Gastrointestinal Residue Removal Using a Balloon Overtube under Ultrathin Endoscopic Navigation: Ex Vivo and In Vivo Experimental Studies
Abstract
:1. Introduction
2. Materials and Methods
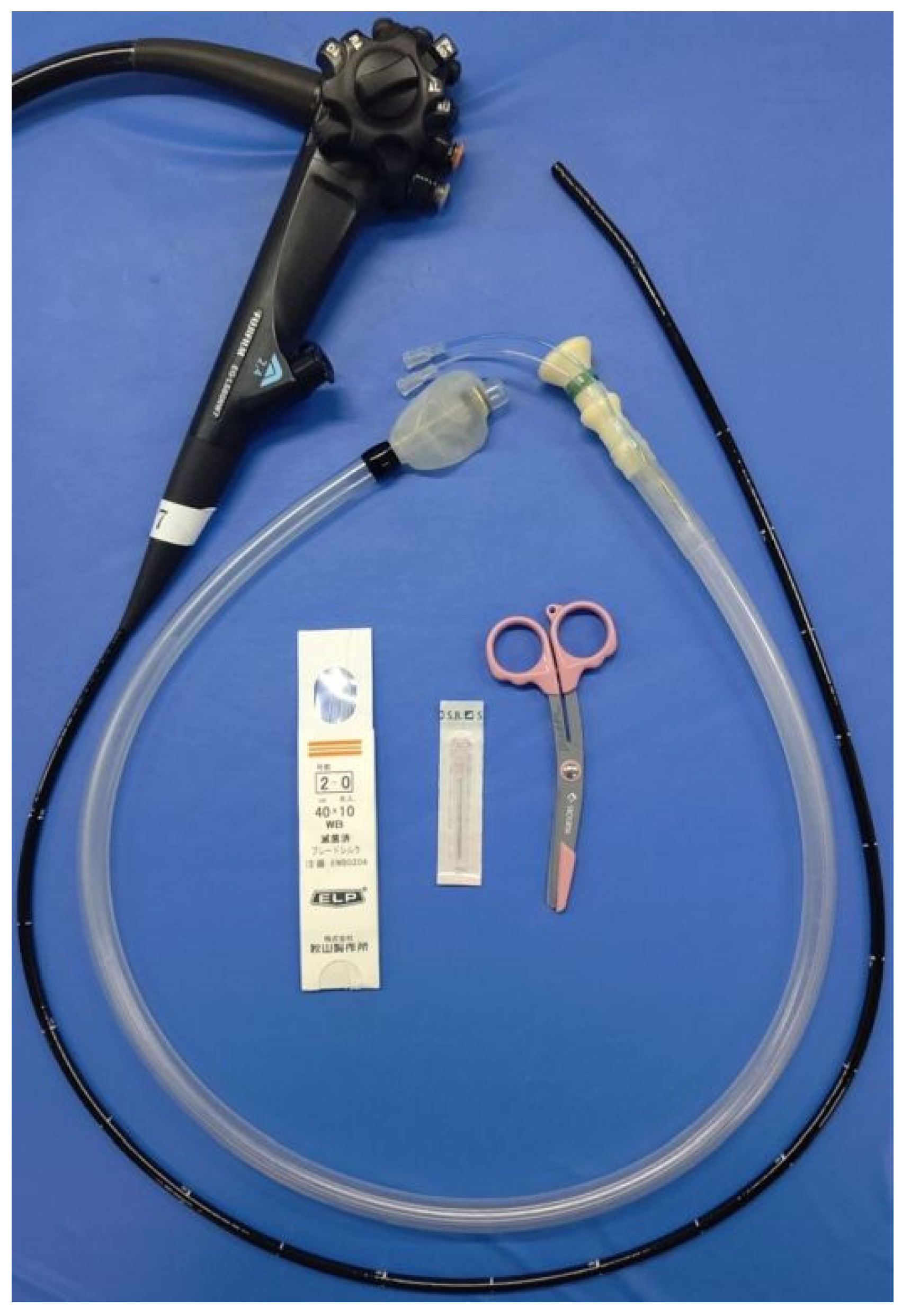
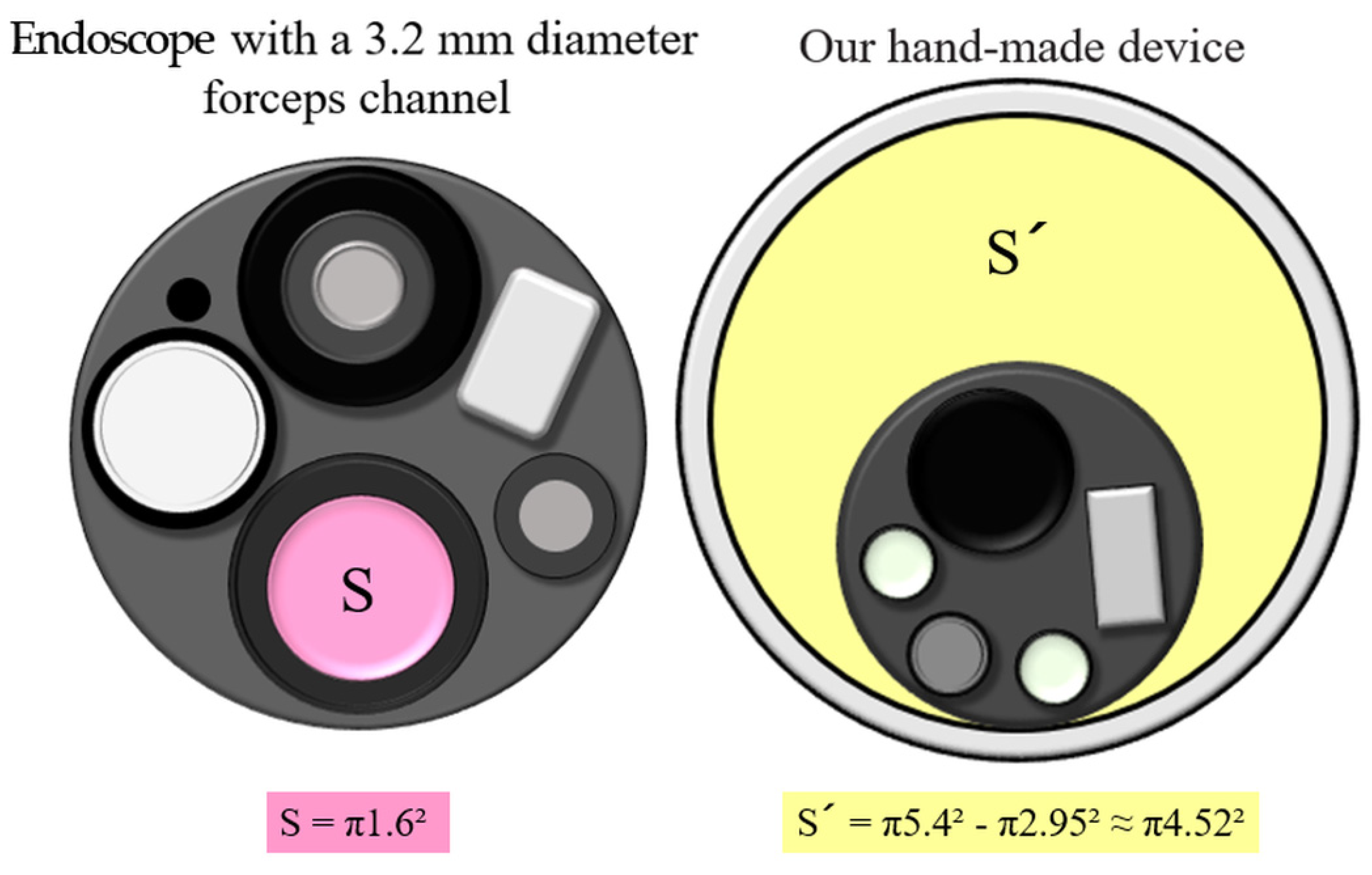
2.1. Experimental Equipment
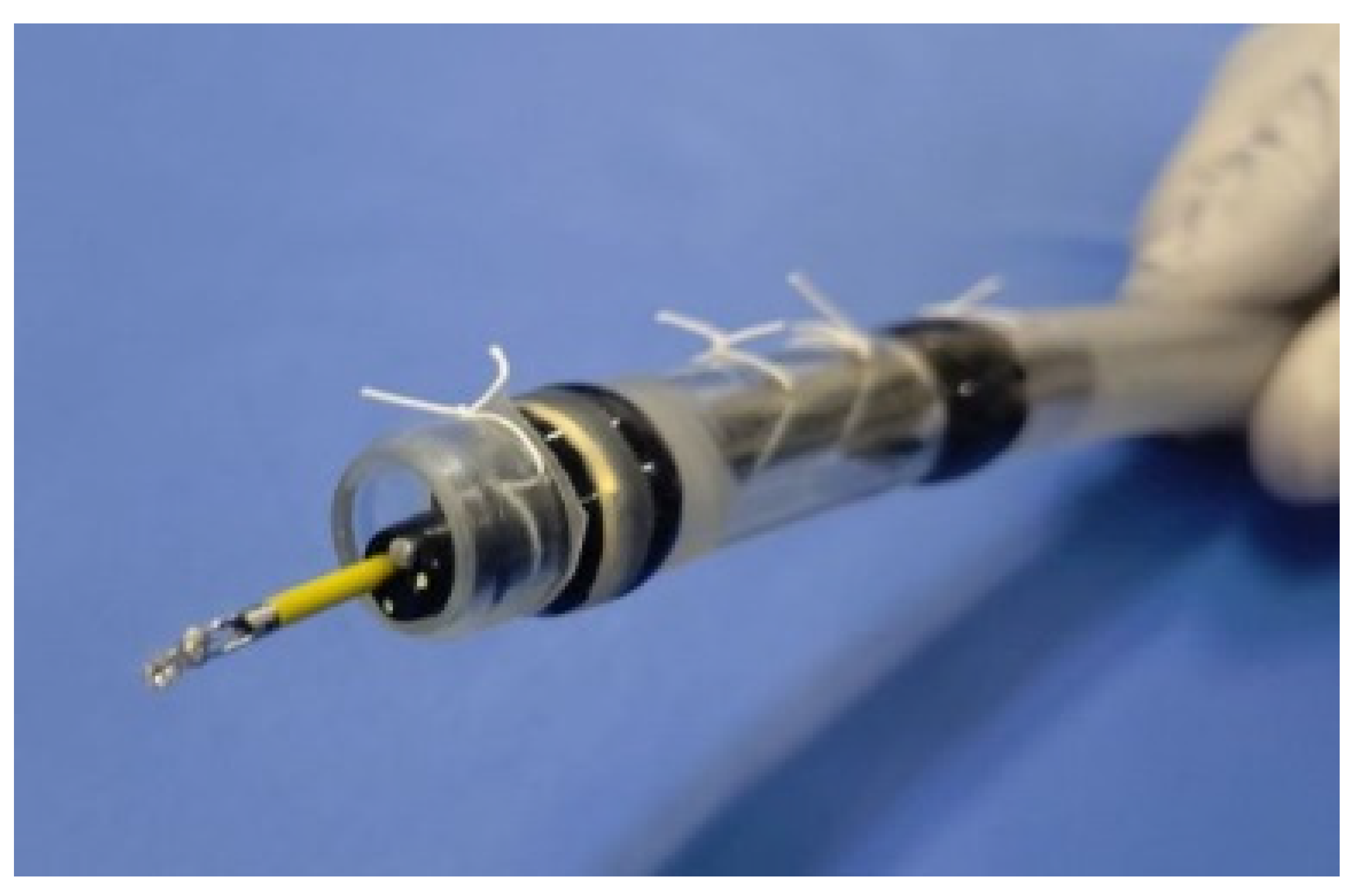
2.2. Preparations
- Step 1: Removal of the overtube-mounted balloon part using scissors (Figure 2A);
- Step 2: A 10 × 10 mm cross incision was made with scissors 10 cm from the base of the overtube, and the ultrathin endoscope was inserted into the tube. For endoscopy, sterile lubricating gel was applied to the opening so that the endoscope could be easily inserted (Figure 2B–D);
- Step 3: The endoscope was fixed 2 mm from the distal tip of the overtube through the incision hole and was connected by using silk thread at four points. In detail, the tube was pierced with an 18-G needle to avoid damaging the scope and was fixed by passing a silk thread through the needle (Figure 2E,F);
- Step 4: The cross-incision was reinforced with vinyl tape to prevent the loss of suction pressure (Figure 2G);
- Step 5: The suction tube was connected to the base of the overtube (Figure 2H).
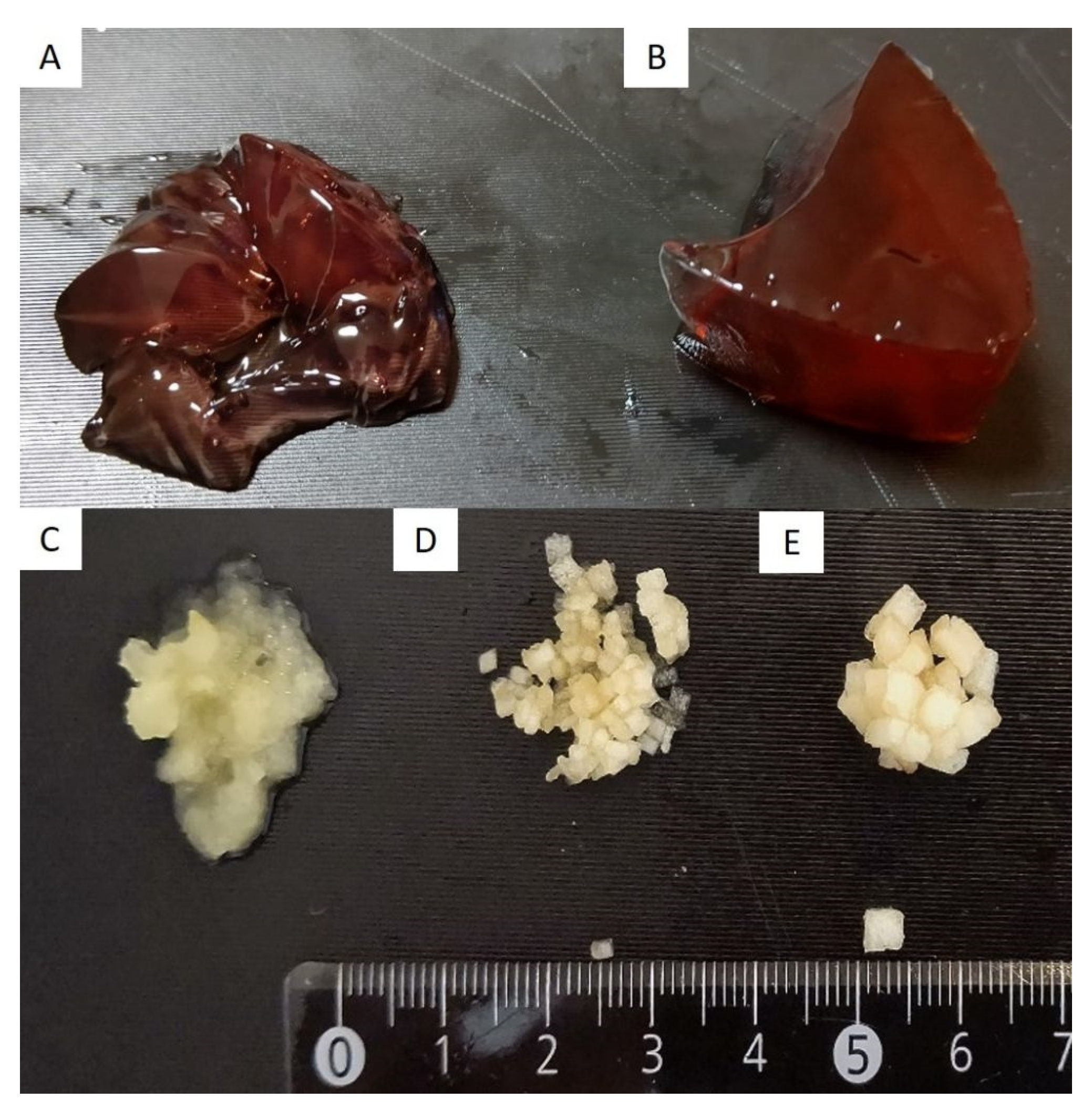
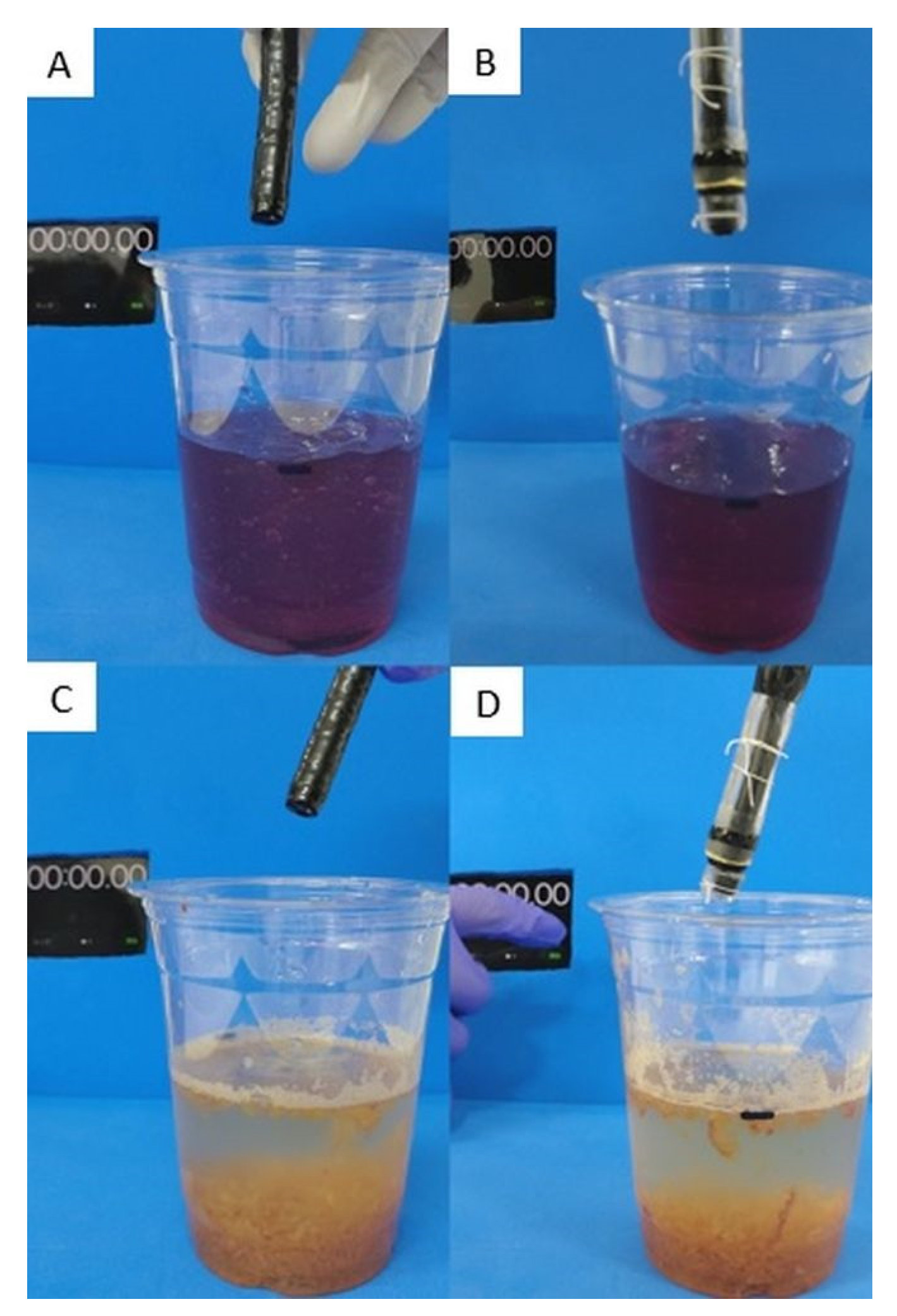
2.3. Ex Vivo Study: Comparison of Suction Ability between a Standard Endoscope and Our Hand-Made Device
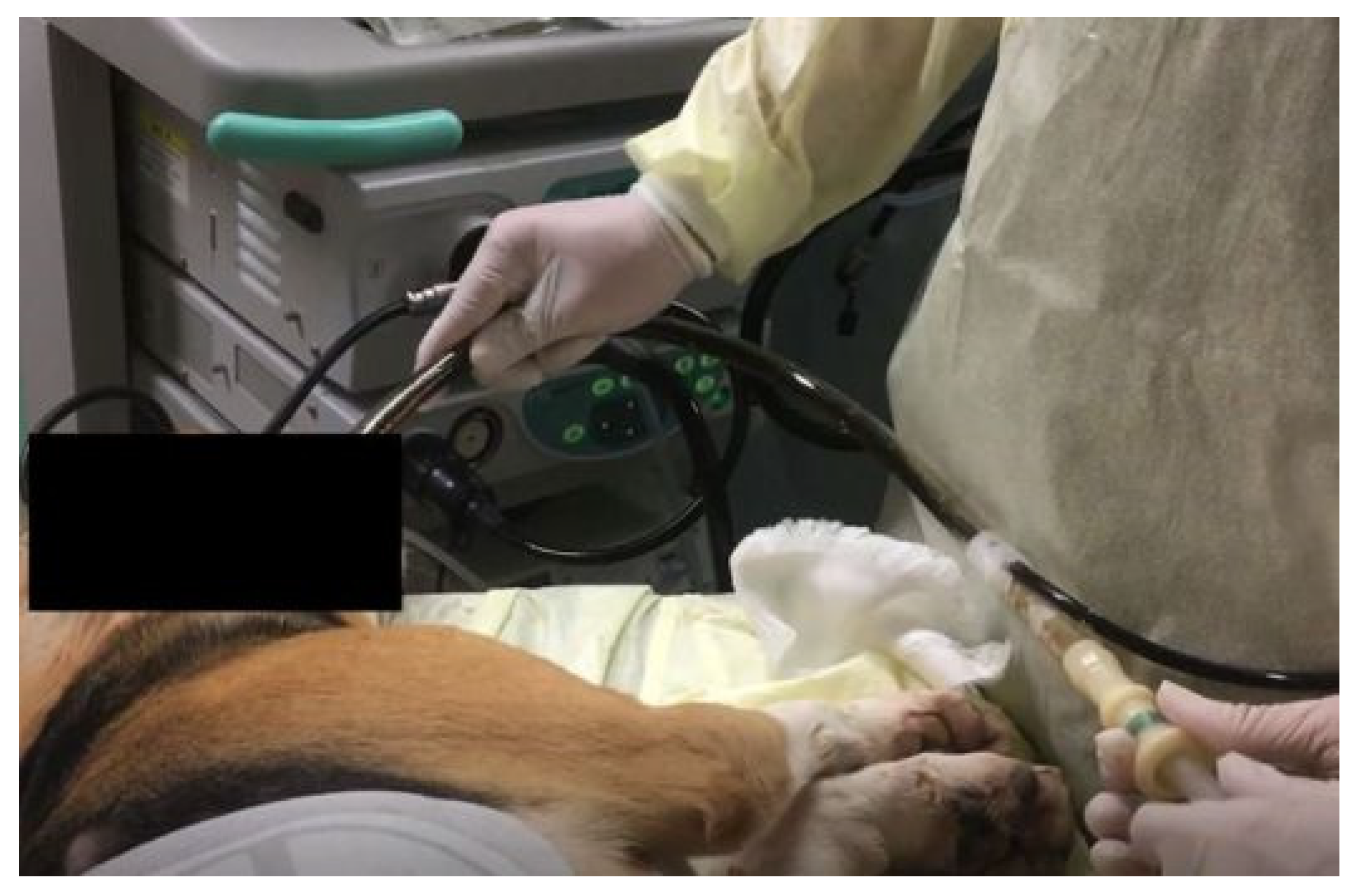
2.4. In Vivo Animal Study
- Step 1: The manufactured overtube was inserted into the stomach under the guidance of an ultrathin endoscope;
- Step 2: After the visualization of the simulated GI residue under ultrathin endoscopy, the biopsy forceps were inserted via the forceps channel of the endoscope (Figure 5). The biopsy forceps were pressed on the superficial mucosa to prevent suctioning the mucosa;
- Step 3: The GI residue was suctioned under 40 kPa negative pressure while the targeted residue was visualized using the ultrathin endoscope (Figure 6);
- Step 4: An appropriate distance between the tube and superficial mucosa was maintained using the biopsy forceps (as described in Step 2), leading to continuous and effective suction (Figure 7);
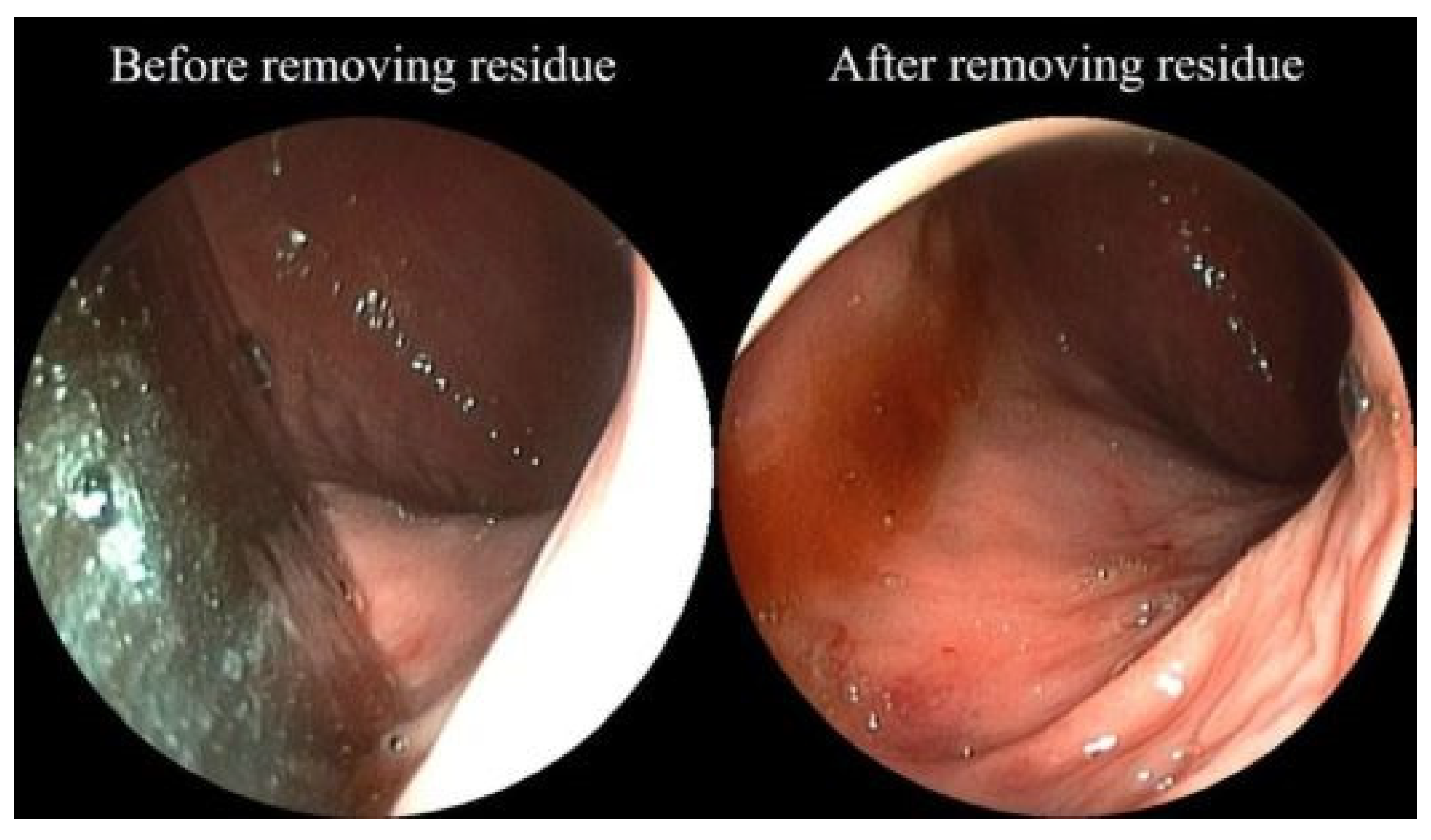
- Step 5: Successful suction was completed when the mucosal membrane hidden by the GI residue appeared on the greater curvature side (Figure 8).
2.5. Outcome Measures in the Ex Vivo Study
2.6. Outcome Measures in the In Vivo Animal Study
2.7. Statistical Analyses
3. Results
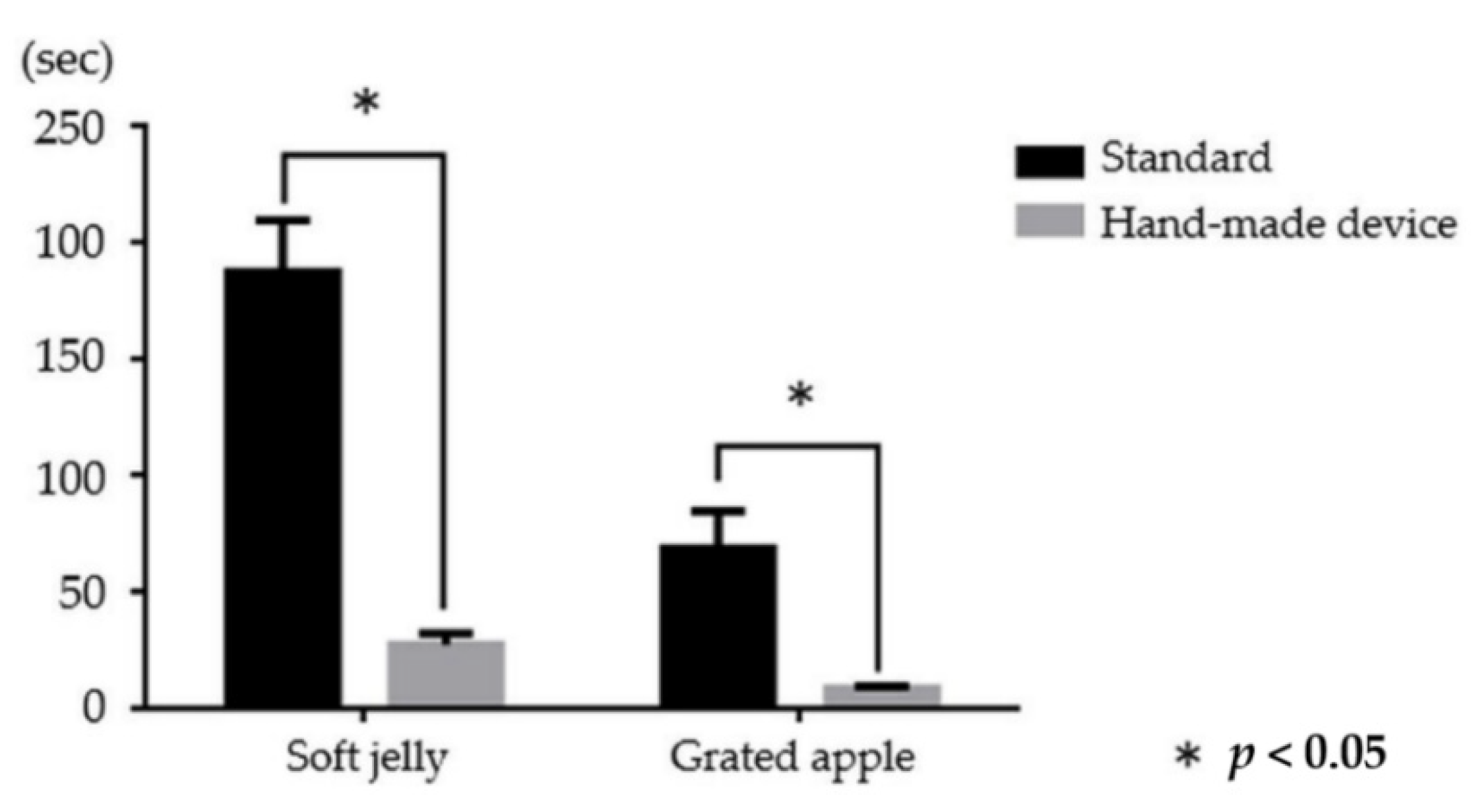
3.1. Results of the Ex Vivo Study
3.2. Results in Experimental Animal Study
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cooper, G.S.; Kou, T.D.; Wong, R.C. Use and Impact of Early Endoscopy in Elderly Patients with Peptic Ulcer Hemorrhage: A Population-Based Analysis. Gastrointest. Endosc. 2009, 70, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Coleski, R.; Baker, J.R.; Hasler, W.L. Endoscopic Gastric Food Retention in Relation to Scintigraphic Gastric Emptying Delays and Clinical Factors. Dig. Dis. Sci. 2016, 61, 2593–2601. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Adachi, W.; Koide, N.; Yazawa, I. Food Residue at Endoscopy in Patients Who Have Previously Undergone Distal Gastrectomy: Risk Factors and Patient Preparation. Endoscopy 2003, 35, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Kubosawa, Y.; Mori, H.; Kinoshita, S.; Nakazato, Y.; Fujimoto, A.; Kikuchi, M.; Nishizawa, T.; Suzuki, M.; Suzuki, H. Changes of Gastric Ulcer Bleeding in the Metropolitan Area of Japan. World, J. Gastroenterol. 2019, 25, 6342–6353. [Google Scholar] [CrossRef] [PubMed]
- Kozuka, K.; Kobara, H.; Nishiyama, N.; Chiyo, T.; Kobayashi, N.; Yachida, T.; Masaki, T. Novel Method Using Small-Caliber Endoscope and Balloon Overtube for Removing Gastrointestinal Residue. Endoscopy 2021, 53, E130–E131. [Google Scholar] [CrossRef] [PubMed]
- Japanese Ministry of Health, Labour and Welfare. The NDB Open Data in 2017. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/kanja/10syoubyo/dl/h29syobyo.pdf (accessed on 21 April 2021).
- Toka, B.; Eminler, A.T.; Karacaer, C.; Uslan, M.I.; Koksal, A.S.; Parlak, E. Comparison of Monopolar Hemostatic Forceps with Soft Coagulation Versus Hemoclip for Peptic Ulcer Bleeding: A Randomized Trial (with Video). Gastrointest. Endosc. 2019, 89, 792–802. [Google Scholar] [CrossRef]
- Panés, J.; Viver, J.; Forné, M.; Garcia-Olivares, E.; Marco, C.; Garau, J. Controlled Trial of Endoscopic Sclerosis in Bleeding Peptic Ulcers. Lancet 1987, 2, 1292–1294. [Google Scholar] [CrossRef]
- Raju, G.S.; Gajula, L. Endoclips for GI Endoscopy. Gastrointest. Endosc. 2004, 59, 267–279. [Google Scholar] [CrossRef]
- Ito, M.; Takata, S.; Tatsugami, M.; Wada, Y.; Imagawa, S.; Matsumoto, Y.; Takamura, A.; Kitamura, S.; Matsuo, T.; Tanaka, S.; et al. Clinical Prevention of Gastric Cancer by Helicobacter pylori Eradication Therapy: A Systematic Review. J. Gastroenterol. 2009, 44, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, D.; Iizuka, T.; Nomura, K.; Kuribayashi, Y.; Tanaka, M.; Yamashita, S.; Furuhata, T.; Matsui, A.; Mitani, T.; Makino, S.; et al. Feasibility of Autologous Fibrin Glue and Polyglycolic Acid Sheets to Prevent Delayed Bleeding After Endoscopic Submucosal Dissection of Gastric Neoplasms in Patients Receiving Antithrombotic Therapy. Gastroenterol. Res. Pract. 2018, 2174957. [Google Scholar] [CrossRef] [PubMed]
- Kobara, H.; Mori, H.; Nishiyama, N.; Fujihara, S.; Okano, K.; Suzuki, Y.; Masaki, T. Over-the-Scope Clip System: A Review of 1517 Cases over 9 Years. J. Gastroenterol. Hepatol. 2019, 34, 22–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saetta, J.P.; Quinton, D.N. Residual Gastric Content after Gastric Lavage and Ipecacuanha-Induced Emesis in Self-poisoned Patients: An Endoscopic Study. J. R. Soc. Med. 1991, 84, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.B.; Yoon, K.W.; Park, S.Y.; Lee, W.S.; Park, C.H.; Joo, Y.E.; Kim, H.S.; Choi, S.K.; Rew, J.S. Risk Factors for Food Residue after Distal Gastrectomy and a New Effective Preparation for Endoscopy: The Water-Intake Method. Gut Liver 2009, 3, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Avgerinos, A.; Vlachogiannakos, J.; Viazis, N.; Raptis, S.A. Clearing the Stomach before Emergency Endoscopy in Cirrhotics with Acute Upper Gastrointestinal Bleeding. A Gastrokinetic or a Vasoactive Drug? J. Hepatol. 2003, 39, 130–131. [Google Scholar] [CrossRef]
- Coffin, B.; Pocard, M.; Panis, Y.; Riche, F.; Lainé, M.J.; Bitoun, A.; Lémann, M.; Bouhnik, Y.; Valleur, P.; Groupe des endoscopistes de garde á l’AP-HP. Erythromycin Improves the Quality of EGD in Patients with Acute Upper GI Bleeding: A Randomized Controlled Study. Gastrointest. Endosc. 2002, 56, 174–179. [Google Scholar] [CrossRef]
- Zeng, X.; Yan, P.; Ye, L.; Guo, L.; Wu, N.; Hu, B. Tube-Assisted Suction: A Novel Technique for Removing Massive Food Residue During Gastroscopy. Endoscopy 2019, 51, E73–E74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishiyama, N.; Kobara, H.; Yachida, T.; Mori, H.; Shi, T.; Okano, K.; Masaki, T. Strategy of small-caliber endoscopic submucosal dissection for esophageal neoplasia distal to severe stricture. Endoscopy 2020, 52, E94–E95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikuchi, D.; Tanaka, M.; Nakamura, S.; Nomura, K.; Hayasaka, J.; Ochiai, Y.; Odagiri, H.; Yamashita, S.; Matsui, A.; Hoteya, S. Feasibility of ultrathin endoscope for esophageal endoscopic submucosal dissection. Endosc. Int. Open 2021, 9, E606–E609. [Google Scholar] [CrossRef] [PubMed]


| Endoscope | Soft Jelly | Hard Jelly | Grated Apple | 1 mm2 Apple Pieces | 3 mm2 Apple Pieces |
|---|---|---|---|---|---|
| Standard | 100 | 0 | 100 | 0 | 0 |
| Hand-made device | 100 | 100 | 100 | 100 | 0 |
| Endoscope | Soft Jelly | Hard Jelly | Grated Apple | 1 mm2 Apple Sections | 3 mm2 Apple Sections |
|---|---|---|---|---|---|
| Standard | 188 ± 22 | - | 69 ± 16 | - | - |
| Hand-made device | 28 ± 5 | 377 ± 34 | 9 ± 1 | 8 ± 2 | - |
| Case | Attempt | Residue Volume (mL) | Suction Pressure (kPa) | Procedure Time (sec) | Successful Residue Removal | Complications |
|---|---|---|---|---|---|---|
| 1 | 1 | 150 | 40 | 235 | Yes | None |
| 2 | 150 | 40 | 265 | Yes | None | |
| 2 | 3 | 150 | 40 | 540 | Yes | None |
| 4 | 150 | 40 | 200 | Yes | None | |
| 3 | 5 | 150 | 40 | 390 | Yes | None |
| 6 | 150 | 40 | 130 | Yes | None | |
| 4 | 7 | 150 | 40 | 210 | Yes | None |
| 8 | 150 | 40 | 352 | Yes | None | |
| 5 | 9 | 150 | 40 | 530 | Yes | None |
| 10 | 150 | 40 | 180 | Yes | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kozuka, K.; Kobara, H.; Nishiyama, N.; Fujihara, S.; Tada, N.; Matsui, T.; Takata, T.; Chiyo, T.; Kobayashi, N.; Shi, T.; et al. Gastrointestinal Residue Removal Using a Balloon Overtube under Ultrathin Endoscopic Navigation: Ex Vivo and In Vivo Experimental Studies. J. Clin. Med. 2021, 10, 3796. https://doi.org/10.3390/jcm10173796
Kozuka K, Kobara H, Nishiyama N, Fujihara S, Tada N, Matsui T, Takata T, Chiyo T, Kobayashi N, Shi T, et al. Gastrointestinal Residue Removal Using a Balloon Overtube under Ultrathin Endoscopic Navigation: Ex Vivo and In Vivo Experimental Studies. Journal of Clinical Medicine. 2021; 10(17):3796. https://doi.org/10.3390/jcm10173796
Chicago/Turabian StyleKozuka, Kazuhiro, Hideki Kobara, Noriko Nishiyama, Shintaro Fujihara, Naoya Tada, Takanori Matsui, Tadayuki Takata, Taiga Chiyo, Nobuya Kobayashi, Tingting Shi, and et al. 2021. "Gastrointestinal Residue Removal Using a Balloon Overtube under Ultrathin Endoscopic Navigation: Ex Vivo and In Vivo Experimental Studies" Journal of Clinical Medicine 10, no. 17: 3796. https://doi.org/10.3390/jcm10173796
APA StyleKozuka, K., Kobara, H., Nishiyama, N., Fujihara, S., Tada, N., Matsui, T., Takata, T., Chiyo, T., Kobayashi, N., Shi, T., Fujita, K., Tani, J., Yachida, T., Kondo, A., Kumamoto, K., Okano, K., Nishiyama, A., Deguchi, K., & Masaki, T. (2021). Gastrointestinal Residue Removal Using a Balloon Overtube under Ultrathin Endoscopic Navigation: Ex Vivo and In Vivo Experimental Studies. Journal of Clinical Medicine, 10(17), 3796. https://doi.org/10.3390/jcm10173796









