Postoperative Changes in Pulmonary Function after Valve Surgery: Oxygenation Index Early after Cardiopulmonary Is a Predictor of Postoperative Course
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Approval and Patients
2.2. Anesthesia and Surgical Technique
2.3. Ventilator Setting, Blood Gas Analyses, and Extubation Criteria
2.4. Data Collection and Statistical Analysis
3. Results
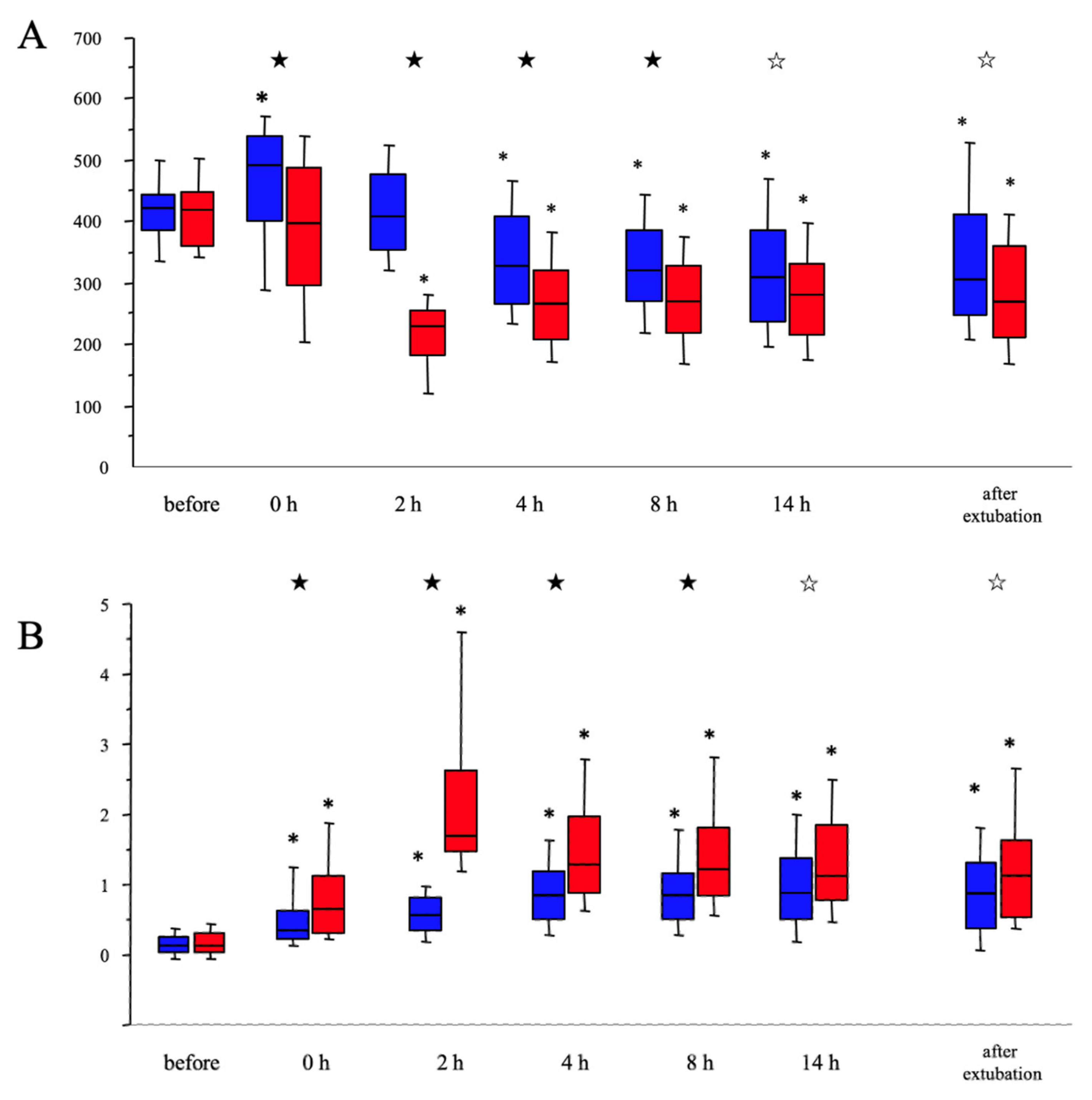
3.1. Patient Characteristics and Perioperative Changes in Pulmonary Function
3.2. Univariate and Multivariate Analysis for Prolonged DMV
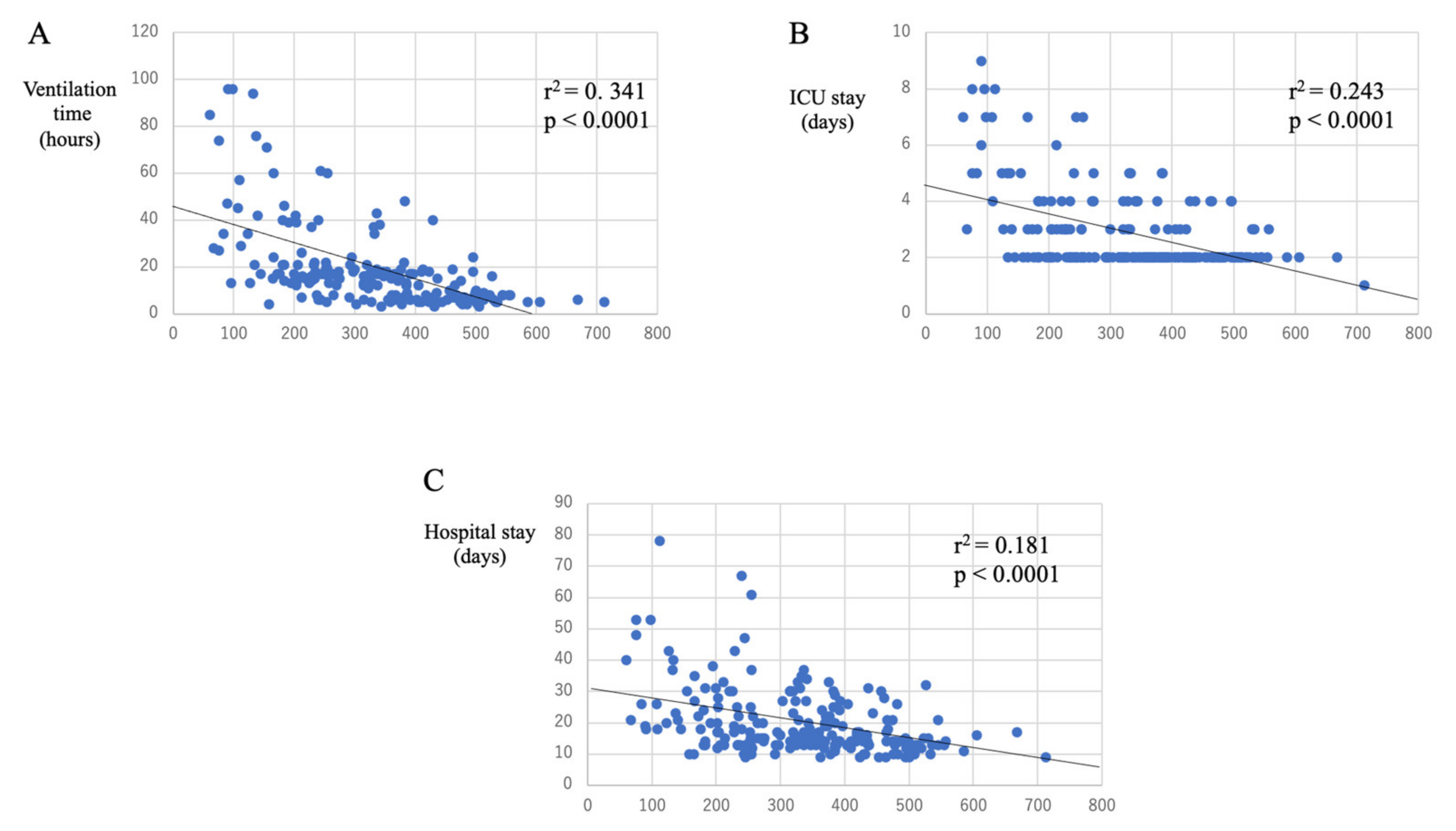
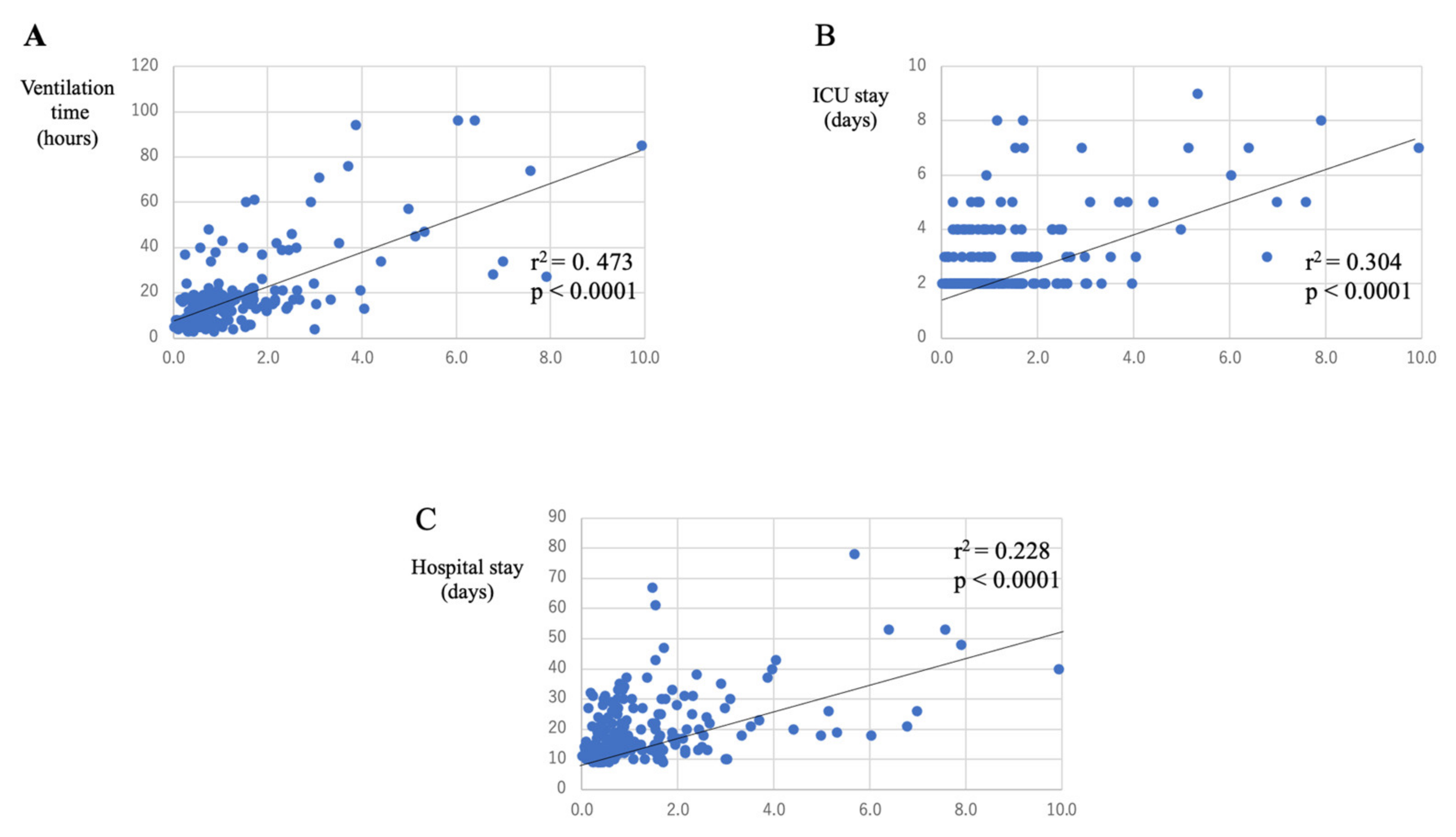
3.3. Relationship between Post-CPB Pulmonary Function and Postoperative Course
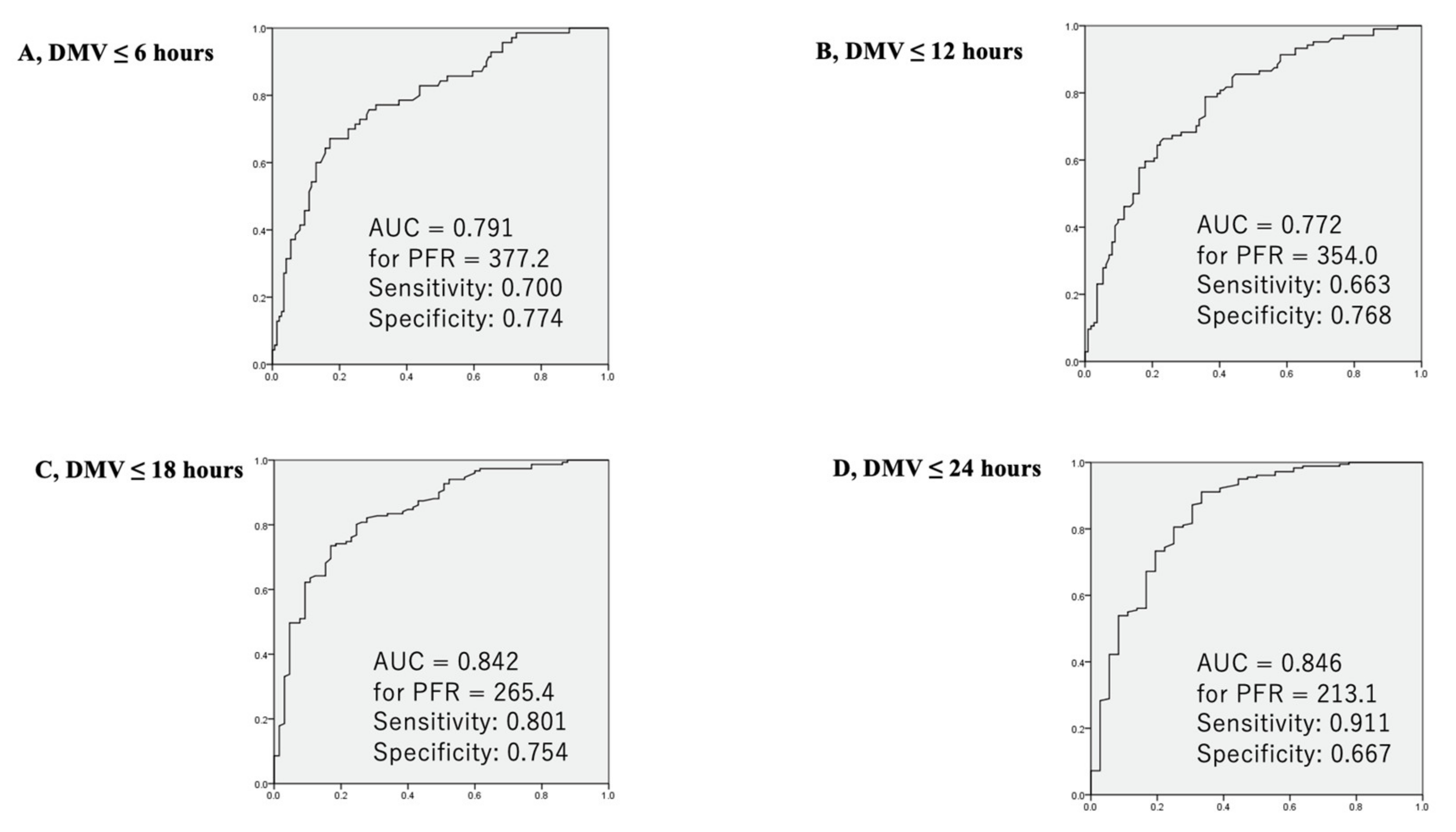
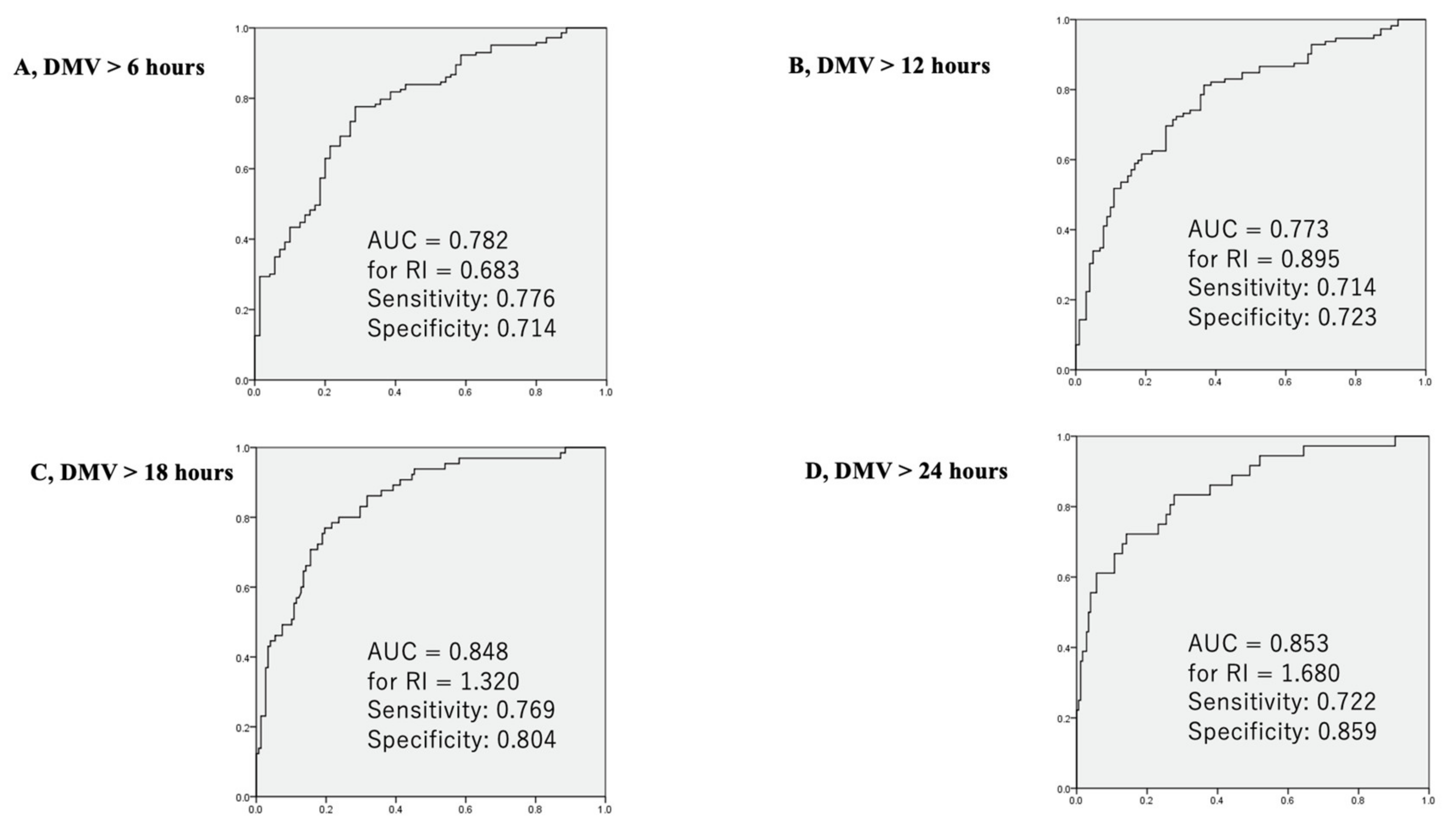
3.4. ROC Analysis between Pulmonary Functions at Two Hours after CPB and DMV
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, W.; Li, N.; Jin, Z.-H.; Lv, X.-Q.; Cui, X.-G. Effect of preoperative inhaled budesonide on pulmonary injury after cardiopulmonary bypass: A randomized pilot study. J. Thorac. Cardiovasc. Surg. 2019, 157, 272–284. [Google Scholar] [CrossRef] [PubMed]
- Apostolakis, E.; Filos, K.S.; Koletsis, E.; Dougenis, D. Lung Dysfunction Following Cardiopulmonary Bypass. J. Card. Surg. 2010, 25, 47–55. [Google Scholar] [CrossRef]
- Taggart, D.P.; El-Fiky, M.; Carter, R.; Bowman, A.; Wheatley, D.J. Respiratory dysfunction after uncomplicated cardiopulmonary bypass. Ann. Thorac. Surg. 1993, 56, 1123–1128. [Google Scholar] [CrossRef]
- Zhu, F.; Lee, A.; Chee, Y.E. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst. Rev. 2012, 10, CD003587. [Google Scholar]
- Wong, W.T.; Lai, V.K.; Chee, Y.E.; Lee, A. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst. Rev. 2016, 9, CD003587. [Google Scholar] [CrossRef] [PubMed]
- Rhee, K.-Y.; Sung, T.-Y.; Kim, J.D.; Kang, H.; Mohamad, N.; Kim, T.-Y. High-dose ulinastatin improves postoperative oxygenation in patients undergoing aortic valve surgery with cardiopulmonary bypass: A retrospective study. J. Int. Med. Res. 2018, 46, 1238–1248. [Google Scholar] [CrossRef]
- Fan, E.; Brodie, D.; Slutsky, A. Acute respiratory distress syndrome advances in diagnosis and treatment. JAMA 2018, 319, 698–710. [Google Scholar] [CrossRef] [PubMed]
- García-Delgado, M.; Navarrete-Sánchez, I.; Colmenero, M. Preventing and managing perioperative pulmonary complications following cardiac surgery. Curr. Opin. Anaesthesiol. 2014, 27, 146–152. [Google Scholar] [CrossRef]
- Saleh, H.Z.; Shaw, M.; Al-Rawi, O.; Yates, J.; Pullan, M.; Chalmers, J.A.C.; Fabri, B.M. Outcomes and predictors of prolonged ventilation in patients undergoing elective coronary surgery. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 51–56. [Google Scholar] [CrossRef]
- Cislaghi, F.; Condemi, A.M.; Corona, A. Predictors of prolonged mechanical ventilation in a cohort of 5123 cardiac surgical patients. Eur. J. Anesthesiol. 2009, 26, 396–403. [Google Scholar] [CrossRef] [PubMed]
- London, M.J.; Shroyer, A.L.; Coll, J.R.; Mawhinney, S.; Fullerton, D.A.; Hammermeister, K.E.; Grover, F.L. Early Extubation following Cardiac Surgery in a Veterans Population. Anesthesiology 1998, 88, 1447–1458. [Google Scholar] [CrossRef]
- Zhu, F.; Gomersall, C.D.; Ng, S.K.; Underwood, M.J.; Lee, A. A Randomized Controlled Trial of Adaptive Support Ventilation Mode to Wean Patients after Fast-track Cardiac Valvular Surgery. Anesthesiology 2015, 122, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Hiromoto, A.; Maeda, M.; Murata, T.; Shirakawa, M.; Okamoto, J.; Maruyama, Y.; Imura, H. Early extubation in current valve surgery requiring long cardiopulmonary bypass: Benefits and predictive value of preoperative spirometry. Heart Lung 2020, 49, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, N.; Morimoto, K.; Morimoto, Y.; Takahashi, H.; Asano, M.; Matsumori, M.; Okada, K.; Okita, Y. Sivelestat attenuates postoperative pulmonary dysfunction after total arch replacement under deep hypothermia. Eur. J. Cardio-Thoracic Surg. 2008, 34, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Gasparovic, H.; Plestina, S.; Sutlic, Z.; Husedzinovic, I.; Coric, V.; Ivancan, V.; Jelic, I. Pulmonary lactate release following cardiopulmonary bypass. Eur. J. Cardio-Thoracic Surg. 2007, 32, 882–887. [Google Scholar] [CrossRef][Green Version]
- Imura, H.; Caputo, M.; Lim, K.; Ochi, M.; Suleiman, M.S.; Shimizu, K.; Angelini, G.D. Pulmonary injury after cardiopulmonary bypass: Beneficial effects of low-frequency mechanical ventilation. J. Thorac. Cardiovasc. Surg. 2009, 137, 1530–1537. [Google Scholar] [CrossRef] [PubMed]
- Weiss, Y.G.; Merin, G.; Koganov, E.; Ribo, A.; Oppenheim-Eden, A.; Medalion, B.; Peruanski, M.; Reider, E.; Bar-Ziv, J.; Hanson, W.C.; et al. Postcardiopulmonary bypass hypoxemia: A prospective study on incidence, risk factors, and clinical significance. J. Cardiothorac. Vasc. Anesth. 2000, 14, 506–513. [Google Scholar] [CrossRef]
- Huffmyer, J.L.; Groves, D.S. Pulmonary complications of cardiopulmonary bypass. Best Pr. Res. Clin. Anaesthesiol. 2015, 29, 163–175. [Google Scholar] [CrossRef]
- Magnusson, L.; Zemgulis, V.; Tenling, A.; Wernlund, J.; Tyden, H.; Thelin, S.; Hedenstierna, G. Use of a vital capacity maneuver to prevent atelectasis after cardiopulmonary bypass an experimental study. Anesthesiologists 1998, 88, 134–142. [Google Scholar] [CrossRef]
- Rodrigues, R.R.; Sawada, A.Y.; Rouby, J.J.; Fukuda, M.J.; Neves, F.H.; Carmona, M.J.; Pelosi, P.; Auler, J.O.; Malbouisson, L.M. Computed tomography assessment of lung structure in patients undergoing cardiac surgery with cardiopulmonary bypass. Braz. J. Med. Biol. Res. 2011, 44, 598–605. [Google Scholar] [CrossRef]
- Walthall, H.; Ray, S.R. Do any intraoperative variables have an effect on the timing of tracheal extubation after coronary artery bypass graft surgery? Heart Lung 2002, 31, 432–439. [Google Scholar] [CrossRef] [PubMed]
| Whole Cohort | PFR *7 ≥ 300 | PFR < 300 | p-Value *8 | |
|---|---|---|---|---|
| Number of patients | 225 | 137 | 88 | |
| Age (years) | 67.7 ± 13.16 | 66.6 ± 14.22 | 69.3 ± 11.20 | 0.299 |
| Octogenarian (%) | ||||
| Male (%) | 154 (68.4%) | 91 (66.4%) | 63 (71.6%) | 0.464 |
| Body mass index | 22.9 ± 3.99 | 22.3 ± 3.85 | 23.8 ± 4.07 | 0.017 |
| Previous smoking (%) | 119 (52.9%) | 67 (48.9%) | 52 (59.1%) | 0.171 |
| Current smoking (%) | 33 (14.7%) | 17 (12.4%) | 16 (18.2%) | 0.251 |
| Diabetes mellitus (%) | 52 (23.1%) | 25 (18.2%) | 27 (30.7%) | 0.036 |
| Hypertension (%) | 170 (75.6%) | 97 (70.8%) | 73 (83.0%) | 0.040 |
| Hyperlipidemia (%) | 135 (60.0%) | 78 (56.9%) | 57 (64.8%) | 0.266 |
| Hemodialysis (%) | 16 (7.1%) | 4 (2.9%) | 12 (13.6%) | 0.003 |
| eGFR *1 | 60.13 ± 26.20 | 65.07 ± 26.01 | 56.18 ± 27.53 | 0.039 |
| Previous stroke (%) | 29 (12.9%) | 13 (9.5%) | 16 (18.2%) | 0.068 |
| Hemoglobin (g/dL) | 12.7 ± 3.94 | 12.6 ± 1.96 | 12.9 ± 5.82 | 0.245 |
| Platelet (/mL) | 203.5 ± 83.64 | 208.8 ± 91.16 | 195.3 ± 69.99 | 0.472 |
| NYHA ≥ II (%) | 160 (71.1%) | 95 (69.3%) | 65 (73.8%) | 0.547 |
| Peripheral arterial disease | 12 (5.3%) | 4 (2.9%) | 8 (9.1%) | 0.066 |
| LVEF (%) | 62.5 ± 18.6 | 62.8 ± 14.20 | 62.0 ± 23.99 | 0.116 |
| Pulmonary hypertension *2 (%) | 47 (20.9%) | 25 (18.2%) | 22 (25.0%) | 0.242 |
| COPD *3 (%) | 67 (29.8%) | 38 (27.7%) | 29 (33.0%) | 0.455 |
| PO2 *4 (mmHg) | 85.9 ± 14.51 | 88.2 ± 14.11 | 82.2 ± 15.18 | 0.337 |
| PCO2 *4 (mmHg) | 39.0 ± 5.23 | 39.8 ± 5.18 | 37.8 ± 5.34 | 0.782 |
| %VC *5 | 86.4 ± 18.56 | 90.9 ± 18.47 | 79.4 ± 18.78 | 0.659 |
| FEV1% *6 | 88.2 ± 23.64 | 92.5 ± 23.77 | 81.4 ± 23.56 | 0.655 |
| Whole Cohort | PFR ≥ 300 | PFR *9 < 300 | p-Value *10 | |
|---|---|---|---|---|
| (Type of operation) | ||||
| Mitral valve surgery | 96 (42.7%) | 68 (49.6%) | 28 (31.8%) | 0.009 |
| Aortic valve surgery | 106 (47.1%) | 64 (46.7%) | 42 (47.7%) | 0.892 |
| Mitral + Aortic valves | 23 (10.2%) | 5 (3.6%) | 18 (20.5%) | <0.001 |
| Additional procedures | 118 (52.4%) | 65 (47.4%) | 53 (60.2%) | 0.075 |
| Tricuspid repair | 47 (20.9%) | 34 (24.8%) | 13 (14.8%) | 0.092 |
| CABG *1 | 52 (23.1%) | 26 (19.0%) | 26 (29.5%) | 0.076 |
| Maze | 34 (15.1%) | 15 (10.9%) | 19 (21.6%) | 0.036 |
| Emergency | 15 (6.7%) | 5 (3.6%) | 10 (11.4%) | 0.003 |
| Re-sternotomy | 5 (2.2%) | 1 (1.1%) | 4 (2.9%) | 0.651 |
| (Intraoperative parameters) | ||||
| Operation time (min) | 305.3 ± 107.18 | 281.3 ± 89.4 | 342.7 ± 119.1 | <0.001 |
| CPB *2 time (min) | 166.1 ± 68.52 | 147.2 ± 50.4 | 195.4 ± 80.4 | <0.001 |
| ACC *3 time (min) | 101.7 ± 38.0 | 96.2 ± 33.4 | 110.4 ± 41.9 | <0.001 |
| Fentanyl | 17.4 ± 4.5 | 17.2 ± 4.8 | 17.7 ± 4.3 | 0.463 |
| RBC *4 transfusion (unit) | 99 (44.0%) | 50 (36.5%) | 49 (55.7%) | 0.003 |
| FFP *5 transfusion (unit) | 74 (32.9%) | 38 (27.7%) | 36 (40.9%) | 0.040 |
| Platelet transfusion (%) | 33 (14.7%) | 10 (7.3%) | 23 (26.1%) | <0.001 |
| Water balance (mL) | 2560 ± 2080 | 2148 ± 1655 | 3200 ± 2447 | <0.001 |
| lowest hemoglobin *6 | 6.8 ± 1.23 | 6.9 ± 1.27 | 6.6 ± 1.17 | 0.516 |
| (Postoperative parameters) | ||||
| Inotrope ≥ medium *7 | 44 (19.6%) | 24 (17.5%) | 20 (22.7%) | 0.305 |
| Transfusion *8 | 21 (9.3%) | 9 (6.6%) | 12 (13.6%) | 0.097 |
| Adverse events (%) | 41 (18.2%) | 16 (11.7%) | 25 (28.4%) | 0.001 |
| Ventilation time (h) | 18.9 ± 22.75 | 11.4 ± 7.9 | 30.5 ± 31.78 | <0.001 |
| ICU stay (days) | 3.2 ± 5.47 | 2.9 ± 6.62 | 3.6 ± 2.72 | <0.001 |
| Hospital stay (days) | 20.0 ± 17.47 | 18.4 ± 19.23 | 22.6 ± 13.72 | <0.001 |
| Hospital death (%) | 0.9 | 0.0 | 2.3 | 0.152 |
| Ventilation Time | ICU *4 Stay | Hospital Stay | ||||
|---|---|---|---|---|---|---|
| Time after CPB *1 | Coefficient (r2) | p-Value | Coefficient (r2) | p-Value | Coefficient (r2) | p-Value |
| (immediate) | ||||||
| PFR *2 | 0.104 | <0.001 | 0.038 | 0.006 | 0.034 | 0.011 |
| RI *3 | 0.112 | <0.001 | 0.067 | 0.001 | 0.071 | <0.001 |
| (2 h) | ||||||
| PFR | 0.294 | <0.001 | 0.145 | <0.001 | 0.126 | <0.001 |
| RI | 0.369 | <0.001 | 0.213 | <0.001 | 0.121 | <0.001 |
| (4 h) | ||||||
| PFR | 0.085 | <0.001 | 0.045 | 0.002 | 0.053 | 0.001 |
| RI | 0.181 | <0.001 | 0.091 | 0.006 | 0.061 | <0.001 |
| (8 h) | ||||||
| PFR | 0.102 | <0.001 | 0.074 | <0.001 | 0.060 | <0.001 |
| RI | 0.264 | <0.001 | 0.153 | <0.001 | 0.061 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murata, T.; Maeda, M.; Amitani, R.; Hiromoto, A.; Shirakawa, M.; Kambe, M.; Maruyama, Y.; Imura, H. Postoperative Changes in Pulmonary Function after Valve Surgery: Oxygenation Index Early after Cardiopulmonary Is a Predictor of Postoperative Course. J. Clin. Med. 2021, 10, 3262. https://doi.org/10.3390/jcm10153262
Murata T, Maeda M, Amitani R, Hiromoto A, Shirakawa M, Kambe M, Maruyama Y, Imura H. Postoperative Changes in Pulmonary Function after Valve Surgery: Oxygenation Index Early after Cardiopulmonary Is a Predictor of Postoperative Course. Journal of Clinical Medicine. 2021; 10(15):3262. https://doi.org/10.3390/jcm10153262
Chicago/Turabian StyleMurata, Tomohiro, Motohiro Maeda, Ryosuke Amitani, Atsushi Hiromoto, Makoto Shirakawa, Masaru Kambe, Yuji Maruyama, and Hajime Imura. 2021. "Postoperative Changes in Pulmonary Function after Valve Surgery: Oxygenation Index Early after Cardiopulmonary Is a Predictor of Postoperative Course" Journal of Clinical Medicine 10, no. 15: 3262. https://doi.org/10.3390/jcm10153262
APA StyleMurata, T., Maeda, M., Amitani, R., Hiromoto, A., Shirakawa, M., Kambe, M., Maruyama, Y., & Imura, H. (2021). Postoperative Changes in Pulmonary Function after Valve Surgery: Oxygenation Index Early after Cardiopulmonary Is a Predictor of Postoperative Course. Journal of Clinical Medicine, 10(15), 3262. https://doi.org/10.3390/jcm10153262






