Long-Term Effects of Pedicle Clamping during Major Hepatectomy for Colorectal Liver Metastases
Abstract
1. Introduction
2. Materials and Methods
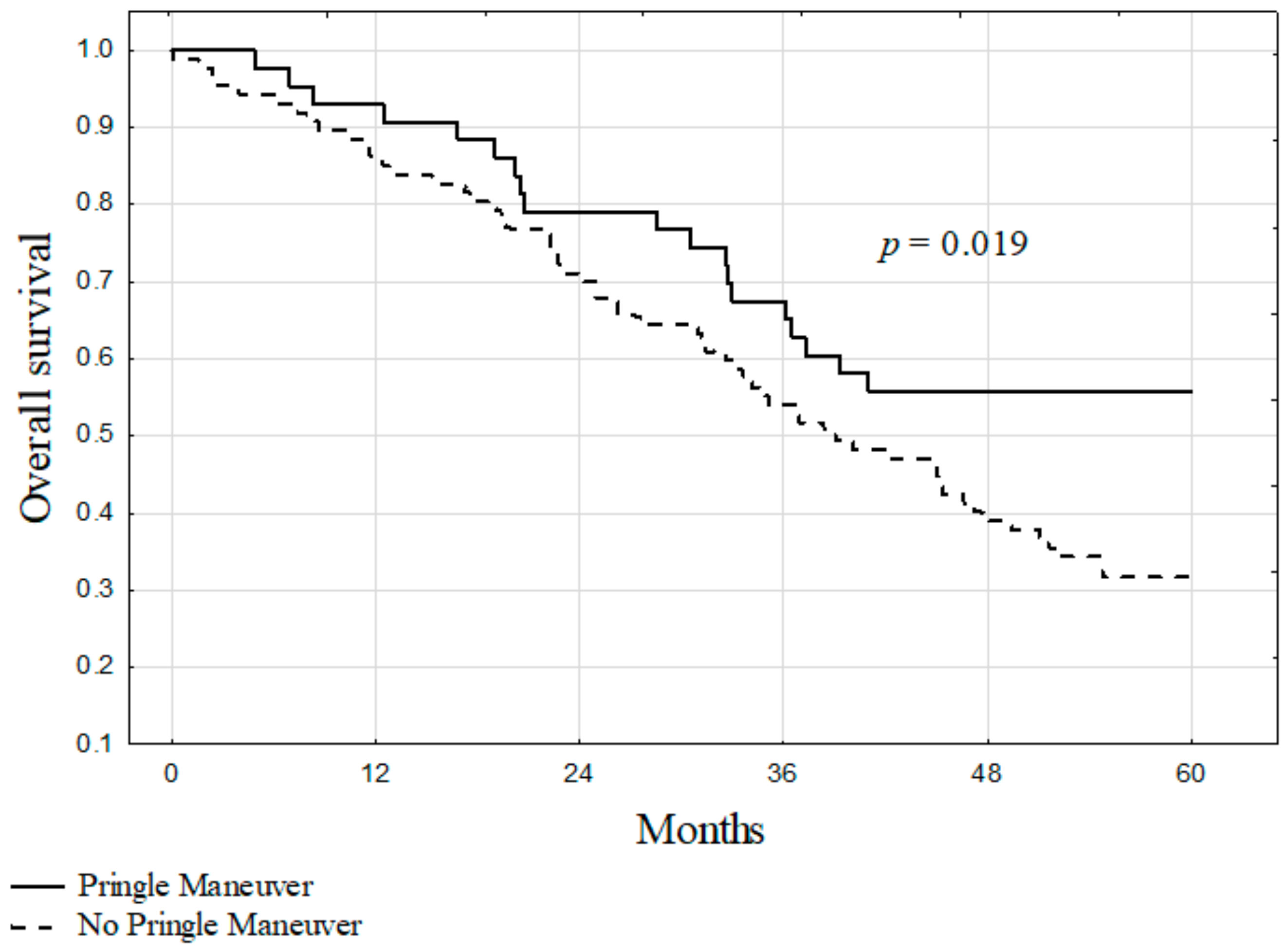
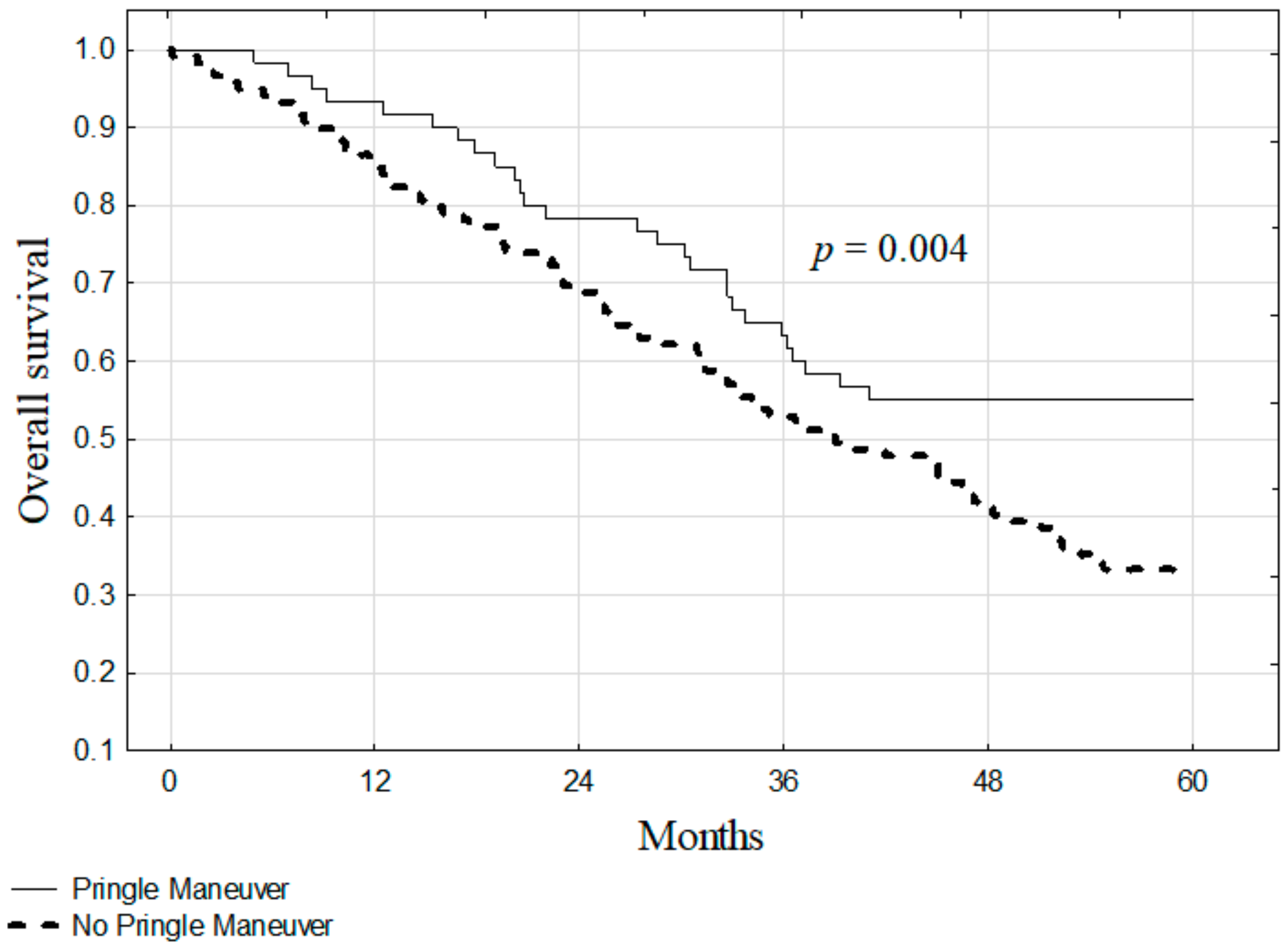
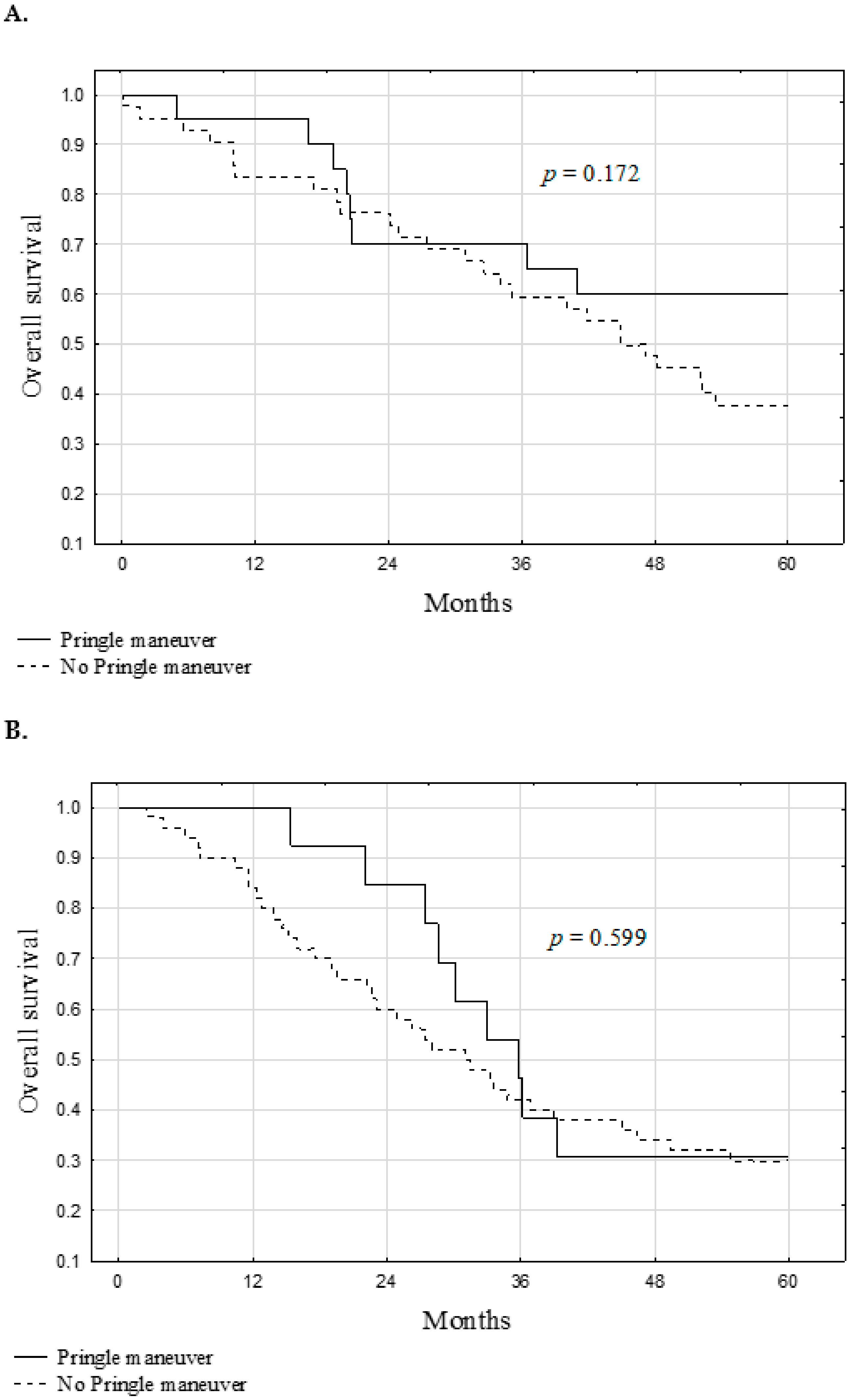
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Latchana, N.; Hirpara, D.H.; Hallet, J.; Karanicolas, P.J. Red blood cell transfusion in liver resection. Langenbecks Arch. Surg. 2019, 404, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, E.K.; Noun, R.; Belghiti, J. Hepatic vascular occlusion: Which technique? Surg. Clin. N. Am. 2004, 84, 563–585. [Google Scholar] [CrossRef]
- Jamieson, G.G.; Corbel, L.; Campion, J.P.; Launois, B. Major liver resection without a blood transfusion: Is it a realistic objective? Surgery 1992, 112, 32–36. [Google Scholar]
- Quesnelle, K.M.; Bystrom, P.V.; Toledo-Pereyra, L.H. Molecular responses to ischemia and reperfusion in the liver. Arch. Toxicol. 2015, 89, 651–657. [Google Scholar] [CrossRef]
- Zhai, Y.; Petrowsky, H.; Hong, J.C.; Busuttil, R.W.; Kupiec-Weglinski, J.W. Ischaemia-reperfusion injury in liver transplantation--from bench to bedside. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 79–89. [Google Scholar] [CrossRef]
- Jimenez-Castro, M.B.; Cornide-Petronio, M.E.; Gracia-Sancho, J.; Peralta, C. Inflammasome-Mediated Inflammation in Liver Ischemia-Reperfusion Injury. Cells 2019, 8, 1131. [Google Scholar] [CrossRef]
- Hao, S.; Chen, S.; Yang, X.; Wan, C. Impact of intermittent portal clamping on the early recurrence of hepatocellular carcinoma after surgery. Surg. Today 2016, 46, 1290–1295. [Google Scholar] [CrossRef] [PubMed]
- van der Bilt, J.D.; Kranenburg, O.; Nijkamp, M.W.; Smakman, N.; Veenendaal, L.M.; Te Velde, E.A.; Voest, E.E.; van Diest, P.J.; Borel Rinkes, I.H. Ischemia/reperfusion accelerates the outgrowth of hepatic micrometastases in a highly standardized murine model. Hepatology 2005, 42, 165–175. [Google Scholar] [CrossRef]
- Sasaki, K.; Morioka, D.; Conci, S.; Margonis, G.A.; Sawada, Y.; Ruzzenente, A.; Kumamoto, T.; Iacono, C.; Andreatos, N.; Guglielmi, A.; et al. The Tumor Burden Score: A New “Metro-ticket” Prognostic Tool for Colorectal Liver Metastases Based on Tumor Size and Number of Tumors. Ann. Surg. 2018, 267, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Fagenson, A.M.; Gleeson, E.M.; Nabi, F.; Lau, K.N.; Pitt, H.A. When does a Pringle Maneuver cause harm? HPB 2021, 23, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Ishizuka, M.; Kubota, K.; Kita, J.; Shimoda, M.; Kato, M.; Sawada, T. Duration of hepatic vascular inflow clamping and survival after liver resection for hepatocellular carcinoma. Br. J. Surg. 2011, 98, 1284–1290. [Google Scholar] [CrossRef] [PubMed]
- Xia, F.; Lau, W.Y.; Xu, Y.; Wu, L.; Qian, C.; Bie, P. Does hepatic ischemia-reperfusion injury induced by hepatic pedicle clamping affect survival after partial hepatectomy for hepatocellular carcinoma? World J. Surg. 2013, 37, 192–201. [Google Scholar] [CrossRef]
- Huang, J.; Tang, W.; Hernandez-Alejandro, R.; Bertens, K.A.; Wu, H.; Liao, M.; Li, J.; Zeng, Y. Intermittent hepatic inflow occlusion during partial hepatectomy for hepatocellular carcinoma does not shorten overall survival or increase the likelihood of tumor recurrence. Medicine 2014, 93, e288. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.F.; Chong, C.C.N.; Cheung, S.Y.S.; Wong, J.; Fung, A.K.Y.; Lok, H.T.; Lai, P.B.S. Impact of Intermittent Pringle Maneuver on Long-Term Survival After Hepatectomy for Hepatocellular Carcinoma: Result from Two Combined Randomized Controlled Trials. World J. Surg. 2019, 43, 3101–3109. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.F.; Cheung, Y.S.; Wong, J.; Chong, C.C.; Wong, J.S.; Lai, P.B. Randomized clinical trial of open hepatectomy with or without intermittent Pringle manoeuvre. Br. J. Surg. 2012, 99, 1203–1209. [Google Scholar] [CrossRef]
- Ferrero, A.; Russolillo, N.; Vigano, L.; Lo Tesoriere, R.; Muratore, A.; Capussotti, L. Does Pringle maneuver affect survival in patients with colorectal liver metastases? World J. Surg. 2010, 34, 2418–2425. [Google Scholar] [CrossRef] [PubMed]
- Nanji, S.; Mir, Z.M.; Karim, S.; Brennan, K.E.; Patel, S.V.; Merchant, S.J.; Booth, C.M. Perioperative blood transfusion and resection of colorectal cancer liver metastases: Outcomes in routine clinical practice. HPB 2021, 23, 404–412. [Google Scholar] [CrossRef]
- De Carlis, L.; Di Sandro, S.; Giacomoni, A.; Mihaylov, P.; Lauterio, A.; Mangoni, I.; Cusumano, C.; Poli, C.; Tripepi, M.; Bencardino, K. Colorectal liver metastases: Hepatic pedicle clamping during hepatectomy reduces the incidence of tumor recurrence in selected patients. Case-matched analysis. Eur. J. Surg. Oncol. 2013, 39, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Fong, Y.; Fortner, J.; Sun, R.L.; Brennan, M.F.; Blumgart, L.H. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: Analysis of 1001 consecutive cases. Ann. Surg. 1999, 230, 309–318, discussion 318–321. [Google Scholar] [CrossRef] [PubMed]
- Al-Saeedi, M.; Ghamarnejad, O.; Khajeh, E.; Shafiei, S.; Salehpour, R.; Golriz, M.; Mieth, M.; Weiss, K.H.; Longerich, T.; Hoffmann, K.; et al. Pringle Maneuver in Extended Liver Resection: A propensity score analysis. Sci. Rep. 2020, 10, 8847. [Google Scholar] [CrossRef]
- Tsang, M.E.; Karanicolas, P.J.; Habashi, R.; Cheng, E.; Hanna, S.S.; Coburn, N.G.; Law, C.H.; Hallet, J. The impact of portal pedicle clamping on survival from colorectal liver metastases in the contemporary era of liver resection: A matched cohort study. HPB 2015, 17, 796–803. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dona don, M.; Molinari, A.F.; Corazzi, F.; Rocchi, L.; Zito, P.; Cimino, M.; Costa, G.; Raimondi, F.; Torzilli, G. Pharmacological Modulation of Ischemic-Reperfusion Injury during Pringle Maneuver in Hepatic Surgery. A Prospective Randomized Pilot Study. World J. Surg. 2016, 40, 2202–2212. [Google Scholar] [CrossRef] [PubMed]

| Variables | Number (%) or Median (IQR) | Pringle Group | No-Pringle Group | p |
|---|---|---|---|---|
| Sex | 0.338 | |||
| male | 108 (60.3%) | 38 (63.3%) | 70 (58.8%) | |
| female | 71 (39.7%) | 22 (36.7%) | 49 (41.2%) | |
| Age (years) | 62 (56–70) | 64 (57–72) | 61 (55–69) | 0.129 |
| Liver resection | ||||
| right hemihepatectomy | 128 (71.5%) | 39 (65.0%) | 89 (74.8%) | |
| extended right hemihepatectomy | 20 (11.2%) | 8 (13.3%) | 12 (10.1%) | |
| right hemihepatectomy and non-anatomical resection | 31 (17.3%) | 13 (21.7%) | 18 (15.1%) | |
| Pringle maneuver | 60 (33.5%) | |||
| Pringle maneuver (median duration [min]) | 30 | |||
| Intraoperative blood transfusion (PRBCs units) | 0 (0–5) * | 0 (0–5) * | 0 (0–3) | 0.474 |
| Number of tumors | 2 (1–3) | 2 (1–4) | 2 (1–3) | 0.496 |
| Tumor Burden Score zone | 0.610 | |||
| Zone 1 | 6 (10.0%) | 14 (12.1%) | ||
| Zone 2 | 43 (71.7%) | 87 (75.0%) | ||
| Zone 3 | 11 (18.3%) | 15 (12.9%) | ||
| Diameter of the largest tumor (mm) | 45 (29–65) | 48.5 (30.0–67.0) | 41.0 (27.5–65.0) | 0.533 |
| Tumor Burden Score (quantitative) | 5.40 (4.03–7.39) | 6.08 (4.35–7.63) | 5.01 (3.88–7.28) | 0.132 |
| Preoperative laboratory results | ||||
| White Blood Cell (103/µL) | 6.30 (4.80–7.78) | 6.70 (5.30–9.04) | 6.03 (4.70–7.32) | 0.023 |
| Hemoglobin (g/dL) | 13.10 (11.70–14.00) | 13.40 (11.50–14.00) | 13.00 (11.90–14.00) | 0.658 |
| Platelets (103/µL) | 236 (184–292) | 268 (220–311) | 211 (176–262) | 0.001 |
| Aspartate aminotransferase (IU/L) | 30 (22–41) | 31 (20–47) | 30 (23–39) | 0.659 |
| Alanine aminotransferase (IU/L) | 25 (19–37) | 23 (20–51) | 25 (19–37) | 0.592 |
| Bilirubin (mg/dL) | 0.56 (0.37–0.78) | 0.47 (0.34–0.59) | 0.61 (0.41–0.90) | 0.001 |
| Albumin (g/dL) | 4.00 (3.70–4.20) | 4.00 (3.60–4.40) | 4.00 (3.70–4.15) | 0.464 |
| INR | 0.99 (0.96–1.04) | 1.01 (0.96–1.04) | 0.99 (0.95–1.04) | 0.836 |
| Creatinine (mg/dL) | 0.81 (0.71–0.94) | 0.81 (0.76–0.93) | 0.81 (0.68–0.94) | 0.345 |
| Carcinoembryonic antigen (ng/mL) | 10.80 (3.30–49.50) | 6.00 (2.00–19.00) | 12.66 (4.00–62.15) | 0.026 |
| Carbohydrate antigen 19-9 (ng/mL) | 20.00 (6.60–79.13) | 27.00 (5.80–136.10) | 15.60 (7.00–66.40) | 0.357 |
| Peak 3-day postoperative bilirubin (mg/dL) | 2.29 (1.61–3.20) | 2.71 (1.94–3.78) | 2.06 (1.43–2.91) | 0.002 |
| Peak 3-day postoperative ALT (U/L) | 334 (205–492) | 315 (190–492) | 343 (210–496) | 0.415 |
| Peak postoperative lactate (mmol/L) | 3.85 (2.60–5.60) | 4.70 (3.80–6.30) | 3.60 (2.60–5.30) | 0.113 |
| Pringle vs. No Pringle Maneuver | Covariate | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| 0.55 (0.36–0.86) | 0.009 | Number of tumors (per 1 tumor) | 1.08 (1.01–1.15) | 0.002 |
| 0.57 (0.37–0.88) | 0.001 | Sum of all tumor diameters (per 1 mm) | 1.01 (1.00–1.02) | <0.001 |
| 0.57 (0.36–0.90) | 0.002 | Hemoglobin (per 1 g/dL) | 0.83 (0.73–0.95) | 0.001 |
| 0.73 (0.43–1.26) | 0.265 | CEA (per 1 ln[ng/mL]) | 1.31 (1.00–1.28) | 0.049 |
| HR (95% CI) | p Value | |
|---|---|---|
| Patient sex (male vs. female) | 1.04 (0.70–1.53) | 0.857 |
| Age (per 1 year) | 1.01 (0.99–1.03) | 0.397 |
| Number of tumors (per 1 tumor) | 1.07 (1.00–1.15) | 0.044 |
| Sum of all tumor diameters (per 1 mm) | 1.01 (1.01–1.02) | <0.001 |
| Liver steatosis (yes vs. no) | 0.77 (0.51–1.16) | 0.209 |
| White Blood Cell (per 103/µL) | 1.01 (0.93–1.89) | 0.892 |
| Bilirubin (per 1 mg/dL) | 0.85 (0.59–1.23) | 0.384 |
| Hemoglobin (per 1 g/dL) | 0.84 (0.74–0.96) | 0.009 |
| CEA (per 1 ln[ng/mL]) | 1.14 (1.01–1.29) | 0.029 |
| Peak 3-day postoperative ALT (per 1 ln[U/L]) | 1.16 (0.86–1.56) | 0.327 |
| Peak 3-day postoperative bilirubin (per 1 mg/dL) | 1.02 (0.72–1.46) | 0.897 |
| Peak postoperative lactate (per 1 mmol/L) | 1.03 (0.93–1.15) | 0.542 |
| No Pringle maneuver | 1.71 (1.10–2.64) | 0.017 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krawczyk, P.; Morawski, M.; Krasnodębski, M.; Sieńko, D.; Grąt, M.; Kron, P.; Lodge, P. Long-Term Effects of Pedicle Clamping during Major Hepatectomy for Colorectal Liver Metastases. J. Clin. Med. 2021, 10, 2778. https://doi.org/10.3390/jcm10132778
Krawczyk P, Morawski M, Krasnodębski M, Sieńko D, Grąt M, Kron P, Lodge P. Long-Term Effects of Pedicle Clamping during Major Hepatectomy for Colorectal Liver Metastases. Journal of Clinical Medicine. 2021; 10(13):2778. https://doi.org/10.3390/jcm10132778
Chicago/Turabian StyleKrawczyk, Piotr, Marcin Morawski, Maciej Krasnodębski, Damian Sieńko, Michał Grąt, Philipp Kron, and Peter Lodge. 2021. "Long-Term Effects of Pedicle Clamping during Major Hepatectomy for Colorectal Liver Metastases" Journal of Clinical Medicine 10, no. 13: 2778. https://doi.org/10.3390/jcm10132778
APA StyleKrawczyk, P., Morawski, M., Krasnodębski, M., Sieńko, D., Grąt, M., Kron, P., & Lodge, P. (2021). Long-Term Effects of Pedicle Clamping during Major Hepatectomy for Colorectal Liver Metastases. Journal of Clinical Medicine, 10(13), 2778. https://doi.org/10.3390/jcm10132778






