The ISJ 3D Brace, a Providence Brace Evolution, as a Surgery Prevention Method in Idiopathic Scoliosis
Abstract
1. Introduction
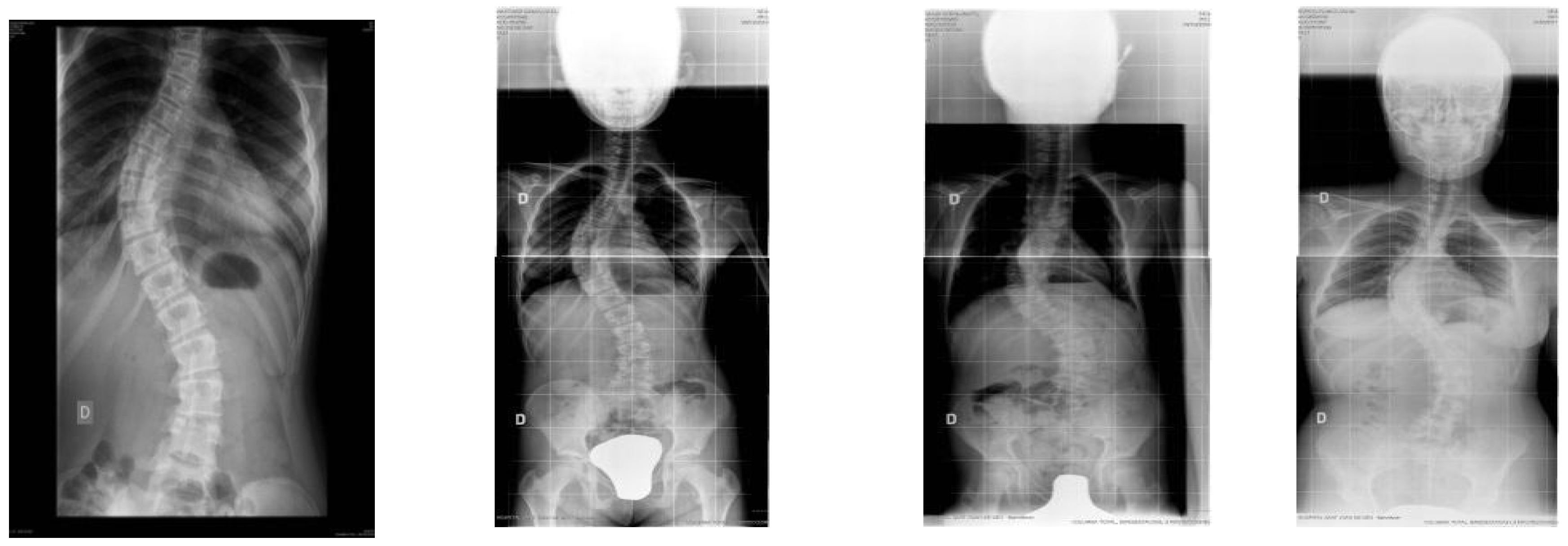
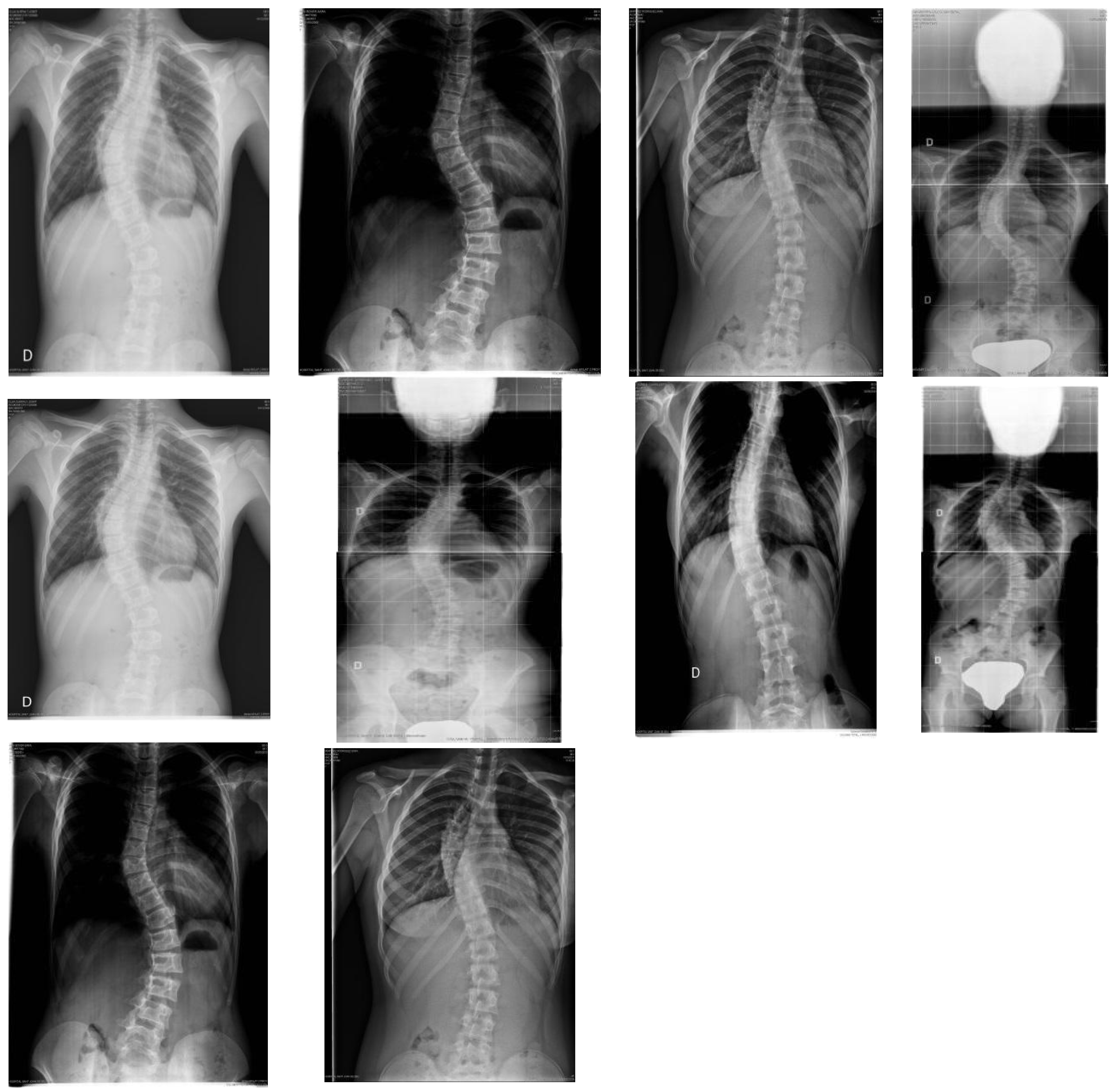
2. Materials and Methods
2.1. Design and Study Sample
2.2. Procedure
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lo, Y.F.; Huang, Y.C. Bracing in adolescent idiopathic scoliosis. J. Nurs. 2017, 64, 117–123. [Google Scholar] [CrossRef]
- Cobb, J.R. Outline for the study os scoliosis. Instr. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Horne, J.P.; Flannery, R.; Usman, S. Adolescent Idiopathic Scoliosis: Diagnosis and Management. Am. Fam. Physician 2014, 89, 193–198. [Google Scholar]
- Choudhry, M.N.; Ahmad, Z.; Verma, R. Adolescent Idiopathic Scoliosis. Open Orthop. J. 2016, 10, 143–154. [Google Scholar] [CrossRef]
- Kuznia, A.L.; Hernandez, A.K.; Lee, L.U. Adolescent Idiopathic Scoliosis: Common Questions and Answers. Am. Fam. Physician 2020, 101, 19–23. [Google Scholar]
- Ylikoski, M. Growth and progression of adolescent idiopathic scoliosis in girls. J. Pediatr. Orthop. 2005, 14, 320–324. [Google Scholar] [CrossRef]
- Zhu, Z.; Xu, L.; Jiang, L.; Sun, X.; Qiao, J.; Qian, B.-P.; Mao, S.; Qiu, Y. Is Brace Treatment Appropriate for Adolescent Idiopathic Scoliosis Patients Refusing Surgery with Cobb Angle Between 40 and 50 Degrees. Clin. Spine Surg. 2017, 30, 85–89. [Google Scholar] [CrossRef]
- Roach, J.W. Adolescent idiopathic scoliosis. Orthop. Clin. North Am. 1999, 30, 353–365. [Google Scholar] [CrossRef]
- Hacquebord, J.H.; Leopold, S.S. In brief: The Risser Classification: A classic tool for the clinician trating Adolescent Idiopathic Scoliosis. Clin. Orthop. Relat. Res. 2012, 470, 2335–2338. [Google Scholar] [CrossRef]
- Kotwicki, T.; Chowanska, J.; Kinel, E.; Czaprowski, D.; Janusz, P.; Tomaszewski, M. Optimal management of idiopathic scoliosis in adolescence. Adolesc. Health Med. Ther. 2013, 4, 59–73. [Google Scholar] [CrossRef][Green Version]
- Pham, V.M.; Herbaux, B.; Schill, A.; Thevenon, A. Evaluation of the Chêneau brace in adolescent idiopathic scoliosis. Ann. Readapt. Med. Phys. 2007, 50, 125–133. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Aulisa, L.; Circo, A.B.; De Mauroy, J.C.; Durmala, J.; Grivas, T.B.; Knott, P.; Kotwicki, T.; Maruyama, T.; et al. 2011 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012, 7, 3. [Google Scholar] [CrossRef]
- Kwiatkowski, M.; Mnich, K.; Karpiński, M.; Domański, K.; Milewski, R.; Popko, J. Assessment of Idiopathic Scoliosis Patients’ Satisfaction with Thoracolumbar Brace Treatment. Ortop. Traumatol. Rehabil. 2015, 17, 111–119. [Google Scholar] [CrossRef]
- Dickson, J.; Mirkovic, S.; Noble, P.; Nalty, T.; Erwin, W. Results of operative treatment of Idiopathic Scoliosis in Adults. J. Bone Jt. Surg. 1998, 77, 513–523. [Google Scholar] [CrossRef]
- Rożek, K.; Potaczek, T.; Zarzycka, M.; Lipik, E.; Jasiewicz, B. Effectiveness of Treatment of Idiopathic Scoliosis by SpineCor Dynamic Bracing with Special Physiotherapy Programme in SpineCor System. Ortop. Traumatol. Rehabil. 2016, 18, 425–434. [Google Scholar] [CrossRef]
- Yrjönen, T.; Ylikoski, M.; Schlenzka, D.; Kinnunen, R.; Poussa, M. Effectiveness of the Providence nighttime bracing in adolescent idiopathic scoliosis: A comparative study of 36 female patients. Eur. Spine J. 2006, 15, 1139–1143. [Google Scholar] [CrossRef]
- Miller, D.J.; Franzone, J.M.; Matsumoto, H.; Gomez, J.A.; Avendaño, J.; Hyman, J.E.; Roye, D.P., Jr.; Vitale, M.G. Electronic Monitoring Improves Brace-Wearing Compliance in Patients with Adolescent Idiopathic Scoliosis: A randomized clinical trial. Spine 2012, 37, 717–721. [Google Scholar] [CrossRef]
- Rahman, T.; Sample, W.; Yorgova, P.; Neiss, G.; Rogers, K.; Shah, S.; Gabos, P.; Kritzer, D.; Bowen, J.R. Electronic monitoring of orthopedic brace compliance. J. Child. Orthop. 2015, 9, 365–369. [Google Scholar] [CrossRef]
- Chalmers, E.; Lou, E.; Hill, D.; Zhao, H.V. An advanced compliance monitor for patients undergoing brace treatment for idiopathic scoliosis. Med. Eng. Phys. 2015, 37, 203–209. [Google Scholar] [CrossRef]
- Lou, E.; Hill, D.; Hedden, D.; Mahood, J.; Moreau, M.; Raso, J. An objective measurement of brace usage for the treatment of adolescent idiopathic scoliosis. Med. Eng. Phys. 2011, 33, 290–294. [Google Scholar] [CrossRef]
- Morton, A.; Riddle, R.; Buchanan, R.; Katz, D.; Birch, J. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2008, 28, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Helfenstein, A.; Lankes, M.; Öhlert, K.; Varoga, D.; Hahne, H.-J.; Ulrich, H.W.; Hassenpflug, J. The Objective Determination of Compliance in Treatment of Adolescent Idiopathic Scoliosis with Spinal Orthoses. Spine 2006, 31, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, G.P.; Ferguson-Pell, M.W.; Smith, K.; Edgar, M.; Morley, T. The Objective Measurement of Spinal Orthosis Use for the Treatment of Adolescent Idiopathic Scoliosis. Spine 2003, 28, 2243–2250. [Google Scholar] [CrossRef] [PubMed]
- Simony, A.; Beuschau, I.; Quisth, L.; Jespersen, S.M.; Carreon, L.Y.; Andersen, M.O. Providence nighttime bracing is effective in treatment for adolescent idiopathic scoliosis even in curves larger than 35°. Eur. Spine J. 2019, 28, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- González Vicente, L. El Corsé Nocturno ISJ 3D en el Tratamiento de las Escoliosis; Tesis Ciencias de la Salud: Burgos, Spain, 2017. [Google Scholar] [CrossRef]
- Stokes, I.A. Analysis and simulation of progressive adolescent scoliosis by biomechanical growth modulation. Eur. Spine J. 2007, 16, 1621–1628. [Google Scholar] [CrossRef]
- Grivas, T.B.; Rodopoulos, G.I.; Bardakos, N.V. Night-time braces for treatment of Adolescent Idiopathic Scoliosis. Disabil. Rehabil. Assist. Technol. 2009, 3, 120–129. [Google Scholar] [CrossRef]
- Grivas, T.B.; Rodopoulos, G.I.; Bardakos, N.V. Biomechanical and clinical perspectives on nighttime bracing for adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2008, 135, 279–290. [Google Scholar]
- Zambudio Periago, R. Prótesis, Ortesis y Ayudas Técnicas, 1st ed.; Elsevier Masson: Issy-les-Moulineaux, France, 2009. [Google Scholar]
- Langensiepen, S.; Semler, O.; Sobottke, R.; Fricke, O.; Franklin, J.; Schönau, E.; Eysel, P. Measuring procedures to determine the Cobb angle in idiopathic scoliosis: A systematic review. Eur. Spine J. 2013, 22, 2360–2371. [Google Scholar] [CrossRef]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2018, 13, 3. [Google Scholar] [CrossRef]
- Buendía, M.; Salvador, R.; Cibrián, R.; Laguia, M.; Sotoca, J.M. Determination of the object surface function by structured light: Application to the study of spinal deformities. Phys. Med. Biol. 1999, 44, 75–86. [Google Scholar] [CrossRef]
- Reamy, B.V.; Slakey, J.B. Adolescent Idiopathic Scoliosis: Review and Current Concepts. Am. Fam. Physician 2001, 64, 111–117. [Google Scholar] [PubMed]
- Negrini, S.; Negrini, F.; Fusco, C.; Zaina, F. Idiopathic scoliosis patients with curves more than 45 Cobb degrees refusing surgery can be effectively treated through bracing with curve improvements. Spine J. 2011, 11, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Edwards, C.C.; Bridwell, K.H. The Lenke classification of adolescent idiopathic scoliosis: How it organizes curve patterns as a template to perform selective fusions of the spine. Spine 2003, 28, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Takemitsu, M.; Bowen, J.R.; Rahman, T.; Glutting, J.J.; Scott, C.B. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine 2004, 29, 2070–2074. [Google Scholar] [CrossRef]
- Schulte, T.L.; Thielsch, M.T.; Gosheger, G.; Boertz, P.; Terheyden, J.H.; Wetterkamp, M. German validation of the quality of life profile for spinal disorders (QLPSD). Eur. Spine J. 2018, 27, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Pham, V.M.; Houlliez, A.; Carpentier, A.; Herbaux, B.; Schill, A.; Thevenon, A. Determination of the influence of the Chêneau brace on the quality of life of adolescents with idiopathic scoliosis. Ann. Readapt. Med. Phys. 2008, 51, 3–15. [Google Scholar] [CrossRef]
- Asher, M.A.; Burton, D.C. Adolescent idiopathic scoliosis: Natural history and long term treatment effects. Scoliosis 2006, 1, 2. [Google Scholar] [CrossRef]
- Rowe, D.E.; Bernstein, S.M.; Riddick, M.F.; Adler, F.; Emans, J.B.; Gardner-Bonneau, D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J. Bone Jt. Surg. Am. 1997, 79, 664–674. [Google Scholar] [CrossRef]
- Landauer, F.; Wimmer, C.; Behensky, H. Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr. Rehabil. 2003, 6, 201–207. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of Bracing in Adolescents with Idiopathic Scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef]
- Brox, J.I.; Lange, J.E.; Gunderson, R.B.; Steen, H. Good brace compliance reduced curve progression and surgical rates in patients with idiopathic scoliosis. Eur. Spine J. 2012, 21, 1957–1963. [Google Scholar] [CrossRef] [PubMed]
- Rahman, T.; Bowen, J.R.; Takemitsu, M.; Scott, C. The Association Between Brace Compliance and Outcome for Patients With Idiopathic Scoliosis. J. Pediatr. Orthop. 2005, 25, 420–422. [Google Scholar] [CrossRef]
- Sanders, J.O.; Newton, P.O.; Browne, R.H.; Katz, D.E.; Birch, J.G.; Herring, J.A. Bracing for idiopathic scoliosis: How many patients require treatment to prevent one surgery? J. Bone Jt. Surg. 2014, 96, 649–653. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Hwang, C.J.; Kim, D.-J.; Kim, J.H.; Kim, Y.-T.; Lee, M.Y.; Yoon, S.J.; Lee, D.-H. Effectiveness of the Charleston Night-time Bending Brace in the Treatment of Adolescent Idiopathic Scoliosis. J. Pediatr. Orthop. 2012, 32, 368–372. [Google Scholar] [CrossRef]
- Sapountzi-Krepia, D.S.; Valavanis, J.; Panteleakis, G.P.; Zangana, D.T.; Vlachojiannis, P.C.; Sapkas, G.S. Perceptions of body image, happiness and satisfaction in adolescents wearing a Boston brace for scoliosis treatment. J. Adv. Nurs. 2001, 35, 683–690. [Google Scholar] [CrossRef]
- De Giorgi, S.; Piazzolla, A.; Tafuri, S.; Borracci, C.; Martucci, A.; De Giorgi, G. Chêneau brace for adolescent idiopathic scoliosis: Long-term results. Can it prevent surgery? Eur. Spine J. 2013, 22, 815–822. [Google Scholar] [CrossRef]
- Kaelin, A.J. Adolescent idiopathic scoliosis: Indications for bracing and conservative treatments. Ann. Transl. Med. 2020, 8. [Google Scholar] [CrossRef]
- Bonilla Carrasco, M.I.; Solano Ruiz, M.C. Perceived self-image in adolescent idiopathic scoliosis: An integrative review of the literature. Rev. Esc. Enferm. USP 2014, 48, 748–757. [Google Scholar] [CrossRef]
- Rezaei Montlagh, F.; Pezham, H.; Babaee, T.; Saeedi, H.; Hedayatu, Z.; Kamali, M. Persian adaptation of the Bad Sobernheim stress questionnaire for adolescent with idiopathic scoliosis. Disabil. Rehabil. 2020, 42, 562–566. [Google Scholar] [CrossRef]
- Liu, S.; Zhou, G.; Xu, N.; Mai, S.; Wang, Q.; Zeng, L.; Du, C.; Du, Y.; Zeng, Y.; Yu, M.; et al. Translation and validation of the Chinese version of Brace Questionnaire (BrQ). Transl. Pediatr. 2021, 1, 598–603. [Google Scholar] [CrossRef]
| Evaluation | M | SD | |
|---|---|---|---|
| ATR thoracic hump | 1 | 5.22 | 3.51 |
| 2 | 5.67 | 4.22 | |
| ATR lumbar hump | 1 | 4.65 | 2.57 |
| 2 | 5.01 | 3.55 | |
| Main cobb | 1 | 29.32 | 5.39 |
| 2 | 32.00 | 13.07 | |
| Vertebral rotation | 1 | 8.53 | 5.22 |
| 2 | 8.90 | 5.36 | |
| Thoracic kyphosis angle | 1 | 27.48 | 7.31 |
| 2 | 27.66 | 7.66 | |
| Lumbar lordosis angle | 1 | 45.21 | 7.75 |
| 2 | 46.89 | 8.61 | |
| DIHP | 1 | 6.22 | 1.33 |
| 2 | 6.86 | 1.61 | |
| PTSI | 1 | 20.01 | 8.63 |
| 2 | 20.91 | 8.88 | |
| CP | 1 | 40.33 | 8.05 |
| 2 | 41.05 | 8.17 |
| Pre-Intervention | Post-Intervention | Student’s T | p-Value | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| (PT) | 12.12 | 8.13 | 15.44 | 10.60 | 3.58 | 0.001 |
| (MT) | 27.26 | 7.19 | 32.48 | 15.56 | 3.84 | 0.000 |
| (TL/L) | 21.85 | 8.26 | 25.36 | 12.66 | 2.73 | 0.008 |
| LENKE Type | Mean | Std. Deviation | N |
|---|---|---|---|
| 1 | 1.34 | 6.99 | 29 |
| 2 | 2.90 | 326 | 11 |
| 3 | 6.28 | 15.65 | 21 |
| 4 | 5.69 | 8.66 | 23 |
| 5 | −0.25 | 6.48 | 12 |
| 6 | 5.58 | 14.39 | 12 |
| Total | 3.68 | 10.32 | 108 |
| Risser | Mean | Std. Deviation | N |
|---|---|---|---|
| 0 | 4.40 | 11.25 | 82 |
| 1 | 2.86 | 6.25 | 15 |
| 2 | 0.00 | 6.52 | 8 |
| 3 | −2.00 | 4.35 | 3 |
| Total | 3.68 | 10.32 | 108 |
| Main Curve | |||
|---|---|---|---|
| Pearson’s Correlation | p-Value | N | |
| Cavidra total | 0.95 | 0.001 | 108 |
| Psychosocial functioning | 0.78 | 0.001 | 108 |
| Sleep disorder | 0.87 | 0.001 | 108 |
| Back pain | 0.74 | 0.001 | 108 |
| Body image | 0.88 | 0.001 | 108 |
| Mobility | 0.83 | 0.001 | 108 |
| Lenke | N | Mean | SD |
|---|---|---|---|
| 1 | 29 | 1.20 | 0.20 |
| 2 | 11 | 1.36 | 0.34 |
| 3 | 21 | 1.47 | 0.44 |
| 4 | 23 | 1.61 | 0.45 |
| 5 | 12 | 1.24 | 0.45 |
| 6 | 12 | 1.73 | 0.44 |
| Total | 108 | 1.42 | 0.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vicente, L.G.; Barrios, M.J.; González-Santos, J.; Santamaría-Peláez, M.; Soto-Cámara, R.; Mielgo-Ayuso, J.; Fernández-Lázaro, D.; González-Bernal, J.J. The ISJ 3D Brace, a Providence Brace Evolution, as a Surgery Prevention Method in Idiopathic Scoliosis. J. Clin. Med. 2021, 10, 3915. https://doi.org/10.3390/jcm10173915
Vicente LG, Barrios MJ, González-Santos J, Santamaría-Peláez M, Soto-Cámara R, Mielgo-Ayuso J, Fernández-Lázaro D, González-Bernal JJ. The ISJ 3D Brace, a Providence Brace Evolution, as a Surgery Prevention Method in Idiopathic Scoliosis. Journal of Clinical Medicine. 2021; 10(17):3915. https://doi.org/10.3390/jcm10173915
Chicago/Turabian StyleVicente, Luis González, María Jiménez Barrios, Josefa González-Santos, Mirian Santamaría-Peláez, Raúl Soto-Cámara, Juan Mielgo-Ayuso, Diego Fernández-Lázaro, and Jerónimo J. González-Bernal. 2021. "The ISJ 3D Brace, a Providence Brace Evolution, as a Surgery Prevention Method in Idiopathic Scoliosis" Journal of Clinical Medicine 10, no. 17: 3915. https://doi.org/10.3390/jcm10173915
APA StyleVicente, L. G., Barrios, M. J., González-Santos, J., Santamaría-Peláez, M., Soto-Cámara, R., Mielgo-Ayuso, J., Fernández-Lázaro, D., & González-Bernal, J. J. (2021). The ISJ 3D Brace, a Providence Brace Evolution, as a Surgery Prevention Method in Idiopathic Scoliosis. Journal of Clinical Medicine, 10(17), 3915. https://doi.org/10.3390/jcm10173915











