Nutrition Assessment and Adverse Outcomes in Hospitalized Patients with Tuberculosis
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patients
2.2. Demography, Comorbidity, and Constitutional Symptoms
2.3. Diagnosis
2.4. Treatment, Adverse Drug Reactions, and Outcomes
2.5. Patient-Generated Subjective Global Assessment
2.6. Statistical Analysis
3. Results
3.1. Demography, Comorbidities, and Clinical Conditions
3.2. Well-Nourished and Malnourished Patients Compared
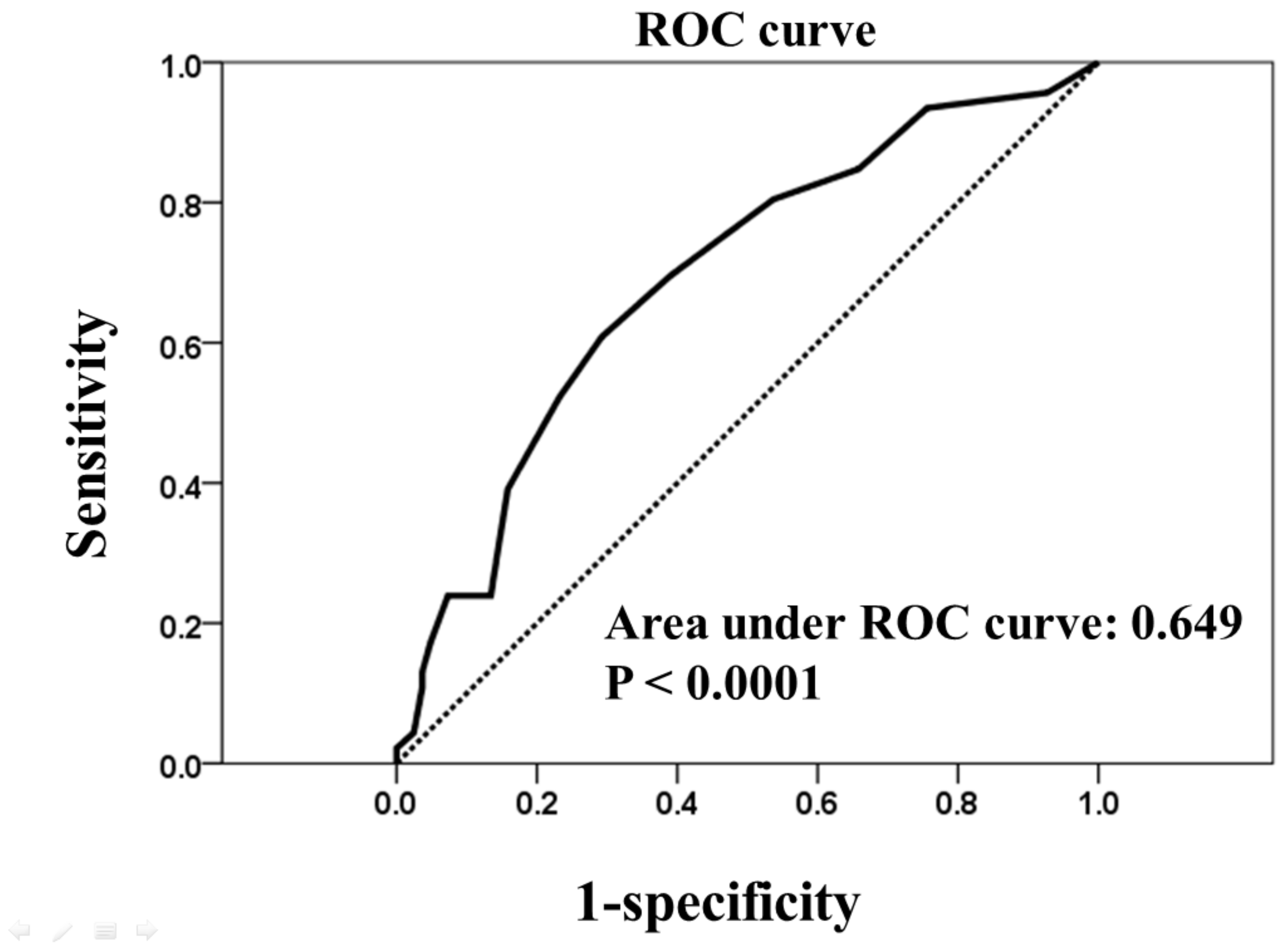
3.3. Factors Associated with Fatal Outcomes
4. Discussion
4.1. Nutrition, Diabetes, and Tuberculosis
4.2. Limitations of BMI Assessment for Elderly Patients
4.3. PG-SGA Scores, Hepatitis, and TB
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2020; World Health Organization: Geneva, Switzerland, 2020; p. 1. [Google Scholar]
- Gupta, K.B.; Gupta, R.; Atreja, A.; Verma, M.; Vishvkarma, S. Tuberculosis and nutrition. Lung India 2009, 26, 9–16. [Google Scholar] [CrossRef]
- Lönnroth, K.; Williams, B.G.; Cegielski, P.; Dye, C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int. J. Epidemiol. 2009, 39, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.J.; Sabina, E.P. Malnutrition and Associated Disorders in Tuberculosis and Its Therapy. J. Diet. Suppl. 2019, 16, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Podewils, L.J.; Holtz, T.; Riekstina, V.; Skripconoka, V.; Zarovska, E.; Kirvelaite, G.; Kreigere, E.; Leimane, V. Impact of malnutrition on clinical presentation, clinical course, and mortality in MDR-TB patients. Epidemiol. Infect. 2010, 139, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, A.; Chatterjee, M.; Jain, Y.; Chatterjee, B.; Kataria, A.; Bhargava, M.; Kataria, R.; D’Souza, R.; Jain, R.; Benedetti, A.; et al. Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality. PLoS ONE 2013, 8, e77979. [Google Scholar] [CrossRef] [PubMed]
- Miyata, S.; Tanaka, M.; Ihaku, D. Subjective Global Assessment in Patients with Pulmonary Tuberculosis. Nutr. Clin. Pract. 2011, 26, 55–60. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Nutritional Care and Support for Patients with Tuberculosis; World Health Organization: Geneva, Switzerland, 2013; p. 3. [Google Scholar]
- Detsky, A.S.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? Parenter Enter. Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef]
- Laky, B.; Janda, M.; Cleghorn, G.; Obermair, A. Comparison of different nutritional assessments and body-composition measurements in detecting malnutrition among gynecologic cancer patients. Am. J. Clin. Nutr. 2008, 87, 1678–1685. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Martinez, L.; Castro-Eguiluz, A.D.; Copca-Mendoza, E.T.; Pérez-Camargo, D.A.; Reyes-Torres, C.A.; Damasco, E.; López-Córdova, G.; Fuentes-Hernández, M.R.; Cetina-Pérez, L.; Milke-García, M.D.P. Nutritional Assessment Tools for the Identification of Malnutrition and Nutritional Risk Associated with Cancer Treatment. Rev. Investig. Clin. 2018, 70, 121–125. [Google Scholar] [CrossRef]
- Thomas, J.M.; Isenring, E.; Kellett, E. Nutritional status and length of stay in patients admitted to an Acute Assessment Unit. J. Hum. Nutr. Diet. 2007, 20, 320–328. [Google Scholar] [CrossRef] [PubMed]
- ter Beek, L.; van der Vaart, H.; Wempe, J.B.; Krijnen, W.P.; Roodenburg, J.L.; van der Schans, C.P.; Jager-Wittenaar, H. Coexistence of Malnutri tion, Frailty, Physical Frailty and Disability in Patients With COPD Starting a Pulmonary Rehabilitation Program. Clin. Nutr. 2020, 39, 2557–2563. [Google Scholar] [CrossRef] [PubMed]
- Ottery, F. Patient-generated subjective global assessment. In The Clinical Guide to Oncology Nutrition; McCallum, P., Polisena, C., Eds.; American Dietetic Association: Chicago, IL, USA, 2000; pp. 11–23. [Google Scholar]
- Tellez-Navarrete, N.A.; Ramon-Luing, L.A.; Muñoz-Torrico, M.; Osuna-Padilla, I.A.; Chavez-Galan, L. Malnutrition and tuberculosis: The gap between basic research and clinical trials. J. Infect Dev. Ctries 2021, 15, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Lönnroth, K.; Roglic, G.; Harries, A.D. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: From evidence to policy and practice. Lancet Diabetes Endocrinol. 2014, 2, 730–739. [Google Scholar] [CrossRef]
- Riza, A.L.; Pearson, F.; Ugarte-Gil, C.; Alisjahbana, B.; van de Vijver, S.; Panduru, N.M.; Hill, P.C.; Ruslami, R.; Moore, D.; Aarnoutse, R.; et al. Clinical management of concurrent diabetes and tuberculosis and the implications for patient services. Lancet Diabetes Endocrinol. 2014, 2, 740–753. [Google Scholar] [CrossRef]
- Huang, T.H.; Chi, C.C.; Liu, C.H.; Chang, C.C.; Kuo, L.M.; Hsieh, C.C. Nutritional status assessed by scored patient-generated subjective global assessment associated with length of hospital stay in adult patients receiving an appendectomy. Biomed. J. 2014, 37, 71–77. [Google Scholar]
- Zachariah, R.; Spielmann, M.; Harries, A.; Salaniponi, F. Moderate to severe malnutrition in patients with tuberculosis is a risk factor associated with early death. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 291–294. [Google Scholar] [CrossRef]
- Hirani, V.; Mindell, J. A comparison of measured height and demi-span equivalent height in the assessment of body mass index among people aged 65 years and over in England. Age Ageing 2008, 37, 311–317. [Google Scholar] [CrossRef]
- Gavriilidou, N.N.; Pihlsgård, M.; Elmståhl, S. High degree of BMI misclassification of malnutrition among Swedish elderly population: Age-adjusted height estimation using knee height and demispan. Eur. J. Clin. Nutr. 2015, 69, 565–571. [Google Scholar] [CrossRef]
- Hassen Ali, A.; Belachew, T.; Yami, A.; Ayen, W.Y. Anti-tuberculosis drug induced hepatotoxicity among TB/HIV co-infected patients at Jimma University Hospital, Ethiopia: Nested case-control study. PLoS ONE 2013, 8, e64622. [Google Scholar] [CrossRef]
- Tostmann, A.; Boeree, M.J.; Aarnoutse, R.E.; de Lange, W.C.; van der Ven, A.J.; Dekhuijzen, R. Antituberculosis drug-induced hepatotoxicity: Concise up-to-date review. J. Gastroenterol. Hepatol. 2008, 23, 192–202. [Google Scholar] [CrossRef]
- Singla, R.; Sharma, S.K.; Mohan, A.; Makharia, G.; Sreenivas, V.; Jha, B.; Kumar, S.; Sarda, P.; Singh, S. Evaluation of risk factors for antituberculosis treatment induced hepatotoxicity. Indian J. Med. Res. 2010, 132, 81–86. [Google Scholar]
- Saukkonen, J.J.; Cohn, D.L.; Jasmer, R.M.; Schenker, S.; Jereb, J.A.; Nolan, C.M.; Peloquin, C.A.; Gordin, F.M.; Nunes, D.; Strader, D.B.; et al. An Official ATS Statement: Hepatotoxicity of Antituberculosis Therapy. Am. J. Respir. Crit. Care Med. 2006, 174, 935–952. [Google Scholar] [CrossRef]
- Singh, J.; Arora, A.; Garg, P.K.; Thakur, V.S.; Pande, J.N.; Tandon, R.K. Antituberculosis treatment-induced hepatotoxicity: Role of predictive factors. Postgrad. Med. J. 1995, 71, 359–362. [Google Scholar] [CrossRef]

| All a | Well-Nourished a | Malnourished a | ||
|---|---|---|---|---|
| Characteristics | n = 128 | n = 65 | n = 63 | p |
| Female a, n (%) | 34 (26.6) | 18 (27.7) | 16 (25.4) | 0769 |
| Elderly b, n (%) | 92 (71.9) | 46 (70.8) | 46 (73.0) | 0.777 |
| Weight (kg) c | 55.3 ± 11.7 | 58.4 ± 11.2 | 52.1 ± 11.4 | 0.002 |
| Body mass index (kg/m2) c,d | 21.4 ± 4.2 | 22.5 ± 3.8 | 20.3 ± 4.3 | 0.002 |
| Body mass index (kg/m2) <18.5 d | 35 (27.7) | 11 (16.9) | 24 (38.4) | 0.007 |
| PG-SGA score c | 5.2 ± 3.7 | 2.6 ± 1.8 | 7.8 ± 3.2 | <0.001 |
| Hemoglobin (mg/dL) c | 11.6 ± 2.6 | 11.9 ± 2.7 | 11.4 ± 2.4 | 0.325 |
| Comorbidity, n (%) | ||||
| Diabetes mellitus | 30 (23.4) | 10 (15.4) | 20 (31.7) | 0.029 |
| Heart disease | 2 (1.6) | 0 (0.0) | 2 (3.2) | 0.240 |
| COPD | 13 (10.2) | 8 (12.3) | 5 (7.9) | 0.413 |
| CKD stage 5 | 6 (4.7) | 3 (4.6) | 3 (4.8) | 1.000 |
| DLC | 3 (2.3) | 2 (3.1) | 1 (1.6) | 1.000 |
| Solid tumor cancer | 23 (18.0) | 10 (15.4) | 13 (20.6) | 0.439 |
| Hematological malignancies | 5 (3.9) | 1 (1.5) | 4 (6.3) | 0.204 |
| Constitutional symptom, n (%) | ||||
| Fever | 34 (26.6) | 14 (21.5) | 20 (31.7) | 0.191 |
| Body weight loss | 10 (7.8) | 5 (9.2) | 5 (9.5) | 1.000 |
| Infectious source, n (%) | ||||
| Pulmonary | 117 (91.4) | 58 (89.2) | 59 (93.7) | 0.372 |
| Extrapulmonary | 19 (14.8) | 11 (16.9) | 8 (12.7) | 0.502 |
| Dissemination | 8 (6.3) | 4 (6.2) | 4 (6.3) | 1.000 |
| Smear positive | 55 (43.0) | 25 (38.5) | 30 (47.6) | 0.295 |
| Liver injury during therapy, n (%) | 26 (20.3) | 8 (12.3) | 18 (28.6) | 0.022 |
| Fatal outcome, n (%) | 26 (20.3) | 5 (7.7) | 21 (33.3) | <0.001 |
| Liver Injury a | Non-Liver Injury a | ||
|---|---|---|---|
| Variables | n = 26 | n = 102 | p |
| Female, n (%) | 5 (19.2) | 29 (28.4) | 0.343 |
| Elderly b, n (%) | 19 (73.1) | 73 (71.6) | 0.879 |
| Body mass index (kg/m2) c,d | 20.7 ± 3.0 | 21.6 ± 4.4 | 0.204 |
| Body mass index (kg/m2) < 18.5 d | 8 (30.8) | 27 (27.0) | 0.717 |
| PG-SGA score c | 7.3 ± 3.6 | 4.7 ± 3.5 | 0.002 |
| Hgb c | 12.3 ± 2.6 | 11.5 ± 2.6 | 0.166 |
| Comorbidity, n (%) | |||
| Diabetes mellitus | 5 (19.2) | 25 (24.5) | 0.571 |
| Heart disease | 2 (7.7) | 0 (0.0) | 0.004 |
| COPD | 4 (15.4) | 9 (8.8) | 0.299 |
| CKD stage 5 | 1 (3.8) | 5 (4.9) | 1.000 |
| DLC | 1 (3.8) | 2 (2.0) | 0.497 |
| Solid tumor cancer | 2 (7.7) | 21 (20.6) | 0.160 |
| Hematological malignancies | 0 (0) | 5 (4.9) | 0.582 |
| Constitutional symptom, n (%) | |||
| Fever | 7 (26.9) | 27 (26.7) | 0.963 |
| Body weight loss | 1 (3.8) | 9 (8.8) | 0.686 |
| Infectious source, n (%) | |||
| Pulmonary | 24 (92.3) | 93 (91.2) | 1.000 |
| Extrapulmonary | 3 (11.5) | 16 (15.7) | 0.762 |
| Dissemination | 1 (3.8) | 7 (6.9) | 1.000 |
| Smear positive, n (%) | 10 (38.5) | 45 (44.1) | 0.603 |
| Multivariate | |||||
|---|---|---|---|---|---|
| Fatal a | Favorable a | Univariate | Odds Ratio | ||
| Variables | n = 26 | n = 102 | p | 95% CI | p |
| Female a, n (%) | 5 (19.2) | 29 (28.4) | 0.343 | ||
| Elderly b, n (%) | 21 (80.8) | 71 (69.6) | 0.258 | ||
| BMI (kg/m2) c,d | 20.9 ± 4.4 | 21.6 ± 4.1 | 0.467 | ||
| BMI (kg/m2) < 18.5 d | 9 (34.6) | 26 (26.0) | 0.525 | ||
| PG-SGA score c | 6.7 ± 4.0 | 4.8 ± 3.5 | 0.028 | 1.142 (1.012–1.288) | 0.031 |
| Hgb c | 11.5 ± 2.5 | 11.7 ± 2.6 | 0.745 | ||
| Comorbidity, n (%) | |||||
| Diabetes mellitus | 10 (38.5) | 20 (19.6) | 0.043 | 1.993 (0.757–5.248) | 0.163 |
| Heart disease | 0 (0.0) | 2 (2.0) | 1.000 | ||
| COPD | 2 (7.8) | 11 (10.8) | 1.000 | ||
| CKD stage 5 | 2 (7.8) | 4 (3.9) | 0.601 | ||
| DLC | 1 (3.8) | 2 (2.0) | 0.497 | ||
| Solid tumor cancer | 8 (30.8) | 15 (14.7) | 0.083 | 2.251 (0.785–6.456) | 0.131 |
| Hematological malignancies | 2 (7.8) | 3 (2.9) | 0.268 | ||
| Constitutional symptom, n (%) | |||||
| Fever | 10 (38.5) | 24 (23.5) | 0.124 | ||
| Body weight loss | 2 (7.8) | 8 (7.8) | 1.000 | ||
| Infectious source, n (%) | |||||
| Pulmonary | 25 (96.2) | 92 (90.2) | 0.460 | ||
| Extrapulmonary | 2 (7.8) | 17 (16.7) | 0.360 | ||
| Dissemination | 1 (3.8) | 7 (6.9) | 1.000 | ||
| Smear positive, n (%) | 15 (57.7) | 40 (39.2) | 0.089 | 1.677 (0.664–4.238) | 0.274 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, H.-S.; Lin, M.-S.; Chi, C.-C.; Ye, J.-J.; Hsieh, C.-C. Nutrition Assessment and Adverse Outcomes in Hospitalized Patients with Tuberculosis. J. Clin. Med. 2021, 10, 2702. https://doi.org/10.3390/jcm10122702
Lin H-S, Lin M-S, Chi C-C, Ye J-J, Hsieh C-C. Nutrition Assessment and Adverse Outcomes in Hospitalized Patients with Tuberculosis. Journal of Clinical Medicine. 2021; 10(12):2702. https://doi.org/10.3390/jcm10122702
Chicago/Turabian StyleLin, Huang-Shen, Ming-Shyan Lin, Ching-Chi Chi, Jung-Jr Ye, and Ching-Chuan Hsieh. 2021. "Nutrition Assessment and Adverse Outcomes in Hospitalized Patients with Tuberculosis" Journal of Clinical Medicine 10, no. 12: 2702. https://doi.org/10.3390/jcm10122702
APA StyleLin, H.-S., Lin, M.-S., Chi, C.-C., Ye, J.-J., & Hsieh, C.-C. (2021). Nutrition Assessment and Adverse Outcomes in Hospitalized Patients with Tuberculosis. Journal of Clinical Medicine, 10(12), 2702. https://doi.org/10.3390/jcm10122702






