A Retrospective Study of Herpetic Keratitis in Patients with Keratoconus after Crosslinking Surgery
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spörl, E.; Seiler, T.; Huhle, M.; Kasper, M. Increased rigidity of the cornea caused by intrastromal cross-linking. Ophthal Mologe 1997, 94, 902–906. [Google Scholar]
- Ting, D.S.J.; Henein, C.; Said, D.G.; Dua, H.S. Photoactivated chromophore for infectious keratitis—Corneal cross-linking (PACK-CXL): A systematic review and meta-analysis. Ocul. Surf. 2019, 17, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Choy, B.N.K.; Ng, A.L.K.; Zhu, M.M.; Liu, C.C.; Xu, S.; Lai, J.S.M. Randomized Control Trial on the Effectiveness of Collagen Cross-linking on Bullous Keratopathy. Cornea 2020, 39, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Abbouda, A.; Abicca, I.; Alió, J.L. Current and Future Applications of Photoactivated Chromophore for Keratitis-Corneal Collagen Cross-Linking (PACK-CXL): An Overview of the Different Treatments Proposed. Semin. Ophthalmol. 2018, 33, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Abbouda, A.; Abicca, I.; Alió, J.L. Infectious Keratitis Following Corneal Crosslinking: A Systematic Review of Reported Cases: Management, Visual Outcome, and Treatment Proposed. Semin. Ophthalmol. 2016, 31, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, S.; Rao, K.; Natrajan, S. Complications of corneal collagen cross-linking. J. Ophthalmol. 2011, 2011, 869015. [Google Scholar] [CrossRef] [PubMed]
- Al-Dujaili, L.J.; Clerkin, P.P.; Clement, C.; McFerrin, H.E.; Bhattacharjee, P.S.; Varnell, E.D.; Kaufman, H.E.; Hill, J.M. Ocular herpes simplex virus: How are latency, reactivation, recurrent disease and therapy interrelated? Future Microbiol. 2011, 6, 877–907. [Google Scholar] [CrossRef] [PubMed]
- Kymionis, G.D.; Portaliou, D.M.; Bouzoukis, D.I.; Suh, L.H.; Pallikaris, A.I.; Markomanolakis, M.; Yoo, S.H. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J. Cataract. Refract. Surg. 2007, 33, 1982–1984. [Google Scholar] [CrossRef] [PubMed]
- Al-Qarni, A.; AlHarbi, M. Herpetic Keratitis after Corneal Collagen Cross-Linking with Riboflavin and Ultraviolet-A for Kerato-conus. Middle East Afr. J. Ophthalmol. 2015, 22, 389–392. [Google Scholar] [CrossRef] [PubMed]
- MYuksel, N.; Bilgihan, K.; Hondur, A.M. Herpetic keratitis after corneal collagen cross-linking with riboflavin and ultraviolet-A for progressive keratoconus. Int. Ophthalmol. 2011, 31, 513–515. [Google Scholar] [CrossRef] [PubMed]
- Sitaula, S.; Singh, S.K.; Gurung, A. Bilateral viral keratitis following corneal collagen crosslinking for progressive keratoconus. J. Ophthalmic Inflamm. Infect. 2019, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Khalili, M.R.; Jahadi, H.R.; Karimi, M.; Yasemi, M. Corneal Collagen Cross-linking for Treatment of Bacterial and Herpetic Keratitis. J. Clin. Diagn. Res. 2017, 11, NC12–NC16. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Liu, T.; Li, H. Effect of Collagen Cross-Linking on Alkali Burn-Induced Corneal Neovascularization in Rabbits. J. Ophthalmol. 2018, 2018, 7325483. [Google Scholar] [CrossRef] [PubMed]


| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Age | 38 | 40 | 31 | 16 | 21 | 18 | 24 | 19 | 29 |
| Gender | M | M | F | F | M | M | M | F | M |
| Keratoconus degree (Amsler–Krumeich classification) | 2–3 | 2 | 3 | 3 | 1–2 | 1–2 | 2 | 2 | 2–3 |
| Previous HSV history | No | Recurrent herpes simplex labialis | No | No | No | No | No | No | No |
| Time of CXL to HSV reactivation (days) | 4 | 6 | 4 | 2 | 5 | 4 | 5 | 3 | 6 |
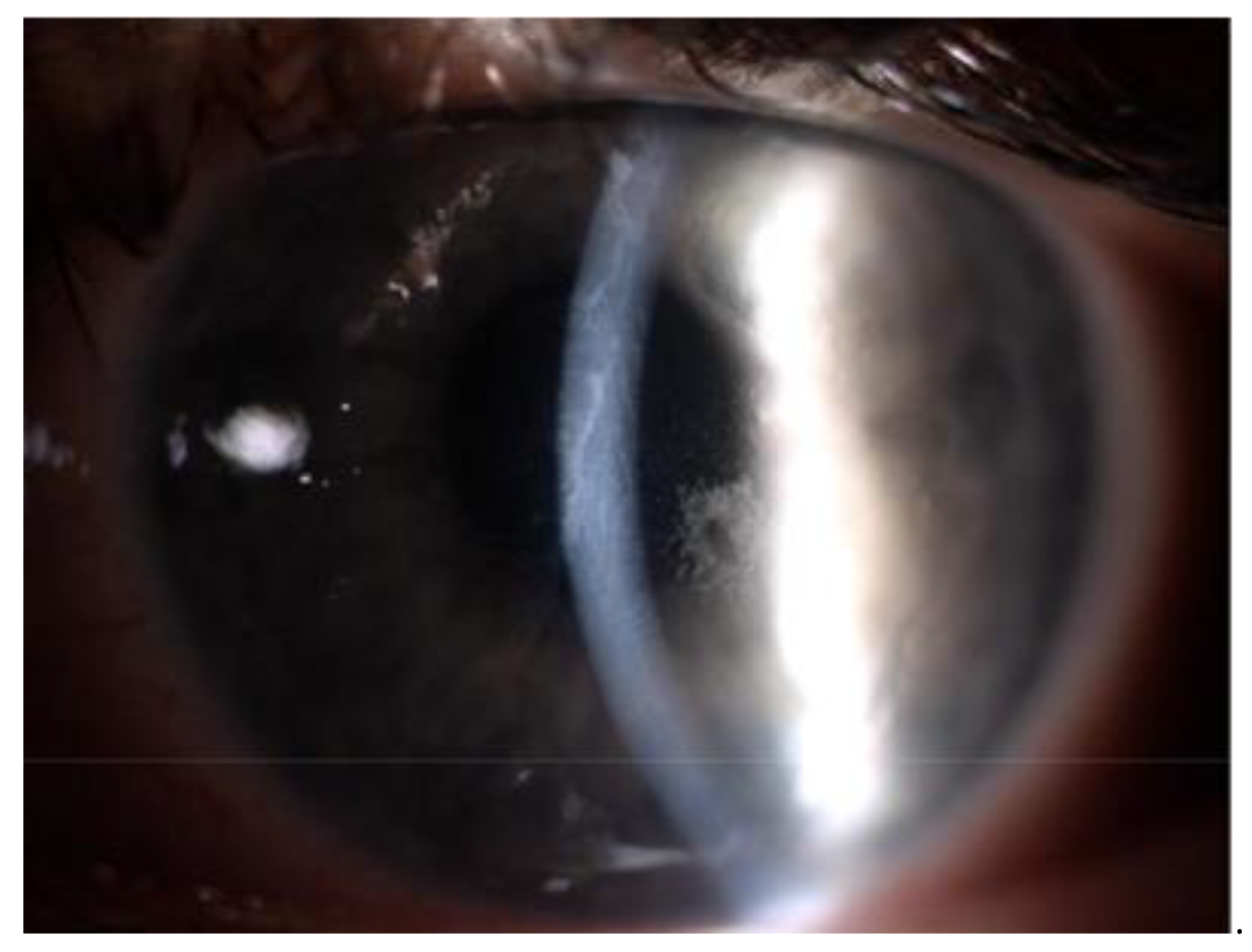
| HSV infection symptom | Dendritic ulcer, Transient corneal opacification | Dendritic ulcer | Dendritic ulcer, Transient corneal opacification | Dendritic ulcer, Significant iritis, Significant corneal edema | Dendritic ulcer | Geographic ulcer | Dendritic ulcer | Dendritic ulcer Mild iritis | Geographic ulcer |
| Time of complete ulcer healing (days) | 10 | 18 | 20 | 21 | 11 | 14 | 10 | 14 | 14 |
| Follow-up time (months) | 38 | 20 | 82 | 36 | 16 | 79 | 52 | 58 | 63 |
| Recurrence of HSV keratitis in follow-up time | No | No | No | No | No | No | No | Yes, one time after 8 months | No |
| Kmean before CXL | 43.6 | 42.5 | 45.8 | 45.5 | 40.3 | 42.0 | 48.2 | 43.6 | 47.8 |
| Kmean 1 year after CXL | 43.2 | 41.8 | 45.8 | 48.4 | 40.2 | 41.9 | 48.0 | 43.6 | 47.8 |
| Kmax before CXL | 53.6 | 50.2 | 54.4 | 56.5 | 45.4 | 49.2 | 54.0 | 50.6 | 58.6 |
| Kmax 1 year after CXL | 52.0 | 49.0 | 54.0 | 57.4 | 47.0 | 48.9 | 53.2 | 49.7 | 57.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wróblewska-Czajka, E.; Nowińska, A.; Dobrowolski, D.; Szkodny, D.; Wylęgała, E. A Retrospective Study of Herpetic Keratitis in Patients with Keratoconus after Crosslinking Surgery. J. Clin. Med. 2021, 10, 2684. https://doi.org/10.3390/jcm10122684
Wróblewska-Czajka E, Nowińska A, Dobrowolski D, Szkodny D, Wylęgała E. A Retrospective Study of Herpetic Keratitis in Patients with Keratoconus after Crosslinking Surgery. Journal of Clinical Medicine. 2021; 10(12):2684. https://doi.org/10.3390/jcm10122684
Chicago/Turabian StyleWróblewska-Czajka, Ewa, Anna Nowińska, Dariusz Dobrowolski, Dominika Szkodny, and Edward Wylęgała. 2021. "A Retrospective Study of Herpetic Keratitis in Patients with Keratoconus after Crosslinking Surgery" Journal of Clinical Medicine 10, no. 12: 2684. https://doi.org/10.3390/jcm10122684
APA StyleWróblewska-Czajka, E., Nowińska, A., Dobrowolski, D., Szkodny, D., & Wylęgała, E. (2021). A Retrospective Study of Herpetic Keratitis in Patients with Keratoconus after Crosslinking Surgery. Journal of Clinical Medicine, 10(12), 2684. https://doi.org/10.3390/jcm10122684







