Analysis of Muscle Activity Following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial
Abstract
:1. Introduction
2. Study Objective
3. Methods
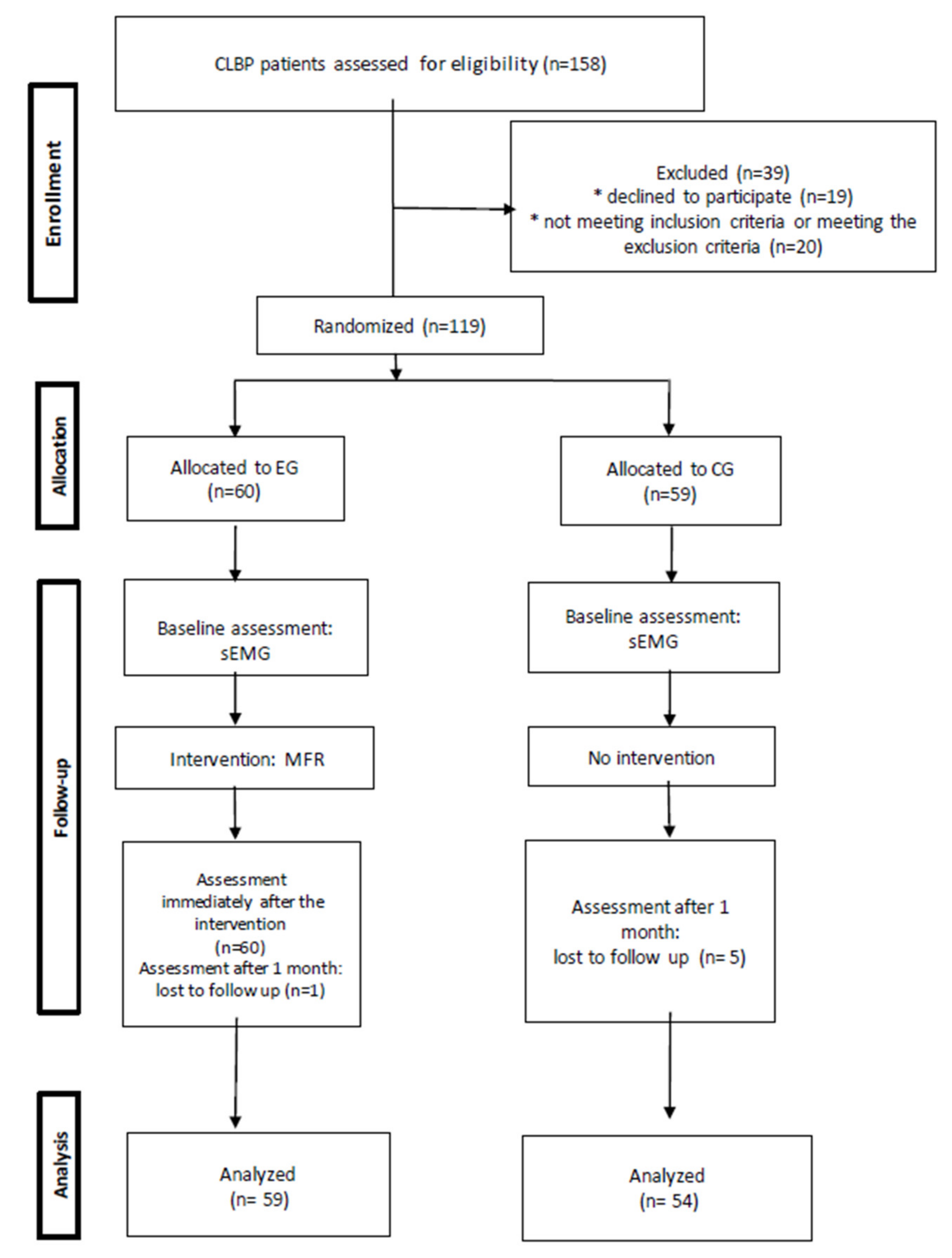
3.1. Study Design
- Age 40–60 years;
- Chronic low-back pain (lasting more than 3 months).
- Neurological conditions, previous surgical treatment, spine injury, contraindications to MFR treatment (acute inflammations, viral and bacterial infections, infectious diseases, fever, deep vein thrombosis, active malignant disease, aneurysms), contraindications to surface electromyography (sEMG) exam (pacemaker, artificial heart valve);
- Physiotherapeutic interventions in the last 6 months;
- The following coexisting conditions—cancer, diabetes, osteoporosis, pregnancy; digestive system, cardiovascular system, rheumatic, psychic, and gynaecological diseases.
- The slump test;
- The Babinski test and ankle clonus test;
- Sciatic nerve tests (straight leg raise and bowstring test), femoral nerve test (in the supine lying position and side-lying position);
- Knee and ankle reflexes test, strength testing of indicator muscles in the lumbosacral spine;
- Evaluation of exteroceptive sensation along dermatomes associated with lumbosacral nerve roots.
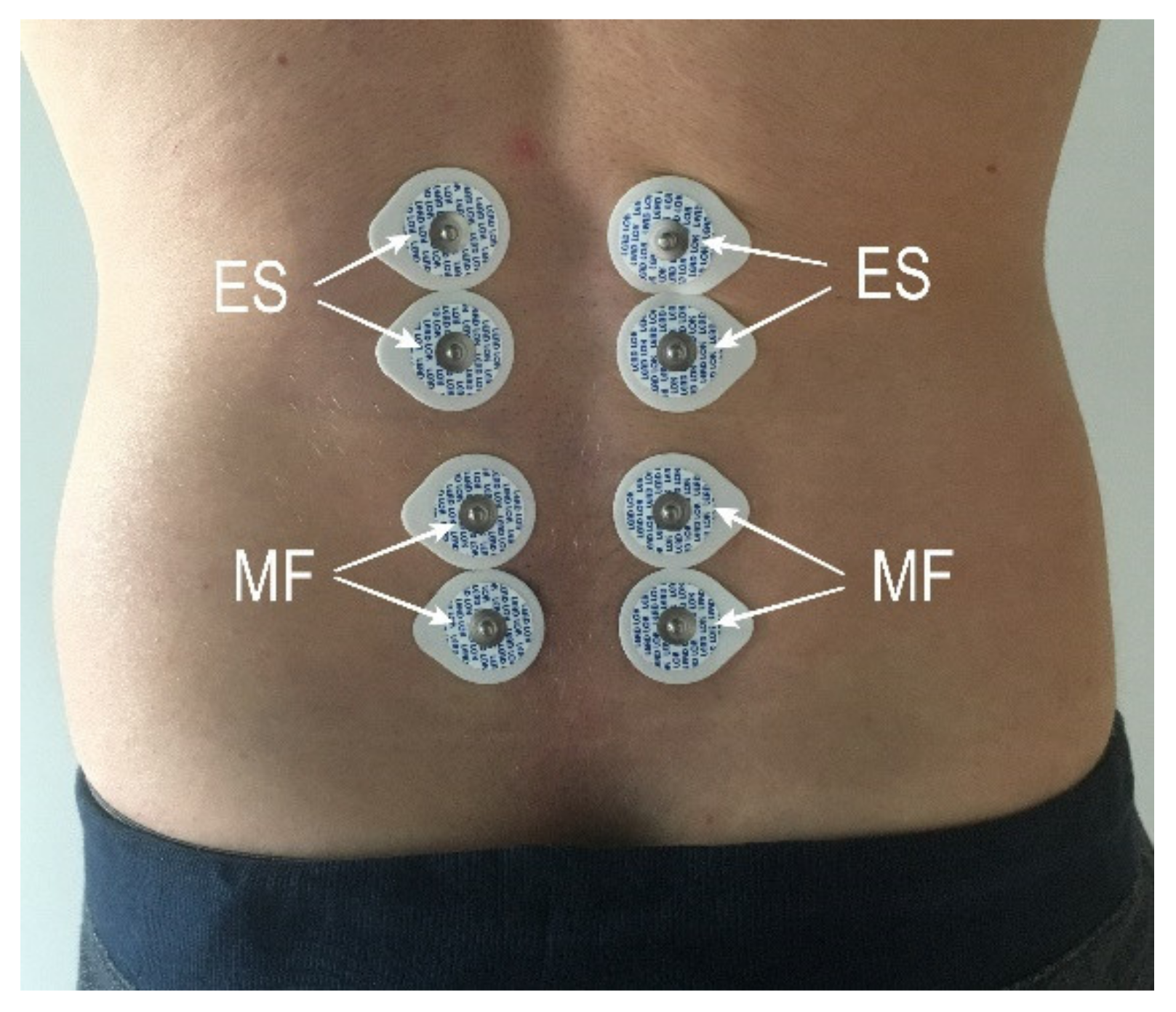
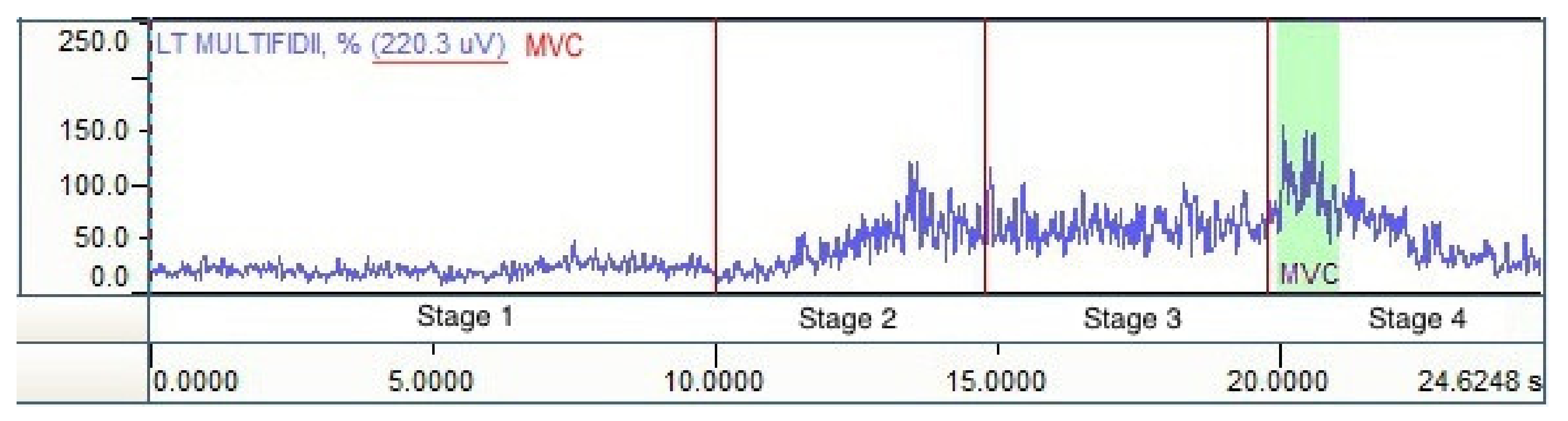
3.2. Measurements
- Assessment of the resting activity in a relaxed standing position (10 s);
- Trunk flexion (forward bend) within available range of motion performed with knee extension (5 s);
- Maintaining trunk flexion with knee extension and relaxed shoulder girdle and upper limbs (5 s);
- Returning to a standing position—trunk extension (5 s).
3.3. Intervention
3.4. Statistical Analyses
4. Results
5. Discussion
6. Conclusions
- A single MFR treatment in a group of patients with CLBP immediately decreases resting activity of the erector spinae and multifidus muscles in the lumbodorsal spine area. The comparison of the results with those of the control group results reveal that the effects are definitely stronger for the multifidus muscle.
- Data collected a month after the treatment confirm maintenance of the treatment effect in terms of muscular activity of the erector spinae and multifidus muscles in the lumbosacral spine.
7. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DePalma, M.J.; Ketchum, J.M.; Saullo, T. What is the source of Chronic Low Back Pain and does age Play a Role? Pain Med. 2011, 12, 224–233. [Google Scholar] [CrossRef] [Green Version]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [Green Version]
- Tesarz, J.; Hoheisel, U.; Wiedenhofer, B.; Mense, S. Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience 2011, 194, 302–308. [Google Scholar] [CrossRef]
- Schleip, R.; Findley, T.W.; Chaitow, L.; Huijing, P.A. Fascia: The Tensional Network of the Human Body: The Science and Clinical Applications in Manual and Movement Therapy, 1st ed.; Elsevier: London, UK, 2012; pp. 93–121. [Google Scholar]
- Langevin, H.M.; Fox, J.R.; Koptiuch, C.; Badger, G.J.; Greenan-Naumann, A.C.; Bouffard, N.A.; Konofagou, E.E.; Lee, W.N.; Triano, J.J.; Henry, S.M. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskelet. Disord. 2011, 12, 203. [Google Scholar] [CrossRef] [PubMed]
- Ranger, T.A.; Teichtahl, A.J.; Cicuttini, F.M.; Wang, Y.; Wluka, A.E.; O Sullivan, R.; Jones, G.; Urquhart, D.M. Shorter Lumbar Paraspinal Fascia Is Associated With High Intensity Low Back Pain and Disability. Spine 2016, 41, 489–493. [Google Scholar] [CrossRef] [Green Version]
- Panjabi, M.M. A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction. Eur. Spine J. 2006, 15, 668–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mense, S. Innervation of the thoracolumbar fascia. Eur. J. Transl. Myol. 2019, 29, 151–158. [Google Scholar] [CrossRef]
- Stecco, C.; Stern, R.; Porzionato, A.; Macchi, V.; Masiero, S.; Stecco, A.; De Caro, R. Hyaluronan within fascia in the etiology of myofascial pain. Surg. Radiol. Anat. 2011, 33, 891–896. [Google Scholar] [CrossRef]
- Geisser, M.E. Surface Electromyography and Low Back Pain. Biofeedback 2007, 35, 13–16. [Google Scholar]
- Geisser, M.E.; Ranavaya, M.; Haig, A.J.; Roth, R.S.; Zucker, R.; Ambroz, C.; Caruso, M. A meta- analytic review of surface electromyography among persons with low back pain and normal, healthy controls. J. Pain. 2005, 6, 711–726. [Google Scholar] [CrossRef]
- Coppeta, L.; Gentili, S.; Mugnaini, S.; Balbi, O.; Massimiani, S.; Armieri, G.; Pietroiusti, A.; Magrini, A. Neuromuscular Functional Assessment in Low Back Pain by Surface Electromyography (SEMG). Open Public Health J. 2019, 12, 61–67. [Google Scholar] [CrossRef]
- Luchau, T. Advanced Myofascial Techniques–Volume 2: Neck, Head, Spine and Ribs, 1st ed.; Handspring Publishing Limited: Fountainhall, UK, 2017; pp. 3–29. [Google Scholar]
- Riggs, A. Deep Tissue Massage, Revised Edition: A Visual Guide to Techniques; North Atlantic Books: Berkeley, CA, USA, 2007. [Google Scholar]
- Earls, J.; Myers, T.W. Fascial Release for Structural Balance; Lotus Publishing: Chichester, UK, 2017; pp. 25–48. [Google Scholar]
- Diallo, S.; Cour, F.; Josephson, A.; Vidart, A.; Botto, H.; Lebret, T.; Bonan, B. Evaluating single- incision slings in female stress urinary incontinence: The usefulness of the CONSORT statement criteria. Urology 2012, 80, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Freriks, B.; Hermens, H.J. SENIAM 9: European Recommendations for Surface ElectroMyoGraphy, Results of the SENIAM Project; Roessingh Research and Development: Enschede, The Netherlands, 1999. [Google Scholar]
- Merletti, R.; Farina, D. Surface Electromyography: Physiology, Engineering, and Applications; Wiley-IEEE Press: Hoboken, NJ, USA, 2016. [Google Scholar]
- Chowdhury, R.H.; Reaz, M.B.I.; Ali, M.A.B.M.; Bakar, A.A.A.; Chellappan, K.; Chang, T.G. Surface Electromyography Signal Processing and Classification Techniques. Sensors 2013, 13, 12431–12466. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.W. Anatomy Trains. Myofascial Meridians for Manual and Movement Therapist, 2nd ed.; Churchill Livingstone Elsevier: London, UK, 2009; pp. 13–65. [Google Scholar]
- Manheim, C.J.; Lavett, D.K. The Myofascial Release Manual, 4th ed.; SLACK, Inc.: Thorofare, NJ, USA, 2008. [Google Scholar]
- Bürkner, P.C. Brms: An R Package for Bayesian Multilevel Models Using Stan. J. Stat. Softw. 2017, 80, 1–28. [Google Scholar] [CrossRef] [Green Version]
- Vehtari, A.; Gelman, A.; Gabry, J. Practical Bayesian model evaluation using leave-one- out cross-validation and WAIC. Stat. Comput. 2017, 27, 1413–1432. [Google Scholar] [CrossRef] [Green Version]
- Burnham, K.; Anderson, D. Model Selection and Multi-Model Inference; Springer: New York, NY, USA, 2002. [Google Scholar]
- Gelman, A.; Goodrich, B.; Gabry, J.; Vehtari, A. R-squared for Bayesian Regression Models. Am. Stat. 2018, 73, 1–6. [Google Scholar] [CrossRef]
- Willard, F.H.; Vleeming, A.; Schuenke, M.D.; Danneels, L.; Schleip, R. The thoracolumbar fascia anatomy, function and clinical conoideratrions. J. Anat. 2012, 221, 507–536. [Google Scholar] [CrossRef] [Green Version]
- Schleip, R.; Vleeming, A.; Lehmann-Horn, F.; Klinger, W. Letter to the Editor concerning ‘A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction’ (M. Panjabi). Eur. Spine J. 2007, 16, 1733–1735. [Google Scholar] [CrossRef] [Green Version]
- Schleip, R.; Klingler, W.; Lehmann-Horn, F. Active fascial contractility: Fascia may be able to contract in a smooth muscle-like manner and thereby influence musculoskeletal dynamics. Med. Hypotheses. 2005, 65, 273–277. [Google Scholar] [CrossRef]
- Stecco, A.; Gesi, M.; Stecco, C.; Stern, R. Fascial components of the myofascial pain syndrome. Curr. Pain. Headache Rep. 2013, 17, 352. [Google Scholar] [CrossRef]
- Pavan, P.G.; Stecco, A.; Stern, R.; Stecco, C. Painful connections: Densification versus fibrosis of fascia. Curr. Pain. Headache Rep. 2014, 18, 441. [Google Scholar] [CrossRef]
- Marizeiro, D.F.; Florêncio, A.C.L.; Nunes, A.C.L.; Campos, N.G.; Lima, P.O.P. Immediate effects of diaphragmatic myofascial release on the physical and functional outcomes in sedentary women: A randomized placebo-controlled trial. J. Bodyw. Mov. Ther. 2018, 22, 924–929. [Google Scholar] [CrossRef]
- Tozzi, P.; Bongiorno, D.; Vitturini, C. Fascial release effects on patients with non-specific cervical or lumbar pain. J. Bodyw. Mov. Ther. 2011, 15, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Chai, H.M.; Shau, Y.W.; Wang, C.L.; Wang, S.F. Increased sliding of transverse abdominis during contraction after myofascial release in patients with chronic low back pain. Man. Ther. 2016, 23, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Shah, Y.; Arkesteijn, M.; Thomas, D.; Whyman, J.; Passfield, L. The acute effects of integrated myofascial techniques on lumbar paraspinal blood flow compared with kinesio-taping: A pilot study. J. Bodyw. Mov. Ther. 2017, 21, 459–467. [Google Scholar] [CrossRef] [Green Version]
- Arguisuelas, M.D.; Lisón, J.F.; Doménech-Fernández, J.; Martínez-Hurtado, I.; Salvador Coloma, P.; Sánchez-Zuriaga, D. Effects of myofascial release in erector spinae myoelectric activity and lumbar spine kinematics in non-specific chronic low back pain: Randomized controlled trial. Clin. Biomech. 2019, 63, 27–33. [Google Scholar] [CrossRef] [PubMed]



| Dependent Variable | Model | LOOIC/KFOLDIC | Dependent Variable 2 | R-Squared EG | Total R-Squared |
|---|---|---|---|---|---|
| MVC | null model | −1945 | MF left | - | - |
| MF right | |||||
| ES left | |||||
| ES right | |||||
| measurement | −1956 | MF left | 0.02 [0.01, 0.05] | 0.74 [0.64, 0.80] | |
| MF right | 0.02 [0, 0.05] | 0.58 [0.43, 0.69] | |||
| ES left | 0.02 [0, 0.05] | 0.62 [0.52, 0.70] | |||
| ES right | 0.05 [0.02, 0.09] | 0.69, [0.62, 0.74] |
| Dependent Variable | Model | LOOIC/KFOLDIC | Dependent Variable 2 | R-Squared EG | total R-Squared |
|---|---|---|---|---|---|
| MVC (kfold) | null model | −1865 | MF left | - | - |
| MF right | |||||
| ES left | |||||
| ES right | |||||
| EG | −1859 | MF left | 0.06 [0.01, 0.13] | 0.73 [0.63, 0.80] | |
| MF right | 0.04 [0, 0.11] | 0.58 [0.43, 0.70] | |||
| ES left | 0.01 [0, 0.04] | 0.63 [0.52, 0.72] | |||
| ES right | 0.02 [0, 0.06] | 0.67 [0.58, 0.73] | |||
| EGI | −1880 | MF left | 0.07 [0.02, 0.14] | 0.75 [0.67, 0.82] | |
| MF right | 0.06 [0.02, 0.12] | 0.60 [0.46, 0.72] | |||
| ES left | 0.02 [0, 0.06] | 0.64 [0.53, 0.73] | |||
| ES right | 0.03 [0.01, 0.07] | 0.68 [0.6, 0.74] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ożóg, P.; Weber-Rajek, M.; Radzimińska, A.; Goch, A. Analysis of Muscle Activity Following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial. J. Clin. Med. 2021, 10, 4039. https://doi.org/10.3390/jcm10184039
Ożóg P, Weber-Rajek M, Radzimińska A, Goch A. Analysis of Muscle Activity Following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial. Journal of Clinical Medicine. 2021; 10(18):4039. https://doi.org/10.3390/jcm10184039
Chicago/Turabian StyleOżóg, Piotr, Magdalena Weber-Rajek, Agnieszka Radzimińska, and Aleksander Goch. 2021. "Analysis of Muscle Activity Following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial" Journal of Clinical Medicine 10, no. 18: 4039. https://doi.org/10.3390/jcm10184039
APA StyleOżóg, P., Weber-Rajek, M., Radzimińska, A., & Goch, A. (2021). Analysis of Muscle Activity Following the Application of Myofascial Release Techniques for Low-Back Pain—A Randomized-Controlled Trial. Journal of Clinical Medicine, 10(18), 4039. https://doi.org/10.3390/jcm10184039






