Optimizing Care for Adults with Congenital Heart Disease: Results of a Conjoint Analysis Based on a Nationwide Sample of Patients Included in the German National Register
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Questionnaire
- Step one (Description of the perfect world scenario): The participants were asked to provide information about the perfect scenario regarding an adult CHD doctor’s consultation if no restrictions were present.
- Step two (Testing acceptable trade-offs): Based on the answers given in step one, the participants were asked to limit the selection and to evaluate different scenarios (trade-offs) regarding a doctor’s consultation and to decide whether different scenarios would be acceptable.
- Step three (Combining Steps 1 and 2): Based on the information from steps one and two, participants were presented with three scenarios to choose from. Study participants were asked to choose the most preferable of the remaining options. For in-depth information on the technique employed and the calculations performed, we refer to the published literature [25].
2.2. Statistical Analysis
3. Results
3.1. Descriptive Conjoint Analysis
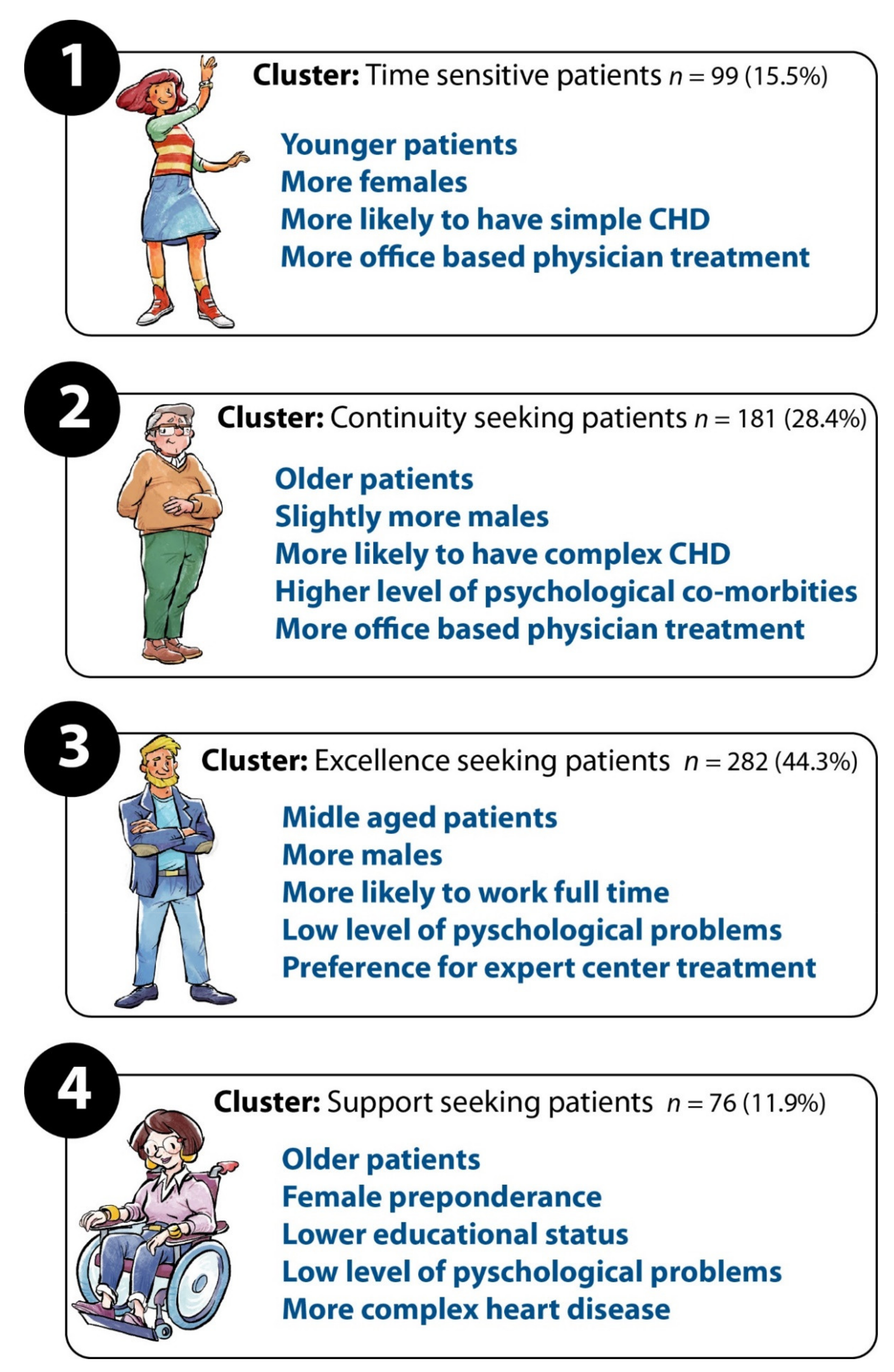
3.2. Cluster Analysis
- Time-sensitive patients focusing on organizational aspects of care with high preference for quick appointments, short driving and waiting time.
- Excellence-seeking patients favoring centers with a high level of expertise and 170 state-of-the art technical equipment.
- Continuity of care cluster of patients seeking to consult the same physician.
- High level of individual support patients including detailed explanations by health care professionals as well as holistic medical treatment.
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CA | Conjoint Analysis |
| CHD | Congenital heart disease |
| SD | Standard deviation |
Appendix A
| Variable | Simple vs. mod. | Simple vs. Complex | Mod. vs. Complex |
|---|---|---|---|
| Medical qualification | p = 0.09 | p < 0.05 | p = 0.62 |
| Care continuity | p = 0.41 | p < 0.05 | p < 0.05 |
| Support by physician | p = 0.09 | p = 0.71 | p = 0.06 |
| Holistic care | p = 0.26 | p = 0.134 | p = 0.53 |
| Explanations | p = 0.35 | p = 0.25 | p = 0.74 |
| Drive time | p = 0.08 | p < 0.01 | p = 0.26 |
| Car access | p = 0.22 | p = 0.44 | p < 0.01 |
| Opening hours | p = 0.77 | p = 0.56 | p = 0.65 |
| Wait for appt. | p = 0.06 | p = 0.25 | p = 0.14 |
| Availability | p = 0.70 | p = 0.13 | p = 0.12 |
| Wait for physician | p = 0.63 | p = 0.08 | p = 0.06 |
| Quality of equipment | p = 0.91 | p = 0.75 | p = 0.53 |
| Hotel aspects | p = 0.63 | p < 0.05 | p = 0.05 |
References
- Hoffman, J.I.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef] [Green Version]
- Schwedler, G.; Lindinger, A.; Lange, P.E.; Sax, U.; Olchvary, J.; Peters, B.; Bauer, U.; Hense, H.W. Frequency and spectrum of congenital heart defects among live births in Germany: A study of the Competence Network for Congenital Heart Defects. Clin. Res. Cardiol. 2011, 100, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef] [PubMed]
- Helm, P.C.; Kempert, S.; Körten, M.A.; Lesch, W.; Specht, K.; Bauer, U.M.M. Congenital heart disease patients’ and parents’ perception of disease-specific knowledge: Health and impairments in everyday life. Congenit. Heart Dis. 2018, 13, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Helm, P.C.; Kaemmerer, H.; Breithardt, G.; Sticker, E.J.; Keuchen, R.; Neidenbach, R.; Diller, G.P.; Tutarel, O.; Bauer, U.M.M. Transition in Patients with Congenital Heart Disease in Germany: Results of a Nationwide Patient Survey. Front. Pediatr. 2017, 5, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marelli, A.J.; Mackie, A.S.; Ionescu-Ittu, R.; Rahme, E.; Pilote, L. Congenital heart disease in the general population: Changing prevalence and age distribution. Circulation 2007, 115, 163–172. [Google Scholar] [CrossRef]
- Kovacs, A.H.; Verstappen, A. The whole adult congenital heart disease patient. Prog. Cardiovasc. Dis. 2011, 53, 247–253. [Google Scholar] [CrossRef]
- Sable, C.; Foster, E.; Uzark, K.; Bjornsen, K.; Canobbio, M.M.; Connolly, H.M.; Graham, T.P.; Gurvitz, M.Z.; Kovacs, A.; Meadows, A.K.; et al. Best practices in managing transition to adulthood for adolescents with congenital heart disease: The transition process and medical and psychosocial issues: A scientific statement from the American Heart Association. Circulation 2011, 123, 1454–1485. [Google Scholar] [CrossRef] [Green Version]
- Diller, G.P.; Breithardt, G.; Baumgartner, H. Congenital heart defects in adulthood. Dtsch. Arztebl. Int. 2011, 108, 452–459. [Google Scholar] [CrossRef]
- Moons, P.; Bovijn, L.; Budts, W.; Belmans, A.; Gewillig, M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 2010, 122, 2264–2272. [Google Scholar] [CrossRef] [Green Version]
- Mackie, A.S.; Ionescu-Ittu, R.; Therrien, J.; Pilote, L.; Abrahamowicz, M.; Marelli, A.J. Children and adults with congenital heart disease lost to follow-up: Who and when? Circulation 2009, 120, 302–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wacker, A.; Kaemmerer, H.; Hollweck, R.; Hauser, M.; Deutsch, M.A.; Brodherr-Heberlein, S.; Eicken, A.; Hess, J. Outcome of operated and unoperated adults with congenital cardiac disease lost to follow-up for more than five years. Am. J. Cardiol. 2005, 95, 776–779. [Google Scholar] [CrossRef]
- Diller, G.; Orwat, S.; Lammers, A.; Radke, R.; De-Torres-Alba, F.; Schmidt, R.; Marschall, U.; Bauer, U.; Enders, D.; Bronstein, L.; et al. Lack of specialist care is associated with increased morbidity and mortality in adult congenital heart disease: A population-based study. Eur. Heart J. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Van Deyk, K.; Marquet, K.; Raes, E.; De Bleser, L.; Budts, W.; De Geest, S. Individual quality of life in adults with congenital heart disease: A paradigm shift. Eur. Heart J. 2005, 26, 298–307. [Google Scholar] [CrossRef]
- Vigl, M.; Niggemeyer, E.; Hager, A.; Schwedler, G.; Kropf, S.; Bauer, U. The importance of socio-demographic factors for the quality of life of adults with congenital heart disease. Qual. Life Res. 2011, 20, 169–177. [Google Scholar] [CrossRef]
- Carroll, J.D.; Green, P.E. Psychometric methods in marketing research: Part I, conjoint analysis. J. Mark. Res. 1995, 32, 385–391. [Google Scholar] [CrossRef] [Green Version]
- Green, P.E.; Srinivasan, V. Conjoint analysis in marketing: New developments with implications for research and practice. J. Mark. 1990, 54, 3–19. [Google Scholar] [CrossRef]
- Hair, J.; Black, W.C.; Babin, B.; Anderson, R. Multivariate Data Analysis; Prentice-Hall: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Iacobucci, D.; Churchill, G. Marketing Research: Methodological Foundations; Cengage Learning: Andover, UK, 2009. [Google Scholar]
- Ryan, M.; Farrar, S. Using conjoint analysis to elicit preferences for health care. BMJ 2000, 320, 1530–1533. [Google Scholar] [CrossRef] [Green Version]
- Ryan, M.; Scott, D.A.; Reeves, C.; Bate, A.; van Teijlingen, E.R.; Russell, E.M.; Napper, M.; Robb, C.M. Eliciting public preferences for healthcare: A systematic review of techniques. Health Technol. Assess. 2001, 5, 1–186. [Google Scholar] [CrossRef]
- Helm, P.C.; Koerten, M.A.; Abdul-Khaliq, H.; Baumgartner, H.; Kececioglu, D.; Bauer, U.M. Representativeness of the German National Register for Congenital Heart Defects: A clinically oriented analysis. Cardiol. Young 2016, 26, 921–926. [Google Scholar] [CrossRef]
- Franklin, R.C.; Jacobs, J.P.; Krogmann, O.N.; Béland, M.J.; Aiello, V.D.; Colan, S.D.; Elliott, M.J.; William Gaynor, J.; Kurosawa, H.; Maruszewski, B.; et al. Nomenclature for congenital and paediatric cardiac disease: Historical perspectives and The International Pediatric and Congenital Cardiac Code. Cardiol. Young 2008, 18 (Suppl. 2), 70–80. [Google Scholar] [CrossRef] [PubMed]
- Warnes, C.A.; Liberthson, R.; Danielson, G.K.; Dore, A.; Harris, L.; Hoffman, J.I.; Somerville, J.; Williams, R.G.; Webb, G.D. Task force 1: The changing profile of congenital heart disease in adult life. J. Am. Coll. Cardiol. 2001, 37, 1170–1175. [Google Scholar] [CrossRef] [Green Version]
- Cunningham, C.E.; Deal, K.; Chen, Y. Adaptive choice-based conjoint analysis: A new patient-centered approach to the assessment of health service preferences. Patient 2010, 3, 257–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonferroni, C. Teoria statistica delle classi e calcolo delle probabilita. Pubbl. R Ist. Super. Sci. Econ. Commericiali Firenze 1936, 8, 3–62. [Google Scholar]
- Kempny, A.; Diller, G.P.; Dimopoulos, K.; Alonso-Gonzalez, R.; Uebing, A.; Li, W.; Babu-Narayan, S.; Swan, L.; Wort, S.J.; Gatzoulis, M.A. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int. J. Cardiol. 2016, 203, 245–250. [Google Scholar] [CrossRef]
- Diller, G.P.; Arvanitaki, A.; Opotowsky, A.R.; Jenkins, K.; Moons, P.; Kempny, A.; Tandon, A.; Redington, A.; Khairy, P.; Mital, S.; et al. Lifespan Perspective on Congenital Heart Disease Research: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 2219–2235. [Google Scholar] [CrossRef]
- Lesch, W.; Specht, K.; Lux, A.; Frey, M.; Utens, E.; Bauer, U. Disease-specific knowledge and information preferences of young patients with congenital heart disease. Cardiol. Young 2014, 24, 321–330. [Google Scholar] [CrossRef]
- Gatzoulis, M.A. Adult congenital heart disease: Education, education, education. Nat. Clin. Pract. Cardiovasc. Med. 2006, 3, 2–3. [Google Scholar] [CrossRef]
- Heery, E.; Sheehan, A.M.; While, A.E.; Coyne, I. Experiences and Outcomes of Transition from Pediatric to Adult Health Care Services for Young People with Congenital Heart Disease: A Systematic Review. Congenit. Heart Dis. 2015, 10, 413–427. [Google Scholar] [CrossRef]





| Variable | All Subjects | Time | Excellence | Continuity | Support |
|---|---|---|---|---|---|
| n = 637 | n = 100 | n = 278 | n = 183 | n = 76 | |
| Physician qualification | 13.3 ± 5.5 | 7.9 ± 3.7 | 15.7 ± 4.6 | 14.5 ± 5.2 | 8.6 ± 3.5 |
| Care continuity | 7.0 ± 4.6 | 4.8 ± 2.9 | 4.9 ± 2.9 | 11.9 ± 4.1 | 5.5 ± 3.4 |
| Support by physician | 8.3 ± 3.3 | 7.0 ± 3.3 | 8.4 ± 3.2 | 8.0 ± 3.2 | 10.5 ± 3.4 |
| Holistic care | 10.4 ± 5 | 9.0 ± 4.7 | 10.1 ± 4.6 | 9.1 ± 4.6 | 16.9 ± 2.7 |
| Explanations | 14.5 ± 4.3 | 15.1 ± 4.4 | 13.5 ± 3.8 | 14.6 ± 4.7 | 17.7 ± 3.6 |
| Drive time | 6.0 ± 3.4 | 9.9 ± 3.5 | 5.4 ± 2.8 | 5.7 ± 3.0 | 4.1 ± 2.2 |
| Car access | 5.1 ± 3.7 | 6.7 ± 4.7 | 5.0 ± 3.3 | 4.7 ± 3.2 | 4.9 ± 4.0 |
| Opening hrs. | 4.1 ± 2.1 | 5.0 ± 2.3 | 3.9 ± 2.0 | 4.1 ± 2.2 | 3.8 ± 2.0 |
| Appt. wait time | 2.7 ± 2.1 | 3.4 ± 2.4 | 2.6 ± 1.9 | 2.7 ± 2.3 | 2.5 ± 1.6 |
| Center availability | 4.0 ± 2.0 | 4.6 ± 2.1 | 3.7 ± 1.8 | 4.2 ± 2.1 | 4.1 ± 1.7 |
| Wait at appt. | 11.6 ± 5.2 | 17.4 ± 3.9 | 11.3 ± 4.8 | 10.2 ± 4.5 | 8.4 ± 4.1 |
| Quality of equipment | 10.2 ± 4.8 | 6.9 ± 3.4 | 13.1 ± 4.2 | 7.4 ± 3.6 | 10.7 ± 4.4 |
| Hotel aspects | 2.6 ± 17.0 | 2.5 ± 1.7 | 2.5 ± 1.6 | 2.9 ± 1.9 | 2.5 ± 1.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lammers, A.E.; Helm, P.C.; Bauer, U.M.; van Huelsen, A.-K.; Schneider, H.; Baumgartner, H.; Diller, G.-P. Optimizing Care for Adults with Congenital Heart Disease: Results of a Conjoint Analysis Based on a Nationwide Sample of Patients Included in the German National Register. J. Clin. Med. 2021, 10, 3483. https://doi.org/10.3390/jcm10163483
Lammers AE, Helm PC, Bauer UM, van Huelsen A-K, Schneider H, Baumgartner H, Diller G-P. Optimizing Care for Adults with Congenital Heart Disease: Results of a Conjoint Analysis Based on a Nationwide Sample of Patients Included in the German National Register. Journal of Clinical Medicine. 2021; 10(16):3483. https://doi.org/10.3390/jcm10163483
Chicago/Turabian StyleLammers, Astrid E., Paul C. Helm, Ulrike M. Bauer, Ann-Kathrin van Huelsen, Helmut Schneider, Helmut Baumgartner, and Gerhard-Paul Diller. 2021. "Optimizing Care for Adults with Congenital Heart Disease: Results of a Conjoint Analysis Based on a Nationwide Sample of Patients Included in the German National Register" Journal of Clinical Medicine 10, no. 16: 3483. https://doi.org/10.3390/jcm10163483
APA StyleLammers, A. E., Helm, P. C., Bauer, U. M., van Huelsen, A.-K., Schneider, H., Baumgartner, H., & Diller, G.-P. (2021). Optimizing Care for Adults with Congenital Heart Disease: Results of a Conjoint Analysis Based on a Nationwide Sample of Patients Included in the German National Register. Journal of Clinical Medicine, 10(16), 3483. https://doi.org/10.3390/jcm10163483






