The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade
Abstract
1. Introduction
2. Methods
2.1. Information Sources and Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Risk of Bias in Individual Studies
2.4. Data Collection Process
3. Results
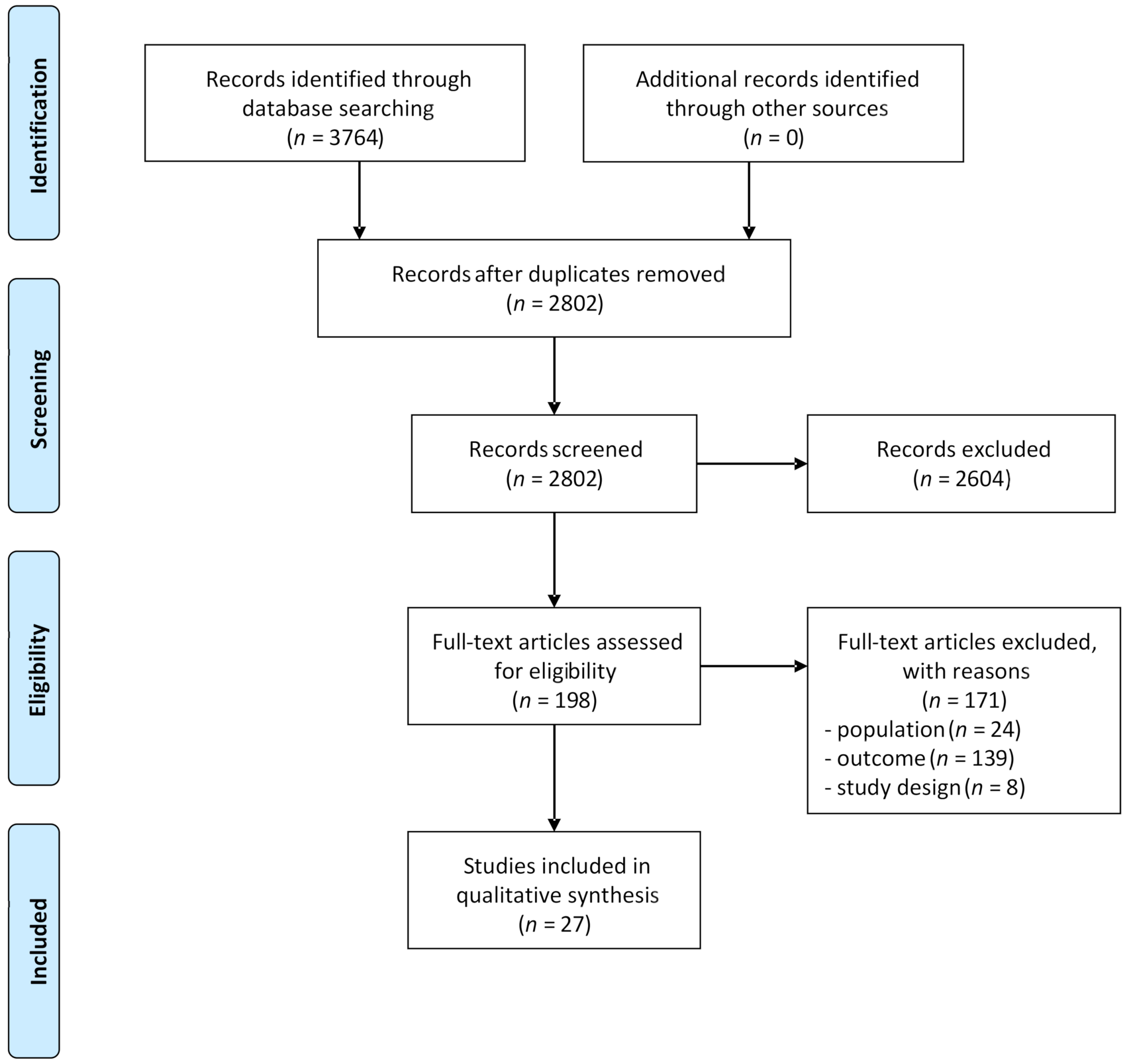
3.1. Study Selection
3.2. Risk of Bias and Level of Evidence
3.3. Study Characteristics
3.4. Synthesis of Results
3.5. Associations between Sleep Parameters and Chronic Spinal Pain
3.5.1. Sleep Quality
Association between Sleep Quality and Pain Intensity
Association between Sleep Quality and Pain Duration
Association between Sleep Quality and the Presence of CLBP
Association between Sleep Sufficiency and CLBP
3.5.2. Insomnia and Sleep Disturbances
Association between Insomnia Severity and Pain Intensity
Association between Sleep Disturbance and Pain Intensity
Association between Insomnia Severity and Pain Duration
Association between Insomnia Severity and CLBP
Association between Sleep Disturbance and CLBP
Association between Sleep Problems and CNP
3.5.3. Sleep Duration and Sleep Sufficiency
Association between Sleep Deprivation and Pain Intensity
Association between Objective Sleep Parameters and Pain Intensity
Association between Sleep Duration and CLBP
3.5.4. Sleepiness
Association between Sleepiness and Pain Intensity
Association between Sleepiness and Pain Duration
3.5.5. Summary of Results for the Association between Sleep Parameters and CSP
3.6. Sleep Problems as Predictor for CSP
Summary of Results for Sleep Problems as Predictor for CSP
3.7. CSP as Predictor for Sleep Problems
Summary of Results for CSP as Predictor for Sleep Problems
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coggeshall, M.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best Pract. Res. Clin. Reum. 2010, 24, 783–792. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Roussel, N.A.; Nijs, J.; Meeus, M.; Mylius, V.; Fayt, C.; Oostendorp, R. Central sensitization and altered central pain processing in chronic low back pain: Fact or myth? Clin. J. Pain 2013, 29, 625–638. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Clark, J.; Malfliet, A.; Ickmans, K.; Voogt, L.; Don, S.; den Bandt, H.; Goubert, D.; Kregel, J.; Coppieters, I.; et al. In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention for low back pain. Clin. Exp. Rheumatol. 2017, 35, S108–S115. [Google Scholar]
- Van Oosterwijck, J.; Nijs, J.; Meeus, M.; Paul, L. Evidence for central sensitization in chronic whiplash: A systematic literature review. Eur. J. Pain 2013, 17, 299–312. [Google Scholar] [CrossRef]
- Manchikanti, L.; Singh, V.; Datta, S.; Cohen, S.P.; Hirsch, J.A. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician 2009, 12, 35–70. [Google Scholar] [CrossRef]
- Zielinski, M.R.; McKenna, J.T.; McCarley, R.W. Functions and mechanisms of sleep. AIMS Neurosci. 2016, 3, 67–104. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.K.Y.; Wright, K.J.; Salkovskis, P.M. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J. Sleep Res. 2007, 16, 85–95. [Google Scholar] [CrossRef]
- Alsaadi, S.M.; McAuley, J.H.; Hush, J.M.; Maher, C.G. Prevalence of sleep disturbance in patients with low back pain. Eur. Spine J. 2011, 20, 737–743. [Google Scholar] [CrossRef]
- Artner, J.; Cakir, B.; Spiekermann, J.A.; Kurz, S.; Leucht, F.; Reichel, H.; Lattig, F. Prevalence of sleep deprivation in patients with chronic neck and back pain: A retrospective evaluation of 1016 patients. J. Pain Res. 2013, 6, 1–6. [Google Scholar] [CrossRef]
- Bahouq, H.; Allali, F.; Rkain, H.; Hmamouchi, I.; Hajjaj-Hassouni, N. Prevalence and severity of insomnia in chronic low back pain patients. Rheumatol. Int. 2013, 33, 1277–1281. [Google Scholar] [CrossRef]
- Purushothaman, B.; Singh, A.; Lingutla, K.; Bhatia, C.; Pollock, R.; Krishna, M. Prevalence of insomnia in patients with chronic back pain. J. Orthop. Surg. 2013, 21, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The association of sleep and pain: An update and a path forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Herrero Babiloni, A.; De Koninck, B.P.; Beetz, G.; De Beaumont, L.; Martel, M.O.; Lavigne, G.J. Sleep and pain: Recent insights, mechanisms, and future directions in the investigation of this relationship. J. Neural Transm. 2020, 127, 647–660. [Google Scholar] [CrossRef] [PubMed]
- Kelly, G.A.; Blake, C.; Power, C.K.; Okeeffe, D.; Fullen, B.M. The association between chronic low back pain and sleep: A systematic review. Clin. J. Pain 2011, 27, 169–181. [Google Scholar] [CrossRef]
- Moldofsky, H. Sleep and pain. Sleep Med. Rev. 2001, 5, 385–396. [Google Scholar] [CrossRef]
- Menefee, L.A.; Cohen, M.J.M.; Anderson, W.R.; Doghramji, K.; Frank, E.D.; Lee, H. Sleep Disturbance and Nonmalignant Chronic Pain: A Comprehensive Review of the Literature. Pain Med. 2000, 1, 156–172. [Google Scholar] [CrossRef]
- Schuh-Hofer, S.; Wodarski, R.; Pfau, D.B.; Caspani, O.; Magerl, W.; Kennedy, J.D.; Treede, R.D. One night of total sleep deprivation promotes a state of generalized hyperalgesia: A surrogate pain model to study the relationship of insomnia and pain. Pain 2013, 154, 1613–1621. [Google Scholar] [CrossRef]
- Smith, M.T.; Edwards, R.R.; McCann, U.D.; Haythomthwaite, J.A. The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep 2007, 30, 494–505. [Google Scholar] [CrossRef]
- Edwards, R.R.; Almeida, D.M.; Klick, B.; Haythomthwaite, J.A.; Smith, M.T. Duration of Sleep to Next-Day Pain Report in the General Population. Pain 2008, 137, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Woo, A.; Ratnayake, G. Sleep and pain management: A review. Pain Manag. 2020, 10, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Drake, C.L.; Harvey, A.G.; Krystal, A.D.; Manber, R.; Riemann, D.; Spiegelhalder, K. Insomnia disorder. Nat. Rev. Dis. Prim. 2015, 1, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Mathias, J.L.; Cant, M.L.; Burke, A.L.J. Sleep disturbances and sleep disorders in adults living with chronic pain: A meta-analysis. Sleep Med. 2018, 52, 198–210. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Mairesse, O.; Neu, D.; Leysen, L.; Danneels, L.; Cagnie, B.; Meeus, M.; Moens, M.; Ickmans, K.; Goubert, D. Sleep disturbances in chronic pain: Neurobiology, assessment, and treatment in physical therapist practice. Phys. Ther. 2018, 98, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Carpenter, J.S.; Andrykowski, M.A. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J. Psychosom. Res. 1998, 45, 5–13. [Google Scholar] [CrossRef]
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Dolenc Groselj, L.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700. [Google Scholar] [CrossRef] [PubMed]
- Rolke, R.; Magerl, W.; Campbell, K.A.; Schalber, C.; Caspari, S.; Birklein, F.; Treede, R.D. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain 2006, 10, 77. [Google Scholar] [CrossRef]
- Agmon, M.; Armon, G. Increased insomnia symptoms predict the onset of back pain among employed adults. PLoS ONE 2014, 9, e103591. [Google Scholar] [CrossRef]
- Kääriä, S.; Laaksonen, M.; Rahkonen, O.; Lahelma, E.; Leino-Arjas, P. Risk factors of chronic neck pain: A prospective study among middle-aged employees. Eur. J. Pain 2012, 16, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Mork, P.J.; Vik, K.L.; Moe, B.; Lier, R.; Bardal, E.M.; Nilsen, T.I.L. Sleep problems, exercise and obesity and risk of chronic musculoskeletal pain: The Norwegian HUNT study. Eur. J. Public Health 2014, 24, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Pakpour, A.H.; Yaghoubidoust, M.; Campbell, P. Persistent and Developing Sleep Problems: A Prospective Cohort Study on the Relationship to Poor Outcome in Patients Attending a Pain Clinic with Chronic Low Back Pain. Pain Pract. 2018, 18, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Skarpsno, E.S.; Mork, P.J.; Nilsen, T.I.L.; Nordstoga, A.L. Influence of sleep problems and co-occurring musculoskeletal pain on long-term prognosis of chronic low back pain: The HUNT Study. J. Epidemiol. Community Health 2020, 74, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Uhlig, B.L.; Sand, T.; Nilsen, T.I.; Mork, P.J.; Hagen, K. Insomnia and risk of chronic musculoskeletal complaints: Longitudinal data from the HUNT study, Norway. BMC Musculoskelet. Disord. 2018, 19, 128. [Google Scholar] [CrossRef]
- Häggman-Henrikson, B.; Grönqvist, J.; Eriksson, P.O. Frequent jaw-face pain in chronic Whiplash-Associated Disorders. Swed. Dent. J. 2011, 35, 123–131. [Google Scholar]
- Heffner, K.; France, C.; Trost, Z.; Mei, H.; Pigeon, W. Chronic Low Back Pain, Sleep Disturbance, and Interleukin-6. Clin. J. Pain 2011, 2723, 35–41. [Google Scholar] [CrossRef]
- Hong, J.H.; Kim, H.D.; Shin, H.H.; Huh, B. Assessment of depression, anxiety, sleep disturbance, and quality of life in patients with chronic low back pain in Korea. Korean J. Anesthesiol. 2014, 66, 444–450. [Google Scholar] [CrossRef]
- O’Donoghue, G.M.; Fox, N.; Heneghan, C.; Hurley, D.A. Objective and subjective assessment of sleep in chronic low back pain patients compared with healthy age and gender matched controls: A pilot study. BMC Musculoskelet. Disord. 2009, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, M.; Hasanefendiotlu, E.Z.; Sungur, M.A.; Incel, N.A.; Çimen, Ö.B.; Kanik, A.; Şahin, G. Sleep quality in patients with chronic low back pain: A cross-sectional study assesing its relations with pain, functional status and quality of life. J. Back Musculoskelet. Rehabil. 2015, 28, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Burgess, H.J.; Burns, J.W.; Buvanendran, A.; Gupta, R.; Chont, M.; Kennedy, M.; Bruehl, S. Associations between Sleep Disturbance and Chronic Pain Intensity and Function: A Test of Direct and Indirect Pathways. Clin. J. Pain 2019, 35, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Gerhart, J.I.; Burns, J.W.; Post, K.M.; Smith, D.A.; Porter, L.S.; Burgess, H.J.; Schuster, E.; Buvanendran, A.; Fras, A.M.; Keefe, F.J. Relationships Between Sleep Quality and Pain-Related Factors for People with Chronic Low Back Pain: Tests of Reciprocal and Time of Day Effects. Ann. Behav. Med. 2017, 51, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.K.N.; Simic, M.; Cvancarova Småstuen, M.; De Barros Pinheiro, M.; Ferreira, P.H.; Bakke Johnsen, M.; Heuch, I.; Grotle, M.; Zwart, J.A.; Nilsen, K.B. The association between insomnia, c-reactive protein, and chronic low back pain: Cross-sectional analysis of the HUNT study, Norway. Scand. J. Pain 2019, 19, 765–777. [Google Scholar] [CrossRef]
- Juan, W.; Rui, L.; Wei-Wen, Z. Chronic neck pain and depression: The mediating role of sleep quality and exercise. Psychol. Health Med. 2020, 25, 1029–1035. [Google Scholar] [CrossRef]
- Kennedy, P.C.; Purtill, H.; O’Sullivan, K. Musculoskeletal pain in Primary Care Physiotherapy: Associations with demographic and general health characteristics. Musculoskelet. Sci. Pract. 2018, 35, 61–66. [Google Scholar] [CrossRef]
- Kim, S.H.; Sun, J.M.; Yoon, K.B.; Moon, J.H.; An, J.R.; Yoon, D.M. Risk factors associated with clinical insomnia in chronic low back pain: A retrospective analysis in a University Hospital in Korea. Korean J. Pain 2015, 28, 137–143. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, D.H.; Yoon, K.B.; An, J.R.; Yoon, D.M. Factors Associated with Increased Risk for Clinical Insomnia in Patients with Chronic Neck Pain. Pain Physician 2015, 18, 593–598. [Google Scholar]
- Ouchi, K.; Watanabe, M.; Tomiyama, C.; Nikaido, T.; Oh, Z.; Hirano, T.; Akazawa, K.; Mandai, N. Emotional effects on factors associated with chronic low back pain. J. Pain Res. 2019, 12, 3343–3353. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-De-Souza, D.P.; Fernández-De-Las-Peñas, C.; Martín-Vallejo, F.J.; Blanco-Blanco, J.F.; Moro-Gutiérrez, L.; Alburquerque-Sendín, F. Differences in pain perception, health-related quality of life, disability, mood, and sleep between Brazilian and spanish people with chronic non-specific low back pain. Braz. J. Phys. Ther. 2016, 20, 412–421. [Google Scholar] [CrossRef]
- Shmagel, A.; Foley, R.; Ibrahim, H. Epidemiology of Chronic Low Back Pain in US Adults: Data from the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 2016, 68, 1688–1694. [Google Scholar] [CrossRef]
- Srivastava, S.; Yadav, P.; Panchal, B.N.; Vala, A.U.; Ratnani, I.; Khania, P. Association of depression and chronic lower-back pain. Arch. Psychiatry Psychother. 2018, 20, 37–46. [Google Scholar] [CrossRef]
- Uchmanowicz, I.; Kołtuniuk, A.; Stępień, A.; Uchmanowicz, B.; Rosińczuk, J. The influence of sleep disorders on the quality of life in patients with chronic low back pain. Scand. J. Caring Sci. 2019, 33, 119–127. [Google Scholar] [CrossRef]
- Wang, H.Y.; Fu, T.S.; Hsu, S.C.; Hung, C.I. Association of depression with sleep quality might be greater than that of pain intensity among outpatients with chronic low back pain. Neuropsychiatr. Dis. Treat. 2016, 12, 1993–1998. [Google Scholar] [CrossRef]
- Yamada, K.; Kubota, Y.; Shimizu, Y.; Shibata, M.; Morotomi, N. Association of sleep sufficiency and duration with chronic pain prevalence: A population-based cross-sectional study. J. Psychosom. Res. 2019, 120, 74–80. [Google Scholar] [CrossRef]
- Whibley, D.; Alkandari, N.; Kristensen, K.; Barnish, M.; Rzewuska, M.; Druce, K.L.; Tang, N.K.Y. Sleep and Pain: A Systematic Review of Studies of Mediation. Clin. J. Pain 2019, 35, 544–558. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Sacket, D.L.; Richardson, W.S.; Rosenberg, W. Evidence-Based Medicine: How to Practice and Teach EBM; Churchill Livingstone: New York, NY, USA, 1997. [Google Scholar]
- Roehrs, T.; Roth, T. Sleep and pain: Interaction of two vital functions. Semin. Neurol. 2005, 25, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.K.Y.; Goodchild, C.E.; Sanborn, A.N.; Howard, J.; Salkovskis, P.M. Deciphering the Temporal Link between Pain and Sleep in a Heterogeneous Chronic Pain Patient Sample: A Multilevel Daily Process Study. Sleep 2012, 35, 675–687. [Google Scholar] [CrossRef] [PubMed]
- Haack, M.; Simpson, N.; Sethna, N.; Kaur, S.; Mullington, J. Sleep deficiency and chronic pain: Potential underlying mechanisms and clinical implications. Neuropsychopharmacology 2020, 45, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Loggia, M.L.; Polli, A.; Moens, M.; Huysmans, E.; Goudman, L.; Meeus, M.; Vanderweeën, L.; Ickmans, K.; Clauw, D. Sleep disturbances and severe stress as glial activators: Key targets for treating central sensitization in chronic pain patients? Expert Opin. Ther. Targets 2017, 21, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Hastings Hagenauer, M.; Crodelle, J.A.; Piltz, S.H.; Toporikova, N.; Ferguson, P.; Booth, V. The Modulation of Pain by Circadian and Sleep-Dependent Processes: A Review of the Experimental Evidence. Assoc. Women Math. Ser. 2017, 8, 1–21. [Google Scholar] [CrossRef]
- Babiloni, A.H.; Beetz, G.; Tang, N.K.; Heinzer, R.; Nijs, J.; Martel, M.; Lavigne, G. Towards the endotyping of the sleep-pain interaction: A topical review on multitarget strategies based on phenotypic vulnerabilities and putative pathways. Pain 2021, 162, 1281–1288. [Google Scholar] [CrossRef]
- Tang, N.K.Y.; Goodchild, C.E.; Salkovskis, P.M. Hybrid cognitive-behaviour therapy for individuals with insomnia and chronic pain: A pilot randomised controlled trial. Behav. Res. Ther. 2012, 50, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Pigeon, W.R.; Moynihan, J.; Matteson-rusby, S.; Jungquist, C.R.; Xia, Y.; Tu, X.; Perlis, M.L. Comparative effectiveness of CBT interventions for co-morbid chronic pain & insomnia: A pilot study. Behav. Res. Ther. 2012, 50, 685–689. [Google Scholar] [CrossRef]
- Morin, C.M.; Vallières, A.; Ivers, H. Dysfunctional beliefs and attitudes about sleep (DBAS): Validation of a brief version (DBAS-16). Sleep 2007, 30, 1547–1554. [Google Scholar] [CrossRef]
- Kushida, C.A.; Littner, M.R.; Morgenthaler, T.; Alessi, C.A.; Bailey, D.; Coleman, J.; Friedman, L.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 2005, 28, 499–521. [Google Scholar] [CrossRef]
- Association, A.S.D. An American Sleep Disorders Association Report Practice Parameters for the Use of Actigraphy in the Clinical Assessment of Sleep Disorders. Sleep 1995, 18, 288–302. [Google Scholar]
- Jensen, M.P.; Tomé-Pires, C.; de la Vega, R.; Galàn, S.; Solé, E.; Miró, J. What determines whether a pain is rated as mild, moderate, or severe? The importance of pain beliefs and pain interference. Clin. J. Pain 2017, 33, 414–421. [Google Scholar] [CrossRef]
- Szmyd, B.; Rogut, M.; Białasiewicz, P.; Gabryelska, A. The impact of glucocorticoids and statins on sleep quality. Sleep Med. Rev. 2021, 55, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Van Gastel, A. Drug-Induced Insomnia and Excessive Sleepiness. Sleep Med. Clin. 2018, 13, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Karppinen, J.; Leino-Arjas, P.; Solovieva, S.; Viikari-Juntura, E. The association between obesity and low back pain: A meta-analysis. Am. J. Epidemiol. 2010, 171, 135–154. [Google Scholar] [CrossRef] [PubMed]
| Population | AND | Outcome | |
|---|---|---|---|
| chronic | back pain/ache | sleep | |
| persistent | neck pain/ache | insomnia | |
| lasting | cervical pain/ache | agrypnia | |
| longterm | spinal pain/ache | ||
| long term | vertebral pain/ache | ||
| lumbar pain/ache | |||
| lumbosacral pain/ache | |||
| backpain | |||
| backache | |||
| dorsalgia | |||
| lumbago | |||
| lumbalgia | |||
| lumbodynia | |||
| whiplash | |||
| fbss | |||
| failed back surgery | |||
| failed back syndrome | |||
| postlaminectomy syndrome | |||
| post-laminectomy syndrome | |||
| cervicobrachial neuralgia/pain/syndrome/disease/radiculopathy/compression syndrome | |||
| cervico-brachial neuralgia/pain/syndrome/disease/radiculopathy/compression syndrome | |||
| cervical neuralgia/syndrome/disease/radiculopathy/compression syndrome | |||
| neck shoulder arm syndrome | |||
| shoulder arm neck syndrome | |||
| Study | Selection | Comparability | Exposure | Level of Evidence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Agmon et al. [33] | − | + | − | − | + | − | − | + | − | B |
| Kääria et al. [34] | − | + | − | − | + | + | − | + | + | B |
| Mork et al. [35] | + | + | − | − | + | + | − | + | − | B |
| Pakpour et al. [36] | − | + | − | − | + | + | − | + | + | B |
| Skarpsno et al. [37] | + | + | − | − | + | + | − | + | − | B |
| Uhlig et al. [38] | + | + | − | − | + | + | − | + | − | B |
| Study | Selection | Comparability | Exposure | Level of Evidence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Häggmann-Henrikson et al. [39] | − | + | − | + | + | − | − | + | − | B |
| Heffner et al. [40] | − | + | + | + | + | + | − | + | − | B |
| Hong et al. [41] | + | − | + | + | + | − | − | + | − | B |
| O’Donoghue et al. [42] | − | − | − | + | + | − | + | + | − | B |
| Sezgin et al. [43] | − | − | − | + | + | − | − | + | − | B |
| Study | Selection | Comparability | Outcome | Level of Evidence | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Artner et al. [11] | − | − | − | + | + | − | − | + | C |
| Bahouq et al. [12] | − | − | − | + | + | − | − | + | C |
| Burgess et al. [44] | + | + | − | + | − | + | − | + | C |
| Gerhart et al. [45] | + | − | − | + | + | − | − | + | C |
| Ho et al. [46] | + | + | − | + | + | + | − | + | C |
| Juan et al. [47] | − | − | − | + | − | − | − | + | C |
| Kennedy et al. [48] | − | − | − | + | + | − | − | + | C |
| Kim et al. [49] | − | − | − | + | + | + | − | + | C |
| Kim et al. [50] | − | − | − | + | + | − | − | + | C |
| Ouchi et al. [51] | − | − | + | + | + | + | − | + | C |
| Purushothaman et al. [13] | − | − | − | − | − | − | − | − | C |
| Rodrigues-De-Souza et al. [52] | − | + | − | + | + | + | − | + | C |
| Shmagel et al. [53] | + | − | − | + | + | − | − | + | C |
| Srivastava et al. [54] | − | − | − | − | + | + | − | + | C |
| Uchmanowicz et al. [55] | − | − | − | − | + | − | − | + | C |
| Wang et al. [56] | − | − | − | − | + | + | − | + | C |
| Yamada et al. [57] | − | + | − | + | + | + | − | + | C |
| Intervention | |
|---|---|
| A1 | Systematic review of at least two conducted independent of each other were of evidence level A2 |
| A2 | Randomized double-blinded comparative clinical research of good quality and efficient size |
| B | Comparative research but not with all characteristics as mentioned for A2. This includes also patient-control research and cohort research |
| C | Not comparative research |
| D | Opinion of experts |
| Conclusion Based On | |
|---|---|
| 1 | Research of evidence level A or at least two independently conducted studies of evidence level A |
| 2 | One research work of evidence level A2 or at least 2 independently conducted studies of evidence level B |
| 3 | One research work of evidence level B or C |
| 4 | Opinion of experts or inconclusive or inconsistent results between various studies |
| Study | Subjects | Outcome Measures | Association | Main Results | |
|---|---|---|---|---|---|
| Author Design | Sample Characteristics | Pain | Sleep | Between Sleep and Pain | Correlation Coefficient (r), Regression Coefficient (β or B),Odds Ratio (OR), Risk Ratio (RR) |
| Agmon et al. [33] Cohort study | Healthy subjects (A) No CBP at T1 and T2 n = 1356 Age 45.45 [8.50] ♀ 24% (B) No CBP at T1 n = 1527 Age 45.55 [8.53] ♀ 26% | Medical interview (CBP ≥ 3 m) T1: baseline T1 → T2: 18 m (range 11–19) T2 → T3: 17 m (range 11–29) | AIS (insomnia) | (A) 1. Insomnia at T1 → CBP at T3 relative to T2 2. Insomnia at T2 → CBP at T3 relative to T2 3. Change in insomnia from T1 to T2 → change in CBP from T2 to T3 (B) 1. Change in CBP from T1 to T2 → change in insomnia from T2 to T3 | (A) 1. No association: No insomnia: OR = 1 Insomnia: OR = 0.942, 95% CI = 0.72–1.24, NS (Model 1) 2. ↑ odds of CBP at T3 in patients with insomnia at T2: No insomnia: OR = 1 Insomnia: OR = 1.36, 95% CI = 1.27–1.51, p < 0.05 (Model 1) 3. ↑ odds of CBP at T3 relative to T2 in patients with ↑ insomnia severity from T1 to T2: No insomnia: OR =1 Insomnia: OR = 1.40, 95% CI = 1.10–1.71 (Model 2) (B) 1. No association: β = 0.02, NS Model 1: unadjusted Model 2: adjusted for age, gender, education level, PA intensity, self-rated health, smoking status, BMI, CRP, and time of FU |
| Artner et al. [11] Cross-sectional study | CLBP/CNP n = 1016 Age 57.07 [14.28] ♀ 56% | NRS (pain intensity) | ODQ (sleep deprivation intensity) | 1. Sleep deprivation intensity ~ pain intensity subgroups 2. Sleep deprivation intensity ~ pain intensity | 1. Difference between subgroups NRS < 5 vs. NRS ≥ 5: χ2 = 54.716, r = 0.303, p < 0.001 NRS < 5 vs. NRS > 7: χ2 = 65.664, r = 0.474, p < 0.001 2. + association: β = 0.236, p < 0.00001 |
| Bahouq et al. [12] Cross-sectional study | CLBP n = 100 Age 43.28 [7.5] ♀ 50% | VAS (pain intensity) | ISI (insomnia) | 1. Insomnia ~ pain intensity 2. Insomnia ~ CLBP duration 3. Pain intensity → insomnia | 1. + correlation: r = 0.587, p < 0.0001 2. No correlation: r = 0.001, NS 3. + association: β = 1.984, 95% CI = 1.517–2.451, p < 0.0001 |
| Burgess et al. [44] Cross-sectional study | CLBP n = 87 Age 40.0 [11.49] ♀ 64.4% | MPQ-SF (pain ratings) | PROMIS—SF8a (sleep disturbance) | 1. Sleep disturbance ~ pain intensity | 1. + correlation Sensory pain ratings: r = 0.44, p < 0.05 Affective pain ratings: r = 0.39, p < 0.05 VAS pain intensity: r = 0.51, p < 0.05 |
| Gerhart et al. [45] Cross-sectional study | CLBP n = 105 Age 46.30 [12.1] ♀ 48.6% | Self-reported questionnaire (pain intensity) 14 days, 5x/day between 8.50 a.m. and 8.50 p.m. | Self-reported questionnaire (sleep quality) | 1. Sleep quality ~ pain intensity 2. Prior night sleep quality → subsequent pain intensity 3. Prior night sleep quality → hour by hour pain intensity 4. Prior day pain intensity → subsequent sleep quality | 1. Correlation: r = −0.35, p < 0.01 2. Association: B = −0.16, p ≤ 0.00001 3. Association: 8:50 a.m.: B = −0.42, p < 0.00065 11:50 a.m.: B = −0.15, p < 0.01 No association: 2:50 p.m.: B = −0.07, NS 5:50 p.m.: B = −0.04, NS 8:50 p.m.: B = −0.09, NS 4. No association: NS Model adjusted for gender, age, employment, and disability compensation |
| Häggman-Henrikson et al. [39] Case-control study | Cases: CWAD n = 50 Age 39 [11] ♀ 78% Controls: Healthy subjects n = 50 Age- and sex-matched | Self-reported questionnaire (sleep problems) | 1. CWAD → sleep problems | 1. ↑ odds of sleep problems in CWAD: Controls: OR = 1 CWAD: OR = 15.58, 95% CI = 5.51–44.06, p < 0.0001 * | |
| Heffner et al. [40] Case-control study | Cases: CLBP n = 25 Age 30.82 [11.38] ♀ 60% Controls: Healthy subjects n = 25 Age- and sex-matched | MPQ-SF(pain ratings) | PSQI(sleep quality) | 1. Sleep quality past month ~ morning pain ratings in CLBP 2. Sleep quality past night ~ morning pain ratings in CLBP | 1. + correlation in CLBP: - Sensory pain ratings: r = 0.43, p = 0.03 - Affective pain ratings: r = 0.56, p = 0.004 - MPQ-SF total score: r = 0.51, p = 0.01 2. + correlation in CLBP: - Affective pain ratings: r = 0.47, p = 0.02 No correlation in CLBP:- Sensory pain ratings: NS- MPQ-SF total score: NS |
| Ho et al. [46] Cross-sectional study | Health survey n = 30,699Age 52.2 [15.2]♀ 54.3% | Self-reported questionnaire(CLBP) | Self-reported questionnaires(insomnia) | 1. Insomnia → CLBP | 1. ↑ odds of CLBP in patients with insomnia: No insomnia: OR = 1Insomnia: OR = 1.99, 95% CI = 1.79–2.21, p < 0.001 Model adjusted for age, BMI, sex, smoking, PA, depression, anxiety, and osteoarthritis |
| Hong et al. [41] Case-control study | Cases: CLBP n = 47Age 63.38 [9.55]♀ 59.6%Controls: Healthy subjects n = 44Age 63.64 [4.7] ♀ 63.6% | SF-36 bodily pain scale(bodily pain) | PSQI(sleep quality) | 1. Sleep quality ~ pain duration 2. CLBP → sleep disturbance | 1. No correlation: r = 0.015, NS 2. No association: Controls: OR = 1 CLBP: OR = 1.01, 95% CI = 0.43–2.37, NS * |
| Juan et al. [47] Cross-sectional study | CNP n = 231 Age 48.9 [13.9] ♀ 71.0% | VAS (pain intensity) | PSQI (sleep quality) | 1. Sleep quality ~ pain intensity 2. Pain intensity → sleep quality | 1. - correlation: r = 0.15, p < 0.05 2. EE = 0.136, CR = 1.994, p = 0.046 |
| Kääria et al. [34] Cohort study | Health survey No CNP at T1 n = 5277 ♀ 80.7% | Self-reported questionnaire (CNP) T1: baseline T2: 5–7 y | 4-item Jenkins Sleep Questionnaire (sleep problems) | 1. Rare/occasional sleep problems at T1 → CNP at T2 2. Frequent sleep problems at T1 → CNP at T2 | 1. ♀ ↑ odds of CNP in women with rare/occasional sleep problems: No sleep problems: OR = 1 OR = 1.28, 95% CI = 1.05–1.55 (Model 1); NS in Model 2 and 3 ♂ No association: NS in Model 1, 2, and 3 (No sleep problems: OR = 1) 2. ♀ ↑ odds of CNP in women with frequent sleep problems: No sleep problems: OR = 1 OR = 1.54, 95% CI = 1.22–1.95 (Model 3) ♂ ↑ odds of CNP in men with frequent sleep problems: No sleep problems: OR = 1 OR = 1.91, 95% CI = 1.10–3.33 (Model 1) NS in Model 2 and 3 ♀ /♂ Model 1: adjusted for age ♀ Model 2: adjusted for age, physical workload, emotional exhaustion, bullying, GHQ, sleep problems, acute NP, LBP, and BMI ♂ Model 2: adjusted for age, occupational class, emotional exhaustion, sleep problems, acute NP, and LBP ♀ Model 3: adjusted for age, bullying, sleep problems, acute NP, LBP, and BMI ♂ Model 3: adjusted for age, occupational class, emotional exhaustion, acute NP, and LBP |
| Kim et al. [49] Cross-sectional study | CLBP n = 481 Age 58.2 [16.7] ♀ 59% | NRS (pain intensity) Self-reported questionnaire (pain duration) | ISI (insomnia) | 1. Insomnia ~ pain duration 2. Pain intensity → insomnia | 1. No association: NS 2. ↑ odds of insomnia in patients with high pain intensity: <7 NRS: OR = 1 ≥7 NRS: OR = 2.342, 95% CI = 1.257–4.365, p = 0.007 Model adjusted for age, gender, pain intensity, comorbid neuropathic and musculoskeletal pain, anxiety, and depression |
| Kim et al. [50] Cross-sectional study | CNP n = 218 Age 52.8 [14.3] ♀ 56.9% | NRS (pain intensity) Self-reported questionnaire (pain duration) | ISI (insomnia) | 1. Insomnia ~ pain duration 2. Insomnia ~ pain intensity 3. Pain duration → clinical insomnia 4. Pain intensity → clinical insomnia | 1. No correlation: R = 0.094, NS 2. + correlation: R = 0.350, p < 0.001 3. No association: <1 y: OR = 1 ≥1 y: OR= 1.469, 95% CI 0.778–2.772), NS 4. ↑ odds of insomnia in patients with high pain intensity: <7 NRS: OR = 1 ≥7 NRS: OR = 2.457, 95% CI = 1.119–5.395, p = 0.025 Model adjusted for pain intensity, comorbid neuropathic and musculoskeletal pain, anxiety, and depression |
| Mork et al. [35] Cohort study | Health survey No CLBP/CNP at T1 n = 26,896 ♀ 50.2% | Self-reported questionnaire (CLBP and CNP/shoulder pain) T1: baseline T2: 11 y (range 9–13) | Self-reported questionnaire (sleep problems) | 1. Sleep problems at T1 → CLBP at T2 2. Sleep problems at T1 → CNP at T2 | 1. ↑ risk of CLBP in patients with sometimes or often/always sleep problems: Never: RR = 1 ♀ Sometimes: RR = 1.32, 95% CI = 1.22–1.43 ♂ Sometimes: RR = 1.30, 95% CI = 1.18–1.43 ♀ Often/always: RR = 1.66, 95% CI = 1.41–1.95 ♂ Often/always: RR = 1.51, 95% CI = 1.20–1.91 2. ↑ risk of CNP in patients with sometimes or often/always sleep problems: Never: RR = 1 ♀ Sometimes: RR = 1.31, 95% CI = 1.24–1.40 ♂ Sometimes: RR = 1.23, 95% CI = 1.15–1.33 ♀ Often/always: RR = 1.53, 95% CI = 1.35–1.74 ♂ Often/always: RR = 1.58, 95% CI = 1.35–1.86 Model adjusted for age, BMI, physical exercise, psychological well-being, smoking status, and occupation |
| O’Donoghue et al. [42] Case-control study | Cases: CLBP n = 15 Age 45.0 [11.53] ♀ 53% Controls: Healthy subjects n = 15 Age 38.46 [10.57] ♀ 53% | SF36-v2 bodily pain scale (pain intensity) | PSQI (sleep quality) ISI (insomnia) Actiwatch (TST, WASO, SOL, SE) | 1. Objective sleep~pain intensity 2. Sleep quality~pain intensity 3. Insomnia~pain intensity | 1. Correlation in CLBP: no description of correlation coefficient or p-value 2. Correlation in CLBP: r = -.59, p = 0.021 (strong correlation) 3. Correlation in CLBP: r = -.74, p = 0.001 (strong correlation) |
| Ouchi et al. [51] Cross-sectional study | Health survey CLBP n = 286 Age 40.5 [10.8] ♀ 46,5% | JOABPEQ (CLBP) | Self-reported questionnaire (sleep duration) | 1. CLBP → sleep duration | 1. No association with sleep duration of 7 to 8 h and ≥8 h ↑ odds of a sleep duration of <6 h in CLBP patients: 6–7 h: OR = 1 <6 h: OR = 1.402, 95% CI = 1.009–1.947, p = 0.044 7–8 h: OR 1.460, 95% CI = 0.974–2.188, NS ≥8 h: OR = 0.614, 95% CI = 0.320–1.178, NS |
| Pakpour et al. [36] Cohort study | CLBP n = 761 Age 41.15 [12.24] ♀ 44.6% | VAS (pain intensity, recovery) T1: baseline T2: 6 m | PSQI (sleep quality) | 1. Sleep problems at T1 → pain intensity at T2 2. Developing sleep problems → recovery from CLBP 3. Persistent sleep problems → recovery from CLBP 4. Resolving sleep problems → recovery from CLBP | 1. ↑ odds of pain intensity at T2 in patients with sleep problems at T1/ No sleep problems at T1: OR = 1 Sleep problems: OR = 2.48, 95% CI = 1.62–3.70 2. ↑ odds of non-recovery in terms of pain intensity for developing sleep problems: No sleep problems at T1 and T2: OR = 1 Developing sleep problems: OR = 2.88, 95% CI = 1.32–6.31 3. ↑ odds of non-recovery in terms of pain intensity for persistent sleep problems: No sleep problems at T1 and T2: OR = 1 Persistent sleep problems: OR = 3.45, 95% CI = 1.59–7.46 4. ↓ odds of non-recovery in terms of pain intensity for resolving sleep problems No sleep problems at T1 and T2: OR = 1 Resolving sleep problems: OR = 0.49, 95% CI = 0.26–0. 93 Model adjusted for baseline depressive symptoms, baseline pain intensity and duration, anxiety, age gender, BMI, and occupational status |
| Purushotaman et al. [13] Cross-sectional study | CBP n = 120 Age 55 ♀ 52.5% | NRS (pain intensity) | ISI (insomnia) | 1. Insomnia ~ pain intensity | 1. + correlation: r = 0.38, p < 0.001 |
| Rodrigues-De-Souza et al. [52] Cross-sectional study | CLBP Spain n = 30 Age 51.1 [13] ♀ 87.5 Brazil n = 30 Age 49.7 [10.5] ♀ 76.5 | NPRS (pain intensity) PRI (MPQ) (pain ratings) PPI (MPQ) (pain intensity) | PSQI (sleep quality) | 1. Sleep quality ~ pain intensity in Brazilian subjects 2. Sleep quality ~ pain intensity in Spanish subjects | 1. No correlation for NPRS, PRI, PPI: NS 2. + correlation NPRS: r = 0.364, p < 0.05 (weak correlation) PRI: r = 0.486, p < 0.01 (moderate correlation) No correlation for PPI: NS |
| Sezgin et al. [43] Case-control Study | Cases: CLBP n = 200 Age 50.2 [14.2] ♀ 50% Controls: Healthy subjects n = 200 Age 49.7 [13.6] ♀ 50% | MPQ-SF (pain intensity) Self-reported questionnaire (pain duration) | PSQI (sleep quality) | 1. CLBP → sleep quality 2. Sleep quality ~ pain duration 3. Sleep quality ~ pain intensity | 1. ↑ odds of poor sleep quality (PSQI > 5) in CLBP: Controls: OR = 1 CLBP: OR = 4.54, 95% CI = 2.98–6.91, p < 0.0001 * 2. ↑ daytime dysfunction in patients with pain duration > 11 y: p = 0.02 3. + correlation: Sensory pain ratings: r = 0.47, p < 0.001 Affective pain ratings: r = 0.35, p < 0.001 MPQ-SF total score: r = 0.47, p < 0.001 VAS: r = 0.34, p < 001 ETPI: r = 0.35, p < 001 |
| Shmagel et al. [53] Cross-sectional study | Health Survey n = 5103 ♀ 50.8% | Self-reported questionnaire (CLBP) | Self-reported questionnaire (sleep disturbance) | 1. CLBP → sleep disturbances | 1. ↑ odds of sleep disturbances in CLBP patients: No CLBP: OR = 1 CLBP: OR = 3.90; 95% CI = 3.22–4.73, p < 0.0001 Model adjusted for age, race, gender, and education |
| Skarpsno et al. [37] Cohort study | CLBP n = 6200 ♀ 59.9% | Self-reported questionnaire (CLBP) T1: baseline T2: ± 10 y | Self-reported questionnaire (sleeplessness) Self-reported questions (insomnia) | 1. Sleeplessness at T1 → recovery from CLBP at T2 2. Number of insomnia symptoms at T1 → recovery from CLBP at T2 | 1. ↑ risk of non-recovery from CLBP in ♀ and ♂ when experiencing sleeplessness often/always: Never/seldom: RR = 1 ♀ Often/always: RR = 0.65, 95% CI = 0.57–0.74 ♂ Often/always: RR = 0.81, 95% CI = 0.69–0.95 2. ↑ risk of non-recovery from CLBP in ♀ with ↑ number of insomnia symptoms No symptoms: RR = 1 ♀ 1 symptom: RR = 0.81, 95% CI = 0.72–0.91 ♀ 2 symptoms: RR = 0.68, 95% CI = 0.57–0.80 ♀ 3 symptoms: RR = 0.60, 95% CI = 0.46–0.77 No association in ♂: ♂ 1 symptom: RR = 0.99, 95% CI = 0.89–1.10 ♂ 2 symptoms: RR = 0.84, 95% CI = 0.71–1.00 ♂ 3 symptoms: RR = 0.82, 95% CI = 0.59–1.14 |
| Srivastava et al. [54] Cross-sectional | CLBP n = 100 ♀ 64% | Self-reported (pain duration) | PSQI (sleep quality) | 1. Sleep quality ~ pain duration | 1. No difference in sleep quality between pain duration ≤ 1 year and > 1 year: p = 0.06 |
| Uchmanowicz et al. [55] Cross-sectional study | CLBP n = 100 Age 49.53 [10.92] ♀ 62% | VAS (pain intensity) | AIS (insomnia) ESS (sleepiness) | 1. Insomnia ~ pain intensity 2. Insomnia ~ pain duration 3. Sleepiness ~ pain intensity 4. Sleepiness ~ pain duration 5. pain intensity → insomnia 6. pain duration → insomnia 7. pain duration → sleepiness | 1. + correlation: r = 0.462, p < 0.001 (weak correlation) 2. − correlation: r = −0.335, p = 0.001 (weak correlation) 3. + correlation: r = 0.233, p = 0.02 (very weak correlation) 4. - correlation: r = −0.307, p = 0.002 (weak correlation) 5. Pain intensity is an independent predictor of insomnia: R = 1.515, p < 0.001 6. Pain duration is an independent predictor of insomnia: R = −0.303, p = 0.009 7. Pain duration is an independent predictor of sleepiness: R = −0.247, p = 0.014 |
| Uhlig et al. [38] Cohort study | Health Survey No CLBP/CNP at T1 No insomnia at T1 n = 13,113 Age 43.4 [12.2] ♀ 54.8% Insomnia at T1 n = 316 Age 44.5 [12.2] ♀ 57.3% | Self-reported questionnaire (CLBP and CNP) T1: baseline T2: 11 y (range 9–13) | Self-reported questionnaire (insomnia) | 1. Insomnia at T1 → CLBP at T2 2. Insomnia at T1 → CNP at T2 | 1. ↑ risk of CLBP in T1 insomnia: No insomnia: RR = 1 Insomnia: RR = 1.36, 95% CI = 1.11–1.68 2. ↑ risk of CNP in T1 insomnia: No insomnia: RR = 1 Insomnia: RR = 1.34, 95% CI = 1.10–1.63 Model adjusted for sex, age, BMI, physical activity, education, HADS, and smoking |
| Wang et al. [56] Cross-sectional study | CLBP n = 225 Age 40.7 [11.4] ♀ 45.8% | VAS (pain intensity) | ISI (insomnia) | 1. Insomnia~severe CLBP 2. Severe CLBP → insomnia | 1. + correlation: r = 0.33, p < 0.01 2. ↑ odds of clinical insomnia in severe CLBP compared to no severe CLBP: No severe CLBP: OR = 1 Severe CLBP: OR = 2.80, 95% CI = 1.52–5.17, p = 0.001 |
| Yamada et al. [57] Cross-sectional study | Health survey n = 22,948 Age 52.1 [9.8] ♀ 96.8% | Self-reported questionnaire (CLBP) | Self-reported questionnaire (sleep sufficiency and duration) |
1. sleep sufficiency
→
CLBP 2. sleep duration → CLBP | 1. ↑ odds of CLBP in persons with lower sleep sufficiency: More than enough sleep: OR = 1 (Model 1) Enough sleep: OR = 1.68, 95% CI = 1.52–1.86, p < 0.001 Not enough sleep: OR = 2.65, 95% CI = 2.36–2.97, p < 0.001 No sleep at all: OR = 4.58, 95% CI = 3.62–5.81, p < 0.001 2. ↑ odds of CLBP in persons with sleep duration of <5 h and ≥5 h to <6 h: ≥6 h to <7 h: OR = 1 (Model 2) <5 h: OR = 1.44, 95% CI = 1.30–1.60, p < 0.001 ≥5 h to <6 h: OR = 1.11, 95% CI = 1.03–1.19, p < 0.01 ↓ odds of CLBP in persons with sleep duration of ≥7 h to <8 h: ≥6 h to <7 h: OR = 1 (Model 2) ≥7 h to <8 h: OR = 0.89, 95% CI = 0.80–0.98, p < 0.05 No association for sleep duration of ≥7 h to <8 h and ≥9 h: ≥8 h to <9 h: OR = 0.91, 95% CI = 0.75–1.12, NS ≥9 h: OR = 0.77, 95% CI = 0.44–1.33, NS Model 1: adjusted for age, sex, BMI, regular exercise, smoking, employment status, mood, anxiety, and sleep sufficiency Model 2: adjusted for age, sex, BMI, regular exercise, smoking, employment status, mood, and anxiety |
| Outcome | Assessment Tool | Construct | Time Span | Interpretation | Cut-Off Score | ||
|---|---|---|---|---|---|---|---|
| SLEEP | Sleep quality | Pittsburgh Sleep Quality Index (PSQI) [36,40,41,42,43,46,52,56] | 24 items 7 dimensions Total score ranging from 0 to 21 | Past month Past night [40] | ↑ scores = ↓ sleep quality | ≥5 [36] >5 [41,42] >6 [40] >8 [52] | Clinical sleep disturbance Sleep disturbance Clinical sleep disturbance Poor sleep quality |
| Self-reported questionnaire [52] Rate the overall quality of your sleep. | 5-point Likert scale | past night | 0—not at all restful 1—a little restful 2—somewhat restful 3—very restful 4—extremely restful | ||||
| Insomnia | Insomnia Severity Index (ISI) [12,13,42,48,49,50,54,56] | 7 items 5-point Likert scale Total score ranging from 0 to 28 | Past 2 weeks | ↑ scores = ↑ insomnia severity 0–7 no clinically significant insomnia 8–14 sub-threshold insomnia [12,13,42,49,50,56] 15–21 clinical insomnia (moderate severity) [12,13,42,49,50,56] 22–28 clinical insomnia (severe) | 14 [13,59] >15 [57] ≥15 [49,56] | Primary insomnia Clinical insomnia Clinical insomnia | |
| Athens Insomnia Scale (AIS) AIS-5 [33] AIS-8 [47] | Past month | ↑ scores = ↑ insomnia severity | ≥6 [47] | Insomnia | |||
| Self-reported question(s) How often during the last 3 months have you: (1) Had difficulty falling asleep at night? (2) Woken up repeatedly during the night? (3) Woken too early and could not get back to sleep? (4) Felt sleepy during the day? [55] (1) Have you had problems falling asleep during the last month, (2) During the last month, did you ever wake up too early, not being able to fall asleep again? (3) During the last year, have you been troubled by sleepiness to such a degree that it affected your work? [37,38] | Past 3 months Past month | (1–3) never/seldom, sometimes, several times a week (1–2) never, occasionally/sometimes, often, almost every night (3) yes, no | Insomnia if person answered several times a week to question 4 and at least one of questions 1–3; Insomnia if person answered often or almost every night to questions 1 and 2 or yes to question 3 | ||||
| Sleep disturbance/problems/sleeplessness | PROMIS sleep disturbance—short form 8a [51] | 5-point Likert scale | Past week | ↑ scores = ↑ sleep disturbance | T score > 50 | disturbed sleep | |
| 4-item Jenkins Sleep Questionnaire (JSQ) [34] | 6-point Likert scale | Past 4 weeks | ↑ scores = ↑ sleep disturbance 1—not at all 2—1 to 3 days 3—4 to 7 days 4—8 to 14 days 5—15 to 21 days 6—22 to 28 days | Rare to occasional sleep problems if any of the problems occurred 1–14 times; frequent sleep problems if any of the problems occurred ≥ 15 times | |||
| Self-reported question During the last month, have you had any problems falling asleep or sleep problems? [35] Sleep problems [39] Have you ever told a doctor or other health professional that you have trouble sleeping? [45] How often do you suffer from sleeplessness? [37] | Past month | (1) never, sometimes, often, almost every night 0—no, never 1—yes, seldom, every year 2—yes, often, every month 3—yes, very often, every week 4—yes, always, every day 1—never, or just a few times a year 2—1–2 times a month 3—approximately once a week 4—more than once a week | 1 or 2 3 or 4 | Low frequency Frequent | |||
| Sleep deprivation intensity | Oswestry Disability Questionnaire (ODQ) [11] | 10 items 6-point Likert scale | No disturbance No disturbance when taking analgesics Sleep < 6 h even when using analgesics Severe sleep deprivation (<4 h) due to pain, even when using analgesics | ||||
| Sleep sufficiency | Self-reported questionnaire Sleep sufficiency [60] | Past month | Not at all Not enough Enough More than enough | ||||
| Sleep duration | Self-reported questionnaire Sleep duration [44] Average sleep duration [50] | Past month | <6 h per night 6–7 h per night 7–8 h per night ≥8 h per night <5 h ≥5 to <6 h ≥6 to <7 h ≥7 to <8 h ≥8 to <9 h ≥9 h | ||||
| Daytime sleepiness | Epworth Sleepiness Scale (ESS) [12] | 8 questions 4-point scale Global score ranging from 0 to 24 | Recent times (past few weeks to few months) | ↑ scores = ↑ level of daytime sleepiness 0–5 lower normal daytime sleepiness 6–10 higher normal daytime sleepiness 11–12 mild excessive daytime sleepiness 13–15 moderate excessive daytime sleepiness 16–24 severe excessive daytime sleepiness | |||
| Objective sleep parameters | Actiwatch [36] Total sleep time, awakenings after sleep onset, sleep onset latency, sleep efficiency | Sleep efficiency < 85% | sleep disturbance | ||||
| PAIN | Pain intensity | McGill Pain Questionnaire short form (MPQ-SF) [13,40,48,54] | 3 subscales Sensory and affective pain ratings on 4-point rating scale Pain intensity | Current Past month [54] | ↑ scores = ↑ pain | ||
| Numeric (Pain) Rating Scale (NPRS) [13,42,49,50,52,56] | Single item | Past week | ↑ scores = ↑ pain intensity Scale from 0 (no pain) to 10 (pain as bad as it could be/worst imaginable pain) | ||||
| Visual Analogue Scale (VAS) [12,33,41,43,47] | Single 11-point item | Current Past week | ↑ scores = ↑ pain intensity 0–4 no pain 5–44 mild pain 45–74 moderate pain 75–100 severe pain | ||||
| SF-36 Bodily Pain Scale (BPS) [54] | Past 4 weeks | ↑ scores = ↑ bodily pain | |||||
| Self-reported questionnaire [48] How intense was your pain? | 9-point scale | Past 3 h | 0—not at all 2—somewhat 4—much 6—very much 8—extremely | ||||
| Pain duration | Self-reported questionnaire [13,42,56] Duration of pain | <1 year ≥1 year | |||||
| Pain | Sleep | Association | Strength of Conclusion | |
|---|---|---|---|---|
| CLBP | CNP | |||
| Pain intensity | Sleep quality | − | ** [40,42,43,45,52] | * [47] |
| Insomnia severity | + | ** [12,13,42,49,55,56] | * [50] | |
| Sleep disturbance Sleep duration Sleepiness Objective TST and SE Objective SOL and WASO | + | * [44] | * [11] | |
| − | * [11] | |||
| + | * [55] | |||
| − | * [42] | |||
| + | * [42] | |||
| Pain duration | Sleep quality Insomnia severity Insomnia severity Sleepiness | No | ** [41,43,54] | * [50] |
| No | * [12,49] | |||
| − | * [55] | |||
| − | * [55] | |||
| ↑ odds of CLBP versus controls | Insomnia severity Sleep duration Sleep sufficiency | + | * [46] | |
| − | * [51,57] | |||
| − | * [57] | |||
| CLBP | ↑ odds of poor sleep quality versus good sleep quality ↑ odds of sleep disturbances versus no sleep disturbances | − | * [43] | |
| + | * [41] | |||
| CNP (whiplash) | ↑ odds of sleep problems versus no sleep problems | + | * [39] | |
| Independent Variable | Dependent Variable | Association | Strength of Conclusion | |
|---|---|---|---|---|
| CLBP | CNP | |||
| Sleep problems | Occurrence of CSP | + | ** [33,35,38] | ** [34,35,38] |
| Pain intensity at FU | + | * [36] | ||
| Odds of non-recovery | + | * [36] | ||
| Insomnia symptoms | Risk of non-recovery | + | * [37] | |
| CLBP | Insomnia | No | * [33] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Looveren, E.; Bilterys, T.; Munneke, W.; Cagnie, B.; Ickmans, K.; Mairesse, O.; Malfliet, A.; De Baets, L.; Nijs, J.; Goubert, D.; et al. The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade. J. Clin. Med. 2021, 10, 3836. https://doi.org/10.3390/jcm10173836
Van Looveren E, Bilterys T, Munneke W, Cagnie B, Ickmans K, Mairesse O, Malfliet A, De Baets L, Nijs J, Goubert D, et al. The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade. Journal of Clinical Medicine. 2021; 10(17):3836. https://doi.org/10.3390/jcm10173836
Chicago/Turabian StyleVan Looveren, Eveline, Thomas Bilterys, Wouter Munneke, Barbara Cagnie, Kelly Ickmans, Olivier Mairesse, Anneleen Malfliet, Liesbet De Baets, Jo Nijs, Dorien Goubert, and et al. 2021. "The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade" Journal of Clinical Medicine 10, no. 17: 3836. https://doi.org/10.3390/jcm10173836
APA StyleVan Looveren, E., Bilterys, T., Munneke, W., Cagnie, B., Ickmans, K., Mairesse, O., Malfliet, A., De Baets, L., Nijs, J., Goubert, D., Danneels, L., Moens, M., & Meeus, M. (2021). The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade. Journal of Clinical Medicine, 10(17), 3836. https://doi.org/10.3390/jcm10173836







