Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Decreases Persistent Postoperative Pain Severity in Patients Undergoing Both Open and Laparoscopic Nephrectomies—A Randomized Controlled Trial
Abstract
:1. Introduction
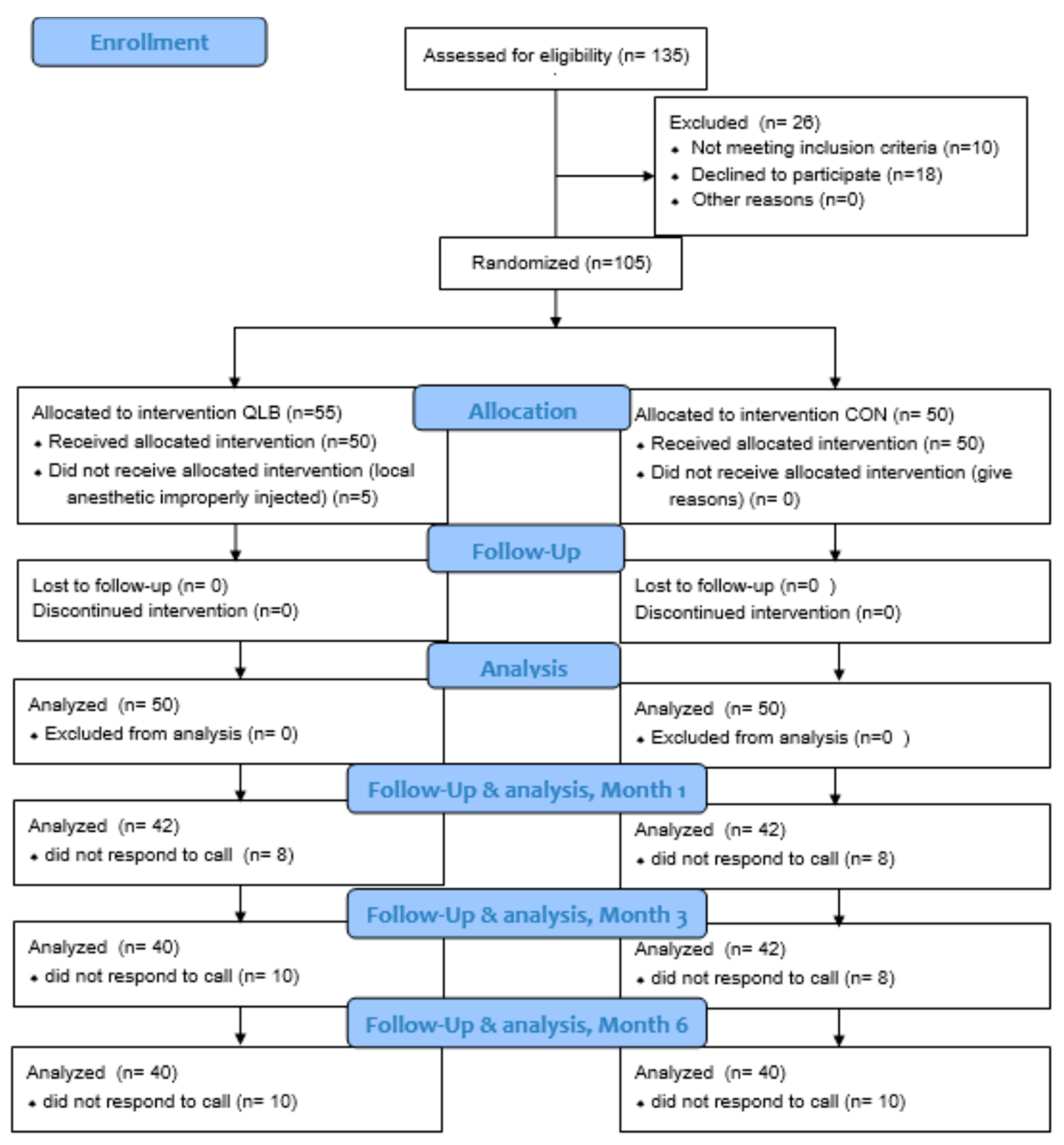
2. Materials and Methods
2.1. Ethical Considerations
2.2. Patient Selection
2.3. Interventions
2.4. Postoperative Care and Pain Management
2.5. Outcomes
2.6. Statistical Analysis
2.7. Power Analysis
3. Results
3.1. Oxycodone Consumption with PCA
3.2. Acute Postoperative Pain and Patient Satisfaction
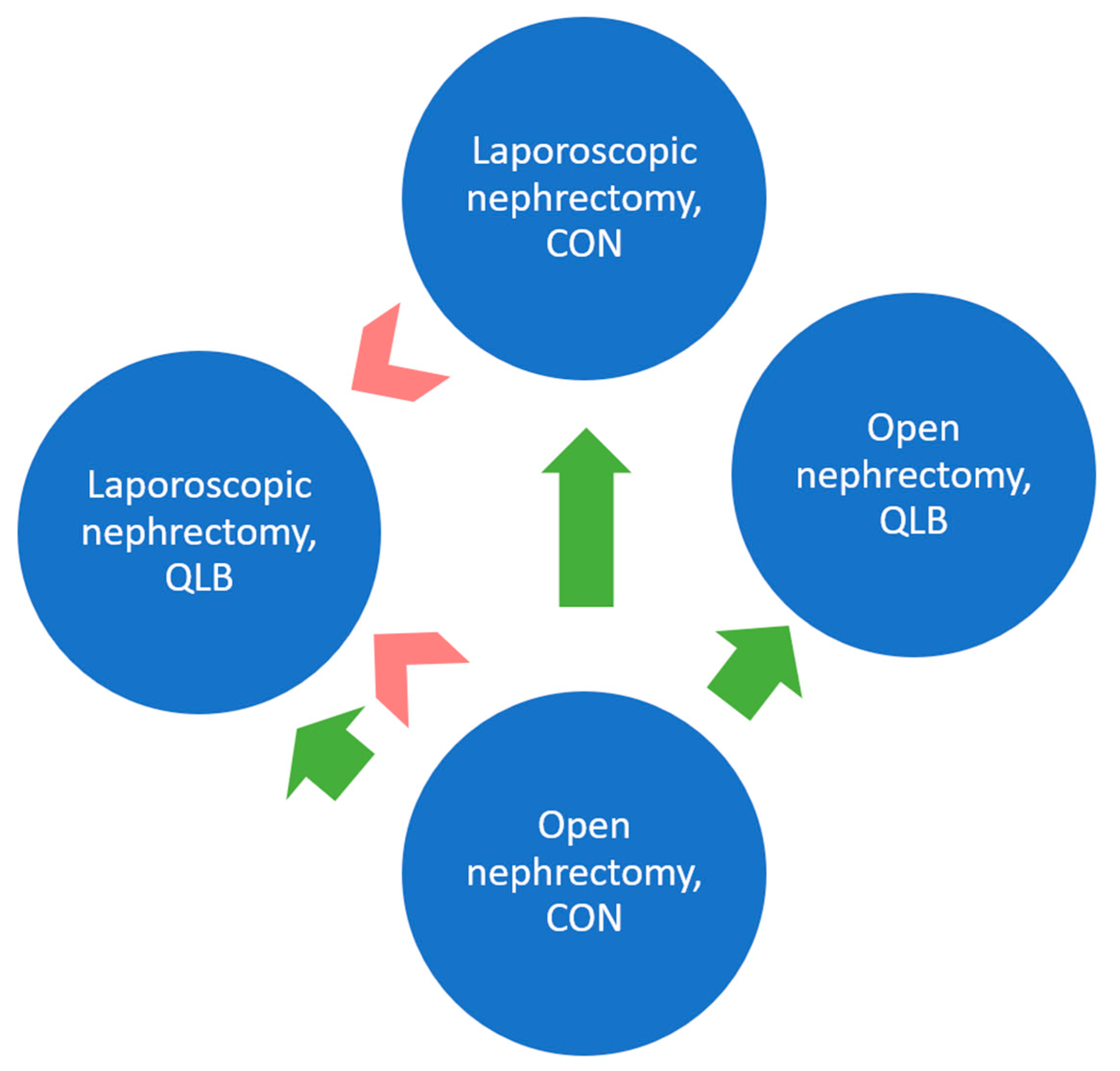
3.3. Presence and Severity of Persistent Postoperative Pain
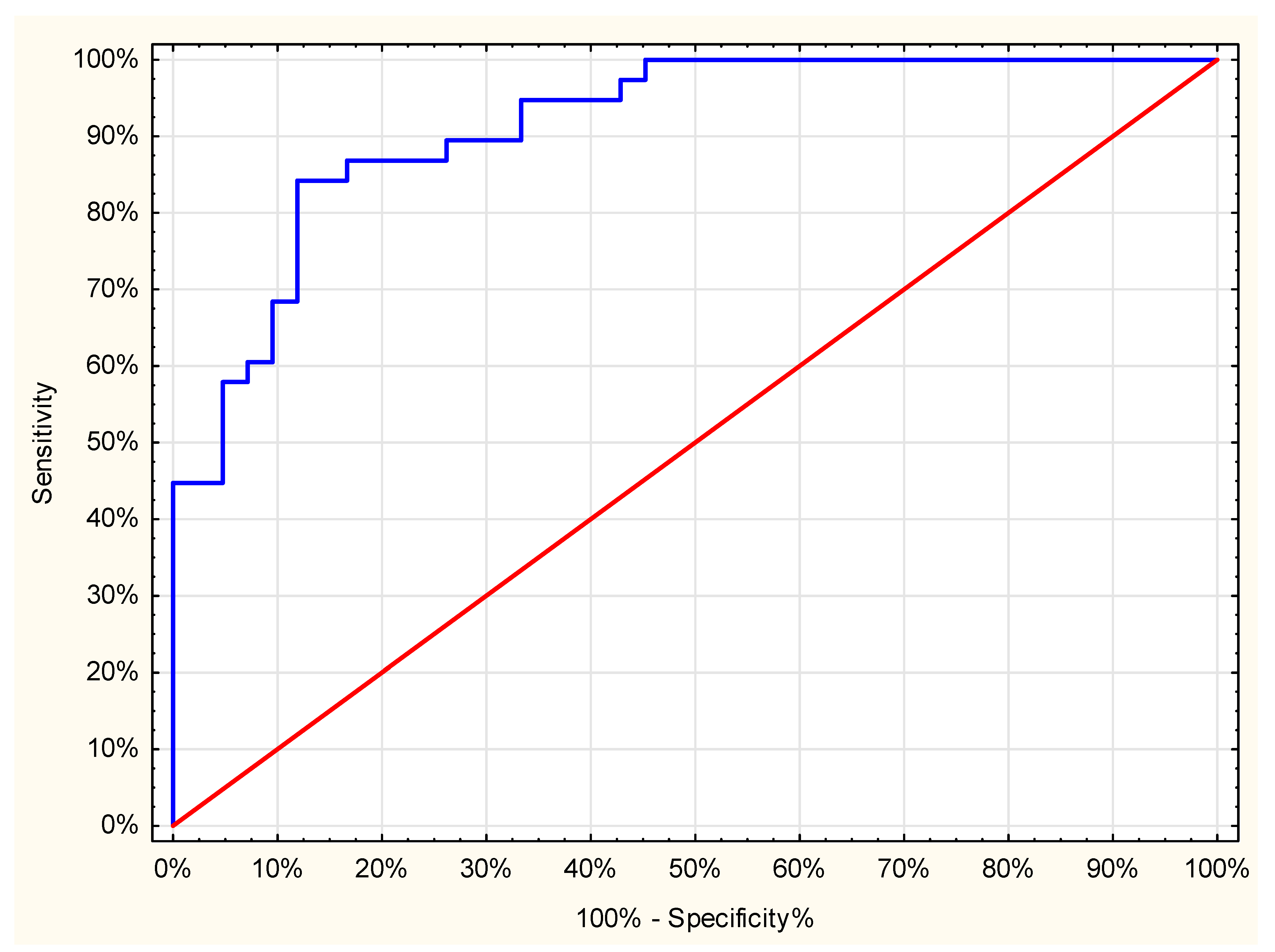
3.4. Persistent Pain Predictors
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alper, I.; Yüksel, E. Comparison of Acute and Chronic Pain After Open Nephrectomy Versus Laparoscopic Nephrectomy: A Prospective Clinical Trial. Medicine 2016, 95, e3433. [Google Scholar] [CrossRef] [PubMed]
- Koo, C.H.; Ryu, J.H. Anesthetic Considerations for Urologic Surgeries. Korean J. Anesthesiol. 2020, 73, 92–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santonastaso, D.P.; de Chiara, A.; Musetti, G.; Bagaphou, C.T.; Gamberini, E.; Agnoletti, V. Ultrasound Guided Erector Spinae Plane Block for Open Partial Nephrectomy: Only an Alternative? J. Clin. Anesth. 2019, 56, 55–56. [Google Scholar] [CrossRef] [PubMed]
- Kwak, K.H.; Baek, S.I.; Kim, J.K.; Kim, T.H.; Yeo, J. Analgesic Effect of Ultrasound-Guided Preoperative Unilateral Lateral Quadratus Lumborum Block for Laparoscopic Nephrectomy: A Randomized, Double-Blinded, Controlled Trial. J. Pain Res. 2020, 13, 1647–1654. [Google Scholar] [CrossRef] [PubMed]
- Dam, M.; Hansen, C.; Poulsen, T.D.; Azawi, N.H.; Laier, G.H.; Wolmarans, M.; Chan, V.; Bendtsen, T.F.; Børglum, J. Transmuscular Quadratus Lumborum Block Reduces Opioid Consumption and Prolongs Time to First Opioid Demand after Laparoscopic Nephrectomy. Reg. Anesth. Pain Med. 2021, 46, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Misiołek, H.; Zajączkowska, R.; Daszkiewicz, A.; Woroń, J.; Dobrogowski, J.; Wordliczek, L.; Owczuk, R. Postoperative Pain Management—2018 Consensus Statement of the Section of Regional Anaesthesia and Pain Therapy of the Polish Society of Anaesthesiology and Intensive Therapy, the Polish Society of Regional Anaesthesia and Pain Therapy, the Polish Association for the Study of Pain and the National Consultant in Anaesthesiology and Intensive Therapy. Anaesthesiol Intensive Ther. 2018, 50, 173–199. [Google Scholar] [CrossRef] [PubMed]
- Blanco, R.; McDonnell, J.G. Optimal Point of Injection: The Quadratus Lumborum Type I and II Blocks. Available online: http://www.respond2articles.com/ANA/forums/post/1550.aspx (accessed on 14 May 2021).
- Baidya, D.K.; Maitra, S.; Arora, M.K.; Agarwal, A. Quadratus Lumborum Block: An Effective Method of Perioperative Analgesia in Children Undergoing Pyeloplasty. J. Clin. Anesth. 2015, 27, 694–696. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, J.; Sá, M.; Reis, H.; Almeida, L.; Sampaio, J.; Pinheiro, C.; Machado, D. Type II Quadratus Lumborum Block for a Sub-Total Gastrectomy in a Septic Patient. Rev. Bras. Anestesiol. 2018, 68, 186–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borys, M.; Zamaro, A.; Horeczy, B.; Gęszka, E.; Janiak, M.; Węgrzyn, P.; Czuczwar, M.; Piwowarczyk, P. Quadratus Lumborum and Transversus Abdominis Plane Blocks and Their Impact on Acute and Chronic Pain in Patients after Cesarean Section: A Randomized Controlled Study. Int. J. Environ. Res. Public Health 2021, 18, 3500. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Sondekoppam, R.; Kalagara, H. Quadratus Lumborum Block: A Technical Review. Curr. Anesthesiol. Rep. 2019, 9, 257–262. [Google Scholar] [CrossRef] [Green Version]
- Aditianingsih, D.; Pryambodho, A.N.; Tantri, A.R.; Mochtar, C.A. A Randomized Controlled Trial on Analgesic Effect of Repeated Quadratus Lumborum Block Versus Continuous Epidural Analgesia Following Laparoscopic Nephrectomy. BMC Anesthesiol. 2019, 19, 221. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Qi, Y.; He, H.; Lou, J.; Pei, Q.; Mei, Y. Analgesic Effect of the Ultrasound-Guided Subcostal Approach to Transmuscular Quadratus Lumborum Block in Patients Undergoing Laparoscopic Nephrectomy: A Randomized Controlled Trial. BMC Anesthesiol. 2019, 19, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouhassira, D.; Attal, N.; Fermanian, J.; Alchaar, H.; Gautron, M.; Masquelier, E.; Rostaing, S.; Lanteri-Minet, M.; Collin, E.; Grisart, J.; et al. Development and Validation of the Neuropathic Pain Symptom Inventory. Pain 2004, 108, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Borys, M.; Hanych, A.; Czuczwar, M. Paravertebral Block Versus Preemptive Ketamine Effect on Pain Intensity After Posterolateral Thoracotomies: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borys, M.; Potręć-Studzińska, B.; Wiech, M.; Piwowarczyk, P.; Sysiak-Sławecka, J.; Rypulak, E.; Gęca, T.; Kwaśniewska, A.; Czuczwar, M. Transversus Abdominis Plane Block and Quadratus Lumborum Block Did Not Reduce the Incidence or Severity of Chronic Postsurgical Pain Following Cesarean Section: A Prospective, Observational Study. Anaesthesiol. Intensive Ther. 2019, 51, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.; Lorgelly, P.; Serpell, M. Chronic Pain Following Donor Nephrectomy—A Study of the Incidence, Nature and Impact of Chronic Post-Nephrectomy Pain. Eur. J. Pain 2010, 14, 732–734. [Google Scholar] [CrossRef] [PubMed]

| Feature | QLB (n = 50) | CON (n = 50) | p-Value |
|---|---|---|---|
| Age (yr) | 61 (49–71) | 62 (57–68) | 0.69 |
| Female | 17 (34%) | 15 (30) | 0.83 |
| Weight (kg) | 80 (72–88) | 80 (74–90) | 0.28 |
| Height (cm) | 171 (164–176) | 169 (164–176) | 0.69 |
| BMI | 27.1 (24.2–30.5) | 28.0 (26.1–30.8) | 0.19 |
| Laparoscopic surgery | 27 (54%) | 22 (44%) | 0.42 |
| Time of surgery (min) | 90 (75–100) | 90 (80–100) | 0.62 |
| Time of anesthesia (min) | 120 (100–135) | 115 (100–125) | 0.09 |
| Intraoperative fentanyl consumption (mcg) | 200 (200–250) | 200 (200–250) | 0.53 |
| Postoperative nausea/vomiting | 4/1 | 7/2 | 0.52/1.0 |
| Hours Post-Surgery | QLB (mm) | CON (mm) | p-Value |
|---|---|---|---|
| 2 | 40 (25–60) | 50 (32–60) | 0.03 |
| 4 | 40 (20–50) | 40 (30–50) | 0.06 |
| 8 | 31 (20–43) | 40 (24–50) | 0.21 |
| 12 | 30 (20–40) | 30 (20–40) | 0.65 |
| 24 | 24 (12–30) | 25 (20–30) | 0.50 |
| Feature | QLB | CON | p-Value |
|---|---|---|---|
| Assessed by patient | 4 (4–5) | 4 (3–4) | <0.001 |
| Assessed by researcher | 4 (4–5) | 4 (3–4) | <0.001 |
| Months after Discharge | QLB | CON | p-Value |
|---|---|---|---|
| Median (interquartile range) persistent pain severity | |||
| 1 | 25 (19–35) | 43 (34–48) | <0.001 |
| 3 | 15 (13–22) | 29 (17–32) | <0.001 |
| 6 | 7 (4–11) | 15 (7–21) | <0.001 |
| Number (%) of patients with persistent pain | |||
| 1 | 41 (98) | 40 (95) | 1 |
| 3 | 38 (95) | 40 (95) | 1 |
| 6 | 34 (85) | 38 (95) | 0.26 |
| Months after Discharge | Laparoscopic Surgery | Open Surgery | p-Value |
|---|---|---|---|
| Median (interquartile range) persistent pain severity | |||
| 1 | 25 (14–38) | 42 (26–47) | <0.001 |
| 3 | 17 (12–23) | 24 (16–32) | <0.01 |
| 6 | 7 (4–11) | 14 (7–20) | <0.01 |
| Number (%) of patients with persistent pain | |||
| 1 | 38 (93) | 43 (100) | 0.11 |
| 3 | 37 (90) | 41 (100) | 0.12 |
| 6 | 34 (85) | 38 (95) | 0.26 |
| Months after Discharge | QLB | CON | p-Value | ||
|---|---|---|---|---|---|
| Laparoscopic Surgery | Open Surgery | Laparoscopic Surgery | Open Surgery | ||
| Median (interquartile range) persistent pain severity | |||||
| 1 | 22 (14–28) | 35 (25–39) | 39 (10–43) | 47 (43–49) | <0.001 |
| 3 | 14 (10–20) | 18 (14–23) | 19 (12–30) | 32 (23–35) | <0.001 |
| 6 | 5 (3–9) | 8 (5–14) | 11 (6–16) | 18 (9–23) | <0.001 |
| Number (%) of patients with persistent pain | |||||
| 1 | 22 (96) | 19 (100) | 16 (89) | 24 (100) | 0.16 |
| 3 | 21 (91) | 17 (100) | 16 (89) | 24 (100) | 0.22 |
| 6 | 19 (83) | 15 (88) | 15 (88) | 23 (100) | 0.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borys, M.; Szajowska, P.; Jednakiewicz, M.; Wita, G.; Czarnik, T.; Mieszkowski, M.; Tuyakov, B.; Gałkin, P.; Rahnama-Hezavah, M.; Czuczwar, M.; et al. Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Decreases Persistent Postoperative Pain Severity in Patients Undergoing Both Open and Laparoscopic Nephrectomies—A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 3590. https://doi.org/10.3390/jcm10163590
Borys M, Szajowska P, Jednakiewicz M, Wita G, Czarnik T, Mieszkowski M, Tuyakov B, Gałkin P, Rahnama-Hezavah M, Czuczwar M, et al. Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Decreases Persistent Postoperative Pain Severity in Patients Undergoing Both Open and Laparoscopic Nephrectomies—A Randomized Controlled Trial. Journal of Clinical Medicine. 2021; 10(16):3590. https://doi.org/10.3390/jcm10163590
Chicago/Turabian StyleBorys, Michał, Patrycja Szajowska, Mariusz Jednakiewicz, Grzegorz Wita, Tomasz Czarnik, Marcin Mieszkowski, Bułat Tuyakov, Piotr Gałkin, Mansur Rahnama-Hezavah, Mirosław Czuczwar, and et al. 2021. "Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Decreases Persistent Postoperative Pain Severity in Patients Undergoing Both Open and Laparoscopic Nephrectomies—A Randomized Controlled Trial" Journal of Clinical Medicine 10, no. 16: 3590. https://doi.org/10.3390/jcm10163590
APA StyleBorys, M., Szajowska, P., Jednakiewicz, M., Wita, G., Czarnik, T., Mieszkowski, M., Tuyakov, B., Gałkin, P., Rahnama-Hezavah, M., Czuczwar, M., & Piwowarczyk, P. (2021). Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Decreases Persistent Postoperative Pain Severity in Patients Undergoing Both Open and Laparoscopic Nephrectomies—A Randomized Controlled Trial. Journal of Clinical Medicine, 10(16), 3590. https://doi.org/10.3390/jcm10163590






