Survival of Peritoneal Membrane Function on Biocompatible Dialysis Solutions in a Peritoneal Dialysis Cohort Assessed by a Novel Test
Abstract
:1. Introduction
2. Materials and Methods
2.1. Calculations
- 1
- We estimated classic peritoneal transport parameters such as D/P creatinine, D/P urea,
- 2
- We calculated dipping of sodium expressed as
- 3
- Free water transport (FWT) was calculated as follows:
- 4
- Sodium removal = [Dialysate V in 1 h (L) × Dialysate sodium at 1 h (mmol/L)] − [Dialysate V instilled (L) × Dialysate sodium at 0 min (mmol/L)]
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jager, K.J.; Merkus, M.P.; Dekker, F.W.; Boeschoten, E.W.; Tijssen, J.G.; Stevens, P.; Bos, W.J.; Krediet, R.T.; NECOSAD Study Group. Mortality and technique failure in patients starting chronic peritoneal dialysis: Results of The Netherlands Cooperative Study on the Adequacy of Dialysis. NECOSAD Study Group. Kidney Int. 1999, 55, 1476–1485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krediet, R.T.; Balafa, O. Cardiovascular risk in the peritoneal dialysis patient. Nat. Rev. Nephrol. 2010, 6, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Mujais, S.; Nolph, K.; Gokal, R.; Blake, P.; Burkart, J.; Coles, G.; Kawaguchi, Y.; Kawanishi, H.; Korbet, S.; Krediet, R.; et al. Evaluation and management of ultrafiltration problems in peritoneal dialysis. International Society for Peritoneal Dialysis Ad Hoc Committee on Ultrafiltration Management in Peritoneal Dialysis. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2000, 20 (Suppl. 4), S5–S21. [Google Scholar] [CrossRef]
- Krediet, R.T. Ultrafiltration Failure Is a Reflection of Peritoneal Alterations in Patients Treated With Peritoneal Dialysis. Front. Physiol. 2018, 9, 1815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morelle, J.; Sow, A.; Hautem, N.; Bouzin, C.; Crott, R.; Devuyst, O.; Goffin, E. Interstitial Fibrosis Restricts Osmotic Water Transport in Encapsulating Peritoneal Sclerosis. J. Am. Soc. Nephrol. JASN 2015, 26, 2521–2533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nolph, K.D.; Twardowski, Z.J.; Popovich, R.P.; Rubin, J. Equilibration of peritoneal dialysis solutions during long-dwell exchanges. J. Lab. Clin. Med. 1979, 93, 246–256. [Google Scholar] [PubMed]
- Van Biesen, W.; Heimburger, O.; Krediet, R.; Rippe, B.; La Milia, V.; Covic, A.; Vanholder, R. Evaluation of peritoneal membrane characteristics: Clinical advice for prescription management by the ERBP working group. Nephrol. Dial. Transpl. 2010, 25, 2052–2062. [Google Scholar] [CrossRef] [Green Version]
- Morelle, J.; Stachowska-Pietka, J.; Öberg, C.; Gadola, L.; La Milia, V.; Yu, Z.; Lambie, M.; Mehrotra, R.; de Arteaga, J.; Davies, S. ISPD recommendations for the evaluation of peritoneal membrane dysfunction in adults: Classification, measurement, interpretation and rationale for intervention. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2021, 41, 352–372. [Google Scholar] [CrossRef]
- La Milia, V.; Di Filippo, S.; Crepaldi, M.; Del Vecchio, L.; Dell’Oro, C.; Andrulli, S.; Locatelli, F. Mini-peritoneal equilibration test: A simple and fast method to assess free water and small solute transport across the peritoneal membrane. Kidney Int. 2005, 68, 840–846. [Google Scholar] [CrossRef] [Green Version]
- Cnossen, T.T.; Smit, W.; Konings, C.J.; Kooman, J.P.; Leunissen, K.M.; Krediet, R.T. Quantification of free water transport during the peritoneal equilibration test. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2009, 29, 523–527. [Google Scholar] [CrossRef]
- La Milia, V.; Pozzoni, P.; Virga, G.; Crepaldi, M.; Del Vecchio, L.; Andrulli, S.; Locatelli, F. Peritoneal transport assessment by peritoneal equilibration test with 3.86% glucose: A long-term prospective evaluation. Kidney Int. 2006, 69, 927–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernardo, A.P.; Bajo, M.A.; Santos, O.; Del Peso, G.; Carvalho, M.J.; Cabrita, A.; Selgas, R.; Rodrigues, A. Two-in-one protocol: Simultaneous small-pore and ultrasmall-pore peritoneal transport quantification. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2012, 32, 537–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venturoli, D.; Rippe, B. Validation by computer simulation of two indirect methods for quantification of free water transport in peritoneal dialysis. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2005, 25, 77–84. [Google Scholar] [CrossRef]
- Smit, W.; Struijk, D.G.; Ho-Dac-Pannekeet, M.M.; Krediet, R.T. Quantification of free water transport in peritoneal dialysis. Kidney Int. 2004, 66, 849–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parikova, A.; Smit, W.; Struijk, D.G.; Zweers, M.M.; Krediet, R.T. The contribution of free water transport and small pore transport to the total fluid removal in peritoneal dialysis. Kidney Int. 2005, 68, 1849–1856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coester, A.M.; Smit, W.; Struijk, D.G.; Parikova, A.; Krediet, R.T. Longitudinal analysis of peritoneal fluid transport and its determinants in a cohort of incident peritoneal dialysis patients. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2014, 34, 195–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, J.D.; Craig, K.J.; Topley, N.; Von Ruhland, C.; Fallon, M.; Newman, G.R.; Mackenzie, R.K.; Williams, G.T. Morphologic changes in the peritoneal membrane of patients with renal disease. J. Am. Soc. Nephrol. JASN 2002, 13, 470–479. [Google Scholar] [CrossRef]
- Mehrotra, R.; Ravel, V.; Streja, E.; Kuttykrishnan, S.; Adams, S.V.; Katz, R.; Molnar, M.Z.; Kalantar-Zadeh, K. Peritoneal Equilibration Test and Patient Outcomes. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 1990–2001. [Google Scholar] [CrossRef] [Green Version]
- Elphick, E.H.; Teece, L.; Chess, J.A.; Do, J.Y.; Kim, Y.L.; Lee, H.B.; Davison, S.N.; Topley, N.; Davies, S.J.; Lambie, M. Biocompatible Solutions and Long-Term Changes in Peritoneal Solute Transport. Clin. J. Am. Soc. Nephrol. CJASN 2018, 13, 1526–1533. [Google Scholar] [CrossRef] [Green Version]
- Van Esch, S.; Struijk, D.G.; Krediet, R.T. The Natural Time Course of Membrane Alterations During Peritoneal Dialysis Is Partly Altered by Peritonitis. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2016, 36, 448–456. [Google Scholar] [CrossRef]
- Fussholler, A.; zur Nieden, S.; Grabensee, B.; Plum, J. Peritoneal fluid and solute transport: Influence of treatment time, peritoneal dialysis modality, and peritonitis incidence. J. Am. Soc. Nephrol. JASN 2002, 13, 1055–1060. [Google Scholar] [CrossRef]
- Van Diepen, A.T.; van Esch, S.; Struijk, D.G.; Krediet, R.T. The first peritonitis episode alters the natural course of peritoneal membrane characteristics in peritoneal dialysis patients. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2015, 35, 324–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, D.W.; Brown, F.G.; Clarke, M.; Boudville, N.; Elias, T.J.; Foo, M.W.; Jones, B.; Kulkarni, H.; Langham, R.; Ranganathan, D.; et al. The effect of low glucose degradation product, neutral pH versus standard peritoneal dialysis solutions on peritoneal membrane function: The balANZ trial. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2012, 27, 4445–4453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Diepen, A.T.N.; Coester, A.M.; Janmaat, C.J.; Dekker, F.W.; Struijk, D.G.; Krediet, R.T. Comparison of Longitudinal Membrane Function in Peritoneal Dialysis Patients According to Dialysis Fluid Biocompatibility. Kidney Int. Rep. 2020, 5, 2183–2194. [Google Scholar] [CrossRef] [PubMed]
- Honda, K.; Nitta, K.; Horita, S.; Yumura, W.; Nihei, H.; Nagai, R.; Ikeda, K.; Horiuchi, S. Accumulation of advanced glycation end products in the peritoneal vasculature of continuous ambulatory peritoneal dialysis patients with low ultra-filtration. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 1999, 14, 1541–1549. [Google Scholar] [CrossRef] [PubMed]

| Age (years) | 61.15 ± 15.12 |
| Gender (male-female) | 51(60%)–34(40%) |
| Weight (kgr) | 72.61 ± 13.06 |
| Time to 1st PET (days) | 113.50 (IQR 58.50, 497.50) |
| Primary kidney disease | |
| glomerulonephritis | 24 (28.2%) |
| ischaemic/hypertensive nephropathy | 20(23.5%) |
| diabetic nephropathy | 13(15.3%), |
| polycystic disease | 5(5.8%) |
| unknown | 23 (27%) |
| Co-morbidities | |
| Diabetes | 20 (23.5%) |
| Coronary atheromatic disease | 14 (16.5%) |
| Peripheral vascular disease | 12(14.1%) |
| Congestive Heart failure | 5 (5.8%) |
| APD | 20 (23.5%) |
| Albumin (g/dL) | 3.64 ± 0.38 |
| Urea (mg/dL) | 115 (IQR 105, 137) |
| Creatinine (mg/dL) | 5.71 (IQR 4.62, 8.20) |
| KT/V peritoneal | 1.02 (IQR 0.82, 1.27) |
| Residual GFR(mL/min/1.73 m2) | 10.2 ± 4.12 |
| Daily urine volume (mL) | 1312.40 ± 700.20 |
| 60 min | |
| DipDPNa | 0.05 ± 0.04 |
| UF60 (mL) | 375 (IQR 250, 480) |
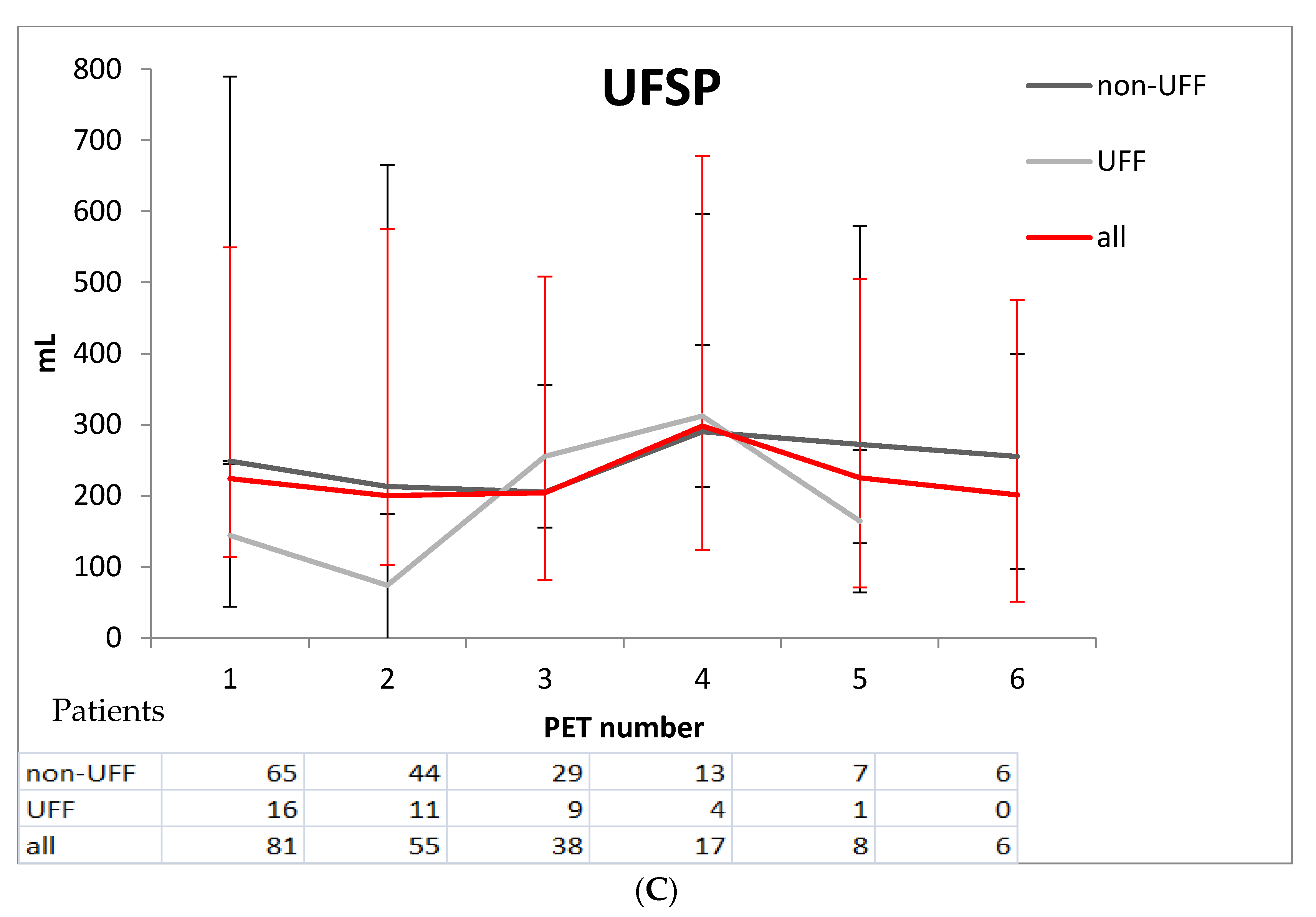
| UFSP (mL) | 235.60 (IQR 111.30, 315.40) |
| FWT (mL) | 175.20± 50.4 |
| corrected FWT (mL) | 214.90 ± 194.70 |
| 240 min | |
| D/P creatinine | 0.74 ± 0.11 |
| D/D0 glucose | 0.29 (IQR 0.24, 0.33) |
| UF 240 (mL) | 655 ± 265 |
| Non UFF (n = 69) | UFF(n = 16) | p-Value | |
|---|---|---|---|
| Age (years) | 64.80 (IQR 51.90, 72.50) | 63.30 (IQR 49.60, 70.60) | 0.6 |
| Gender (male/female) | 26/43 | 8/8 | 0.47 |
| PD duration (months) | 34.40 (IQR 21.30, 63.30) | 49.90 (IQR 26.60, 83.60) | 0.07 |
| UF (mL) | 722 (IQR 622, 848) | 349 (IQR 120.5, 375) | <0.001 |
| D/P cre | 0.71 (IQR 0.66, 0.76) | 0.83 (IQR 0.77, 0.89) | <0.001 |
| Dip D/PNa | 0.048 (IQR 0.03, 0.07) | 0.04 (IQR 0.01, 0.08) | 0.19 |
| UF60 mL | 391 (IQR 292, 480) | 265 (IQR 1, 391) | <0.001 |
| FWT mL | 175.20 (IQR 126.70, 242.10) | 173.30 (IQR 58.50, 202.20) | 0.01 |
| Urine volume (mL) | 1272.10 ± 677.40 | 1490.80 ± 800.10 | 0.01 |
| Standardized β Coefficient | z-Test | p-Value | |
|---|---|---|---|
| D/P cre (0.01 increase) | 13.9 | 3.36 | 0.001 |
| FWT (mL) | −0.0084 | −2.44 | 0.015 |
| UFSP (mL) | −0.0078 | −2.59 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balafa, O.; Duni, A.; Tseke, P.; Rapsomanikis, K.; Pavlakou, P.; Ikonomou, M.; Tatsis, V.; Dounousi, E. Survival of Peritoneal Membrane Function on Biocompatible Dialysis Solutions in a Peritoneal Dialysis Cohort Assessed by a Novel Test. J. Clin. Med. 2021, 10, 3650. https://doi.org/10.3390/jcm10163650
Balafa O, Duni A, Tseke P, Rapsomanikis K, Pavlakou P, Ikonomou M, Tatsis V, Dounousi E. Survival of Peritoneal Membrane Function on Biocompatible Dialysis Solutions in a Peritoneal Dialysis Cohort Assessed by a Novel Test. Journal of Clinical Medicine. 2021; 10(16):3650. https://doi.org/10.3390/jcm10163650
Chicago/Turabian StyleBalafa, Olga, Anila Duni, Paraskevi Tseke, Karolos Rapsomanikis, Paraskevi Pavlakou, Margarita Ikonomou, Vasileios Tatsis, and Evangelia Dounousi. 2021. "Survival of Peritoneal Membrane Function on Biocompatible Dialysis Solutions in a Peritoneal Dialysis Cohort Assessed by a Novel Test" Journal of Clinical Medicine 10, no. 16: 3650. https://doi.org/10.3390/jcm10163650
APA StyleBalafa, O., Duni, A., Tseke, P., Rapsomanikis, K., Pavlakou, P., Ikonomou, M., Tatsis, V., & Dounousi, E. (2021). Survival of Peritoneal Membrane Function on Biocompatible Dialysis Solutions in a Peritoneal Dialysis Cohort Assessed by a Novel Test. Journal of Clinical Medicine, 10(16), 3650. https://doi.org/10.3390/jcm10163650






