Impact of Bundle Branch Block on Permanent Pacemaker Implantation after Transcatheter Aortic Valve Implantation: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Strategy
2.2. Eligibility Criteria and Studies Selection
2.3. Statistical Analysis
3. Results
3.1. Study Inclusion
3.2. Baseline Characteristics of Included Patients and Permanent Pacemaker Implantation Details
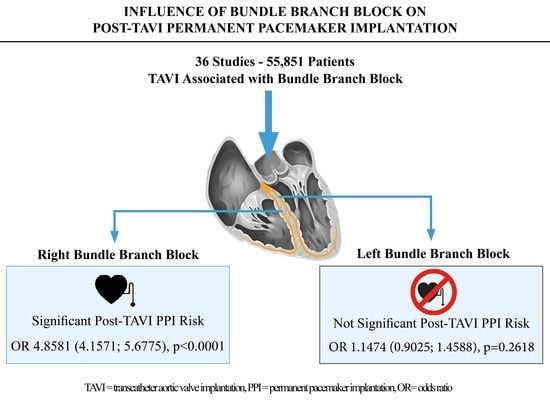
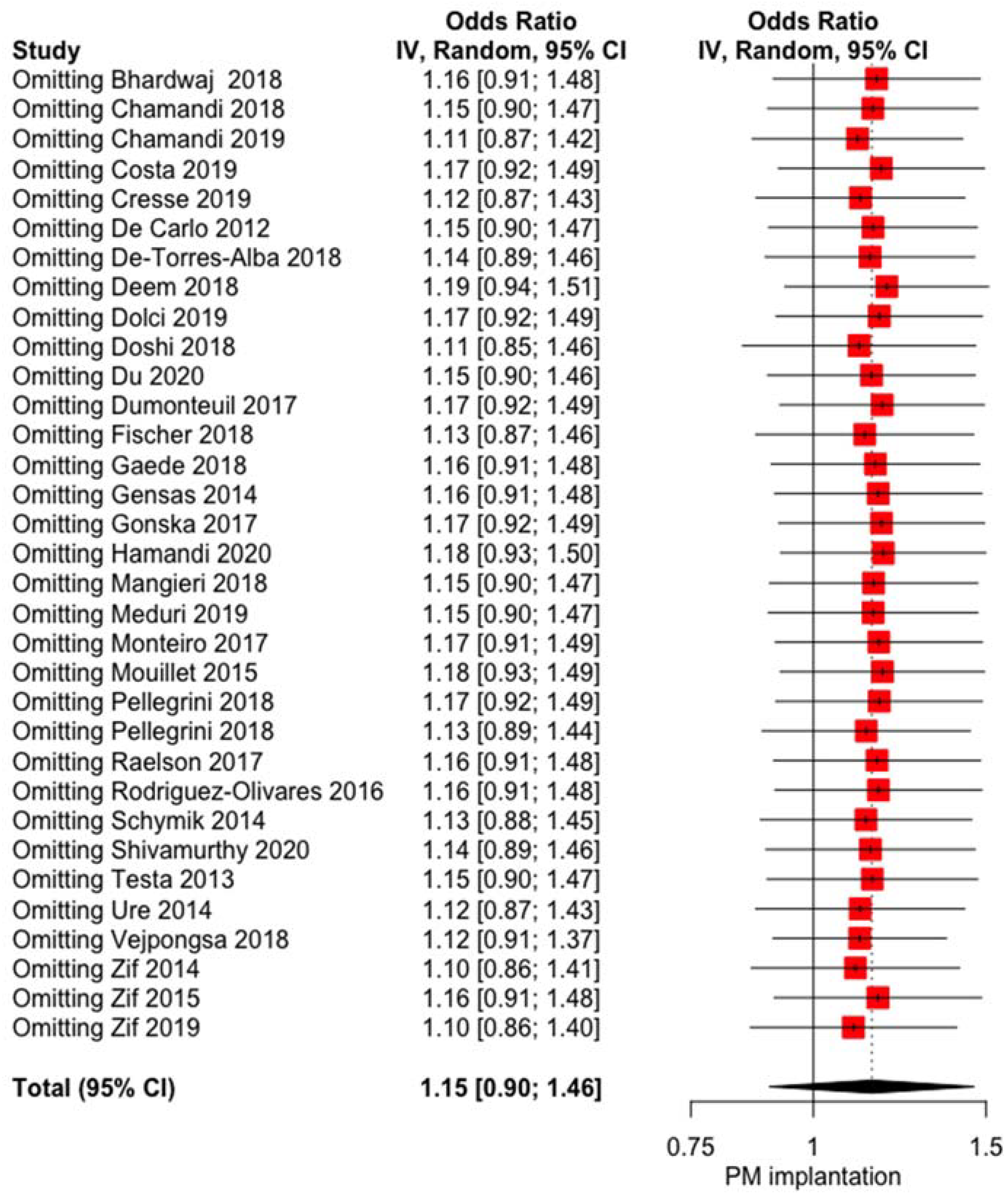
3.3. Influence of LBBB on PPI
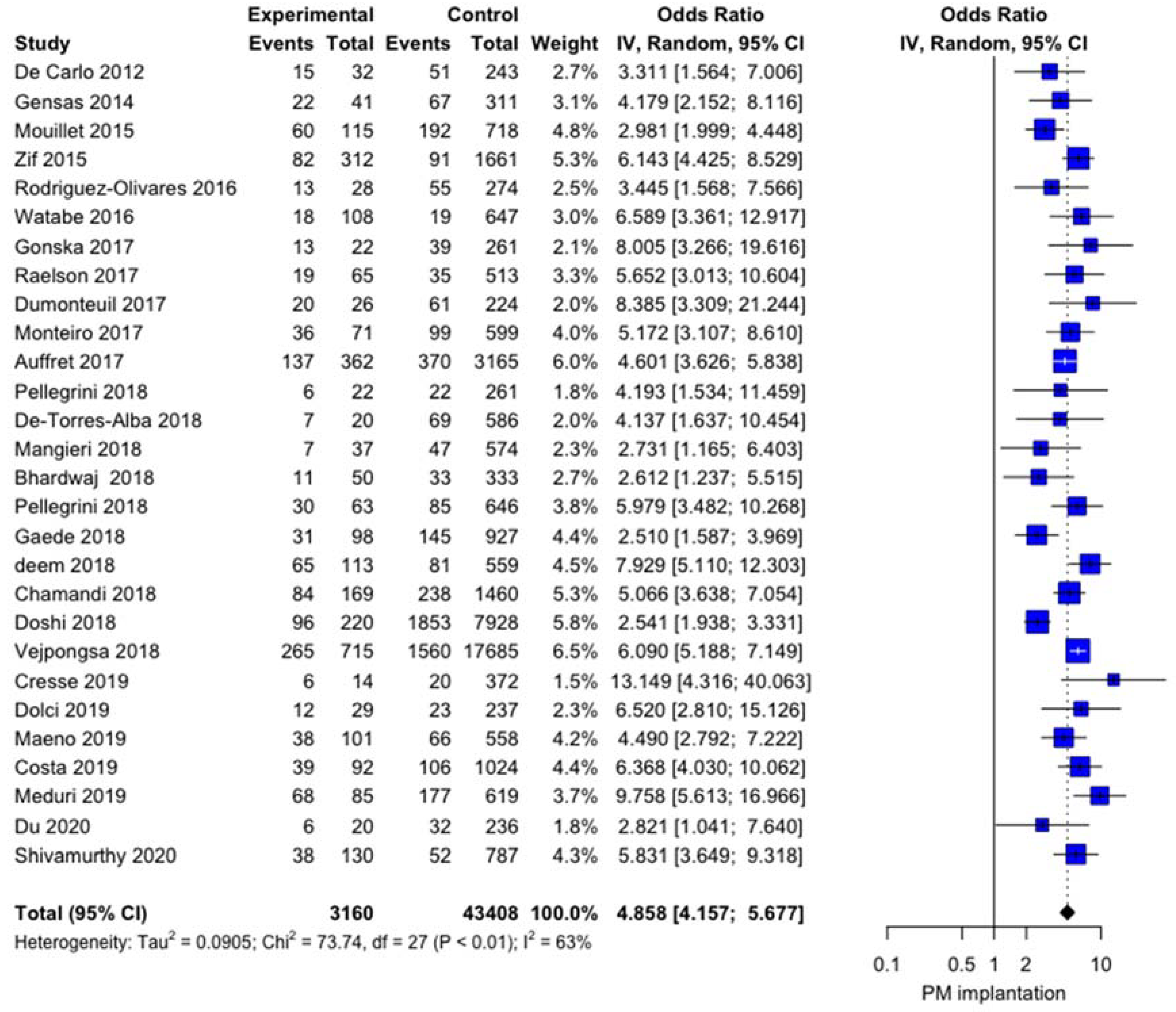
3.4. Influence of RBBB on PPI
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Erkapic, D.; De Rosa, S.; Kelava, A.; Lehmann, R.; Fichtlscherer, S.; Hohnloser, S.H. Risk for permanent pacemaker after transcatheter aortic valve implantation: A comprehensive analysis of the literature. J. Cardiovasc. Electrophysiol. 2012, 23, 391–397. [Google Scholar] [CrossRef]
- Siontis, G.C.; Jüni, P.; Pilgrim, T.; Stortecky, S.; Büllesfeld, L.; Meier, B.; Wenaweser, P.; Windecker, S. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: A meta-analysis. J. Am. Coll. Cardiol. 2014, 64, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Van Gils, L.; Tchetche, D.; Lhermusier, T.; Abawi, M.; Dumonteuil, N.; Rodriguez-Olivares, R.; Molina-Martin, D.N.J.; Stella, P.R.; Carrié, D.; De Jaegere, P.P.; et al. Transcatheter Heart Valve Selection and Permanent Pacemaker Implantation in Patients with Pre-Existent Right Bundle Branch Block. J. Am. Heart Assoc. 2017, 6, e005028. [Google Scholar] [CrossRef]
- Lopez-Aguilera, J.; Saint-Gerons, J.M.S.; Bellido, F.M.; Suarez, D.L.H.D.T.J.; Pineda, S.O.; Alvarez-Ossorio, M.P.; Angel, R.M.M.; Pavlovic, D.; Suarez, D.L.C.C.J. Effect of New-Onset Left Bundle Branch Block After Transcatheter Aortic Valve Implantation (CoreValve) on Mortality, Frequency of Re-Hospitalization, and Need for Pacemaker. Am. J. Cardiol. 2016, 118, 1380–1385. [Google Scholar] [CrossRef]
- Rodès-Cabau, J. Transcatheter aortic valve implantation: Current and future approaches. Nat. Rev. Cardiol. 2012, 9, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Waksman, R.; Rogers, T.; Torguson, R.; Gordon, P.; Ehsan, A.; Wilson, S.R.; Goncalves, J.; Levitt, R.; Hahn, C.; Parikh, P.; et al. Transcatheter Aortic Valve Replacement in Low-Risk Patients with Symptomatic Severe Aortic Stenosis. J. Am. Coll. Cardiol. 2018, 72, 2095–2105. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, A.; Rozenbaum, Z.; Halkin, A.; Banai, S.; Bazan, S.; Barbash, I.; Segev, A.; Fefer, P.; Maor, E.; Danenberg, H.; et al. Outcomes of Transcatheter Aortic Valve Implantation in Patients with Low Versus Intermediate to High Surgical Risk. Am. J. Cardiol. 2019, 123, 644–649. [Google Scholar] [CrossRef]
- Voigtländer, L.; Seiffert, M. Expanding TAVI to Low and Intermediate Risk Patients. Front. Cardiovasc. Med. 2018, 5, 92. [Google Scholar] [CrossRef] [PubMed]
- Regueiro, A.; Abdul-Jawad, A.O.; Del Trigo, M.; Campelo-Parada, F.; Puri, R.; Urena, M.; Philippon, F.; Rodès-Cabau, J. Impact of New-Onset Left Bundle Branch Block and Periprocedural Permanent Pacemaker Implantation on Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement: A systematic Review and Meta-Analysis. Circ. Cardiovasc. Interv. 2016, 9, e003635. [Google Scholar] [CrossRef] [PubMed]
- Croix, G.R.S.; Spencer, C.; Hrachian, H.L.; Beohar, N. Clinical Impact of Preexisting Right Bundle Branch Block after Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Analysis. J. Interv. Cardiol. 2020, 2020, 1789516. [Google Scholar]
- Massouillé, G.; Bordachar, P.; Ellenbogen, K.A.; Souteyrand, G.; Jean, F.; Combaret, N.; Vorilhon, C.; Clerfond, G.; Farhat, M.; Ritter, P.; et al. New-onset left bundle branch block induced by transcutaneous aortic valve implantation. Am. J. Cardiol. 2016, 117, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Rivard, L.; Schram, G.; Asgar, A.; Khairy, P.; Andrade, J.G.; Bonan, R.; Dubuc, M.; Guerra, P.G.; Ibrahim, R.; Macle, L.; et al. Electrocardiographic and electrophysiological predictors of atrioventricular block after transcatheter aortic valve replacement. Heart Rhythm. 2015, 12, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Warton, D.I.; Hui, F.K.C. The arcsine is asinine: The analysis of proportions in ecology. Ecology 2011, 92, 3–10. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials 2015, 45 Pt A, 139–145. [Google Scholar] [CrossRef]
- Bowden, J.; Tierney, J.F.; Copas, A.J.; Burdett, S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalized Q statistics. BMC Med. Res. Methodol. 2011, 11, 41–52. [Google Scholar] [CrossRef]
- Huedo-Medina, T.B.; Sanchez-Meca, J.; Marin-Martinez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Baujat, B.; Mahé, C.; Pignon, J.-P.; Hill, C. A graphical method for exploring heterogeneity in meta-analyses: Application to a meta-analysis of 65 trials. Stat. Med. 2002, 21, 2641–2652. [Google Scholar] [CrossRef] [PubMed]
- De Carlo, M.; Giannini, C.; Bedogni, F.; Klugmann, S.; Brambilla, N.; De Marco, F.; Zuchelli, G.; Testa, L.; Oreglia, J.; Petronio, A.S. Safety of a conservative strategy of permanent pacemaker implantation after transcatheter aortic CoreValve implantation. Am. Heart J. 2012, 163, 492–499. [Google Scholar] [CrossRef] [PubMed]
- Gensas, C.S.; Caixeta, A.; Siqueira, D.; Carvalho, L.A.; Sarmento-Leite, R.; Mangione, J.A.; Lemos, P.A.; Colafranceschi, A.S.; Caramori, P.; Ferreira, M.C.; et al. Brazilian Registry in Transcatheter Aortic Valve Implantation Investigators. Predictors of permanent pacemaker requirement after transcatheter aortic valve implantation: Insights from a Brazilian registry. Int. J. Cardiol. 2014, 175, 248–252. [Google Scholar] [CrossRef]
- Mouillet, G.; Lellouche, N.; Yamamoto, M.; Oguri, A.; Dubois-Rande, J.L.; Van Belle, E.; Gilard, M.; Laskar, M.; Teiger, E. Outcomes following pacemaker implantation after transcatheter aortic valve implantation with CoreValve (®) devices: Results from the FRANCE 2 Registry. Catheter. Cardiovasc. Interv. 2015, 86, E158–E166. [Google Scholar] [CrossRef] [PubMed]
- Nazif, T.M.; Dizon, J.M.; Hahn, R.T.; Xu, K.; Babaliaros, V.; Douglas, P.S.; El-Chami, M.F.; Herrmann, H.C.; Mack, M.; Makkar, R.R.; et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: The PARTNER (Placement of AoRtic TraNscathertER Valves) trial and registry. JACC Cardiovasc. Interv. 2015, 8 Pt A, 60–69. [Google Scholar] [CrossRef]
- Rodríguez-Olivaresa, R.; van Gils, L.; El Faquir, N.; Rahhab, Z.; Di Martino, L.F.M.; van Weenen, S.; de Vriesa, J.; Galema, T.W.; Geleijnse, M.L.; Budde, R.P.; et al. Importance of the left ventricular outflow tract in the need for pacemaker implantation after transcatheter aortic valve replacement. Int. J. Cardiol. 2016, 216, 9–15. [Google Scholar] [CrossRef]
- Gonska, B.; Seeger, J.; Keßler, M.; Von Keil, A.; Rottbauer, W.; Wöhrle, J. Predictors for permanent pacemaker implantation in patients undergoing transfemoral aortic valve implantation with the Edwards Sapien 3 valve. Clin. Res. Cardiol. 2017, 106, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Raelson, C.A.; Gabriels, J.; Ruan, J.; Ip, J.E.; Thomas, G.; Liu, C.F.; Cheung, J.W.; Lerman, B.B.; Patel, A.; Markowitz, S.M. Recovery of atrioventricular conduction in patients with heart block after transcatheter aortic valve replacement. J. Cardiovasc. Electrophysiol. 2017, 28, 1196–1202. [Google Scholar] [CrossRef]
- Dumonteil, N.; Meredith, I.T.; Blackman, D.J.; Tchétché, D.; Hildick-Smith, D.; Spence, M.S.; Walters, D.L.; Harnek, J.; Worthley, S.G.; Rioufol, G.; et al. Insights into the need for permanent pacemaker following implantation of the repositionable LOTUS valve for transcatheter aortic valve replacement in 250 patients: Results from the REPRISE II trial with extended cohort. Euro Interv. 2017, 13, 796–803. [Google Scholar] [CrossRef]
- Monteiro, C.; Di Leoni, F.A.; Caramori, P.R.; Carvalho, L.A.F.; Siqueira, D.A.; Sao, T.L.E.K.; Perin, M.; De Lima, V.C.; Guérios, E.; Brito, F.S.D., Jr.; et al. Permanent Pacing After Transcatheter Aortic Valve Implantation: Incidence, Predictors and Evolution of Left Ventricular Function. Arq. Bras. Cardiol. 2017, 109, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, C.; Kim, W.K.; Holzamer, A.; Walther, T.; Mayr, N.P.; Michel, J.; Rheude, T.; Nuñez, J.; Kasel, A.M.; Trenkwalder, T.; et al. Multicenter Evaluation of Prosthesis Oversizing of the SAPIEN 3 Transcatheter Heart Valve Impact on Device Failure and New Pacemaker Implantations. Rev. Esp. Cardiol. 2019, 72, 641–648. [Google Scholar] [CrossRef] [PubMed]
- De-Torres-Alba, F.; Kaleschke, G.; Vormbrock, J.; Orwat, S.; Radke, R.; Feurle, M.; Diller, G.P.; Reinecke, H.; Baumgartner, H. Delayed pacemaker requirement after transcatheter aortic valve implantation with a new-generation balloon expandable valve: Should we monitor longer? Int. J. Cardiol. 2018, 273, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Mangieri, A.; Lanzillo, G.; Bertoldi, L.; Jabbour, R.J.; Regazzoli, D.; Ancona, M.B.; Tanaka, A.; Mitomo, S.; Garducci, S.; Montalto, C.; et al. Predictors of Advanced Conduction Disturbances Requiring a Late (≥48 h) Permanent Pacemaker Following Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 1519–1526. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Ramanan, T.; Sawant, A.C.; Sinibaldi, E.; Pham, M.; Khan, S.; Qureshi, R.; Agrawal, N.; Khalil, C.; Hansen, R.; et al. Quality of life outcomes in transcatheter aortic valve replacement patients requiring pacemaker implantation. J. Arrhythm. 2018, 34, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, C.; Husser, O.; Kim, W.K.; Holzamer, A.; Walther, T.; Rheude, T.; Mayr, N.P.; Trenkwalder, T.; Joner, M.; Michel, J.; et al. Predictors of Need for Permanent Pacemaker Implantation and Conduction Abnormalities With a Novel Self-expanding Transcatheter Heart Valve. Rev. Esp. Cardiol. 2019, 72, 145–153. [Google Scholar] [CrossRef]
- Gaede, L.; Kim, W.K.; Liebetrau, C.; Dörr, O.; Sperzel, J.; Blumenstein, J.; Berkowitsch, A.; Walther, T.; Hamm, C.; Elsässer, A.; et al. Pacemaker implantation after TAVI: Predictors of AV block persistence. Clin. Res. Cardiol. 2018, 107, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Nadeem, F.; Tsushima, T.; Ladas, T.P.; Thomas, R.B.; Patel, S.M.; Saric, P.; Patel, T.; Lipinski, J.; Li, J.; Costa, M.A.; et al. Impact of Right Ventricular Pacing in Patients Who Underwent Implantation of Permanent Pacemaker After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2018, 122, 1712–1717. [Google Scholar] [CrossRef] [PubMed]
- Chamandi, C.; Barbanti, M.; Munoz-Garcia, A.; Latib, A.; Nombela-Franco, L.; Gutiérrez-Ibanez, E.; Veiga-Fernandez, G.; Cheema, A.N.; Cruz-Gonzalez, I.; Serra, V.; et al. Long-Term Outcomes in Patients with New Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Doshi, R.; Decter, D.H.; Meraj, P. Incidence of arrhythmias and impact of permanent pacemaker implantation in hospitalizations with transcatheter aortic valve replacement. Clin. Cardiol. 2018, 41, 640–645. [Google Scholar] [CrossRef]
- Vejpongsa, P.; Zhang, X.; Bhise, V.; Kitkungvan, D.; Shivamurthy, P.; Anderson, H.V.; Balan, P.; Nguyen, T.C.; Estrera, A.L.; Dougherty, A.H.; et al. Risk Prediction Model for Permanent Pacemaker Implantation after Transcatheter Aortic Valve Replacement. Struct. Heart 2018, 2, 328–335. [Google Scholar] [CrossRef]
- Cresse, S.; Eisenberg, T.; Alfonso, C.; Cohen, M.G.; DeMarchena, E.; Williams, D.; Carrillo, R. Cardiac conduction abnormalities associated with pacemaker implantation after transcatheter aortic valve replacement. Pacing Clin. Electrophysiol. 2019, 42, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Dolci, G.; Vollema, E.M.; Van Der Kley, F.; De Weger, A.; Marsa, N.A.; Delgado, V.; Bax, J.J. One-Year Follow-Up of Conduction Abdormalities After Transcatheter Aortic Valve Implantation with the SAPIEN 3 Valve. Am. J. Cardiol. 2019, 124, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Costa, G.; Zappulla, P.; Barbanti, M.; Cirasa, A.; Todaro, D.; Rapisarda, G.; Picci, A.; Platania, F.; Tosto, A.; Di Grazia, A.; et al. Pacemaker dependency after transcatheter aortic valve implantation: Incidence, predictors and long-term outcomes. EuroIntervention 2019, 15, 875–883. [Google Scholar] [CrossRef]
- Meduri, C.U.; Kereiakes, D.J.; Rajagopal, V.; Makkar, R.R.; O’Hair, D.; Linke, A.; Waksman, R.; Babliaros, V.; Stoler, R.C.; Mishkel, G.J.; et al. Pacemaker Implantation and Dependency After Transcatheter Aortic Valve Replacement in the REPRISE III Trial. J. Am. Heart Assoc. 2019, 8, e012594. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Zhu, Q.; Jiang, J.; Chen, H.; Liu, X.; Wang, J. Incidence and Predictors of Permanent Pacemaker Implantation in Patients Who Underwent Transcatheter Aortic Valve Replacement: Observation of a Chinese Population. Cardioliology 2019, 145, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Shivamurthy, P.; Vejpongsa, P.; Gurung, S.; Jacob, R.; Zhao, Y.; Anderson, H.V.; Balan, P.; Nguyen, T.C.; Estrera, A.L.; Dougherty, A.H.; et al. Validation of Scoring System Predicting Permanent Pacemaker Implantation after Transcatheter Aortic Valve Replacement. Pacing Clin. Electrophysiol. 2020, 43, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Kozuma, K.; Hioki, H.; Kawashima, H.; Nara, Y.; Kataoka, A.; Nagura, F.; Nakashima, M.; Shirai, S.; Tada, N.; et al. Pre-Existing Right Bundle Branch Block Increases Risk for Death After Transcatheter Aortic Valve Replacement with a Balloon-Expandable Valve. JACC Cardiovasc. Interv. 2016, 9, 2210–2216. [Google Scholar] [CrossRef] [PubMed]
- Auffret, V.; Webb, J.G.; Eltchaninoff, H.; Munoz-Garcia, A.J.; Himbert, D.; Tamburino, C.; Nombela-Franco, L.; Nietlispach, F.; Moris, C.; Ruel, M.; et al. Clinical Impact of Baseline Right Bundle Branch Block in Patients Undergoing Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2017, 10, 1564–1574. [Google Scholar] [CrossRef]
- Maeno, Y.; Abramowitz, Y.; Israr, S.; Yoon, S.-H.; Kubo, S.; Nomura, T.; Miyasaka, H.; Kawamori, H.; Kazuno, Y.; Takahashi, N.; et al. Prognostic impact of Permanent Pacemaker Implantation in Patients with Low Left Ventricular Ejection Fraction Following Transcatheter Aortic Valve Replacement. J. Invasive Cardiol. 2019, 31, E15–E22. [Google Scholar]
- Testa, L.; Latib, A.; De Marco, F.; De Carlo, M.; Agnifili, M.; Latino, R.A.; Petronio, A.S.; Ettori, F.; Poli, A.; De Servi, S.; et al. Clinical Impact of persistent left bundle-branch block after transcatheter aortic valve implantation with CoreValve Revalving System. Circulation 2013, 127, 1300–1307. [Google Scholar] [CrossRef] [PubMed]
- Schymik, G.; Tzamalis, P.; Bramlage, P.; Heimeshoff, M.; Würth, A.; Wondraschek, R.; Gonska, B.-D.; Posival, H.; Schmitt, C.; Schröfel, H.; et al. Clinical impact of a new left bundle branch block following TAVI implantation: 1-year results of the TAVIK cohort. Clin. Res. Cardiol. 2014, 104, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Urena, M.; Webb, J.G.; Cheema, A.; Serra, V.; Toggweiler, S.; Barbanti, M.; Cheung, A.; Ye, J.; Dumont, E.; DeLarochellière, R.; et al. Impact of New-Onset Persistent Left Bundle Branch Block on Late Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Implantation with a Balloon-Expandable Valve. JACC Cardiovasc. Interv. 2014, 7, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Nazif, T.M.; Williams, M.R.; Hahn, R.T.; Kapadia, S.; Babaliaros, V.; Rodés-Cabau, J.; Szeto, W.Y.; Jilaihawi, H.; Fearon, W.F.; Dvir, D.; et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: Analysis of the PARTNER experience. Eur. Heart J. 2014, 35, 1599–1607. [Google Scholar] [CrossRef] [PubMed]
- Fischer, Q.; Himbert, D.; Webb, J.G.; Eltchaninoff, H.; Munoz-Garcia, A.J.; Tamburino, C.; Nombela-Franco, L.; Nietlispach, F.; Moris, C.; Ruel, M.; et al. Impact of Preexisting Left Bundle Branch Block in Transcatheter Aortic Valve Replacement Recipients. Circ. Cardiovasc. Interv. 2018, 11, e006927. [Google Scholar] [CrossRef] [PubMed]
- Chamandi, C.; Barbanti, M.; Munoz-Garcia, A.; Latib, A.; Nombela-Franco, L.; Guttiérrez-Ibanez, E.; Veiga-Fernandez, G.; Cheema, A.N.; Cruz-Gonzales, I.; Serra, V.; et al. Long-term Outcomes in Patients with New-Onset Persistent Left Bundle Branch Block Following TAVR. JACC Cardiovasc. Interv. 2019, 12, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- Nazif, T.M.; Chen, S.; George, I.; Dizon, J.M.; Hahn, R.T.; Crowley, A.; Alu, M.C.; Babaliaros, V.; Thourani, V.H.; Herrmann, H.C.; et al. New-onset left bundle branch block after transcatheter aortic valve replacement is associated with adverse long-term clinical outcomes in intermediate-risk patients: An analysis from the PARTNER II trial. Eur. Heart J. 2019, 40, 2218–2227. [Google Scholar] [CrossRef] [PubMed]
- Hamandi, M.; Tabachnick, D.; Lanfear, A.T.; Baxter, R.; Shin, K.; Zingler, B.; Mack, M.J.; DiMaio, J.M.; Kindsvater, S. Effect of new and persistent left bundle branch block after transcatheter aortic valve replacement on long-term need for pacemaker implantation. Bayl. Univ. Med. Cent. Proc. 2020, 33, 157–162. [Google Scholar] [CrossRef]
- Urena, M.; Webb, J.G.; Eltchaninoff, H.; Munoz-Garcia, A.J.; Bouleti, C.; Tamburino, C.; Nombela-Franco, L.; Nietlispach, F.; Moris, C.; Ruel, M.; et al. Late cardiac death in patients undergoing transcatheter aortic valve replacement: Incidence and predictors of advanced heart failure and sudden cardiac death. J. Am. Coll. Cardiol. 2015, 65, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Erkapic, D.; Kim, W.-K.; Weber, M.; Möllmann, H.; Berkowitsch, A.; Zaltsberg, S.; Pajitnev, D.J.; Rixe, J.; Neumann, T.; Kuniss, M.; et al. Electrocardiographic and further predictors for permanent pacemaker requirement after transcatheter aortic valve implantation. Europace 2010, 12, 1188–1190. [Google Scholar] [CrossRef] [PubMed]
- Van der Boon, R.M.; Nuis, R.J.; Van Mieghem, N.M.; Jordaens, L.; Rodès-Cabau, J.; Van Domburg, R.T.; Seruys, P.W.; Anderson, R.H.; De Jaegere, P.P.T. New conduction abnormalities after TAVI-frequency and causes. Nat. Rev. Cardiol. 2012, 9, 454–463. [Google Scholar] [CrossRef]
- Sasaki, K.; Izumo, M.; Kuwata, S.; Ishibashi, Y.; Kamijima, R.; Watanabe, M.; Kaihara, T.; Okuyama, K.; Koga, M.; Nishikawa, H.; et al. Clinical Impact of New-Onset Left Bundle-Branch Block After Transcatheter Aortic Valve Implantation in the Japanese Population. Circ. J. 2020, 84, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Keßler, M.; Gonska, B.; Seeger, J.; Rottbauer, W.; Wöhrle, J. Long-term clinical outcome of persistent left bundle branch block after transfemoral aortic valve implantation. Catheter. Cardiovasc. Interv. 2018, 93, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Muntané-Carol, G.; Guimaraes, L.; Ferreira-Neto, A.N.; Wintzer-Wehekind, J.; Junquera, L.; Del Val, D.; Faroux, L.; Philippon, F.; Rodés-Cabau, J. How does new-onset left bundle branch block affect the outcomes of transcatheter aortic valve repair? Expert Rev. Med. Devices 2019, 16, 589–602. [Google Scholar] [CrossRef]
- Franzoni, I.; Latib, A.; Maisano, F.; Costopoulos, C.; Testa, L.; Figini, F.; Giannini, F.; Basavarajaiah, S.; Mussardo, M.; Slavich, M.; et al. Comparison of Incidence and Predictors of Left Bundle Branch Block After Transcatheter Aortic Valve Implantation Using the CoreValve Versus the Edwards Valve. Am. J. Cardiol. 2013, 112, 554–559. [Google Scholar] [CrossRef]
- Urena, M.; Mok, M.; Serra, V.; Dumont, E.; Nombela-Franco, L.; DeLarochellière, R.; Doyle, D.; Igual, A.; Larose, E.; Amat-Santos, I.; et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon expandable valve. J. Am. Coll. Cardiol. 2012, 60, 1743–1752. [Google Scholar] [CrossRef]
- Vernooy, K.; Verbeek, X.A.; Peschar, M.; Crijns, H.J.G.M.; Arts, T.; Cornelussen, R.N.M.; Prinzen, F.W. Left bundle branch block induces ventricular remodeling and functional septal hypoperfusion. Eur. Heart J. 2005, 26, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Shoar, S.; Batra, S.; Gulraiz, I.W.; Javed, M.; Hosseini, F.; Naderan, M.; Shoar, N.; John, J.; Modukuru, V.R.; Sharma, S.K. Effect of pre-existing left bundle branch block on post-procedural outcomes of transcatheter aortic valve replacement: A meta-analysis of comparative studies. Am. J. Cardiovasc. Dis. 2020, 10, 294–300. [Google Scholar] [PubMed]
- Egger, F.; Nürnberg, M.; Rohla, M.; Weiss, T.W.; Unger, G.; Smetana, P.; Geppert, A.; Gruber, S.C.; Bambazek, A.; Falkensammer, J.; et al. High-degree atrioventricular block in patients with preexisting bundle branch block or bundle branch block occurring during transcatheter aortic valve implantation. Heart Rhythm. 2014, 11, 2176–2182. [Google Scholar] [CrossRef] [PubMed]
- Waksman, R.; Khan, J.M. Left Bundle Branch Block After TAVR. Buddle or Trouble? JACC Cardiovasc. Interv. 2019, 12, 1185–1187. [Google Scholar] [CrossRef] [PubMed]
- Husser, O.; Pellegrini, C.; Kim, W.-K.; Holzamer, A.; Pilgrim, T.; Toggweiler, S.; Schäfer, U.; Blumenstein, J.; Deuschl, F.; Rheude, T.; et al. Transcatheter Valve SELECTion in Patients with Right Bundle Branch Block and Impact on Pacemaker Implantation. J. Am. Coll. Cardiol. Interv. 2019, 12, 1781–1793. [Google Scholar] [CrossRef] [PubMed]
- Kumpuris, A.G.; Casale, T.B.; Mokotoff, D.M.; Miller, R.R.; Luchi, R.J. Right bundle-branch block. Occurrence following nonpenetrating chest trauma without evidence of cardiac contusion. JAMA 1979, 242, 172–173. [Google Scholar] [CrossRef] [PubMed]
- Kusumoto, F.M.; Schoenfeld, M.H.; Barrett, C.; Edgerton, J.R.; Ellenbogen, K.A.; Gold, M.R.; Goldschlager, N.F.; Hamilton, R.M.; Joglar, J.A.; Kim, R.J.; et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2019, 140, e382–e482. [Google Scholar] [PubMed]
- Brignole, M.; Auricchio, A.; Baron-Esquivias, G.; Bordachar, P.; Boriani, G.; Breithardt, O.-A.; Cleland, J.; Deharo, J.-C.; Delgado, V.; Elliott, P.M.; et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2013, 34, 2281–2329. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Knecht, S.; Schaer, B.; Reichlin, T.; Spies, F.; Madaffari, A.; Vischer, A.; Fahrni, G.; Jeger, R.; Kaiser, C.; Osswald, S.; et al. Electrophysiology Testing to Stratify Patients with Left Bundle Branch Block After Transcatheter Aortic Valve Implantation. J. Am. Heart Assoc. 2020, 9, e014446. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, A.; Tzou, W.; Ream, K.; Valle, J.; Tompkins, C.; Nguyen, D.T.; Sauer, J.D.; Messenger, J.; Aleong, R.G. Heart Block After Discharge in Patients Undergoing TAVR with Latest-Generation Valves. J. Am. Coll. Cardiol. 2018, 71, 577–578. [Google Scholar] [CrossRef] [PubMed]


| Study | Year | Study Design (Nr Centers) | Sample Size | Age (Years) | STS-Score (%) | Inclusion Period | Valve Type | Follow-Up (Months) * | Approach for TAVI | Mortality at 30 Days |
|---|---|---|---|---|---|---|---|---|---|---|
| De Carlo et al. [19] | 2012 | Retrospective (3) | 275 | 82.4 | na | Sep 2007–Jul 20120 | 100% MCV | 12 | na | 3% |
| Gensas et al. [20] | 2014 | Retrospective (18) | 353 | 82 | 14.4 | Jan 2008–Feb 2012 | 85.8% SE 14.2% BE | 60 | na | na |
| Mouillet et al. [21] | 2015 | Retrospective (29) | 833 | 82 | 14.1 | Jan 2010–Oct 2011 | 100% SE | 8 | na | 9.3% |
| Nazif et al. [22] | 2015 | Retrospective (21) | 1973 | 84.5 | 11.4 | May 2007–Sept 2011 | 100% BE | 12 | na | 6.6% |
| Rodriguez-Olivares et al. [23] | 2016 | Retrospective (1) | 302 | 81 | na | Nov 2005–Jan 2015 | 67.2% SE 21.2% BE 11.6% ME | na | na | na |
| Gonska et al. [24] | 2017 | Retrospective (1) | 283 | 79.9 | 6.7 | na | 100% ES3 | na | na | na |
| Raelson et al. [25] | 2017 | Retrospective (1) | 578 | 85,5 | Na | Mar 2009–Dec 2014 | 21% SE 79% BE | 1 | na | na |
| Dumonteil et al. [26] | 2017 | Retrospective (14) | 250 | 84 | 6,3 | Oct 2012–May 2014 | 100% ME | 12 | 100% TF | 4% |
| Monteiro et al. [27] | 2017 | Retrospective (22) | 670 | 81.8 | 10.7 | Jan 2008–Jan 2015 | 74% MCV 26% ES | na | 96% TF 4% others | na |
| Pellegrini et al. [28] | 2018 | Retrospective (3) | 283 | 80.8 | 6 | Jan 2014–Jan 2016 | 100% SE | 12 | 100% TF | na |
| De-Torres-Alba et al. [29] | 2018 | Retrospective (1) | 606 | 81.6 | na | Jan 2014–Jan 2017 | 100% BE | na | na | na |
| Mangieri et al. [30] | 2018 | Retrospective (1) | 611 | 84.4 | 6.9 | Oct 2007–Jul 2015 | 51.7% BE 33.7% SE | 12 | na | na |
| Bhardwaj et al. [31] | 2018 | Retrospective (1) | 383 | 83 | 9 | Jan 2012–July 2016 | 82% BE 18% SE | 9 | 84% TF | na |
| Pellegrini et al. [32] | 2018 | Retrospective (3) | 709 | 81 | na | Jan 2014–Jan 2016 | 100% BE | na | 100% TF | 1.6% |
| Gaede et al. [33] | 2018 | Retrospective (1) | 1025 | 81.9 | na | 2010–2015 | na | 2.4 | na | na |
| Nadeem et al. [34] | 2018 | Retrospective (1) | 672 | 81.4 | 7.4 | 2011–2017 | na | 12 | na | na |
| Chamandi et al. [35] | 2018 | Prospective (9) | 1629 | 81.5 | 10.9 | May 2009–Feb 2015 | 50.3% BE 49.7% SE | 48 | na | 42.3% |
| Doshi et al. [36] | 2018 | Retrospective (na) | 8148 | 82.5 | na | Jan 2012–Dec 2014 | na | na | na | na |
| Vejpongsa et al. [37] | 2018 | Retrospective (na) | 18,400 | 81.2 | na | Jan 2012–Dec 2013 | na | na | TF 75.5% 24.5% TA | na |
| Cresse et al. [38] | 2019 | Retrospective (1) | 386 | 83 | na | Apr 2008–Jun 2017 | na | na | na | na |
| Dolci et al. [39] | 2019 | Retrospective (1) | 266 | 80 | na | Feb 2014–Feb 2018 | 100% BE | 12 | 84% TF 16% TA | na |
| Costa et al. [40] | 2019 | Prospective (1) | 1116 | 82 | 4.4 | June 2007–Feb 2018 | 61.8% SE 27.2% BE 0.5% ME 10.5% Others | 72 | 97% TF 3% others | 3.9% |
| Meduri et al. [41] | 2019 | Prospective (1) | 704 | 82.5 | 6.6 | na | 34% SE 66% ME | 12 | na | na |
| Du et al. [42] | 2020 | Retrospective (1) | 256 | 76.5 | 7.1 | Mar 2013–Oct 2018 | na | 12 | Na | 3.3% |
| Shivamurthy et al. [43] | 2020 | Retrospective (1) | 917 | 80 | na | Nov 2011–Feb 2017 | na | na | 89.7% TF 10.3% TA | na |
| Studies reporting only on RBBB status in pacemaker population (n = 3) | ||||||||||
| Watanabe et al. [44] | 2016 | Prospective (9) | 749 | 85 | 6.9 | Oct 2013–Aug 2015 | 100% BE | 16.4 | 78.5% TF 18.8% TA 2.7% T iliac | 4% |
| Auffret et al. [45] | 2017 | Retrospective (na) | 3527 | 82 | na | na | 55.8% BE 44.2% SE | 23 | 79.6% TF 16.4% TA 1.9% T aortic 2.1% TS | 7.2% |
| Maeno et al. [46] | 2019 | Retrospective (1) | 659 | 83 | na | Jan 2013–Dec 2015 | 85% BE 15% SE | 19.1 | na | 2.6% |
| Studies reporting only on LBBB status in pacemaker population (n = 8) | ||||||||||
| Testa et al. [47] | 2013 | Retrospective (na) | 818 | 82 | na | Oct 2007–Apr 2011 | 100% SE | 9 | 88.6% TF 11.4% TS | 5.5% |
| Schymik et al. [48] | 2014 | Retrospective (1) | 624 | 82 | na | May 2008–Apr 2012 | 80.8% BE 19.2% SE | 12 | na | na |
| Urena et al. [49] | 2014 | Retrospective (4) | 668 | 79.5 | na | na | 100% BE | 13 | 2.8% TAortic 42.9% TA 54.3% TF | na |
| Nazif et al. [50] | 2014 | Retrospective (21) | 1151 | 84 | 11.2 | Mar 2007–Mar 2009 | 100% BE | 12 | 57% TF 43% TA | 3.6% |
| Fischer et al. [51] | 2018 | Prospective (18) | 3404 | 81.5 | 5.9 | Feb 2005–Oct 2017 | 46% SE 54% BE | 22 | 82.2% TF 2.2% TS 14.2% TA 1.4% T aortic | 5.7% |
| Chamandi et al. [52] | 2019 | Retrospective (9) | 1020 | 80.5 | 6.6 | May 2007–Feb 2015 | 48% BE 52% SE | 36 | 84% TF 11% TA 2% Taortic 3% TS | na |
| Nazif et al. [53] | 2019 | Retrospective (51) | 1179 | 81.2 | 5.5 | Dec 2011–Nov 2013 | 100% BE | 24 | 83.5% TF 16.5% Tthoracic | 1.3% |
| Hamandi et al. [54] | 2020 | Retrospective (1) | 424 | 82 | 7.6 | Jan 2012–Mar 2016 | 87% SE 13% BE | 12 | 85% TF 13% TA 3% TAortic | 1.3% |
| Studies Reporting on RBBB and LBBB Status in Pacemaker Population (n = 25) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| De Carlo et al. [19] | 70% AVB 3% SSS 27% others | 4 | 24% | 32 | 37 | 15 | 9 | * lower MCV implantation below aortic annulus * RBBB * left anterior hemiblock * longer PR interval | na |
| Gensas et al. [20] | na | na | 25.2% | 41 | 50 | 22 | 10 | * pre-existing RBBB * balloon pre-dilatation * CoreValve use | na |
| Mouillet et al. [21] | na | na | 30.3% | 115 | 106 | 60 | 24 | na | na |
| Nazif et al. [22] | 79% AVB 17.3% SSS | 3 | 8.8% | 312 | 174 | 82 | 12 | * Pre-existing RBBB * Prosthesis to LV outflow tract diameter ratio * LV-end diastolic diameter | * longer duration of hospitalization * higher rates of repeat hospitalization and mortality or repeat hospitalization at 1 year |
| Rodriguez-Olivares et al. [23] | na | na | 22.5% | 28 | 32 | 13 | 5 | na | *more LVOT oversizing associated with higher PPI |
| Gonska et al. [24] | 94.2% AVB 3.8% B 2% others | 4,3 | 18.4% | 22 | 74 | 13 | 6 | * baseline AV1B * preprocedural complete RBBB | na |
| Raelson et al. [25] | 82% AVB | 3 | 9% | 65 | 50 | 19 | 3 | na | na |
| Dumonteil et al. [26] | 88.9% AVB 5.9% others | 3 | 32% | 26 | 145 | 20 | 14 | * baseline RBBB * LV outflow tract overstretch >10% | * trend lower PPI rate at 30 days with shallower (<=5mm) implant depth |
| Monteiro et al. [27] | na | na | 20.1% | 71 | 93 | 36 | 15 | * previous RBBB * mean aortic gradient >50mmHg * MCV | na |
| Pellegrini et al. [28] | 71.5% AVB 3.5% SSS 25% B | na | 10% | 22 | 25 | 6 | 4 | * higher EuroSCORE | na |
| De-Torres-Alba et al. [29] | 96% AVB 1.4% B 2.6% others | na | 12.5% | 20 | 74 | 7 | 11 | na | na |
| Mangieri et al. [30] | 84% AVB 8.4% B | 0,3 | 8.8% | 37 | 61 | 7 | 5 | na | na |
| Bhardwaj et al. [31] | na | na | 11.5% | 50 | 39 | 11 | 3 | * PPI with short-term reduction in QoL without long-term implications | na |
| Pellegrini et al. [32] | 71.3% AVB 5.2% SSS 23.5% B | na | 16.2% | 63 | 41 | 30 | 4 | * increase in prosthesis oversizing | na |
| Gaede et al. [33] | 90% AVB 8% SSS 2% B | 4 | 14.7% | 98 | 107 | 31 | 17 | * pre-existing RBBB * CoreValve prosthesis | Predictors of lack of recovery of AVB * prior RBBB * higher mean aortic valve gradient * post-dilatation of the prosthesis |
| Nadeem et al. [34] | na | na | 21.7% | 113 | 51 | 65 | 4 | na | * PPI more likely to have heart failure admissions * PPI trend toward increased mortality |
| Chamandi et al. [35] | 76.7% AVB 5.6% SSS 3.1% B 14.6% others | 2 | 19.8% | 169 | 179 | 84 | 37 | na | * PPI higher rates of rehospitalization due to heart failure and combined endpoint of mortality or heart failure rehospitalization * PPI lesser improvement in LVEF over time, particularly in patients with reduced LVEF before TAVI |
| Doshi et al. [36] | na | na | 24% | 220 | 724 | 96 | 253 | * female sex * AF * LBBB * AVB | na |
| Vejpongsa et al. [37] | na | 2 | 9.9% | 715 | 1670 | 265 | 390 | na | na |
| Cresse et al. [38] | na | 4 | 6.7% | 14 | 97 | 6 | 12 | na | * RBBB, LBBB, △PR >40 ms associated with PPI |
| Dolci et al. [39] | 80%AVB 11% B 9% others | 4 | 13% | 29 | 41 | 12 | 3 | * baseline RBBB * QRS width immediately after TAVI | na |
| Costa et al. [40] | 84.8% AVB 4.1%SSS 11% Others | na | 13% | 92 | 99 | 39 | 8 | na | * PPI associated with increased 6 years mortality * baseline RBBB higher chance of being dependent at follow-up |
| Meduri et al. [41] | 90% AVB 6% B 4% others | 2 | 28.4% | 85 | 56 | 68 | 20 | * baseline RBBB * mean depth of valve implantation | * medically-treated diabetes mellitus in LOTUS valve patients |
| Du et al. [42] | 89.5% AVB | 8.7 | 14.8% | 20 | 19 | 6 | 3 | na | na |
| Shivamurthy et al. [43] | na | na | 9.8% | 130 | 79 | 38 | 9 | na | na |
| Studies reporting only on RBBB status in pacemaker population (n = 3) | |||||||||
| Watanabe et al. [44] | na | na | 4.9% | 108 | na | 18 | na | na | na |
| Auffret et al. [45] | na | na | 16.5% | 362 | na | 137 | na | na | na |
| Maeno et al. [46] | 77.9% AVB 11.5% SSS 10.6% | na | 15.8% | 101 | na | 38 | na | na | na |
| Studies reporting only on LBBB status in pacemaker population (n = 8) | |||||||||
| Testa et al. [47] | na | na | 17.4% | na | 224 | na | 41 | na | * LBBB associated with higher short-term PPI |
| Schymik et al. [48] | na | na | 10.8% | na | 197 | na | 28 | * chronic AF * baseline RBBB * MCV | na |
| Urena et al. [49] | 55.5% AVB SSS 20.7% 24.1% B | 365 | 4.3% | na | 128 | na | 11 | na | na |
| Nazif et al. [50] | na | na | 5.1% | na | 121 | na | 12 | na | * LBBB with higher PPI and failure of LVEF |
| Fischer et al. [51] | na | na | 15.5% | na | 398 | na | 84 | * pre-existing LBBB increase risk of death but not late PPI | * pre-existing LBBB associated with lower pre-operative LVEF |
| Chamandi et al. [52] | na | na | 7.2% | na | 212 | na | 29 | na | na |
| Nazif et al. [53] | na | na | 4.8% | na | 179 | na | 9 | na | * LBBB associated with PPI and repeat hospitalizations |
| Hamandi et al. [54] | na | na | 18% | na | 52 | na | 6 | na | na |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ravaux, J.M.; Mauro, M.D.; Vernooy, K.; Mariani, S.; Ronco, D.; Simons, J.; Van't Hof, A.W.; Veenstra, L.; Kats, S.; Maessen, J.G.; et al. Impact of Bundle Branch Block on Permanent Pacemaker Implantation after Transcatheter Aortic Valve Implantation: A Meta-Analysis. J. Clin. Med. 2021, 10, 2719. https://doi.org/10.3390/jcm10122719
Ravaux JM, Mauro MD, Vernooy K, Mariani S, Ronco D, Simons J, Van't Hof AW, Veenstra L, Kats S, Maessen JG, et al. Impact of Bundle Branch Block on Permanent Pacemaker Implantation after Transcatheter Aortic Valve Implantation: A Meta-Analysis. Journal of Clinical Medicine. 2021; 10(12):2719. https://doi.org/10.3390/jcm10122719
Chicago/Turabian StyleRavaux, Justine M., Michele Di Mauro, Kevin Vernooy, Silvia Mariani, Daniele Ronco, Jorik Simons, Arnoud W. Van't Hof, Leo Veenstra, Suzanne Kats, Jos G. Maessen, and et al. 2021. "Impact of Bundle Branch Block on Permanent Pacemaker Implantation after Transcatheter Aortic Valve Implantation: A Meta-Analysis" Journal of Clinical Medicine 10, no. 12: 2719. https://doi.org/10.3390/jcm10122719
APA StyleRavaux, J. M., Mauro, M. D., Vernooy, K., Mariani, S., Ronco, D., Simons, J., Van't Hof, A. W., Veenstra, L., Kats, S., Maessen, J. G., & Lorusso, R. (2021). Impact of Bundle Branch Block on Permanent Pacemaker Implantation after Transcatheter Aortic Valve Implantation: A Meta-Analysis. Journal of Clinical Medicine, 10(12), 2719. https://doi.org/10.3390/jcm10122719