Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Measurements
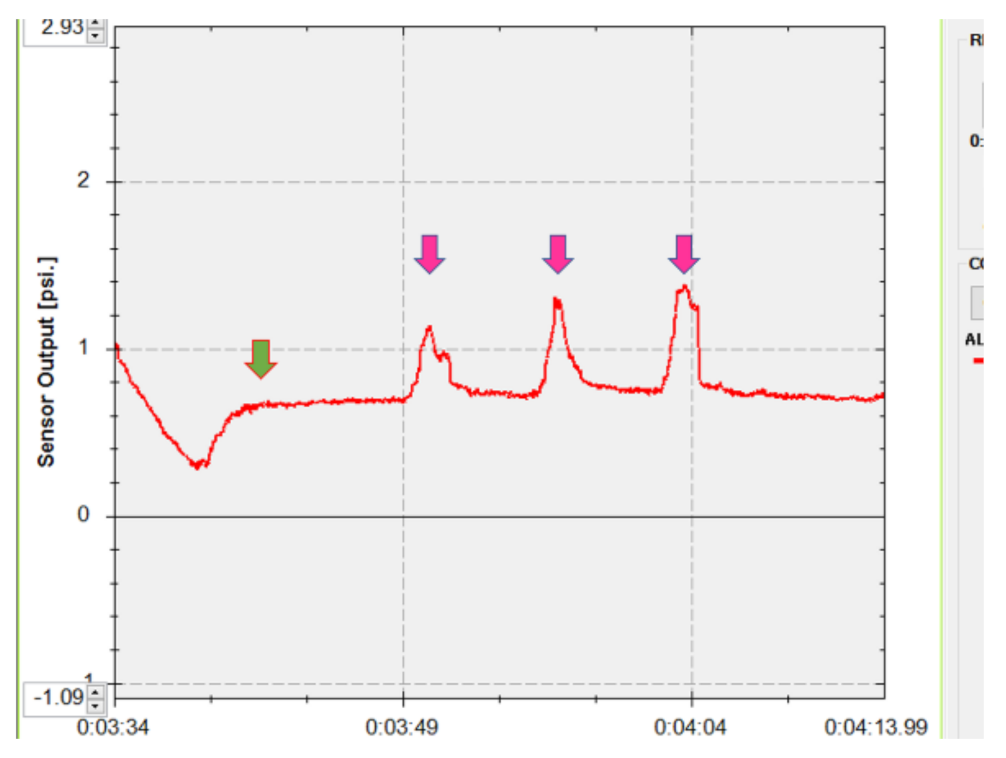
2.2.1. Eyelid Pressure
2.2.2. TED Condition
2.2.3. General Assessment of Dry Eye
2.2.4. TMH
2.2.5. MGD
2.2.6. SLK
2.3. Surgical Procedures
2.3.1. Deep Lateral Orbital Wall Decompression
2.3.2. Medial Orbital Wall Decompression
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Sakai, E.; Shiraishi, A.; Yamaguchi, M.; Ohta, K.; Ohashi, Y. Blepharo-tensiometer: New eyelid pressure measurement system using tactile pressure sensor. Eye Contact Lens 2012, 38, 326–330. [Google Scholar] [CrossRef]
- Takahashi, Y.; Ichinose, A.; Kakizaki, H. Topical rebamipide treatment for superior limbic keratoconjunctivitis in patients with thyroid eye disease. Am. J. Ophthalmol. 2014, 157, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, N.; Maeda, T.; Inoue, T.; Inoue, Y. Clinical study of superior limbic keratoconjunctivitis associated with dysthyroid ophthalmopathy. Folia Ophthalmol. Jpn. 2003, 54, 965–968. (In Japanese) [Google Scholar]
- Park, H.H.; Chun, Y.S.; Moon, N.J.; Kim, J.T.; Park, S.J.; Lee, J.K. Change in eyelid parameters after orbital decompression in thyroid-associated orbitopathy. Eye 2018, 32, 1036–1041. [Google Scholar] [CrossRef]
- Ehrmann, K.; Francis, I.; Stapleton, F. A novel instrument to quantify the tension of upper and lower eyelids. Cont. Lens Anterior Eye 2001, 24, 65–72. [Google Scholar] [CrossRef]
- Francis, I.C.; Stapleton, F.; Ehrmann, K.; Coroneo, M.T. Lower eyelid tensometry in younger and older normal subjects. Eye 2006, 20, 166–172. [Google Scholar] [CrossRef] [Green Version]
- Gürdal, C.; Genç, İ.; Saraç, Ö.; Gönül, İ.; Takmaz, T.; Can, İ. Topical cyclosporine in thyroid orbitopathy-related dry eye: Clinical findings, conjunctival epithelial apotosis, and MMP-9 expression. Curr. Eye Res. 2010, 35, 771–777. [Google Scholar] [CrossRef]
- Kim, H.H.; De Paiva, C.S.; Yen, M.T. Effects of upper eyelid blepharoplasty on ocular surface sensation and tear production. Can. J. Ophthalmol. 2007, 42, 739–742. [Google Scholar] [CrossRef] [PubMed]
- Thorne, A.W.; Rootman, D.B. Influence of surgical approach for decompression on lower eyelid position in thyroid eye disease. Orbit 2020, 39, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Kadrmas, E.F.; Bartley, G.B. Superior limbic keratoconjunctivitis: A prognostic sign for severe Graves ophthalmopathy. Ophthalmology 1995, 102, 1472–1475. [Google Scholar] [CrossRef]
- Perros, P.; Žarković, M.P.; Panagiotou, G.C.; Azzolini, C.; Ayvaz, G.; Baldeschi, L.; Bartalena, L.; Boschi, A.M.; Nardi, M.; Brix, T.H.; et al. The European Group on Graves’ Orbitopathy. Asymmetry indicates more severe and active disease in Graves’ orbitopathy: Results from a prospective cross-sectional multicentre study. J. Endocrinol. Investig. 2020, 43, 1717–1722. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Lee, P.A.L.; Vaidya, A.; Kono, S.; Kakizaki, H. Tear film break-up patterns in thyroid eye disease. Sci. Rep. 2021, 11, 5288. [Google Scholar] [CrossRef] [PubMed]
- Mourits, M.P.; Koornneef, L.; Wiersinga, W.M.; Prummel, M.F.; Berghout, A.; van der Gaag, R. Clinical criteria for the assessment of disease activity in Graves’ ophthalmopathy: A novel approach. Br. J. Ophthalmol. 1989, 73, 639–644. [Google Scholar] [CrossRef] [Green Version]
- Lee, P.A.L.; Vaidya, A.; Kono, S.; Kakizaki, H.; Takahashi, Y. Relationship between eyelid pressure and lacrimal status in mild facial nerve palsy. Cureus 2021, 13, e12830. [Google Scholar]
- Miyata, K.; Amano, S.; Sawa, M.; Nishida, T. A novel grading method for superficial punctate keratopathy magnitude and its correlation with corneal epithelial permeability. Arch. Ophthalmol. 2003, 121, 1537–1539. [Google Scholar] [CrossRef]
- Kakutani, S.; Lee, P.A.L.; Kakizaki, H.; Takahashi, Y. Patency of the lacrimal drainage system in patients with a peripunctaltumour. Orbit 2020, 39, 394. [Google Scholar] [CrossRef]
- Ishikawa, E.; Sabundayo, M.S.; Kono, S.; Kakizaki, H.; Takahashi, Y. Patency of the lacrimal drainage system in patients with a peripunctaltumour. Orbit 2020, 39, 102–106. [Google Scholar] [CrossRef]
- Vaidya, A.; Kakizaki, H.; Takahashi, Y. Postoperative changes in status of meibomian gland dysfunction in patients with involutional entropion. Int. Ophthalmol. 2020, 40, 1397–1402. [Google Scholar] [CrossRef]
- Takahashi, Y.; Kakizaki, H. Meibomian gland dysfunction in cranial nerve VII palsy. Ophthalmic Plast. Reconstr. Surg. 2015, 31, 179–181. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Kutsuna, M.; Uno, T.; Zheng, X.; Kodama, T.; Ohashi, Y. Marx line: Fluorescein staining line on the inner lid as indicator of meibomian gland function. Am. J. Ophthalmol. 2006, 141, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Arita, R.; Itoh, K.; Inoue, K.; Amano, S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 2008, 115, 911–915. [Google Scholar] [CrossRef]
- Vaidya, A.; Kakizaki, H.; Takahashi, Y. Influential factors for changes in binocular single vision field and ocular deviation angle after balanced orbital decompression. Ophthalmic Plast. Reconstr. Surg. 2021, 37, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.A.L.; Vaidya, A.; Kono, S.; Kakizaki, H.; Takahashi, Y. Extraocular muscle expansion after deep lateral orbital wall decompression: Influence on proptosis reduction and its predictive factors. Graefes Arch. Clin. Exp. Ophthalmol. 2021. (Online ahead of print). [Google Scholar] [CrossRef]
- Inoue, S.; Kawashima, M.; Arita, R.; Kozaki, A.; Tsubota, K. Investigation of meibomian gland function and dry eye disease in patients with Graves’ ophthalmopathy. J. Clin. Med. 2020, 9, 2814. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Baek, S. Dry eye syndrome in thyroid eye disease patients: The role of increased incomplete blinking and meibomian gland loss. Acta Ophthalmol. 2019, 97, e800–e806. [Google Scholar] [CrossRef]
- Fionda, B.; Lancellotta, V.; Casà, C.; Boldrini, L.; Marazzi, F.; Cellini, F.; Kovács, G.; Gambacorta, M.A.; Tagliaferri, L. Radiotherapy for benign disorders: Current use in clinical practice. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 3440–3443. [Google Scholar]
- Ito, M.; Takahashi, Y.; Katsuda, E.; Oshima, Y.; Takeuchi, A.; Mori, T.; Abe, S.; Mori, Y.; Kakizaki, H.; Suzuki, K. Predictive factors of prognosis after radiation and steroid pulse therapy in thyroid eye disease. Sci. Rep. 2019, 9, 2027. [Google Scholar] [CrossRef] [Green Version]
- Prabhu, R.S.; Leibman, L.; Wojno, T.; Hayek, B.; Hall, W.A.; Crocker, I. Clinical outcomes of radiotherapy as initial local therapy for Graves’ ophthalmopathy and predictors of the need for post-radiotherapy decompressive surgery. Radiot. Oncol. 2021, 7, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Napoli, P.E.; Coronella, F.; Satta, G.M.; Galantuomo, M.S.; Fossarello, M. Evaluation of the adhesive properties of the cornea by means of optical coherence tomography in patients with meibomian gland dysfunction and lacrimal tear deficiency. PLoS ONE 2014, 9, e115762. [Google Scholar] [CrossRef] [Green Version]
- Nioi, M.; Napoli, P.E.; Mayerson, S.M.; Fossarello, M.; d’Aloja, E. Optical coherence tomography in forensic sciences: A review of the literature. Forensic. Sci. Med. Pathol. 2019, 15, 445–452. [Google Scholar] [CrossRef]
- Ana-Magadia, M.G.; Valencia, M.R.P.; Naito, M.; Nakano, T.; Miyazaki, H.; Kakizaki, H.; Takahashi, Y. Location of the myoneural junction of the inferior oblique muscle: An anatomic study. Ann. Anat 2020, 227, 151429. [Google Scholar] [CrossRef]
| Measurement Parameters | Grading | Findings |
|---|---|---|
| A | 0 | No punctate staining |
| 1 | The staining involving less than one-third of the cornea | |
| 2 | The staining involving one-third to two-thirds of the cornea | |
| 3 | The staining involving more than two-thirds of the cornea | |
| D | 0 | No punctate staining |
| 1 | Sparse density | |
| 2 | Moderate density | |
| 3 | High density and overlapped lesions | |
| Marx line | 0 | The line runs entirely along the conjunctival side of the meibomian gland orifices |
| 1 | Parts of the line touch the meibomian orifices | |
| 2 | The line runs through the meibomian orifices | |
| 3 | The line runs along the eyelid margin side of the meibomian orifices | |
| Meibum expression | 0 | Easy expression of clear meibum with mild eyelid compression |
| 1 | Cloudy meibum expression with mild compression | |
| 2 | Cloudy meibum expression with moderate compression | |
| 3 | Toothpaste-like meibum expression with more than moderate compression | |
| 4 | No expression even with hard compression | |
| Meibography score | 0 | No loss of meibomian glands |
| 1 | Area loss less than one-third of the total meibomian gland area | |
| 2 | Area loss between one-third and two-thirds of total meibomian gland area | |
| 3 | Area loss more than two-thirds of total meibomian gland area |
| Preoperative | Postoperative | p Value | |
|---|---|---|---|
| Maximum upper eyelid pressure (psi) | 1.26 ± 0.37 | 1.26 ± 0.31 | 0.937 |
| Upper eyelid pressure at plateau phase (psi) | 0.94 ± 0.17 | 0.97 ± 0.16 | 0.405 |
| TED condition | |||
| Hertel exophthalmometric value (mm) | 22.0 ± 2.4 | 17.3 ± 2.6 | <0.001 |
| MRD-1 (mm) | 4.6 ± 1.8 | 4.6 ± 1.5 | 0.832 |
| MRD-2 (mm) | 6.6 ± 1.4 | 5.9 ± 1.0 | 0.001 |
| AD score | |||
| A | 1.0 ± 1.0 | 1.0 ± 0.8 | 0.932 |
| D | 1.2 ± 1.2 | 1.8 ± 1.4 | 0.026 |
| TBUT (s) | 1.6 ± 1.2 | 0.9 ± 1.3 | 0.068 |
| Schirmer test (mm) | 20.1 ± 10.7 | 9.2 ± 5.6 | <0.001 |
| Marx line | |||
| Upper eyelid | 4.6 ± 1.9 | 4.3 ± 2.5 | 0.080 |
| Lower eyelid | 4.8 ± 2.0 | 5.4 ± 1.8 | 0.078 |
| MGD score | 1.6 ± 1.3 | 1.2 ± 1.2 | 0.008 |
| Meibum expression | |||
| Upper eyelid | 1.3 ± 1.3 | 1.2 ± 1.4 | 0.638 |
| Lower eyelid | 1.2 ± 1.2 | 1.0 ± 1.0 | 0.276 |
| Meibography | |||
| Upper eyelid | 1.1 ± 0.8 | 0.9 ± 0.7 | 0.008 |
| Lower eyelid | 0.5 ± 0.5 | 0.4 ± 0.6 | 0.157 |
| TMH (μm) | |||
| Upper eyelid | 278.5 ± 77.7 | 274.5 ± 70.5 | 0.843 |
| Lower eyelid | 356.9 ± 106.5 | 361.4 ± 273.3 | 0.931 |
| SLK (presence/absence) | 11/18 | 10/19 | 1.000 |
| Group 1: Decreased Pressure (n = 13) | Group 2: Elevated Pressure (n = 16) | p Value: Postoperative Changes, Group 1 vs. 2 | |||
|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||
| Maximum upper eyelid pressure (psi) | 1.43 ± 0.44 | 1.25 ± 0.42 | 1.12 ± 0.24 | 1.27 ± 0.20 | <0.001 |
| Upper eyelid pressure at plateau phase (psi) | 1.04 ± 0.15 | 0.93 ± 0.20 | 0.86 ± 0.15 | 1.00 ± 0.12 | <0.001 |
| TED condition | |||||
| Hertel exophthalmometric value (mm) | 20.7 ± 1.1 | 17.0 ± 2.1 | 23.0 ± 2.7 | 17.6 ± 3.0 | 0.068 |
| MRD-1 (mm) | 5.0 ± 1.8 | 4.6 ± 1.5 | 4.2 ± 1.7 | 4.5 ± 1.5 | 0.028 |
| MRD-2 (mm) | 6.0 ± 0.8 | 5.3 ± 0.3 | 7.2 ± 1.6 | 6.3 ± 1.2 | 0.714 |
| AD score | |||||
| A | 1.2 ± 0.8 | 0.9 ± 0.9 | 0.8 ± 1.0 | 1.1 ± 0.9 | 0.232 |
| D | 1.8 ± 1.2 | 1.9 ± 1.4 | 0.8 ± 1.0 | 1.8 ± 1.3 | 0.132 |
| TBUT (s) | 1.4 ± 1.4 | 1.0 ± 1.2 | 1.7 ± 1.1 | 0.9 ± 1.5 | 0.288 |
| Schirmer test (mm) | 19.6 ± 9.5 | 9.5 ± 5.7 | 20.4 ± 11.8 | 8.9 ± 5.7 | 0.746 |
| Marx line | |||||
| Upper eyelid | 5.3 ± 1.3 | 4.8 ± 2.2 | 4.0 ± 2.2 | 3.9 ± 2.8 | 0.983 |
| Lower eyelid | 5.4 ± 1.5 | 5.5 ± 1.8 | 4.4 ± 2.2 | 5.3 ± 1.9 | 0.398 |
| MGD score | 1.8 ± 1.2 | 1.5 ± 1.3 | 1.4 ± 1.4 | 1.0 ± 1.2 | 0.846 |
| Meibum expression | |||||
| Upper eyelid | 1.8 ± 1.6 | 1.2 ± 1.3 | 0.9 ± 1.0 | 1.3 ± 1.4 | 0.249 |
| Lower eyelid | 1.8 ± 1.5 | 1.1 ± 1.0 | 0.8 ± 0.7 | 0.9 ± 1.0 | 0.121 |
| Meibography | |||||
| Upper eyelid | 1.2 ± 0.8 | 0.8 ± 0.6 | 1.0 ± 0.8 | 0.6 ± 0.5 | 0.249 |
| Lower eyelid | 0.5 ± 0.5 | 0.5 ± 0.7 | 0.9 ± 0.8 | 0.3 ± 0.4 | 0.121 |
| TMH (μm) | |||||
| Upper eyelid | 280.5 ± 94.9 | 246.6 ± 41.1 | 276.9 ± 63.8 | 346.3 ± 127.7 | 0.423 |
| Lower eyelid | 370.0 ± 75.8 | 292.2 ± 83.9 | 297.2 ± 81.9 | 417.8 ± 355.3 | 0.215 |
| SLK (improvement/absence-absence/deterioration or no improvement) | 4/4/5 | 0/11/5 | 0.030 | ||
| Dependent Variable: Maximum Eyelid Pressure | Univariate | Multivariate Stepwise | ||
|---|---|---|---|---|
| Crude Coefficient (95% CI) | p Value | Crude Coefficient (95% CI) | p Value | |
| Age | 0.005 (−0.006 to 0.015) | 0.364 | ||
| Sex | 0.142 (−0.113 to 0.397) | 0.262 | ||
| Preoperative MRD-1 | 0.063 (0.013 to 0.114) | 0.016 | - | - |
| Changes in MRD-1 | 0.172 (0.078 to 0.266) | 0.001 | 0.172 (0.078 to 0.266) | 0.001 |
| Preoperative MRD-2 | −0.024 (−0.094 to 0.045) | 0.476 | ||
| Changes in MRD-2 | 0.019 (0.077 to 0.115) | 0.691 | ||
| Preoperative Hertel exophthalmometric value | −0.011 (−0.052 to 0.030) | 0.573 | ||
| Changes in Hertel exophthalmometric value | −0.029 (−0.077 to 0.020) | 0.238 | ||
| Dependent Variable: Eyelid Pressure at Plateau Phase | Univariate | Multivariate Stepwise | ||
| Crude Coefficient (95% CI) | p Value | Crude Coefficient (95% CI) | p Value | |
| Age | 0.003 (−0.005 to 0.012) | 0.448 | ||
| Sex | 0.024 (−0.196 to 0.245) | 0.227 | ||
| Preoperative MRD-1 | 0.026 (−0.020 to 0.073) | 0.254 | ||
| Changes in MRD-1 | 0.134 (0.052 to 0.217) | 0.003 | ||
| Preoperative MRD-2 | −0.045 (−0.101 to 0.012) | 0.118 | ||
| Changes in MRD-2 | −0.027 (−0.108 to 0.054) | 0.568 | ||
| Preoperative Hertel exophthalmometric value | −0.020 (−0.054 to 0.013) | 0.226 | ||
| Changes in Hertel exophthalmometric value | −0.035 (−0.075 to 0.005) | 0.080 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, Y.; Vaidya, A.; Kakizaki, H. Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease. J. Clin. Med. 2021, 10, 3687. https://doi.org/10.3390/jcm10163687
Takahashi Y, Vaidya A, Kakizaki H. Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease. Journal of Clinical Medicine. 2021; 10(16):3687. https://doi.org/10.3390/jcm10163687
Chicago/Turabian StyleTakahashi, Yasuhiro, Aric Vaidya, and Hirohiko Kakizaki. 2021. "Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease" Journal of Clinical Medicine 10, no. 16: 3687. https://doi.org/10.3390/jcm10163687
APA StyleTakahashi, Y., Vaidya, A., & Kakizaki, H. (2021). Changes in Eyelid Pressure and Dry Eye Status after Orbital Decompression in Thyroid Eye Disease. Journal of Clinical Medicine, 10(16), 3687. https://doi.org/10.3390/jcm10163687






