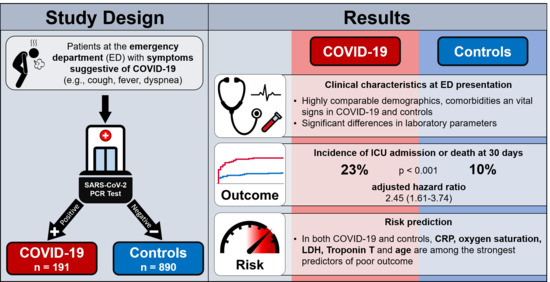
Direct Comparison of Clinical Characteristics, Outcomes, and Risk Prediction in Patients with COVID-19 and Controls—A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Population, and Inclusion Criteria
2.2. Clinical Assessment
2.3. Blood Sampling
2.4. Follow-Up
2.5. Outcomes
2.6. Adjudication of Final Diagnosis
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics in COVID-19 and Controls
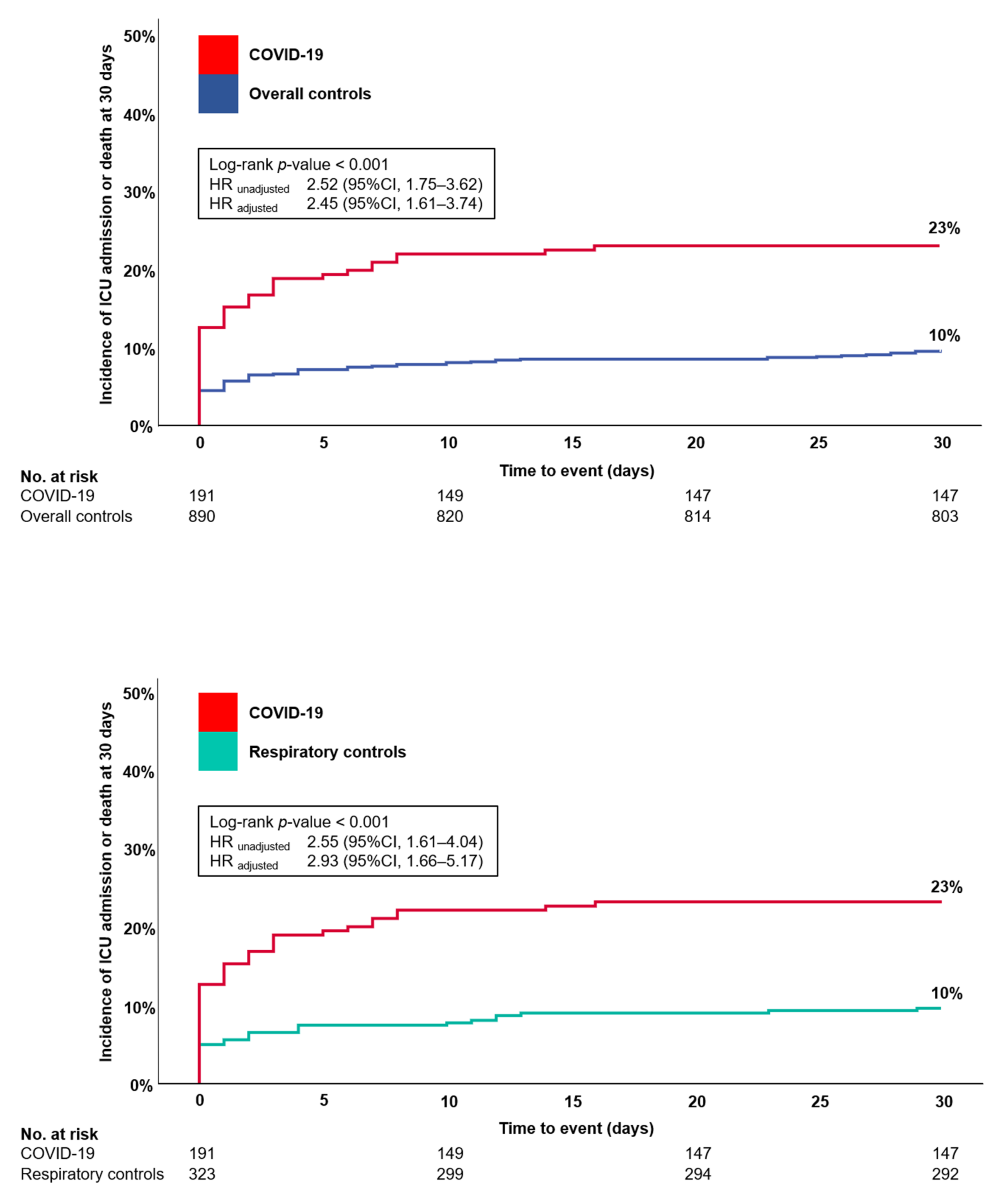
3.2. Patient Management and Outcome in COVID-19 and Controls
3.3. Direct Comparison of Clinical Characteristics between Outcomes in COVID-19 and Controls
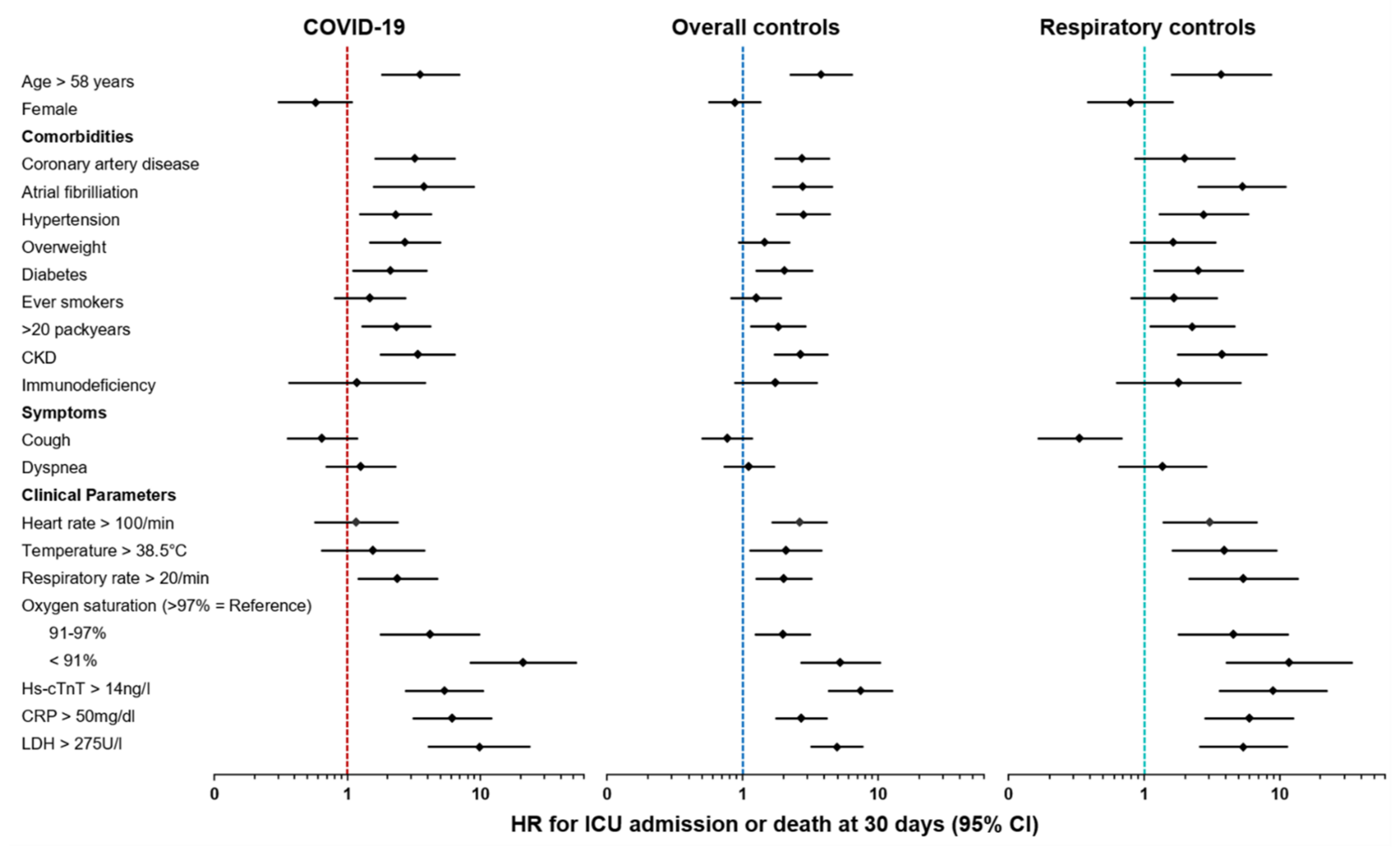
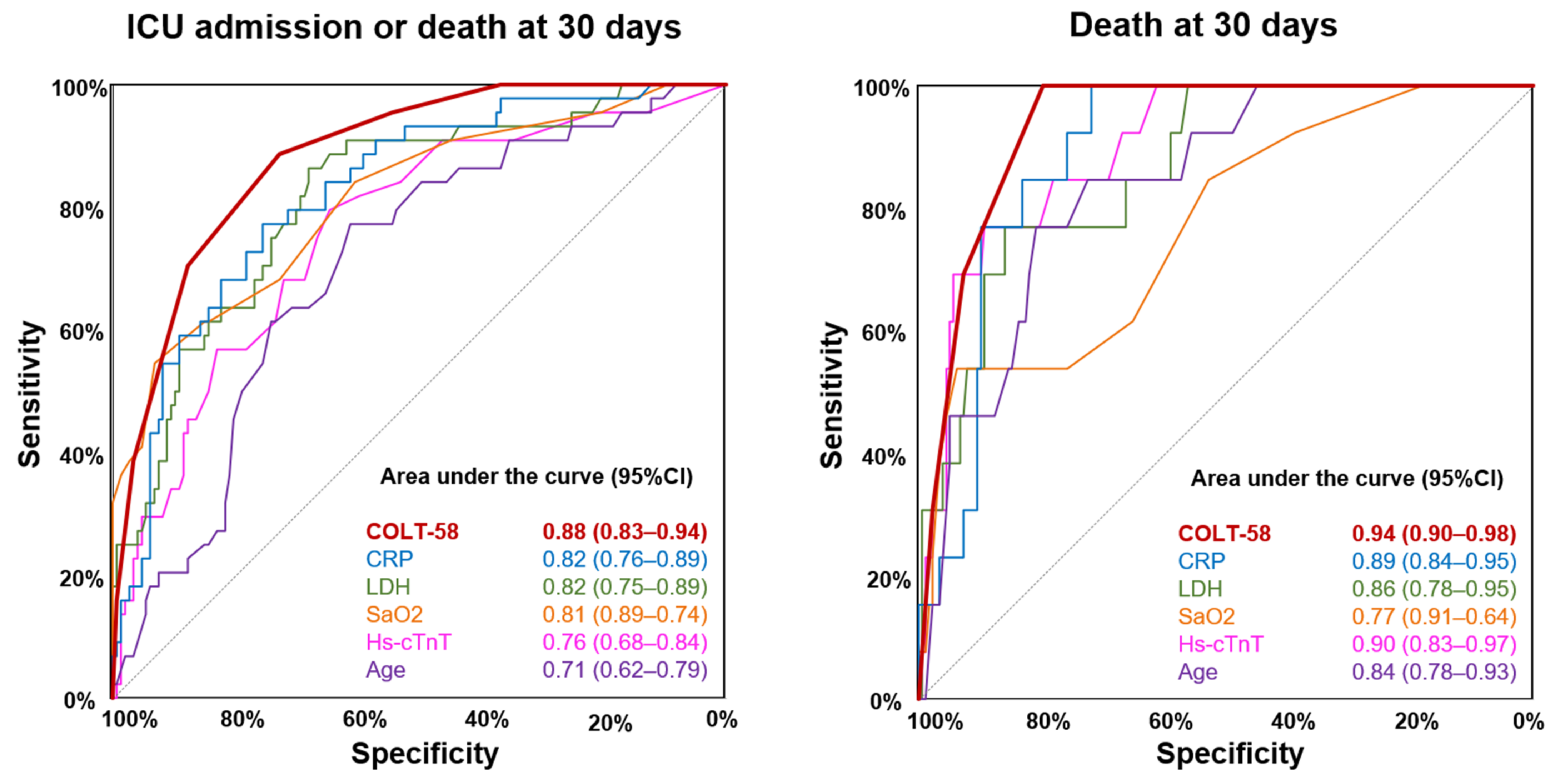
3.4. Predictive Value of Clinical Parameters in COVID-19 and Controls
3.5. Comparison of the COLT-58-Score with the CURB-65-Score
4. Discussion
4.1. Findings
4.2. Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vinay, R.; Baumann, H.; Biller-Andorno, N. Ethics of ICU Triage during COVID-19. Br. Med. Bull. 2021. [Google Scholar] [CrossRef] [PubMed]
- Stang, A.; Stang, M.; Jöckel, K.-H. Estimated Use of Intensive Care Beds Due to COVID-19 in Germany Over Time. Dtsch. Ärztebl. Int. 2020, 117, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Swiss Academy of Medical Sciences. COVID-19 Pandemic: Triage for Intensive-Care Treatment under Resource Scarcity. Swiss Med. Wkly. 2020, 150. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: A Prospective Cohort Study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Lewis, A.M.; Moley, J.R.; Brestoff, J.R. A Systematic Review and Meta-Analysis of Obesity and COVID-19 Outcomes. Sci. Rep. 2021, 11, 7193. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Hu, J.; Zhu, C. Obesity Aggravates COVID-19: A Systematic Review and Meta-Analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Herold, T.; Jurinovic, V.; Arnreich, C.; Lipworth, B.J.; Hellmuth, J.C.; Weinberger, T. Elevated Levels of IL-6 and CRP Predict the Need for Mechanical Ventilation in COVID-19. J. Allergy Clin. Immunol. 2020, 146, 128–136.e4. [Google Scholar] [CrossRef]
- Liu, F.; Li, L.; Xu, M.; Wu, J.; Luo, D. Prognostic Value of Interleukin-6, C-Reactive Protein, and Procalcitonin in Patients with COVID-19. J. Clin. Virol. 2020, 127, 104370. [Google Scholar] [CrossRef]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345. [Google Scholar] [CrossRef]
- Ji, D.; Zhang, D.; Xu, J.; Chen, Z.; Yang, T.; Zhao, P.; Chen, G.; Cheng, G.; Wang, Y.; Bi, J.; et al. Prediction for Progression Risk in Patients With COVID-19 Pneumonia: The CALL Score. Clin. Infect. Dis. 2020, 71, 1393–1399. [Google Scholar] [CrossRef]
- Petrakis, D.; Margină, D.; Tsarouhas, K.; Tekos, F.; Stan, M.; Nikitovic, D.; Kouretas, D.; Spandidos, D.A.; Tsatsakis, A. Obesity —A Risk Factor for Increased COVID-19 Prevalence, Severity and Lethality (Review). Mol. Med. Rep. 2020, 22, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case Characteristics, Resource Use, and Outcomes of 10 021 Patients with COVID-19 Admitted to 920 German Hospitals: An Observational Study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Higuchi, T.; Nishida, T.; Iwahashi, H.; Morimura, O.; Otani, Y.; Okauchi, Y.; Yokoe, M.; Suzuki, N.; Inada, M.; Abe, K. Early Clinical Factors Predicting the Development of Critical Disease in Japanese Patients with COVID-19: A Single-Center, Retrospective, Observational Study. J. Med. Virol. 2021, 93, 2141–2148. [Google Scholar] [CrossRef]
- Ludwig, M.; Jacob, J.; Basedow, F.; Andersohn, F.; Walker, J. Clinical Outcomes and Characteristics of Patients Hospitalized for Influenza or COVID-19 in Germany. Int. J. Infect. Dis. 2021, 103, 316–322. [Google Scholar] [CrossRef]
- Piroth, L.; Cottenet, J.; Mariet, A.-S.; Bonniaud, P.; Blot, M.; Tubert-Bitter, P.; Quantin, C. Comparison of the Characteristics, Morbidity, and Mortality of COVID-19 and Seasonal Influenza: A Nationwide, Population-Based Retrospective Cohort Study. Lancet Respir. Med. 2021, 9, 251–259. [Google Scholar] [CrossRef]
- Brehm, T.T.; van der Meirschen, M.; Hennigs, A.; Roedl, K.; Jarczak, D.; Wichmann, D.; Frings, D.; Nierhaus, A.; Oqueka, T.; Fiedler, W.; et al. Comparison of Clinical Characteristics and Disease Outcome of COVID-19 and Seasonal Influenza. Sci. Rep. 2021, 11, 5803. [Google Scholar] [CrossRef]
- Lim, W.S.; van der Eerden, M.M.; Laing, R.; Boersma, W.G.; Karalus, N.; Town, G.I.; Lewis, S.A.; Macfarlane, J.T. Defining Community Acquired Pneumonia Severity on Presentation to Hospital: An International Derivation and Validation Study. Thorax 2003, 58, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: Hoboken, NJ, USA, 1987; ISBN 978-0-470-31669-6. [Google Scholar]
- Pencina, M.J.; Agostino, R.B.D.; Agostino, R.B.D.; Vasan, R.S. Evaluating the Added Predictive Ability of a New Marker: From Area under the ROC Curve to Reclassification and Beyond. Stat. Med. 2008, 27, 157–172. [Google Scholar] [CrossRef]
- Pencina, M.J.; Steyerberg, E.W.; D’Agostino, R.B. Extensions of Net Reclassification Improvement Calculations to Measure Usefulness of New Biomarkers. Stat. Med. 2011, 30, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-Acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef] [PubMed]
- Ebell, M.H. Outpatient vs. Inpatient Treatment of Community-Acquired Pneumonia. Fam. Pract. Manag. 2006, 13, 41. [Google Scholar]
- De Jong, A.; Molinari, N.; Pouzeratte, Y.; Verzilli, D.; Chanques, G.; Jung, B.; Futier, E.; Perrigault, P.-F.; Colson, P.; Capdevila, X.; et al. Difficult Intubation in Obese Patients: Incidence, Risk Factors, and Complications in the Operating Theatre and in Intensive Care Units. BJA Br. J. Anaesth. 2015, 114, 297–306. [Google Scholar] [CrossRef]
- Capoferri, G.; Osthoff, M.; Egli, A.; Stoeckle, M.; Bassetti, S. Relative Bradycardia in Patients with COVID-19. Clin. Microbiol. Infect. 2021, 27, 295–296. [Google Scholar] [CrossRef]
- Ikeuchi, K.; Saito, M.; Yamamoto, S.; Nagai, H.; Adachi, E. Relative Bradycardia in Patients with Mild-to-Moderate Coronavirus Disease, Japan. Emerg. Infect. Dis. 2020, 26, 2504–2506. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Liang, W.; Jiang, M.; Guan, W.; Zhan, C.; Wang, T.; Tang, C.; Sang, L.; Liu, J.; Ni, Z.; et al. Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. Chest 2020, 158, 97–105. [Google Scholar] [CrossRef] [PubMed]
- The RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, K.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with Covid-19—Preliminary Report. N. Engl. J. Med. [CrossRef]
- WHO Solidarity Trial Consortium; Pan, H.; Peto, R.; Henao-Restrepo, A.-M.; Preziosi, M.-P.; Sathiyamoorthy, V.; Abdool Karim, Q.; Alejandria, M.M.; Hernández García, C.; Kieny, M.-P.; et al. Repurposed Antiviral Drugs for Covid-19—Interim WHO Solidarity Trial Results. N. Engl. J. Med. 2021, 384, 497–511. [Google Scholar] [CrossRef] [PubMed]
- Tworek, A.; Jaroń, K.; Uszyńska-Kałuża, B.; Rydzewski, A.; Gil, R.; Deptała, A.; Franek, E.; Wójtowicz, R.; Życińska, K.; Walecka, I.; et al. Convalescent Plasma Treatment Is Associated with Lower Mortality and Better Outcomes in High-Risk COVID-19 Patients—Propensity-Score Matched Case-Control Study. Int. J. Infect. Dis. 2021, 105, 209–215. [Google Scholar] [CrossRef] [PubMed]
| Measures | COVID-19 | Overall Controls | p-Value 1 | Respiratory Controls | p-Value 2 |
|---|---|---|---|---|---|
| n = 191 | n = 890 | n = 323 | |||
| Demographics | |||||
| Age—years | 57 (44–69) | 59 (41–74) | 0.365 | 58 (42–71) | 0.999 |
| Female | 84 (44) | 385 (43) | 0.855 | 142 (44) | 0.997 |
| Comorbidities–no (%) | |||||
| Cardiac disease | 38 (20) | 261 (29) | 0.008 | 92 (28) | 0.030 |
| Valvular cardiopathy | 8 (4) | 54 (6) | 0.311 | 16 (5) | 0.691 |
| Coronary artery disease | 21 (11) | 131 (15) | 0.179 | 43 (13) | 0.442 |
| Prior myocardial infarction | 9 (5) | 70 (8) | 0.129 | 22 (7) | 0.334 |
| Atrial fibrillation | 9 (5) | 91 (10) | 0.017 | 33 (10) | 0.028 |
| Hypertension | 81 (42) | 367 (41) | 0.765 | 142 (44) | 0.731 |
| Overweight | 74 (39) | 278 (31) | 0.045 | 91 (28) | 0.013 |
| Diabetes | 36 (19) | 145 (16) | 0.391 | 53 (16) | 0.480 |
| Ever smoker | 58 (30) | 361 (41) | 0.009 | 159 (49) | <0.001 |
| -Active smoker | 20 (10) | 209 (23) | <0.001 | 98 (30) | <0.001 |
| -Packyears > 20 | 18 (9) | 164 (18) | 0.003 | 80 (25) | <0.001 |
| Pneumopathy | 37 (19) | 267 (30) | 0.003 | 127 (39) | <0.001 |
| -Asthma | 25 (13) | 112 (13) | 0.849 | 54 (17) | 0.270 |
| -COPD | 9 (5) | 110 (12) | 0.002 | 58 (18) | <0.001 |
| Hepatopathy | 14 (7) | 104 (12) | 0.080 | 37 (11) | 0.131 |
| CKD | 26 (14) | 145 (16) | 0.357 | 39 (12) | 0.612 |
| Stroke | 10 (5) | 70 (8) | 0.208 | 19 (6) | 0.759 |
| Cancer | 17 (9) | 93 (10) | 0.521 | 30 (9) | 0.883 |
| Immunodeficiency | 11 (6) | 56 (6) | 0.782 | 25 (8) | 0.395 |
| Symptoms at ED | |||||
| Symptom duration before ED—days | 7 (3–11) | 3 (2–8) | <0.001 | 4 (2–9) | 0.002 |
| Cough | 126 (66) | 465 (52) | 0.001 | 242 (75) | 0.030 |
| Dyspnea | 81 (42) | 438 (49) | 0.088 | 185 (57) | 0.001 |
| Vital signs at ED | |||||
| Systolic BP—mmHg | 135 (122–148.5) | 137 (121–156) | 0.103 | 139 (122–155) | 0.041 |
| Diastolic BP—mmHg | 82 (71–90) | 81 (72–90) | 0.758 | 82 (73–89) | 0.988 |
| Heart rate—/min | 89 (80–103) | 88 (75–103) | 0.252 | 90 (76–104) | 0.967 |
| Blood oxygen saturation—% | 97 (94–98) | 97 (95–98) | 0.009 | 97 (95–98) | 0.274 |
| Respiratory rate—/min | 20 (16–24) | 18 (16–23) | 0.034 | 19 (16–23) | 0.290 |
| Temperature—°C | 37.1 (36.8–38) | 37.0 (36.5–37.7) | 0.001 | 37.0 (36.6–37.5) | 0.009 |
| Laboratory parameters at ED | |||||
| Leukocytes—G/L | 6.27 (4.95–8.34) | 8.82 (6.82–11.70) | <0.001 | 9.08 (7.12–11.69) | <0.001 |
| Lymphocytes—% | 19.15 (11.85–26.85) | 17.15 (9.80–26.60) | 0.072 | 18.35 (9.45–26.85) | 0.246 |
| Lymphocytes absolute—G/L | 1.07 (0.72–1.57) | 1.47 (0.90–2.08) | <0.001 | 1.60 (1.00–2.19) | <0.001 |
| Thrombocytes—G/L | 218 (177–277) | 240 (196–291) | 0.004 | 249 (205–294) | <0.001 |
| CRP—mg/dL | 28.9 (2.6–73.4) | 7.6 (1.2–47.6) | <0.001 | 9.0 (1.4–48.5) | 0.001 |
| Ferritin—µg/L | 387 (164–823) | 163 (85–329) | <0.001 | 162 (85–296) | <0.001 |
| eGFR—mL/min/1.73 m² | 93 (68–103) | 89 (68–106) | 0.708 | 92 (72–109) | 0.109 |
| Sodium—mmol/L | 137 (134–140) | 139 (136–141) | 0.001 | 138 (136–141) | 0.001 |
| Potassium—mmol/L | 3.9 (3.7–4.2) | 4 (3.8–4.3) | 0.027 | 4 (3.7–4.3) | 0.119 |
| LDH—U/L | 254 (201–352) | 215 (186–259) | <0.001 | 209 (185–254) | <0.001 |
| ASAT—U/L | 32 (23–45) | 26 (21–33) | <0.001 | 26 (21–33) | <0.001 |
| Albumin—g/L | 34 (30–38) | 37 (32–40) | <0.001 | 37 (32–40) | <0.001 |
| Hs-cTnT—ng/L | 7 (4–14) | 9 (4–22) | 0.033 | 7 (4–17) | 0.573 |
| NT-proBNP—pg/mL | 77 (49–242) | 115 (49–462) | 0.019 | 97 (49–272) | 0.359 |
| Measures | COVID-19 | Overall Controls | p-Value 1 | Respiratory Controls | p-Value 2 |
|---|---|---|---|---|---|
| n = 191 | n = 890 | n = 323 | |||
| Patient management—no (%) | |||||
| Outpatient | 77 (40) | 446 (50) | 0.014 | 185 (57) | <0.001 |
| Inpatient | 114 (60) | 444 (50) | 138 (43) | ||
| Length of hospital stay—days | |||||
| -Overall | 4 (0–9) | 0 (0–6) | <0.001 | 0 (0–5) | <0.001 |
| -Inpatients | 7 (4–13) | 6 (3–10) | 0.013 | 6 (3–10) | 0.003 |
| Clinical course and outcomes | |||||
| ICU admission or death at 30 days | 44 (23) | 87 (10) | <0.001 | 31 (10) | <0.001 |
| Death at 30 days | 13 (7) | 34 (4) | 0.063 | 13 (4) | 0.167 |
| ICU admission | 40 (21) | 63 (7) | <0.001 | 23 (7) | <0.001 |
| -Days at ICU | 9 (4–16.5) | 2 (1–4) | <0.001 | 3 (1.5–8.5) | <0.001 |
| Intubation | 30 (16) | 23 (3) | <0.001 | 15 (5) | <0.001 |
| -Days intubated | 9 (6–12) | 2 (1–7) | <0.001 | 3 (1–8) | <0.001 |
| Hemodynamic support | 28 (15) | 26 (3) | <0.001 | 14 (4) | <0.001 |
| ARDS | 26 (14) | 6 (1) | <0.001 | 4 (1) | <0.001 |
| Rehospitalisation for respiratory reasons at 30 days | 4 (2) | 10 (1) | 0.278 | 3 (1) | 0.268 |
| Measures | COVID-19 | p-Value 1 | Overall Controls | p-Value 1 | Respiratory Controls | p-Value 1 | |||
|---|---|---|---|---|---|---|---|---|---|
| n = 191 | n = 890 | n = 323 | |||||||
| Composite Outcome | Composite Outcome | Composite Outcome | |||||||
| yes | no | yes | no | yes | no | ||||
| n = 44 | n = 147 | n = 87 | n = 803 | n = 31 | n = 292 | ||||
| Demographics | |||||||||
| Age—years | 66 (58–74) | 54 (41–64) | <0.001 | 71 (60–79) | 57 (39–73) | <0.001 | 70 (60–77) | 56 (40–69.5) | 0.001 |
| Female | 14 (32) | 70 (48) | 0.064 | 35 (40) | 350 (44) | 0.548 | 12 (39) | 130 (45) | 0.535 |
| Comorbidities—no (%) | |||||||||
| Cardiac disease | 19 (43) | 19 (13) | <0.001 | 53 (61) | 208 (26) | <0.001 | 21 (68) | 71 (24) | <0.001 |
| Valvular cardiopathy | 4 (9) | 4 (3) | 0.064 | 11 (13) | 43 (5) | 0.007 | 3 (10) | 13 (4) | 0.202 |
| Coronary artery disease | 11 (25) | 10 (7) | 0.001 | 27 (31) | 104 (13) | <0.001 | 7 (23) | 36 (12) | 0.11 |
| Prior myocardial infarction | 4 (9) | 5 (3) | 0.118 | 20 (23) | 50 (6) | <0.001 | 4 (13) | 18 (6) | 0.157 |
| Atrial fibrillation | 6 (14) | 3 (2) | 0.001 | 20 (23) | 71 (9) | <0.001 | 11 (35) | 22 (8) | <0.001 |
| Hypertension | 27 (61) | 54 (37) | 0.004 | 57 (66) | 310 (39) | <0.001 | 21 (68) | 121 (41) | 0.005 |
| Overweight | 27 (61) | 47 (32) | <0.001 | 34 (39) | 244 (30) | 0.096 | 12 (39) | 79 (27) | 0.17 |
| Diabetes | 14 (32) | 22 (15) | 0.012 | 24 (28) | 121 (15) | 0.003 | 10 (32) | 43 (15) | 0.012 |
| Ever smoker | 17 (39) | 41 (28) | 0.174 | 40 (46) | 321 (40) | 0.279 | 19 (61) | 140 (48) | 0.158 |
| -Active smoker | 2 (5) | 18 (12) | 0.143 | 24 (28) | 185 (23) | 0.342 | 13 (42) | 85 (29) | 0.14 |
| -Packyears > 20 | 8 (18) | 10 (7) | 0.023 | 25 (29) | 139 (17) | 0.009 | 13 (42) | 67 (23) | 0.02 |
| Pneumopathy | 9 (20) | 28 (19) | 0.836 | 27 (31) | 240 (30) | 0.825 | 12 (39) | 115 (39) | 0.942 |
| -Asthma | 4 (9) | 21 (14) | 0.37 | 2 (2) | 110 (14) | 0.002 | 0 (0) | 54 (18) | 0.009 |
| -COPD | 5 (11) | 4 (3) | 0.018 | 14 (16) | 96 (12) | 0.265 | 9 (29) | 49 (17) | 0.091 |
| Hepatopathy | 2 (5) | 12 (8) | 0.419 | 24 (28) | 80 (10) | <0.001 | 9 (29) | 28 (10) | 0.001 |
| CKD | 14 (32) | 12 (8) | <0.001 | 29 (33) | 116 (14) | <0.001 | 10 (32) | 29 (10) | <0.001 |
| Stroke | 4 (9) | 6 (4) | 0.191 | 14 (16) | 56 (7) | 0.003 | 5 (16) | 14 (5) | 0.011 |
| Cancer | 7 (16) | 10 (7) | 0.063 | 18 (21) | 75 (9) | 0.001 | 7 (23) | 23 (8) | 0.007 |
| Immunodeficiency | 3 (7) | 8 (5) | 0.731 | 9 (10) | 47 (6) | 0.101 | 4 (13) | 21 (7) | 0.258 |
| Symptoms at ED | |||||||||
| Symptom duration before ED—days | 4 (2–10) | 7 (3–11) | 0.047 | 2 (1–3) | 3 (2–9) | <0.001 | 3 (2–3) | 5 (2–10) | 0.001 |
| Cough | 25 (57) | 101 (69) | 0.144 | 40 (46) | 425 (53) | 0.218 | 16 (52) | 226 (77) | 0.002 |
| Dyspnea | 21 (48) | 60 (41) | 0.416 | 45 (52) | 393 (49) | 0.622 | 20 (65) | 165 (57) | 0.391 |
| Vital signs at ED | |||||||||
| Systolic BP—mmHg | 133 (111–149) | 135 (123–148) | 0.288 | 123 (106–151) | 138 (122–156) | <0.001 | 128 (106–154) | 140 (124–155) | 0.074 |
| Diastolic BP—mmHg | 76 (63–90) | 83 (74–89) | 0.037 | 72 (63–82) | 81 (73–90) | <0.001 | 77 (65–85) | 82 (73–89) | 0.02 |
| Heart rate—/min | 91 (82–110) | 88 (80–102) | 0.293 | 100 (81–118) | 87 (74–101) | <0.001 | 110 (77–125) | 89 (76–103) | 0.018 |
| Blood oxygen saturation—% | 93 (89–96) | 97 (95–98) | <0.001 | 96 (93–99) | 97 (96–98) | 0.015 | 94 (90–96) | 97 (95–98) | <0.001 |
| Respiratory rate—/min | 24 (20–28) | 19 (16–23) | <0.001 | 21 (16–25) | 18 (16–22) | 0.001 | 25 (21–30) | 19 (16–22) | <0.001 |
| Temperature—°C | 37.1 (36.5–38.3) | 37.1 (36.8–38) | 0.68 | 37.2 (36.9–38.2) | 37 (36.5–37.6) | 0.007 | 37.35 (36.9–38.8) | 37 (36.6–37.5) | 0.044 |
| Laboratory parameters at ED | |||||||||
| Leukocytes—G/L | 7.63 (5.79–10.53) | 6.04 (4.65–7.55) | 0.002 | 11.70 (7.77–14.92) | 8.67 (6.79–11.21) | <0.001 | 12.535 (8.52–16.53) | 8.87 (7.09–11.185) | 0.001 |
| Lymphocytes—% | 11.4 (6.5–19.4) | 21.2 (13.7–28.5) | <0.001 | 9.5 (5.4–14.4) | 18.4 (10.5–27.3) | <0.001 | 7.6 (5.1–12.9) | 20.1 (11.1–28) | <0.001 |
| Lymphocytes absolute—G/L | 0.77 (0.57–1.31) | 1.14 (0.84–1.65) | <0.001 | 1.06 (0.79–1.39) | 1.53 (0.93–2.14) | <0.001 | 1.03 (0.67–1.36) | 1.67 (1.06–2.22) | <0.001 |
| Thrombocytes—G/L | 208 (146–274) | 219 (180–279) | 0.193 | 223 (178–316) | 241 (197–287) | 0.428 | 231.5 (186–313) | 252 (208–291) | 0.556 |
| CRP—mg/dL | 112.6 (47.6–162.7) | 15.6 (1.6–46.7) | <0.001 | 40.1 (10.8–113.8) | 6.4 (1.1–40.6) | <0.001 | 86.1 (34.7–129.9) | 6.1 (1.3–35.4) | <0.001 |
| Ferritin—µg/L | 1206 (441–2097) | 306 (132–612) | <0.001 | 263 (119–515) | 159 (84–308) | 0.001 | 212 (104–283) | 159 (85–300) | 0.432 |
| eGFR—mL/min/1.73 m² | 67 (41–98) | 95 (77–105) | <0.001 | 72 (44–88) | 91 (72–107) | <0.001 | 70 (48–91) | 93.5 (75–110) | 0.001 |
| Sodium—mmol/L | 136 (134–139) | 137 (134–140) | 0.31 | 138 (135–142) | 139 (136–141) | 0.772 | 136 (133–139) | 139 (136–141) | 0.057 |
| Potassium—mmol/L | 4.1 (3.7–4.6) | 3.9 (3.7–4.1) | 0.181 | 4 (3.7–4.5) | 4 (3.8–4.3) | 0.284 | 4.2 (3.6–4.5) | 4 (3.8–4.2) | 0.299 |
| LDH—U/L | 420 (299–531) | 236 (193–300) | <0.001 | 295 (236–381) | 209 (184–247) | <0.001 | 315 (237–364) | 207 (184–242) | <0.001 |
| ASAT—U/L | 45 (36–64) | 28 (22–40) | <0.001 | 33 (24–56) | 26 (21–32) | <0.001 | 34 (22–50) | 26 (21–32) | 0.079 |
| Albumin—g/L | 29 (26–33) | 35 (31–38) | <0.001 | 31 (25.5–35) | 37 (33–40) | <0.001 | 29 (25–34) | 38 (33–40) | <0.001 |
| Hs-cTnT—ng/L | 18 (9–40) | 6 (4–12) | <0.001 | 34 (20–83) | 8 (4–18) | <0.001 | 30 (21–51) | 6 (4–15) | <0.001 |
| NT-proBNP—pg/mL | 350 (82–1909) | 63 (49–145) | <0.001 | 945 (286–4577) | 96 (49–351) | <0.001 | 2287 (446–11052) | 81 (49–208) | <0.001 |
| Measures | COVID-19 | Overall Controls | Respiratory Controls |
|---|---|---|---|
| HR (95%CI) | HR (95%CI) | HR (95%CI) | |
| Demographics | |||
| Age in decades | 1.42 (1.18–1.71) | 1.35 (1.20–1.52) | 1.35 (1.11–1.66) |
| Female | 0.57 (0.30–1.08) | 0.88 (0.57–1.34) | 0.79 (0.39–1.63) |
| Comorbidities | |||
| Cardiac disease | 3.58 (1.97–6.52) | 4.00 (2.60–6.15) | 5.67 (2.67–12.05) |
| Coronary artery disease | 3.20 (1.62–6.35) | 2.75 (1.74–4.33) | 1.99 (0.86–4.61) |
| Atrial fibrillation | 3.74 (1.58–8.86) | 2.76 (1.68–4.55) | 5.28 (2.53–11.03) |
| Hypertension | 2.30 (1.25–4.22) | 2.81 (1.81–4.37) | 2.76 (1.30–5.85) |
| Overweight | 2.70 (1.47–4.96) | 1.44 (0.94–2.22) | 1.64 (0.79–3.37) |
| Diabetes | 2.09 (1.11–3.94) | 2.03 (1.27–3.25) | 2.52 (1.19–5.34) |
| Ever smoker | 1.49 (0.81–2.73) | 1.26 (0.83–1.92) | 1.66 (0.81–3.42) |
| -Packyears > 20y | 2.34 (1.09–5.04) | 1.83 (1.15–2.91) | 2.27 (1.11–4.64) |
| COPD | 2.86 (1.13–7.25) | 1.38 (0.78–2.44) | 1.89 (0.87–4.11) |
| CKD | 3.37 (1.79–6.37) | 2.69 (1.72–4.21) | 3.78 (1.78–8.02) |
| Cancer | 2.04 (0.91–4.59) | 2.27 (1.35–3.82) | 3.03 (1.31–7.04) |
| Immunodeficiency | 1.18 (0.37, 3.82) | 1.76 (0.88, 3.50) | 1.81 (0.63, 5.17) |
| Symptoms at ED | |||
| Symptom duration before ED—days | 0.97 (0.92–1.02) | 0.84 (0.77–0.92) | 0.78 (0.66–0.93) |
| Cough | 0.65 (0.36–1.18) | 0.77 (0.51–1.17) | 0.34 (0.17–0.68) |
| Dyspnea | 1.26 (0.70–2.27) | 1.12 (0.73–1.70) | 1.38 (0.66–2.87) |
| Vital signs at ED – per unit increase | |||
| Systolic BP | 0.99 (0.97–1.01) | 0.98 (0.97–0.99) | 0.98 (0.96–0.99) |
| Diastolic BP | 0.97 (0.94–0.99) | 0.97 (0.96–0.98) | 0.98 (0.96–0.99) |
| Heart rate | 1.01 (0.99–1.03) | 1.03 (1.02–1.04) | 1.03 (1.01–1.05) |
| Blood oxygen saturation | 0.92 (0.90–0.95) | 0.92 (0.89–0.95) | 0.85 (0.80–0.89) |
| Respiratory rate | 1.11 (1.05–1.17) | 1.09 (1.05–1.12) | 1.14 (1.09–1.19) |
| Temperature | 0.93 (0.62–1.40) | 1.39 (1.11–1.74) | 1.76 (1.20–2.58) |
| Laboratory parameters—per decades | |||
| Leukocytes | 1.534 (1.158–2.031) | 2.434 (1.759–3.369) | 2.708 (1.604–4.572) |
| Lymphocytes | 0.523 (0.363–0.752) | 0.465 (0.359–0.603) | 0.299 (0.177–0.508) |
| Lymphocytes absolute | 1.259 (0.707–2.242) | 0.017 (0.001–0.287) | 0.002 (0.000–0.317) |
| Thrombocytes | 0.984 (0.950–1.020) | 1.000 (0.976–1.024) | 0.980 (0.936–1.027) |
| CRP | 1.105 (1.072–1.140) | 1.065 (1.042–1.088) | 1.094 (1.060–1.129) |
| Ferritin | 1.001 (1.001–1.002) | 1.004 (1.001–1.007) | 1.006 (0.998–1.014) |
| eGFR | 0.809 (0.735–0.890) | 0.842 (0.785–0.902) | 0.865 (0.763–0.980) |
| LDH | 1.035 (1.025–1.045) | 1.011 (1.009–1.014) | 1.009 (1.006–1.013) |
| ASAT | 1.025 (1.010–1.039) | 1.024 (1.016–1.033) | 1.076 (1.034–1.119) |
| Hs-cTnT | 1.110 (1.064–1.157) | 1.005 (1.004–1.007) | 1.004 (1.002–1.007) |
| NT-proBNP | 1.001 (1.000–1.002) | 1.000 (1.000–1.001) | 1.000 (1.000–1.001) |
| Letter | Risk Factor | Score | |
|---|---|---|---|
| C | CRP | >50 mg/dL | +1 |
| O | Oxygen saturation | 91–96% | +1 |
| <91% | +2 | ||
| L | LDH | >275 U/L | +1 |
| T | High-sensitivity Troponin T | >14 ng/L | +1 |
| 58 | Age | >58 years | +1 |
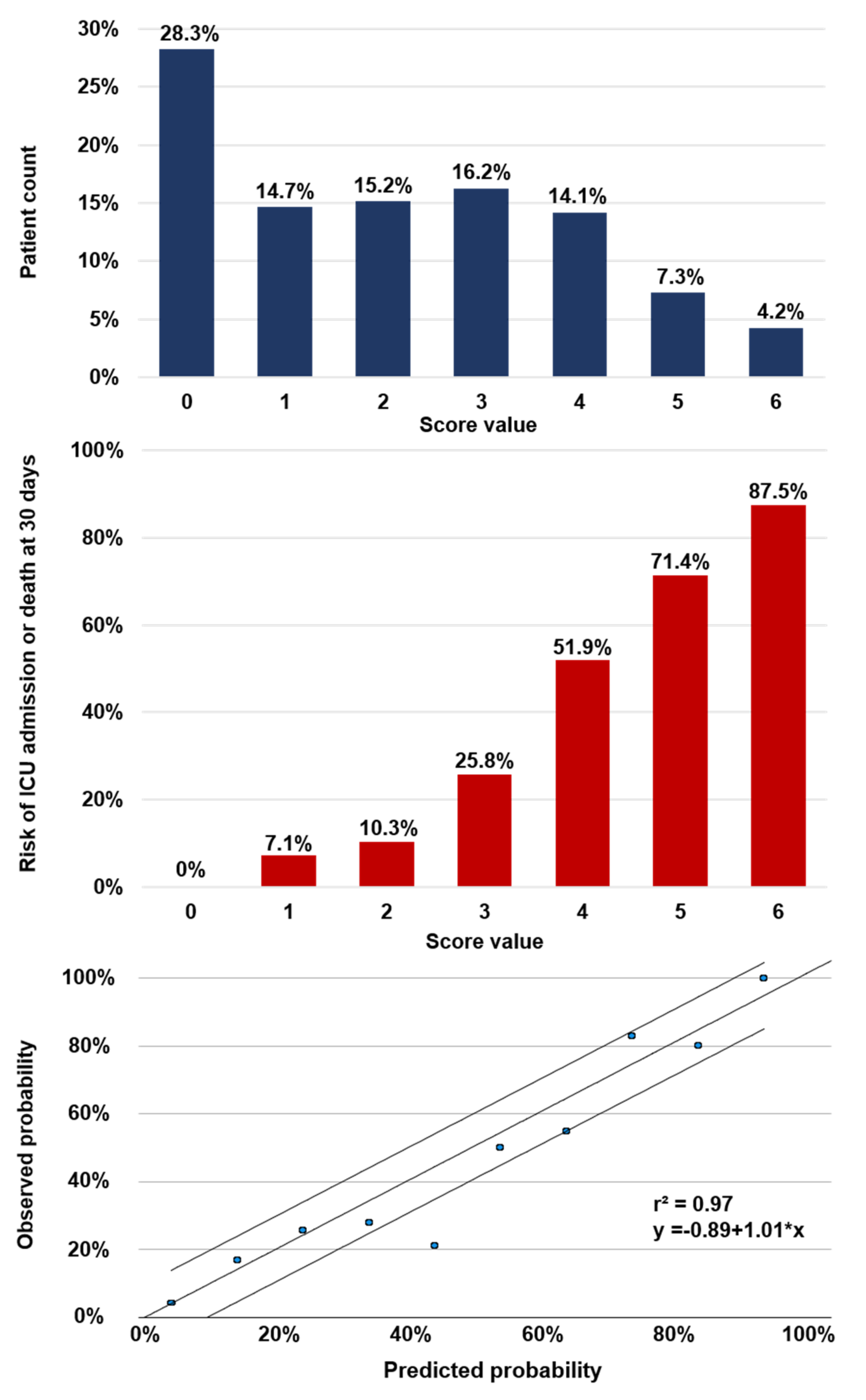
| Cut-off Value | No of Patients (%) | Sensitivity 1 -% (95% CI) | NPV 1 -% (95% CI) | Specificity 1 -% (95% CI) | PPV 1 -% (95% CI) | Composite Outcome -% | Death at 30d -% |
|---|---|---|---|---|---|---|---|
| Rule-out | |||||||
| 0 | 54 (28.3) | 100 (92–100) | 100 (93.4–100) | 36.7 (29.4–44.8) | 32.1 (24.9–40.3) | 0 | 0 |
| ≤1 | 82 (42.9) | 95.5 (84.9–98.7) | 97.6 (91.5–99.3) | 54.4 (46.4–62.3) | 38.5 (29.9–47.9) | 2.4 | 0 |
| ≤2 | 111 (58.1) | 88.6 (76–95) | 95.5 (89.9–98.1) | 72.1 (64.4–78.7) | 48.8 (38.1–59.5) | 4.5 | 0 |
| ≤3 | 142 (74.3) | 70.5 (55.8–81.8) | 90.8 (85–94.6) | 87.8 (81.5–92.1) | 63.3 (49.3–75.3) | 9.2 | 0 |
| Rule-in | |||||||
| ≥3 | 80 (41.9) | 88.6 (76–95) | 95.5 (89.9–98.1) | 72.1 (64.4–78.7) | 48.8 (38.1–59.5) | 48.8 | 16.3 |
| ≥4 | 49 (25.7) | 70.5 (55.8–81.8) | 90.8 (85–94.6) | 87.8 (81.5–92.1) | 63.3 (49.3–75.3) | 63.3 | 26.5 |
| ≥5 | 22 (11.5) | 38.6 (25.7–53.4) | 84.0 (77.8–88.8) | 96.6 (92.3–98.5) | 77.3 (56.6–89.9) | 77.3 | 40.9 |
| 6 | 8 (4.2) | 15.9 (7.9–29.4) | 79.8 (73.4–85) | 99.3 (96.2–99.9) | 87.5 (52.9–97.8) | 87.5 | 50.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lampart, M.; Rüegg, M.; Jauslin, A.S.; Simon, N.R.; Zellweger, N.; Eken, C.; Tschudin-Sutter, S.; Bassetti, S.; Rentsch, K.M.; Siegemund, M.; et al. Direct Comparison of Clinical Characteristics, Outcomes, and Risk Prediction in Patients with COVID-19 and Controls—A Prospective Cohort Study. J. Clin. Med. 2021, 10, 2672. https://doi.org/10.3390/jcm10122672
Lampart M, Rüegg M, Jauslin AS, Simon NR, Zellweger N, Eken C, Tschudin-Sutter S, Bassetti S, Rentsch KM, Siegemund M, et al. Direct Comparison of Clinical Characteristics, Outcomes, and Risk Prediction in Patients with COVID-19 and Controls—A Prospective Cohort Study. Journal of Clinical Medicine. 2021; 10(12):2672. https://doi.org/10.3390/jcm10122672
Chicago/Turabian StyleLampart, Maurin, Marco Rüegg, Andrea S. Jauslin, Noemi R. Simon, Núria Zellweger, Ceylan Eken, Sarah Tschudin-Sutter, Stefano Bassetti, Katharina M. Rentsch, Martin Siegemund, and et al. 2021. "Direct Comparison of Clinical Characteristics, Outcomes, and Risk Prediction in Patients with COVID-19 and Controls—A Prospective Cohort Study" Journal of Clinical Medicine 10, no. 12: 2672. https://doi.org/10.3390/jcm10122672
APA StyleLampart, M., Rüegg, M., Jauslin, A. S., Simon, N. R., Zellweger, N., Eken, C., Tschudin-Sutter, S., Bassetti, S., Rentsch, K. M., Siegemund, M., Bingisser, R., Nickel, C. H., Osswald, S., Kuster, G. M., & Twerenbold, R. (2021). Direct Comparison of Clinical Characteristics, Outcomes, and Risk Prediction in Patients with COVID-19 and Controls—A Prospective Cohort Study. Journal of Clinical Medicine, 10(12), 2672. https://doi.org/10.3390/jcm10122672