Pattern of Prostate Cancer Recurrence Assessed by 68Ga-PSMA-11 PET/CT in Men Treated with Primary Local Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Synthesis of 68Ga-PSMA-11
2.3. 68Ga-PSMA PET/CT Imaging
2.4. Image Analysis and Data Collection
2.5. Statistical Analysis
3. Results
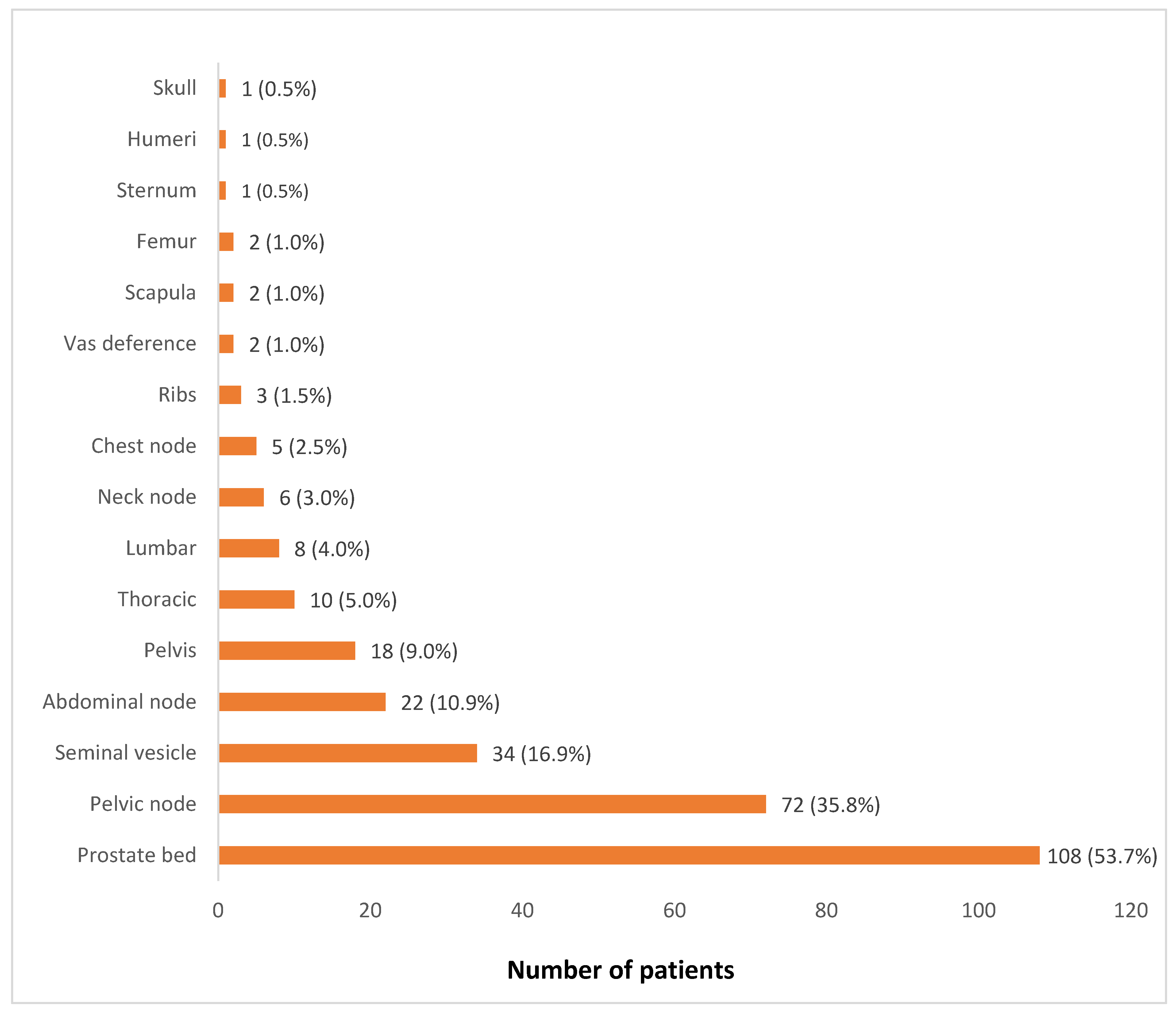
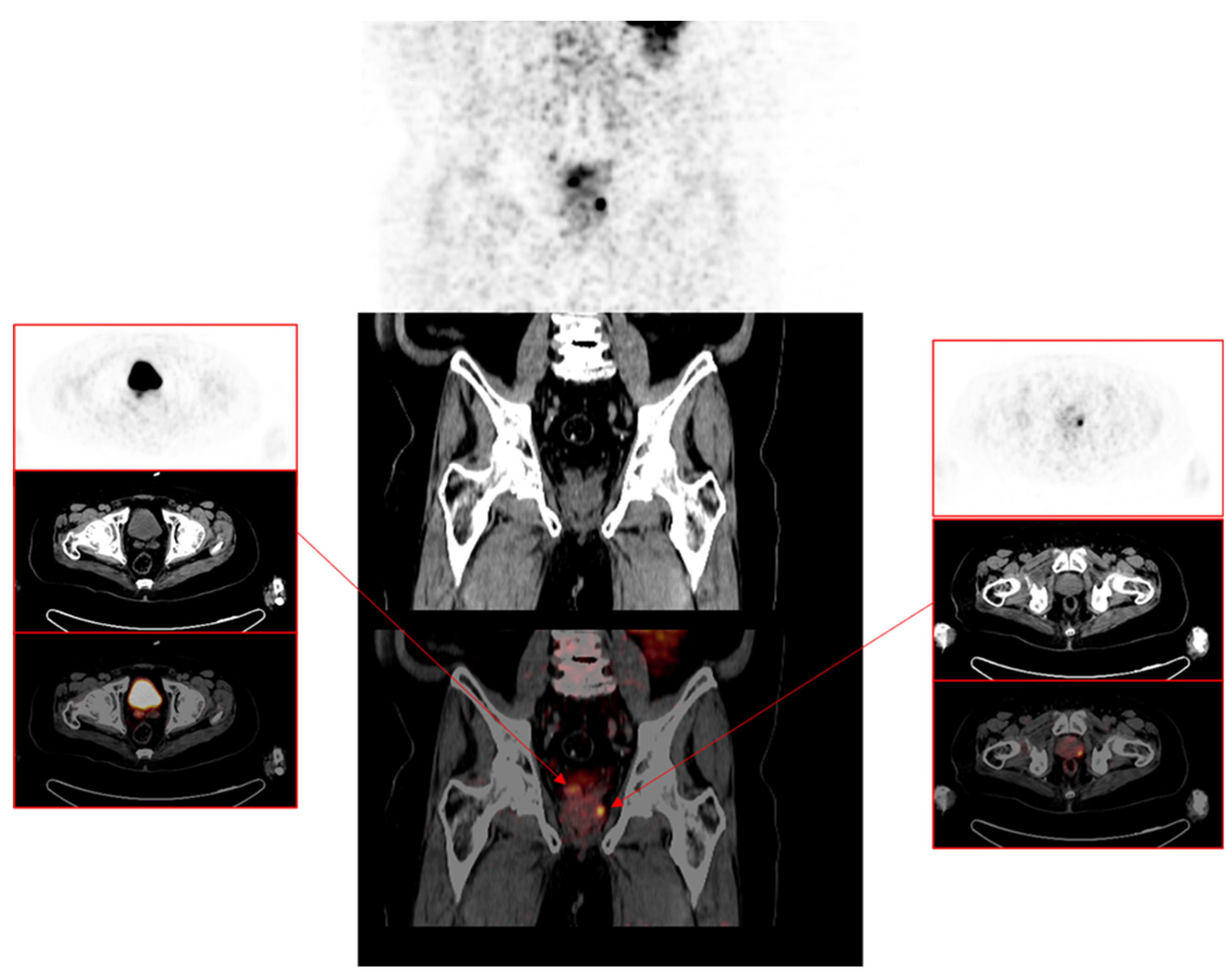
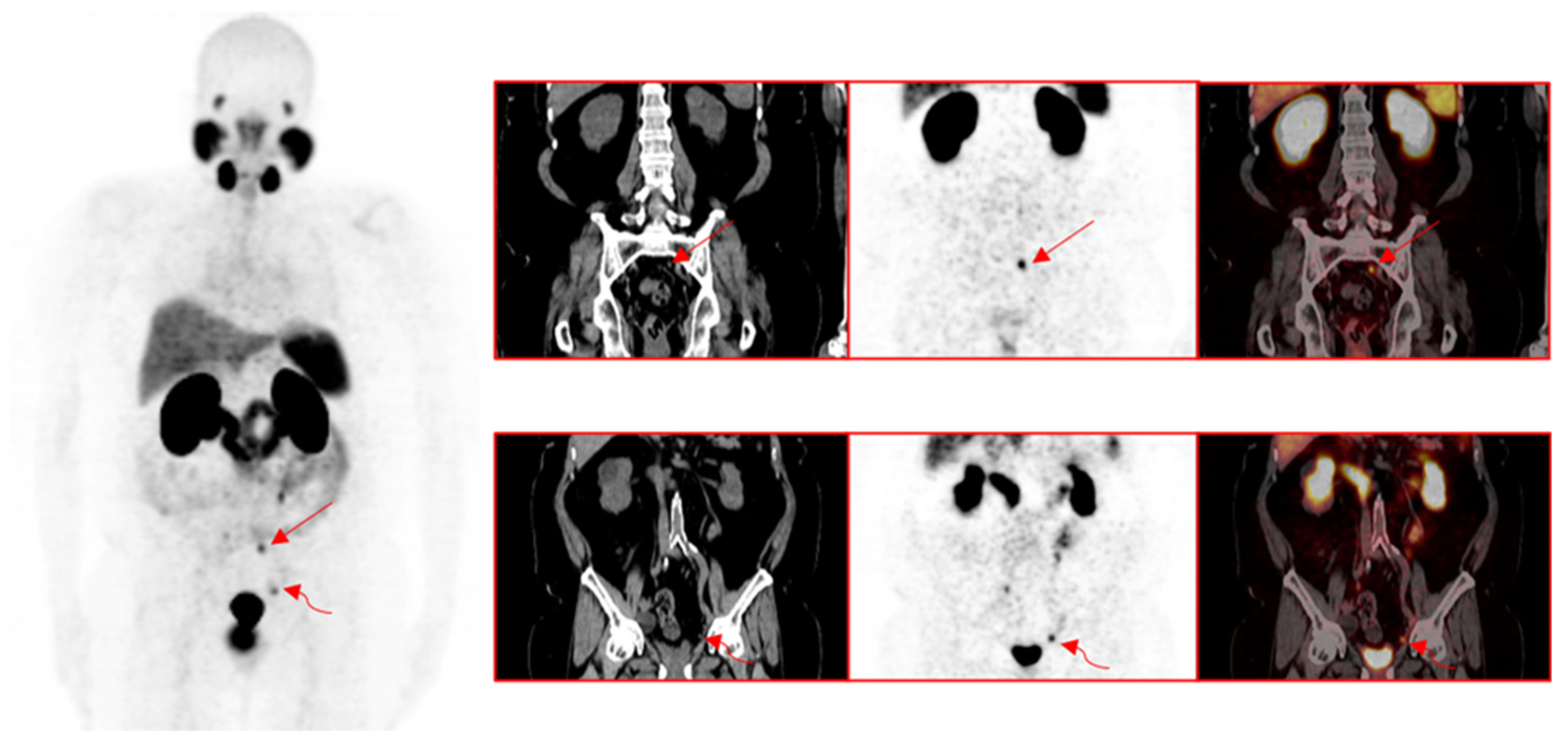
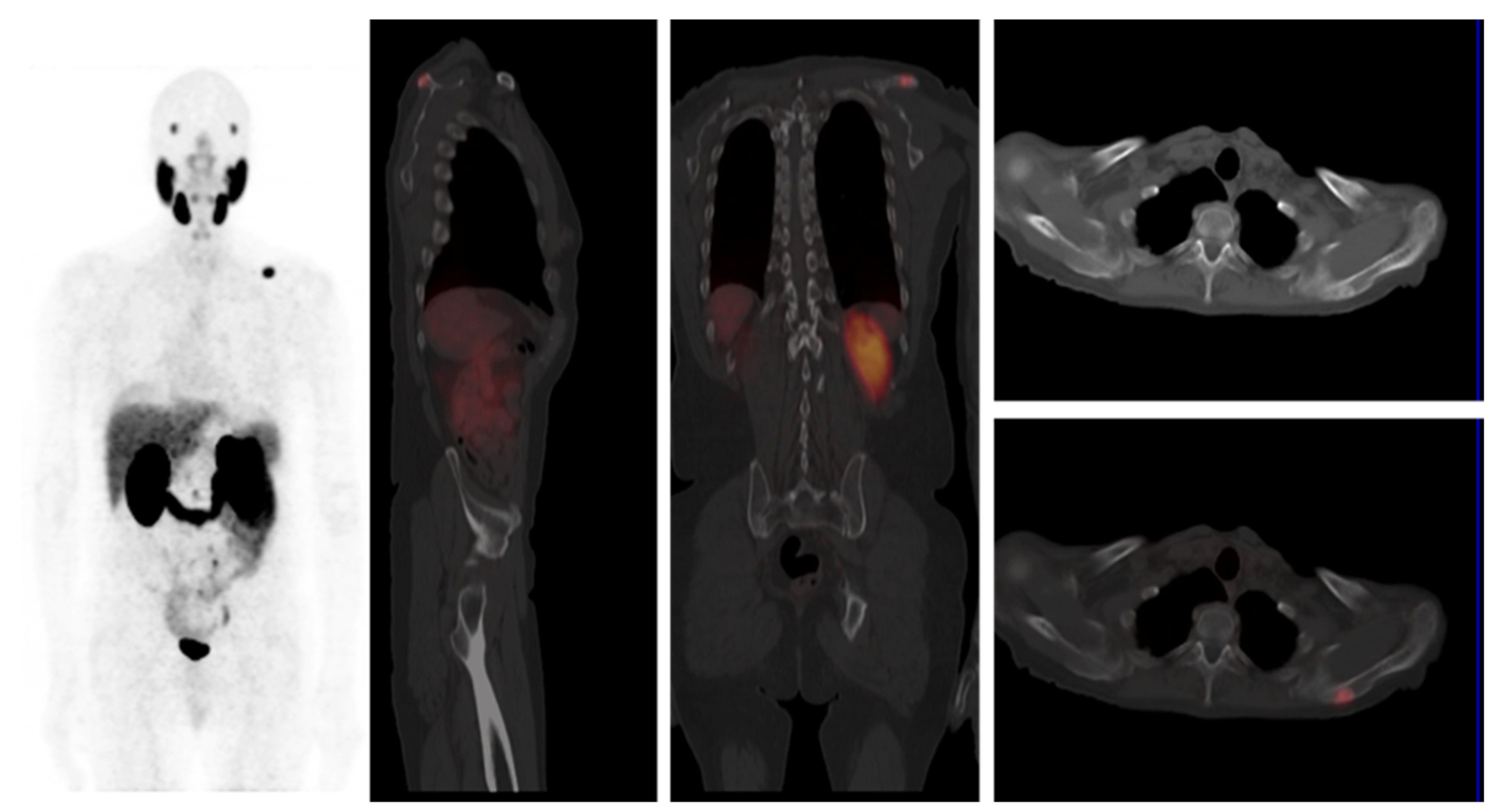
3.1. Pattern of Prostate Cancer Recurrence
3.2. Comparison of Patients with Positive versus Negative Findings for Recurrence on 68Ga-PSMA-11 PET/CT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parker, C.; Castro, E.; Fizazi, K.; Heidenreich, A.; Ost, P.; Procopio, G.; Tombal, B.; Gillessen, S. Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 1119–1134. [Google Scholar] [CrossRef] [PubMed]
- Mottet, N.; van den Bergh, R.C.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Freedland, S.J.; Humphreys, E.B.; Mangold, L.A.; Eisenberger, M.; Dorey, F.J.; Walsh, P.C.; Partin, A.W. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA 2005, 294, 433–439. [Google Scholar] [CrossRef] [Green Version]
- Roehl, K.A.; Han, M.; Ramos, C.G.; Antenor, J.A.; Catalona, W.J. Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: Long-term results. J. Urol. 2004, 172, 910–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kupelian, P.A.; Mahadevan, A.; Reddy, C.A.; Reuther, A.M.; Klein, E.A. Use of different definitions of biochemical failure after external beam radiotherapy changes conclusions about relative treatment efficacy for localized prostate cancer. Urology 2006, 68, 593–598. [Google Scholar] [CrossRef]
- Annunziata, S.; Pizzuto, D.A.; Treglia, G. Diagnostic Performance of PET Imaging Using Different Radiopharmaceuticals in Prostate Cancer According to Published Meta-Analyses. Cancers 2020, 12, 2153. [Google Scholar] [CrossRef]
- Evangelista, L.; Briganti, A.; Fanti, S.; Joniau, S.; Reske, S.; Schiavina, R.; Stief, C.; Thalmann, G.N.; Picchio, M. New Clinical Indications for (18)F/(11)C-choline, New Tracers for Positron Emission Tomography and a Promising Hybrid Device for Prostate Cancer Staging: A Systematic Review of the Literature. Eur. Urol. 2016, 70, 161–175. [Google Scholar] [CrossRef]
- Treglia, G.; Mestre, R.P.; Ferrari, M.; Bosetti, D.G.; Pascale, M.; Oikonomou, E.; De Dosso, S.; Jermini, F.; Prior, J.O.; Roggero, E.; et al. Radiolabelled choline versus PSMA PET/CT in prostate cancer restaging: A meta-analysis. Am. J. Nucl. Med. Mol. Imaging 2019, 9, 127–139. [Google Scholar]
- Benešová, M.; Schäfer, M.; Bauder-Wüst, U.; Afshar-Oromieh, A.; Kratochwil, C.; Mier, W.; Haberkorn, U.; Kopka, K.; Eder, M. Preclinical evaluation of a tailor-made DOTA-conjugated PSMA inhibitor with optimized linker moiety for imaging and endoradiotherapy of prostate cancer. J. Nucl. Med. 2015, 56, 914–920. [Google Scholar] [CrossRef] [Green Version]
- Foss, C.A.; Mease, R.C.; Fan, H.; Wang, Y.; Ravert, H.T.; Dannals, R.F.; Olszewski, R.T.; Heston, W.D.; Kozikowski, A.P.; Pomper, M.G. Radiolabeled small-molecule ligands for prostate-specific membrane antigen: In vivo imaging in experimental models of prostate cancer. Clin. Cancer Res. 2005, 11, 4022–4028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fendler, W.P.; Calais, J.; Eiber, M.; Flavell, R.R.; Mishoe, A.; Feng, F.Y.; Nguyen, H.G.; Reiter, R.E.; Rettig, M.B.; Okamoto, S.; et al. Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial. JAMA Oncol. 2019, 5, 856–863. [Google Scholar] [CrossRef] [Green Version]
- Beheshti, M.; Manafi-Farid, R.; Geinitz, H.; Vali, R.; Loidl, W.; Mottaghy, F.M.; Langsteger, W. Multiphasic 68Ga-PSMA PET/CT in the Detection of Early Recurrence in Prostate Cancer Patients with a PSA Level of Less Than 1 ng/mL: A Prospective Study of 135 Patients. J. Nucl. Med. 2020, 61, 1484–1490. [Google Scholar] [CrossRef]
- Chevalme, Y.M.; Boudali, L.; Gauthé, M.; Rousseau, C.; Skanjeti, A.; Merlin, C.; Robin, P.; Giraudet, A.L.; Janier, M.; Talbot, J.N. Survey by the French Medicine Agency (ANSM) of the imaging protocol, detection rate, and safety of 68Ga-PSMA-11 PET/CT in the biochemical recurrence of prostate cancer in case of negative or equivocal 18F-fluorocholine PET/CT: 1084 examinations. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2935–2950. [Google Scholar] [CrossRef]
- Afshar-Oromieh, A.; Holland-Letz, T.; Giesel, F.L.; Kratochwil, C.; Mier, W.; Haufe, S.; Debus, N.; Eder, M.; Eisenhut, M.; Schäfer, M.; et al. Diagnostic performance of 68Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: Evaluation in 1007 patients. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1258–1268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebenhan, T.; Vorster, M.; Marjanovic-Painter, B.; Wagener, J.; Suthiram, J.; Modiselle, M.; Mokaleng, B.; Zeevaart, J.R.; Sathekge, M. Development of a Single Vial Kit Solution for Radiolabeling of 68Ga-DKFZ-PSMA-11 and Its Performance in Prostate Cancer Patients. Molecules 2015, 20, 14860–14878. [Google Scholar] [CrossRef]
- Lawal, I.O.; Mokoala, K.M.; Mahapane, J.; Kleyhans, J.; Meckel, M.; Vorster, M.; Ebenhan, T.; Rösch, F.; Sathekge, M.M. A prospective intra-individual comparison of [68Ga]Ga-PSMA-11 PET/CT, [68Ga]Ga-NODAGAZOL PET/CT, and [99mTc]Tc-MDP bone scintigraphy for radionuclide imaging of prostate cancer skeletal metastases. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Sathekge, M.; Lengana, T.; Maes, A.; Vorster, M.; Zeevaart, J.; Lawal, I.; Ebenhan, T.; Van de Wiele, C. 68Ga-PSMA-11 PET/CT in primary staging of prostate carcinoma: Preliminary results on differences between black and white South-Africans. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 226–234. [Google Scholar] [CrossRef] [Green Version]
- Lengana, T.; van de Wiele, C.; Lawal, I.; Maes, A.; Ebenhan, T.; Boshomane, T.; Zeevaart, J.R.; Ankrah, A.; Mokgoro, N.; Vorster, M.; et al. 68Ga-PSMA-HBED-CC PET/CT imaging in Black versus White South African patients with prostate carcinoma presenting with a low volume, androgen-dependent biochemical recurrence: A prospective study. Nucl. Med. Commun. 2018, 39, 179–185. [Google Scholar] [CrossRef]
- Fendler, W.P.; Calais, J.; Eiber, M.; Simko, J.P.; Kurhanewicz, J.; Santos, R.D.; Feng, F.Y.; Reiter, R.E.; Rettig, M.B.; Nickols, N.G.; et al. False positive PSMA PET for tumor remnants in the irradiated prostate and other interpretation pitfalls in a prospective multi-center trial. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Perera, M.; Papa, N.; Roberts, M.; Williams, M.; Udovicich, C.; Vela, I.; Christidis, D.; Bolton, D.; Hofman, M.S.; Lawrentschuk, N.; et al. Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-Updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: A systematic review and meta-analysis. Eur. Urol. 2020, 77, 403–417. [Google Scholar]
- Bashir, U.; Tree, A.; Mayer, E.; Levine, D.; Parker, C.; Dearnaley, D.; Oyen, W.J. Impact of Ga-68-PSMA PET/CT on management in prostate cancer patients with early biochemical recurrence after radical prostatectomy. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 901–907. [Google Scholar] [CrossRef] [Green Version]
- Calais, J.; Czernin, J.; Cao, M.; Kishan, A.U.; Hegde, J.V.; Shaverdian, N.; Sandler, K.; Chu, F.I.; King, C.R.; Steinberg, M.L.; et al. 68Ga-PSMA-11 PET/CT mapping of prostate cancer biochemical recurrence after radical prostatectomy in 270 patients with a PSA level of less than 1.0 ng/mL: Impact on salvage radiotherapy planning. J. Nucl. Med. 2018, 59, 230–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emmett, L.; van Leeuwen, P.J.; Nandurkar, R.; Scheltema, M.J.; Cusick, T.; Hruby, G.; Kneebone, A.; Eade, T.; Fogarty, G.; Jagavkar, R.; et al. Treatment outcomes from 68Ga-PSMA-11 PET/CT-informed salvage radiation treatment in men with rising PSA after radical prostatectomy: Prognostic value of a negative PSMA PET. J. Nucl. Med. 2017, 58, 1972–1976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Leeuwen, P.J.; Stricker, P.; Hruby, G.; Kneebone, A.; Ting, F.; Thompson, B.; Nguyen, Q.; Ho, B.; Emmett, L. 68Ga-PSMA has a high detection rate of prostate cancer recurrence outside the prostatic fossa in patients being considered for salvage radiation treatment. BJU Int. 2016, 117, 732–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boreta, L.; Gadzinski, A.J.; Wu, S.Y.; Xu, M.; Greene, K.; Quanstrom, K.; Nguyen, H.G.; Carroll, P.R.; Hope, T.A.; Feng, F.Y. Location of recurrence by Gallium-68 PSMA-PET scan in prostate cancer patients eligible for salvage radiotherapy. Urology 2019, 129, 165–171. [Google Scholar] [CrossRef]
- Huits, T.H.; Luiting, H.B.; van Der Poel, H.G.; Nandurkar, R.; Donswijk, M.; Schaake, E.; Vogel, W.; Roobol, M.J.; Wit, E.; Stricker, P.; et al. Distribution of prostate cancer recurrences on gallium-68 prostate-specific membrane antigen (68Ga-PSMA) positron-emission/computed tomography after radical prostatectomy with pathological node-positive extended lymph node dissection. BJU Int. 2020, 125, 876–883. [Google Scholar] [CrossRef] [PubMed]
- King, C.R. Adjuvant versus salvage radiotherapy for high-risk prostate cancer patients. Semin Radiat. Oncol. 2013, 23, 215–221. [Google Scholar] [CrossRef]
- Roach, M., 3rd; Hanks, G.; Thames, H., Jr.; Schellhammer, P.; Shipley, W.U.; Sokol, G.H.; Sandler, H. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: Recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 965–974. [Google Scholar] [CrossRef]
- Gillessen, S.; Attard, G.; Beer, T.M.; Beltran, H.; Bjartell, A.; Bossi, A.; Briganti, A.; Bristow, R.G.; Chi, K.N.; Clarke, N.; et al. Management of patients with advanced prostate cancer: Report of the Advanced Prostate Cancer Consensus Conference 2019. Eur. Urol. 2020, 77, 508–547. [Google Scholar] [CrossRef]
| Variable | Frequency | Percent |
|---|---|---|
| PSA (ng/mL) | ||
| <0.5 | 39 | 15.8 |
| 0.5–1.0 | 37 | 15.0 |
| 1.1–2.0 | 30 | 12.1 |
| 2.1–5.0 | 70 | 28.3 |
| 5.1–10.0 | 71 | 28.7 |
| Median (IQR) | 2.70 (0.78–5.80) | |
| Range | 0.05–9.91 | |
| ISUP grade group | ||
| 1 | 68 | 27.5 |
| 2 | 55 | 22.3 |
| 3 | 46 | 18.6 |
| 4 | 30 | 12.1 |
| 5 | 21 | 8.5 |
| NA | 27 | 10.9 |
| Median (IQR) | 2 (1–5) | |
| Range | 1–5 | |
| Primary therapy | ||
| Radical prostatectomy | 157 | 63.6 |
| EBRT | 90 | 36.4 |
| 68Ga-PSMA PET-positive for recurrence | ||
| Yes | 201 | 81.4 |
| No | 46 | 18.6 |
| Number of lesions | ||
| Median (IQR) | 1 (1–2) | |
| Range | 1–5 | |
| PSA (ng/mL) | n | Median (IQR) | Range | K | p Value |
|---|---|---|---|---|---|
| <0.5 | 17 | 1.0 (1.0) | 1.0–2.0 | 16.234 | 0.003 |
| 0.5–1.0 | 28 | 1.0 (1.0) | 1.0–3.0 | ||
| 1.1–2.0 | 25 | 1.0 (1.0–1.5) | 1.0–4.0 | ||
| 2.1–5.0 | 63 | 1.0 (1.0–2.0) | 1.0–5.0 | ||
| 5.1–10.0 | 68 | 1.0 (1.0–2.0) | 1.0–5.0 |
| Site of recurrence on 68Ga-PSMA-11 PET/CT | |||||
|---|---|---|---|---|---|
| Pelvic | Extra-Pelvic | Both | ꭓ2 | p Value | |
| Variable | n (%) | n (%) | |||
| ISUP grade group | |||||
| 1 | 32 (57.1) | 16 (28.6) | 8 (14.3) | 15.015 | 0.059 |
| 2 | 27 (67.5) | 11 (27.5) | 2 (5.0) | ||
| 3 | 18 (47.4) | 13 (34.2) | 7 (18.4) | ||
| 4 | 17 (65.4) | 1 (3.8) | 8 (30.8) | ||
| 5 | 11 (57.9) | 4 (21.1) | 4 (21.4) | ||
| PSA (ng/mL) | |||||
| <0.5 | 10 (58.8) | 6 (35.3) | 1 (5.9) | 19.602 | 0.012 |
| 0.5–1.0 | 20 (71.4) | 6 (21.4) | 2 (7.1) | ||
| 1.1–2.0 | 18 (72.0) | 5 (20.0) | 2 (8.0) | ||
| 2.1–5.0 | 41 (65.1) | 15 (23.8) | 7 (11.1) | ||
| 5.1–10.0 | 29 (42.6) | 18 (26.5) | 21 (30.9) | ||
| Primary therapy | |||||
| Radical prostatectomy | 64 (55.7) | 37 (32.2) | 14 (12.2) | 9.131 | 0.010 |
| EBRT | 54 (62.8) | 13 (15.1) | 19 (22.1) | ||
| Primary Therapy | ||||
|---|---|---|---|---|
| Radical Prostatectomy | Radiotherapy | ꭓ2 | p Value | |
| Variable | n (%) | n (%) | ||
| Age (years) | ||||
| Mean ± SD | 65.39 ± 7.52 | 66.28 ± 7.49 | −0.889 t | 0.375 |
| Range | 47–88 | 51–87 | ||
| PSA (ng/mL) | ||||
| <0.5 | 33 (21.0) | 6 (6.7) | 25.770 | <0.001 |
| 0.5–1.0 | 26 (16.6) | 11 (12.2) | ||
| 1.1–2.0 | 25 (15.9) | 5 (5.6) | ||
| 2.1–5.0 | 42 (26.8) | 28 (31.1) | ||
| 5.1–10.0 | 31 (19.7) | 40 (44.4) | ||
| Median (IQR) | 1.77 (0.53–4.26) | 4.35 (1.92–7.60) | 4447.500 U | <0.001 |
| Range | 0.05–9.90 | 0.05–9.91 | ||
| ISUP grade group | ||||
| 1 | 31 (45.6) | 37 (54.4) | 13.816 | 0.008 |
| 2 | 41 (74.5) | 14 (25.5) | ||
| 3 | 33 (71.7) | 13 (28.3) | ||
| 4 | 20 (66.7) | 10 (33.3) | ||
| 5 | 14 (66.7) | 7 (33.3) | ||
| Median (IQR) | 2 (2–3) | 2 (1–3) | 4519.000 U | 0.012 |
| Range | 1–5 | 1–5 | ||
| Recurrence | ||||
| Yes | 115 (73.2) | 86 (95.6) | 18.783 | <0.001 |
| No | 42 (26.8) | 4 (4.4) | ||
| Site of recurrence ** | ||||
| Prostate bed/gland | 50 (31.8) | 58 (64.4) | 24.704 | <0.001 |
| Seminal vesicle | 19 (12.1) | 15 (16.7) | 1.004 | 0.316 |
| Vas deference | 1 (0.6) | 1 (1.1) | 0.160 F | 1.000 |
| Pelvic node | 40 (25.5) | 32 (35.6) | 2.813 | 0.093 |
| Abdominal node | 14 (8.9) | 8 (8.9) | <0.001 | 0.994 |
| Chest node | 3 (1.9) | 2 (2.2) | 0.028 F | 1.000 |
| Neck node | 5 (3.2) | 1 (1.1) | 1.038 F | 0.421 |
| Pelvic bone | 10 (6.4) | 8 (8.9) | 0.537 | 0.463 |
| Lumbar spine | 4 (2.5) | 4 (4.4) | 0.657 F | 0.467 |
| Thoracic spine | 8 (5.1) | 2 (2.2) | 1.216 F | 0.335 |
| Rib | 2 (1.3) | 1 (1.1) | 0.013 F | 1.000 |
| Scapular | 2 (1.3) | 0 (0.0) | 1.156 F | 0.535 |
| Clavicle | 1 (0.6) | 0 (0.0) | 0.576 F | 0.448 |
| Sternum | 1 (0.6) | 0 (0.0) | 0.576 F | 1.000 |
| Humerus | 1 (0.6) | 0 (0.0) | 0.576 F | 1.000 |
| Femur | 2 (1.3) | 0 (0.0) | 1.156 F | 0.535 |
| Skull | 0 (0.0) | 1 (1.1) | 1.752 F | 0.186 |
| 68Ga-PSMA PET Positivity for Recurrence | ||||
|---|---|---|---|---|
| Yes | No | ꭓ2 | p Value | |
| Variable | n (%) | n (%) | ||
| Age (years) | ||||
| Mean ± SD | 66.12 ± 7.38 | 63.96 ± 7.89 | 1.770 t | 0.078 |
| Range | 48–88 | 47–85 | ||
| PSA (ng/mL) | ||||
| <0.5 | 17 (43.6) | 22 (56.4) | 50.760 | <0.001 |
| 0.5–1.0 | 28 (75.7) | 9 (24.3) | ||
| 1.1–2.0 | 25 (83.3) | 5 (16.7) | ||
| 2.1–5.0 | 63 (90.0) | 7 (10.0) | ||
| 5.1–10.0 | 68 (95.8) | 3 (4.2) | ||
| Median (IQR) | 3.22 (1.21–6.58) | 0.51 (0.32–1.79) | 2066.000 U | <0.001 |
| Range | 0.05–9.91 | 0.05–7.64 | ||
| ISUP grade group | ||||
| 1 | 56 (82.4) | 12 (17.6) | 4.503 | 0.342 |
| 2 | 40 (72.7) | 15 (27.3) | ||
| 3 | 38 (82.6) | 8 (17.4) | ||
| 4 | 26 (86.7) | 4 (13.3) | ||
| 5 | 19 (90.5) | 2 (9.5) | ||
| Median (IQR) | 2 (1–4) | 2 (1–3) | 3323.000 U | 0.332 |
| Range | 1–5 | 1–5 | ||
| Primary therapy | ||||
| Radical prostatectomy | 115 (73.2) | 42 (26.8) | 18.783 | <0.001 |
| EBRT | 86 (95.6) | 4 (4.4) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawal, I.O.; Lengana, T.; Popoola, G.O.; Orunmuyi, A.T.; Kgatle, M.M.; Mokoala, K.M.G.; Sathekge, M.M. Pattern of Prostate Cancer Recurrence Assessed by 68Ga-PSMA-11 PET/CT in Men Treated with Primary Local Therapy. J. Clin. Med. 2021, 10, 3883. https://doi.org/10.3390/jcm10173883
Lawal IO, Lengana T, Popoola GO, Orunmuyi AT, Kgatle MM, Mokoala KMG, Sathekge MM. Pattern of Prostate Cancer Recurrence Assessed by 68Ga-PSMA-11 PET/CT in Men Treated with Primary Local Therapy. Journal of Clinical Medicine. 2021; 10(17):3883. https://doi.org/10.3390/jcm10173883
Chicago/Turabian StyleLawal, Ismaheel O., Thabo Lengana, Gbenga O. Popoola, Akintunde T. Orunmuyi, Mankgopo M. Kgatle, Kgomotso M. G. Mokoala, and Mike M. Sathekge. 2021. "Pattern of Prostate Cancer Recurrence Assessed by 68Ga-PSMA-11 PET/CT in Men Treated with Primary Local Therapy" Journal of Clinical Medicine 10, no. 17: 3883. https://doi.org/10.3390/jcm10173883
APA StyleLawal, I. O., Lengana, T., Popoola, G. O., Orunmuyi, A. T., Kgatle, M. M., Mokoala, K. M. G., & Sathekge, M. M. (2021). Pattern of Prostate Cancer Recurrence Assessed by 68Ga-PSMA-11 PET/CT in Men Treated with Primary Local Therapy. Journal of Clinical Medicine, 10(17), 3883. https://doi.org/10.3390/jcm10173883









