Neck Active Movements Assessment in Women with Episodic and Chronic Migraine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants Selection
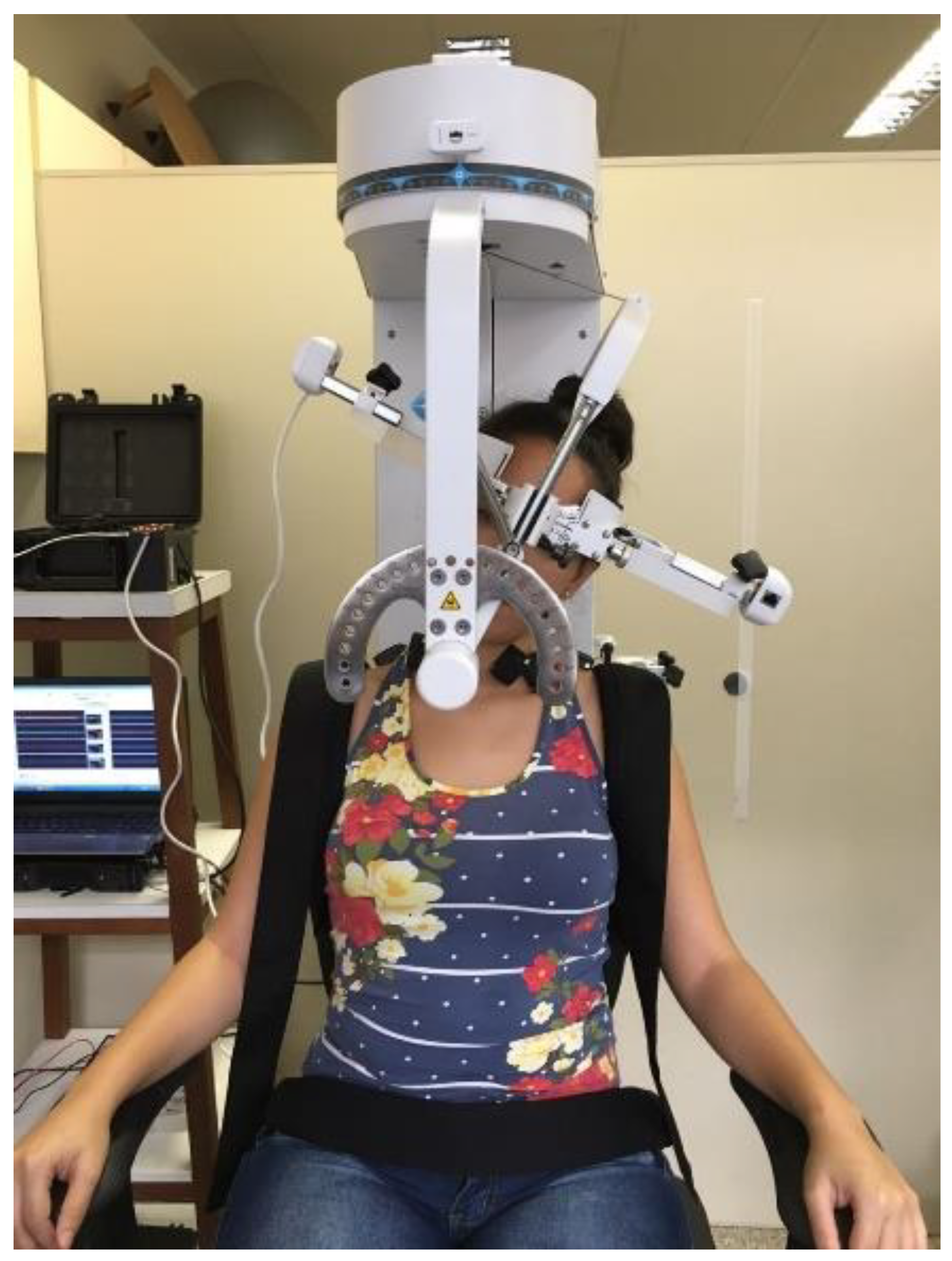
2.2. Instrumentation
2.3. Procedures
2.4. Data Processing
2.5. Statistical Analysis
3. Results
3.1. Demographics
3.2. Cervical ROM and Angular Velocity
3.3. Percentage of Activation
3.4. Correlations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steiner, T.J.; Stovner, L.J.; Jensen, R.; Uluduz, D.; Katsarava, Z. Lifting The Burden: The Global Campaign against Headache. Migraine remains second among the world’s causes of disability, and first among young women: Findings from GBD2019. J. Headache Pain 2020, 21, 137. [Google Scholar] [CrossRef] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd ed. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Burch, R.C.; Buse, D.C.; Lipton, R.B. Migraine: Epidemiology, Burden, and Comorbidity. Neurol. Clin. 2019, 37, 631–649. [Google Scholar] [CrossRef] [PubMed]
- Lipton, R.B.; Fanning, K.M.; Buse, D.C.; Martin, V.T.; Reed, M.L.; Adams, A.M.; Goadsby, P.J. Identifying Natural Subgroups of Migraine Based on Comorbidity and Concomitant Condition Profiles: Results of the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache 2018, 58, 933–947. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Holland, P.R.; Martins-Oliveira, M.; Hoffmann, J.; Schankin, C.; Akerman, S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol. Rev. 2017, 97, 553–622. [Google Scholar] [CrossRef] [PubMed]
- Aguila, M.R.; Rebbeck, T.; Pope, A.; Ng, K.; Leaver, A.M. Six-month clinical course and factors associated with non-improvement in migraine and non-migraine headaches. Cephalalgia 2018, 38, 1672–1686. [Google Scholar] [CrossRef] [PubMed]
- Ford, S.; Calhoun, A.; Kahn, K.; Mann, J.; Finkel, A. Predictors of disability in migraineurs referred to a tertiary clinic: Neck pain, headache characteristics, and coping behaviors. Headache 2008, 48, 523–528. [Google Scholar] [CrossRef]
- Charles, A. The pathophysiology of migraine: Implications for clinical management. Lancet Neurol. 2018, 17, 174–182. [Google Scholar] [CrossRef]
- Liang, Z.; Galea, O.; Thomas, L.; Jull, G.; Treleaven, J. Cervical musculoskeletal impairments in migraine and tension type headache: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2019, 42, 67–83. [Google Scholar] [CrossRef]
- Szikszay, T.M.; Hoenick, S.; von Korn, K.; Meise, R.; Schwarz, A.; Starke, W.; Luedtke, K. Which Examination Tests Detect Differences in Cervical Musculoskeletal Impairments in People With Migraine? A Systematic Review and Meta-Analysis. Phys. Ther. 2019, 99, 549–569. [Google Scholar] [CrossRef]
- Oliveira-Souza, A.I.S.; Florencio, L.L.; Carvalho, G.F.; Fernández-de-Las-Peñas, C.; Dach, F.; Bevilaqua-Grossi, D. Reduced flexion rotation test in women with chronic and episodic migraine. Braz. J. Phys. Ther. 2019, 23, 387–394. [Google Scholar] [CrossRef]
- Bevilaqua-Grossi, D.; Pegoretti, K.S.; Goncalves, M.C.; Speciali, J.G.; Bordini, C.A.; Bigal, M.E. Cervical mobility in women with migraine. Headache 2009, 49, 726–731. [Google Scholar] [CrossRef]
- Ferracini, G.N.; Florencio, L.L.; Dach, F.; Bevilaqua-Grossi, D.; Palacios-Ceña, M.; Ordás-Bandera, C.; Chaves, T.C.; Speciali, J.G.; Fernández-de-las-Peñas, C. Musculoskeletal disorders of the upper cervical spine in women with episodic or chronic migraine. Eur. J. Phys. Rehabil. Med. 2017, 53, 342–350. [Google Scholar] [CrossRef]
- Carvalho, G.F.; Chaves, T.C.; Gonçalves, M.C.; Florencio, L.L.; Braz, C.A.; Dach, F.; Fernández-de-las-Peñas, C.; Bevilaqua-Grossi, D. Comparison between neck pain disability and cervical range of motion in patients with episodic and chronic migraine: A cross-sectional study. J. Manip. Physiol. Ther. 2014, 37, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Luedtke, K.; Starke, W.; May, A. Musculoskeletal dysfunction in migraine patients. Cephalalgia 2018, 38, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Benatto, M.T.; Bevilaqua-Grossi, D.; Carvalho, G.F.; Bragatto, M.M.; Pinheiro, C.F.; Lodovichi, S.S.; Dach, F.; Fernández-de-las-Peñas, C.; Florencio, L.L. Kinesiophobia Is Associated with Migraine. Pain Med. 2019, 20, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Martins, I.P.; Gouveia, R.G.; Parreira, E. Kinesiophobia in migraine. J. Pain 2006, 7, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Salehi, R.; Rasouli, O.; Saadat, M.; Mehravar, M.; Negahban, H.; Shaterzadeh, M.J. Cervical movement kinematic analysis in patients with chronic neck pain: A comparative study with healthy subjects. Musculoskelet. Sci. Pract. 2021, 53, 102377. [Google Scholar] [CrossRef]
- Vikne, H.; Bakke, E.S.; Liestøl, K.; Engen, S.R.; Vøllestad, N. Muscle activity and head kinematics in unconstrained movements in subjects with chronic neck pain; cervical motor dysfunction or low exertion motor output? BMC Musculoskelet. Disord. 2013, 4, 314. [Google Scholar] [CrossRef] [Green Version]
- Tsang, S.M.; Szeto, G.P.; Lee, R.Y. Altered spinal kinematics and muscle recruitment pattern of the cervical and thoracic spine in people with chronic neck pain during functional task. J. Electromyogr. Kinesiol. 2014, 24, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Benatto, M.T.; Florencio, L.L.; Bragatto, M.M.; Lodovichi, S.S.; Dach, F.; Bevilaqua-Grossi, D. Extensor/flexor ratio of neck muscle strength and electromyographic activity of individuals with migraine: A cross-sectional study. Eur. Spine J. 2019, 28, 2311–2318. [Google Scholar] [CrossRef] [PubMed]
- Florencio, L.L.; Oliveira, A.S.; Lemos, T.W.; Carvalho, G.F.; Dach, F.; Bigal, M.E.; Falla, D.; Fernández-de-las-Peñas, C.; Bevilaqua-Grossi, D. Patients with chronic, but not episodic, migraine display altered activity of their neck extensor muscles. J. Electromyogr. Kinesiol. 2016, 30, 66–72. [Google Scholar] [CrossRef]
- Florencio, L.L.; Oliveira, A.S.; Carvalho, G.F.; Tolentino, G.A.; Dach, F.; Bigal, M.E.; Fernández-de-las-Peñas, C.; Bevilaqua-Grossi, D. Cervical Muscle Strength and Muscle Coactivation During Isometric Contractions in Patients With Migraine: A Cross-Sectional Study. Headache 2015, 55, 1312–1322. [Google Scholar] [CrossRef]
- Chiu, T.T.; Sing, K.L. Evaluation of cervical range of motion and isometric neck muscle strength: Reliability and validity. Clin. Rehabil. 2002, 16, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Cook, C.; Richardson, J.K.; Braga, L.; Menezes, A.; Soler, X.; Kume, P.; Zaninelli, M.; Socolows, F.; Pietrobon, R. Cross-cultural adaptation and validation of the Brazilian Portuguese version of the Neck Disability Index and Neck Pain and Disability Scale. Spine (Phila Pa 1976) 2006, 31, 1621–1627. [Google Scholar] [CrossRef] [PubMed]
- Souza, F.S.; Marinho, C.S.; Siqueira, F.B.; Maher, C.G.; Costa, L.O. Psychometric testing confirms that the Brazilian-Portuguese adaptations, the original versions of the Fear-Avoidance Beliefs Questionnaire, and the Tampa Scale of Kinesiophobia have similar measurement properties. Spine (Phila Pa 1976) 2008, 33, 1028–1033. [Google Scholar] [CrossRef]
- Vernon, H. The Neck Disability Index: State-of-the-art, 1991-2008. J. Manip. Physiol. Ther. 2008, 31, 491–502. [Google Scholar] [CrossRef]
- Jorritsma, W.; Dijkstra, P.U.; de Vries, G.E.; Geertzen, J.H.; Reneman, M.F. Detecting relevant changes and responsiveness of Neck Pain and Disability Scale and Neck Disability Index. Eur. Spine J. 2012, 21, 2550–2557. [Google Scholar] [CrossRef] [Green Version]
- Schellingerhout, J.M.; Verhagen, A.P.; Heymans, M.W.; Koes, B.W.; de Vet, H.C.; Terwee, C.B. Measurement properties of disease-specific questionnaires in patients with neck pain: A systematic review. Qual. Life Res. 2012, 21, 659–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vlaeyen, J.W.; Kole-Snijders, A.M.; Rotteveel, A.M.; Ruesink, R.; Heuts, P.H. The role of fear of movement/(re)injury in pain disability. J. Occup. Rehabil. 1995, 5, 235–252. [Google Scholar] [CrossRef]
- Falla, D.; Dall’Alba, P.; Rainoldi, A.; Merletti, R.; Jull, G. Location of innervation zones of sternocleidomastoid and scalene muscles--a basis for clinical and research electromyography applications. Clin. Neurophysiol. 2002, 113, 57–63. [Google Scholar] [CrossRef]
- Joines, S.M.; Sommerich, C.M.; Mirka, G.A.; Wilson, J.R.; Moon, S.D. Low-level exertions of the neck musculature: A study of research methods. J. Electromyogr. Kinesiol. 2006, 16, 485–497. [Google Scholar] [CrossRef]
- Surface ElectroMyoGraphy for the Non-Invasive Assessment of Muscles. Available online: http://www.seniam.org (accessed on 2 June 2014).
- Tsang, S.M.; Szeto, G.P.; Lee, R.Y. Relationship between neck acceleration and muscle activation in people with chronic neck pain: Implications for functional disability. Clin. Biomech. 2016, 35, 27–36. [Google Scholar] [CrossRef]
- Hodges, P.W.; Bui, B.H. A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electroencephalogr. Clin. Neurophysiol. 1996, 101, 511–519. [Google Scholar] [CrossRef]
- Domholdt, E. Physical Therapy Research: Principles and Applications, 2nd ed.; WB Saunders Co.: Philadelphia, PA, USA, 2000. [Google Scholar]
- Sarig Bahat, H.; Chen, X.; Reznik, D.; Kodesh, E.; Treleaven, J. Interactive cervical motion kinematics: Sensitivity, specificity and clinically significant values for identifying kinematic impairments in patients with chronic neck pain. Man. Ther. 2015, 20, 295–302. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, G.F.; Vianna-Bell, F.H.; Florencio, L.L.; Pinheiro, C.F.; Dach, F.; Bigal, M.E.; Bevilaqua-Grossi, D. Presence of vestibular symptoms and related disability in migraine with and without aura and chronic migraine. Cephalalgia 2019, 39, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Sarig Bahat, H.; Weiss, P.L.; Sprecher, E.; Krasovsky, A.; Laufer, Y. Do neck kinematics correlate with pain intensity, neck disability or with fear of motion? Man. Ther. 2014, 19, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Meise, R.; Lüdtke, K.; Probst, A.; Stude, P.; Schöttker-Königer, T. Zervikaler “joint position error” bei Kopfschmerzen: Systematische Literaturübersicht und empirische Daten bei chronischer Migräne [Joint position error in patients with headache: Systematic review of the literature and experimental data for patients with chronic migraine]. Schmerz 2019, 33, 204–211. (In German) [Google Scholar] [CrossRef]
- Sjölander, P.; Michaelson, P.; Jaric, S.; Djupsjöbacka, M. Sensorimotor disturbances in chronic neck pain--range of motion, peak velocity, smoothness of movement, and repositioning acuity. Man. Ther. 2008, 13, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Florencio, L.L.; Oliveira, A.S.; Will-Lemos, T.; Pinheiro, C.F.; Marçal, J.C.D.S.; Dach, F.; Fernández-de-Las-Peñas, C.; Bevilaqua-Grossi, D. Muscle endurance and cervical electromyographic activity during submaximal efforts in women with and without migraine. Clin. Biomech. 2021, 82, 105276. [Google Scholar] [CrossRef] [PubMed]
- Bragatto, M.M.; Bevilaqua-Grossi, D.; Benatto, M.T.; Lodovichi, S.S.; Pinheiro, C.F.; Carvalho, G.F.; Dach, F.; Fernández-de-las-Peñas, C.; Florencio, L.L. Is the presence of neck pain associated with more severe clinical presentation in patients with migraine? A cross-sectional study. Cephalalgia 2019, 39, 1500–1508. [Google Scholar] [CrossRef] [PubMed]

| Control Group (n = 27) | Episodic Migraine (n = 27) | Chronic Migraine (n = 27) | |
|---|---|---|---|
| Age (years) | 31.2 (9.17) | 33.0 (9.05) | 35.5 (10.27) |
| BMI (kg/cm²) | 25.0 (4.00) | 23.7 (3.89) | 23.9 (2.95) |
| Years with migraine | - | 14.1 (8.33) | 18.1 (11.55) |
| Migraine frequency (days/month) | - | 6.7 (3.29) | 24.5 (5.66) |
| Migraine intensity (NPRS) | - | 7.6 (1.49) | 8.0 (1.57) |
| Self-report of neck pain † | 7 (25.9%) | 18 (66.7%) | 21 (77.8%) |
| Years with neck pain | 3.6 (2.17) | 9.2 (4.58) | 8.4 (6.82) |
| Neck pain frequency (days/month) | 13.9 (11.34) | 12.5 (10.70) | 20.5 (8.64) ** |
| Neck pain intensity (NPRS) | 4.4 (1.27) | 5.5 (2.01) | 5.8 (2.18) |
| NDI score | 11.1 (11.65) | 24.9 (11.58) | 35.1 (14.66) * |
| TSK score | 28.7 (7.53) | 36.1 (8.05) * | 37.2 (9.14) * |
| Control Group (n = 27) | Episodic Migraine (n = 27) | Chronic Migraine (n = 27) | |
|---|---|---|---|
| Cervical range of motion (degrees) | |||
| Total range of motion | 310.7 (28.39) | 280.21 (37.01) * | 280.65 (47.39) * |
| Flexion | 58.0 (6.91) | 53.8 (7.68) | 55.5 (12.68) |
| Extension | 59.7 (7.49) | 53.9 (9.71) | 55.2 (9.59) |
| Right lateral flexion | 51.6 (8.26) | 46.3 (7.42) | 46.6 (9.80) |
| Left lateral flexion | 51.0 (7.68) | 46.1 (8.26) | 43.4 (10.53) * |
| Right rotation | 73.0 (8.50) | 65.1 (9.29) * | 65.9 (14.40) |
| Left rotation | 68.9 (11.93) | 61.3 (12.21) | 60.7 (15.81) |
| Angular velocity (degrees/s) | |||
| Mean angular velocity of cervical moviment | 26.60 (4.62) | 22.67 (4.72) * | 22.09 (5.84) * |
| Flexion | 27.17 (5.43) | 23.2 (5.07) | 23.0 (7.34) * |
| Extension | 25.33 (5.51) | 22.7 (5.78) | 22.2 (4.57) |
| Right lateral flexion | 23.07 (5.31) | 19.7 (4.90) | 19.2 (5.80) * |
| Left lateral flexion | 22.9 (5.77) | 19.2 (5.10) | 18.8 (6.13) * |
| Right rotation | 30.4 (5.82) | 26.2 (6.48) | 26.4 (9.44) |
| Left rotation | 30.7 (5.86) | 25.0 (6.57) * | 25.3 (8.04) * |
| Total Cervical Range of Motion (°) | Angular Velocity (°/s) | |
|---|---|---|
| Total sample (n = 81) | ||
| NDI scores | −0.25 * (−0.48 to −0.04) | −0.28 (−0.50 to −0.06) * |
| TSK scores | −0.30 * (−0.51 to −0.08) | −0.40 (−0.60 to −0.19) ** |
| Participants with migraine (n = 54) | ||
| Years with migraine | −0.003 (−0.32 to 0.32) | 0.01 (−0.28 to 0.31) |
| Migraine frequency (days/month) | 0.14 (−0.16 to 0.47) | 0.04 (−0.25 to 0.34) |
| Migraine intensity (NPRS) | 0.13 (−0.39 to 1.07) | 0.02 (−0.64 to 0.74) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinheiro, C.F.; Oliveira, A.S.; Will-Lemos, T.; Florencio, L.L.; Fernández-de-las-Peñas, C.; Dach, F.; Bevilaqua-Grossi, D. Neck Active Movements Assessment in Women with Episodic and Chronic Migraine. J. Clin. Med. 2021, 10, 3805. https://doi.org/10.3390/jcm10173805
Pinheiro CF, Oliveira AS, Will-Lemos T, Florencio LL, Fernández-de-las-Peñas C, Dach F, Bevilaqua-Grossi D. Neck Active Movements Assessment in Women with Episodic and Chronic Migraine. Journal of Clinical Medicine. 2021; 10(17):3805. https://doi.org/10.3390/jcm10173805
Chicago/Turabian StylePinheiro, Carina F., Anamaria S. Oliveira, Tenysson Will-Lemos, Lidiane L. Florencio, César Fernández-de-las-Peñas, Fabiola Dach, and Débora Bevilaqua-Grossi. 2021. "Neck Active Movements Assessment in Women with Episodic and Chronic Migraine" Journal of Clinical Medicine 10, no. 17: 3805. https://doi.org/10.3390/jcm10173805
APA StylePinheiro, C. F., Oliveira, A. S., Will-Lemos, T., Florencio, L. L., Fernández-de-las-Peñas, C., Dach, F., & Bevilaqua-Grossi, D. (2021). Neck Active Movements Assessment in Women with Episodic and Chronic Migraine. Journal of Clinical Medicine, 10(17), 3805. https://doi.org/10.3390/jcm10173805









