185. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Bae, H.; Park, Y.C. Validity of the subjective units of disturbance scale in EMDR. J. EMDR Pract. Res. 2008, 2, 57–62. [Google Scholar] [CrossRef]
- Tuerk, P.W.; Yoder, M.; Grubaugh, A.; Myrick, H.; Hamner, M.; Acierno, R. Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. J. Anxiety Disord. 2011, 25, 397–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nijdam, M.J.; Gersons, B.P.; Reitsma, J.B.; de Jongh, A.; Olff, M. Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing therapy for post-traumatic stress disorder: Randomised controlled trial. Br. J. Psychiatry 2012, 200, 224–231. [Google Scholar] [CrossRef] [Green Version]
- Sripada, R.K.; Ready, D.J.; Ganoczy, D.; Astin, M.C.; Rauch, S.A. When to change the treatment plan: An analysis of diminishing returns in VA patients undergoing prolonged exposure and cognitive processing therapy. Behav. Ther. 2020, 51, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Byllesby, B.M.; Dickstein, B.D.; Chard, K.M. The probability of change versus dropout in veterans receiving cognitive processing therapy for posttraumatic stress disorder. Behav. Res. Ther. 2019, 123, 103483. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, A.; Hackmann, A.; Grey, N.; Wild, J.; Liness, S.; Albert, I.; Clark, D.M. A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. Am. J. Psychiatry 2014, 171, 294–304. [Google Scholar] [CrossRef] [Green Version]
- Ragsdale, K.A.; Watkins, L.E.; Sherrill, A.M.; Zwiebach, L.; Rothbaum, B.O. Advances in PTSD treatment delivery: Evidence base and future directions for intensive outpatient programs. Curr. Treat. Options Psychiatry 2020, 7, 291–300. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Vancampfort, D.; Steel, Z.; Newby, J.; Ward, P.B.; Stubbs, B. Physical activity in the treatment of post-traumatic stress disorder: A systematic review and meta analysis. Psychiatry Res. 2015, 230, 130–136. [Google Scholar] [CrossRef]
- Van Woudenberg, C.; Voorendonk, E.M.; Bongaerts, H.; Zoet, H.A.; Verhagen, M.; Lee, C.W.; De Jongh, A. Effectiveness of an intensive treatment programme combining prolonged exposure and eye movement desensitization and reprocessing for severe post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1487225. [Google Scholar] [CrossRef]
- Foa, E.B.; Hembree, E.A.; Rothbaum, B.O. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide; Oxford University Press: New York, NY, USA, 2007. [Google Scholar]
- De Jongh, A.; Ten Broeke, E. Handboek EMDR: Een Geprotocolleerde Behandelmethode Voor de Gevolgen Van Psychotrauma; Pearson Assessment and Information B.V.: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Shapiro, F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures, 2nd ed.; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- Van Minnen, A.; Voorendonk, E.M.; Rozendaal, L.; de Jongh, A. Sequence matters: Combining Prolonged Exposure and EMDR therapy for PTSD. Psychiatry Res. 2020, 290, 113032. [Google Scholar] [CrossRef]
- Van Minnen, A.; Hendriks, L.; Kleine, R.D.; Hendriks, G.J.; Verhagen, M.; De Jongh, A. Therapist rotation: A novel approach for implementation of trauma-focused treatment in post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1492836. [Google Scholar] [CrossRef] [Green Version]
- Emerson, D.; Sharma, R.; Chaudhry, S.; Turner, J. Trauma-sensitive yoga: Principles, practice, and research. Int. J. Yoga Ther. 2009, 19, 123–128. [Google Scholar] [CrossRef]
- Nolan, C.R. Bending without breaking: A narrative review of trauma-sensitive yoga for women with PTSD. Complementary Ther. Clin. Pract. 2016, 24, 32–40. [Google Scholar] [CrossRef]
- Boeschoten, M.A.; Bakker, A.; Jongedijk, R.A.; van Minnen, A.; Elzinga, B.M.; Rademaker, A.R.; Olff, M. Clinician Administered PTSD Scale for DSM-5—Nederlandstalige Versie Uitgave; Arq Psychotrauma Expert Groep: Diemen, The Netherlands, 2014. [Google Scholar]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5); National Center for PTSD: Boston, MA, USA, 2013.
- Boeschoten, M.A.; Van der Aa, N.; Bakker, A.; Ter Heide FJ, J.; Hoofwijk, M.C.; Jongedijk, R.A.; Olff, M. Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). Eur. J. Psychotraumatol. 2018, 9, 1546085. [Google Scholar] [CrossRef]
- Boeschoten, M.A.; Bakker, A.; Jongedijk, R.A.; Olff, M. PTSD Checklist for the DSM-5—Nederlandstalige Versie Uitgave; Arq Psychotrauma Expert Groep: Diemen, The Netherlands, 2014. [Google Scholar]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5); National Center for PTSD: Boston, MA, USA, 2013.
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Price, M.; Szafranski, D.D.; van Stolk-Cooke, K.; Gros, D.F. Investigation of abbreviated 4 and 8 item versions of the PTSD Checklist 5. Psychiatry Res. 2016, 239, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Meredith, W.; Tisak, J. Latent curve analysis. Psychometrika 1990, 55, 107–122. [Google Scholar] [CrossRef]
- Rosseel, Y. Lavaan: An R package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2019; Available online: https://www.r-project.org/ (accessed on 8 February 2021).
- AKWA. Zorgstandaard Psychotrauma- en Stressorgerelateerde Stoornissen. 2020. Available online: https://www.ggzstandaarden.nl/zorgstandaarden/psychotrauma-en-stressorgerelateerdestoornissen (accessed on 28 May 2021).
- Blake, D.; Weathers, F.; Nagy, L.; Kaloupek, D.; Klauminzer, G.; Charney, D.; Keane, T. Clinician-Administered PTSD Scale (CAPS); National Center for Post-Traumatic Stress Disorder: Boston, MA, USA, 1990.
- Davidson, J.; Smith, R.; Kudler, H. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder: Experience with a structured interview. J. Nerv. Ment. Dis. 1989, 177, 336–341. [Google Scholar] [CrossRef] [PubMed]
| Activity | Duration (Minutes) |
|---|---|
| Pre-treatment Measurement (only on the first day) | 45 |
| Prolonged Exposure | 90 |
| Short Break | 15 |
| Physical Activity (yoga, exercises, running) | 60 |
| Lunch Break | 30–45 |
| EMDR | 90 |
| Short Break | 15 |
| Psycho-education | 60 |
| Measurements (Last treatment day) | 45 |
| Variable | N | M | SD | Min. | Max. |
|---|---|---|---|---|---|
| 89 | −22.05 1 | 19.61 | −69 2 | +12 2 | |
| 99 | −17.29 | 15.47 | −53 2 | +14 2 | |
| 8-item PCL–Day 1 | 107 | 22.49 | 35.54 | 5 | 32 |
| 8-item PCL–Day 2 | 105 | 20.60 | 40.64 | 2 | 32 |
| 8-item PCL–Day 3 | 102 | 19.52 | 48.45 | 1 | 32 |
| 8-item PCL–Day 4 | 106 | 19.29 | 45.09 | 0 | 32 |
| 8-item PCL–Day 5 | 102 | 18.08 | 48.35 | 1 | 32 |
| 8-item PCL–Day 6 | 96 | 17.37 | 55.25 | 1 | 31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alting van Geusau, V.V.P.; Mulder, J.D.; Matthijssen, S.J.M.A. Predicting Outcome in an Intensive Outpatient PTSD Treatment Program Using Daily Measures. J. Clin. Med. 2021, 10, 4152. https://doi.org/10.3390/jcm10184152
Alting van Geusau VVP, Mulder JD, Matthijssen SJMA. Predicting Outcome in an Intensive Outpatient PTSD Treatment Program Using Daily Measures. Journal of Clinical Medicine. 2021; 10(18):4152. https://doi.org/10.3390/jcm10184152
Chicago/Turabian StyleAlting van Geusau, Valentijn V. P., Jeroen D. Mulder, and Suzy J. M. A. Matthijssen. 2021. "Predicting Outcome in an Intensive Outpatient PTSD Treatment Program Using Daily Measures" Journal of Clinical Medicine 10, no. 18: 4152. https://doi.org/10.3390/jcm10184152
APA StyleAlting van Geusau, V. V. P., Mulder, J. D., & Matthijssen, S. J. M. A. (2021). Predicting Outcome in an Intensive Outpatient PTSD Treatment Program Using Daily Measures. Journal of Clinical Medicine, 10(18), 4152. https://doi.org/10.3390/jcm10184152





