Ablation Modalities for Therapeutic Intervention in Arrhythmia-Related Cardiovascular Disease: Focus on Electroporation
Abstract
1. Introduction
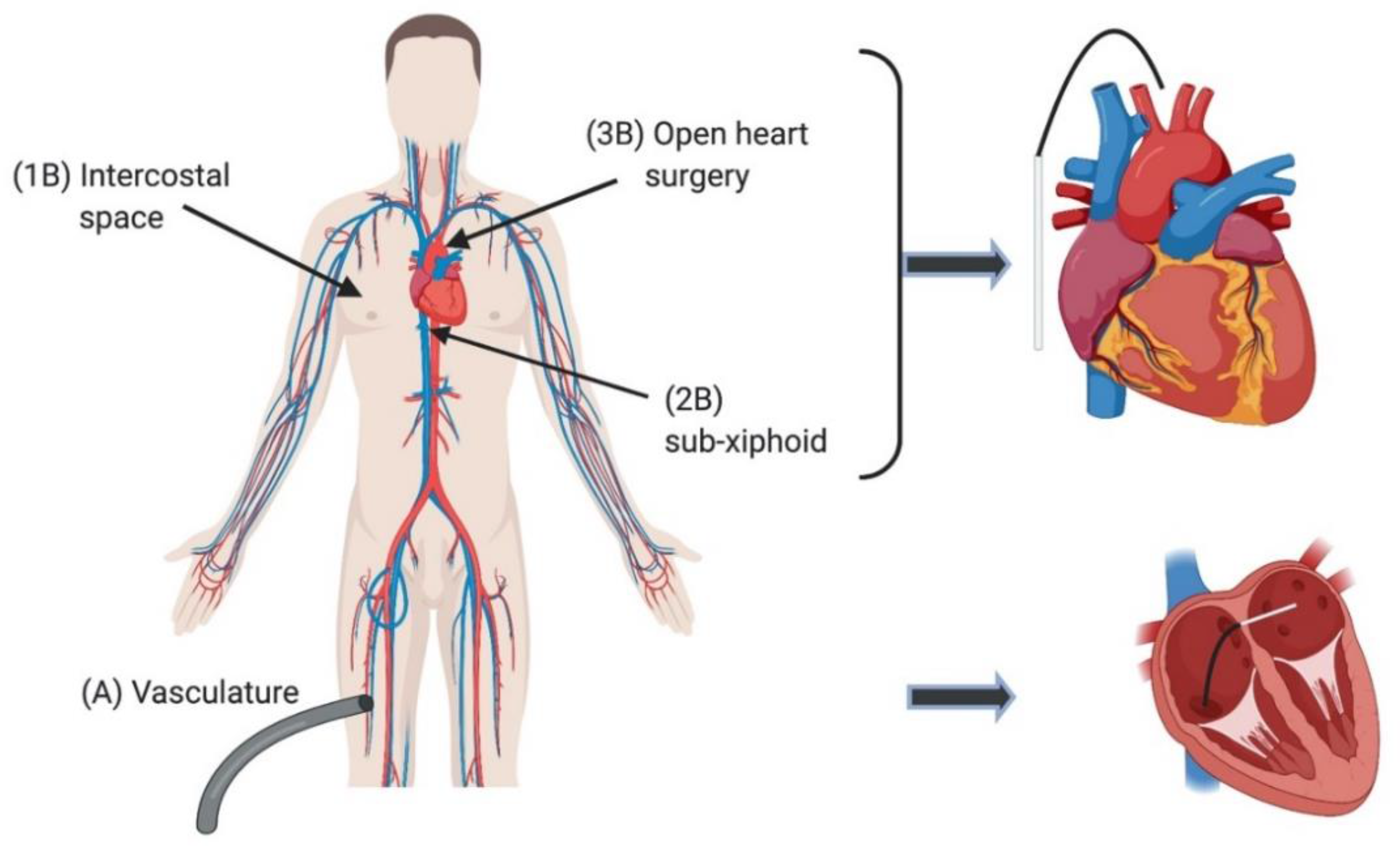
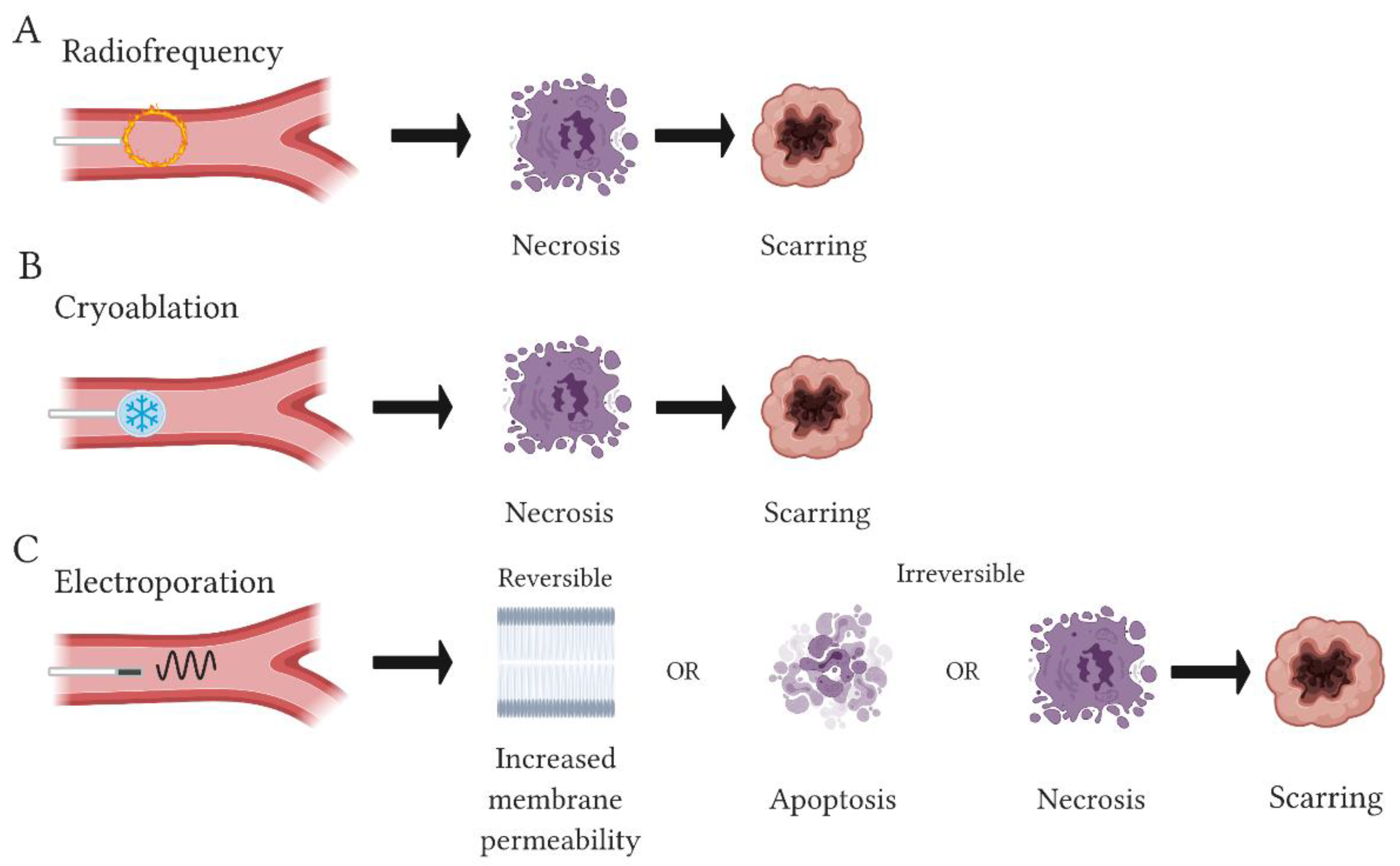
2. Current Ablation Approaches for Treating Arrhythmia
2.1. Hyperthermal Techniques
2.2. Hypothermal or Cryoablation Techniques
2.3. Challenges with Current Ablative Approaches
3. Electroporation as an Ablative Approach
3.1. Pre-Clinical Evaluation of IRE, towards Optimization of Parameters for Clinical Use
3.2. Controlled Lesion Formation with IRE In Vivo
3.3. Advantages and Disadvantages of EP
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heart Disease Facts|cdc.gov. Available online: https://www.cdc.gov/heartdisease/facts.htm (accessed on 9 June 2020).
- Zager, Y.; Kain, D.; Landa, N.; Leor, J.; Maor, E. Optimization of irreversible electroporation protocols for in-vivo myocardial decellularization. PLoS ONE 2016, 11. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Goff, R.; Patana-anake, P.; Iaizzo, P.A.; Bischof, J. Irreversible electroporation of cardiovascular cells and tissues. J. Med. Devices Trans. ASME 2013, 7. [Google Scholar] [CrossRef]
- Avazzadeh, S.; McBride, S.; O’Brien, B.; Coffey, K.; Elahi, A.; O’Halloran, M.; Soo, A.; Quinlan, L.R. Ganglionated Plexi Ablation for the Treatment of Atrial Fibrillation. J. Clin. Med. 2020, 9, 3081. [Google Scholar] [CrossRef]
- Holmes, D.R.; Valeti, U.S.; Nishimura, R.A. Alcohol septal ablation for hypertrophic cardiomyopathy: Indications and technique. Catheter. Cardiovasc. Interv. 2005, 66, 375–389. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Groves, B.M.; Schwartz, L.; Smith, K.M.; Wang, A.; Bach, R.G.; Nielsen, C.; Leya, F.; Buergler, J.M.; Rowe, S.K.; et al. Alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy: A multicenter north american registry. J. Am. Coll. Cardiol. 2011, 58, 2322–2328. [Google Scholar] [CrossRef]
- Wei, C.; Qian, P.; Tedrow, U.; Mak, R.; Zei, P.C. Non-invasive stereotactic radioablation: A new option for the treatment of ventricular arrhythmias. Arrhythmia Electrophysiol. Rev. 2019, 8, 285–293. [Google Scholar] [CrossRef]
- Chiu, M.H.; Mitchell, L.B.; Ploquin, N.; Faruqi, S.; Kuriachan, V.P.; Chiu, M. Review of Stereotactic Arrhythmia Radioablation Therapy for Cardiac Tachydysrhythmias. CJC Open 2020, 3, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Lavee, J.; Onik, G.; Rubinsky, B. A Novel Nonthermal Energy Source for Surgical Epicardial Atrial Ablation: Irreversible Electroporation Single cell manipulation and electroporation View project Isochoric Freezing: A new frontier for cryopreservation View project. Heart Surg. Forum 2007, 10, 96–101. [Google Scholar] [CrossRef]
- Njeim, M.; Bogun, F. Selecting the appropriate ablation strategy: The role of endocardial and/or epicardial access. Arrhythmia Electrophysiol. Rev. 2015, 4, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Davalos, R.V.; Mir, L.M.; Rubinsky, B. Tissue ablation with irreversible electroporation. Ann. Biomed. Eng. 2005, 33, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Sohara, H.; Satake, S.; Takeda, H.; Yamaguchi, Y.; Toyama, H.; Kumagai, K.; Kuwahara, T.; Takahashi, A.; Ohe, T. Radiofrequency hot balloon catheter ablation for the treatment of atrial fibrillation: A 3-center study in Japan. J. Arrhythmia 2013, 29, 20–27. [Google Scholar] [CrossRef]
- Okumura, Y.; Kolasa, M.W.; Johnson, S.B.; Bunch, T.J.; Henz, B.D.; O’brien, C.J.; Miller, D.V.; Packer, D.L. Mechanism of Tissue Heating During High Intensity Focused Ultrasound Pulmonary Vein Isolation: Implications for Atrial Fibrillation Ablation Efficacy and Phrenic Nerve Protection. J. Cardiovasc. Electrophysiol. 2008, 19, 945–951. [Google Scholar] [CrossRef]
- Zhou, Y.-F. High intensity focused ultrasound in clinical tumor ablation. World J. Clin. Oncol. 2011, 2, 8. [Google Scholar] [CrossRef]
- Borchert, B.; Lawrenz, T.; Hansky, B.; Stellbrink, C. Lethal atrioesophageal fistula after pulmonary vein isolation using high-intensity focused ultrasound (HIFU). Heart Rhythm 2008, 5, 145–148. [Google Scholar] [CrossRef]
- Nakagawa, H.; Seres, K.A.; Jackman, W.M. Limitations of esophageal temperature-monitoring to prevent esophageal injury during atrial fibrillation ablation. Circ. Arrhythm. Electrophysiol. 2008, 1, 150–152. [Google Scholar] [CrossRef][Green Version]
- Prasertwitayakij, N.; Vodnala, D.; Pridjian, A.K.; Thakur, R.K. Esophageal injury after atrial fibrillation ablation with an epicardial high-intensity focused ultrasound device. J. Interv. Card. Electrophysiol. 2011, 31, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Bessiere, F.; N’djin, W.A.; Colas, E.C.; Chavrier, F.; Greillier, P.; Chapelon, J.Y.; Chevalier, P.; Lafon, C. Ultrasound-Guided Transesophageal High-Intensity Focused Ultrasound Cardiac Ablation in a Beating Heart: A Pilot Feasibility Study in Pigs. Ultrasound Med. Biol. 2016, 42, 1848–1861. [Google Scholar] [CrossRef]
- Figueras i Ventura, R.M.; Mǎrgulescu, A.D.; Benito, E.M.; Alarcón, F.; Enomoto, N.; Prat-Gonzalez, S.; Perea, R.J.; Borràs, R.; Chipa, F.; Arbelo, E.; et al. Postprocedural LGE-CMR comparison of laser and radiofrequency ablation lesions after pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 2018, 29, 1065–1072. [Google Scholar] [CrossRef]
- Joseph, J.P.; Rajappan, K. Radiofrequency ablation of cardiac arrhythmias: Past, present and future. An. Int. J. Med. 2012, 105, 303–314. [Google Scholar] [CrossRef] [PubMed]
- Wojtaszczyk, A.; Caluori, G.; Pešl, M.; Melajova, K.; Stárek, Z. Irreversible electroporation ablation for atrial fibrillation. J. Cardiovasc. Electrophysiol. 2018, 29, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg Center at Oregon Health & Science University. Radiofrequency Ablation for Atrial Fibrillation: A Guide for Adults. In Comparative Effectiveness Review Summary Guides for Consumers; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2005. [Google Scholar]
- Wazni, O.M.; Marrouche, N.F.; Martin, D.O.; Verma, A.; Bhargava, M.; Saliba, W.; Bash, D.; Schweikert, R.; Brachmann, J.; Gunther, J.; et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: A randomized trial. J. Am. Med. Assoc. 2005, 293, 2634–2640. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, K.; Nakagawa, H.; Shah, D.C.; Lambert, H.; Leo, G.; Aeby, N.; Ikeda, A.; Pitha, J.V.; Sharma, T.; Lazzara, R.; et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ. Arrhythm. Electrophysiol. 2008, 1, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Cosman, E.R.; Dolensky, J.R.; Hoffman, R.A. Factors that affect radiofrequency heat lesion size. Pain Med. 2014, 15, 2020–2036. [Google Scholar] [CrossRef]
- Sweet, W.H.; Mark, V.H. Unipolar anodal electrolytic lesions in the brain of man and cat: Report of Five Human Cases with Electrically Produced Bulbar or Mesencephalic Tractotomies. Arch. Neurol. Psychiatry 1953, 70, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Wittkampf, F.H.M.; Nakagawa, H. RF catheter ablation: Lessons on lesions. PACE-Pacing Clin. Electrophysiol. 2006, 29, 1285–1297. [Google Scholar] [CrossRef]
- Katritsis, D.G.; Giazitzoglou, E.; Zografos, T.; Pokushalov, E.; Po, S.S.; Camm, A.J. Rapid pulmonary vein isolation combined with autonomic ganglia modification: A randomized study. Heart Rhythm 2011, 8, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Budera, P.; Osmancik, P.; Herman, D.; Zdarska, J.; Talavera, D.; Mala, A.; Prochazkova, R.; Straka, Z. Midterm outcomes of two-staged hybrid ablation of persistent and long-standing persistent atrial fibrillation using the versapolar epicardial surgical device and subsequent catheter ablation. J. Interv. Card. Electrophysiol. 2017, 50, 187–194. [Google Scholar] [CrossRef]
- Friedman, P.L. Catheter Cryoablation of Cardiac Arrhythmias. Curr. Opin. Cardiol. 2005, 20, 48–54. [Google Scholar] [PubMed]
- Hunter, R.J.; Baker, V.; Finlay, M.C.; Duncan, E.R.; Lovell, M.J.; Tayebjee, M.H.; Ullah, W.; Siddiqui, M.S.; Mclean, A.; Richmond, L.; et al. Point-by-Point Radiofrequency Ablation Versus the Cryoballoon or a Novel Combined Approach: A Randomized Trial Comparing 3 Methods of Pulmonary Vein Isolation for Paroxysmal Atrial Fibrillation (The Cryo Versus RF Trial). J. Cardiovasc. Electrophysiol. 2015, 26, 1307–1314. [Google Scholar] [CrossRef]
- Wasserlauf, J.; Pelchovitz, D.J.; Rhyner, J.; Verma, N.; Bohn, M.; Li, Z.; Arora, R.; Chicos, A.B.; Goldberger, J.J.; Kim, S.S.; et al. Cryoballoon versus Radiofrequency Catheter Ablation for Paroxysmal Atrial Fibrillation. Pacing Clin. Electrophysiol. 2015, 38, 483–489. [Google Scholar] [CrossRef]
- Bárta, J.; Brát, R. Assessment of the effect of left atrial cryoablation enhanced by ganglionated plexi ablation in the treatment of atrial fibrillation in patients undergoing open heart surgery. J. Cardiothorac. Surg. 2017, 12, 69. [Google Scholar] [CrossRef] [PubMed]
- Boveda, S. Cryoablation for Atrial Fibrillation: A Useful Technique beyond Paroxysmal Forms of Arrhythmia? Rev. Española Cardiol. 2017, 70, 236–238. [Google Scholar] [CrossRef]
- Kim, K.M.; Chung, S.; Kim, S.Y.; Kim, D.J.; Kim, J.S.; Lim, C.; Park, K.H. Comparison of radiofrequency ablation and cryoablation for the recovery of atrial contractility and survival. Korean J. Thorac. Cardiovasc. Surg. 2018, 51, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Kuck, K.-H.; Albenque, J.-P.; Chun, K.R.J.; Fürnkranz, A.; Busch, M.; Elvan, A.; Schlüter, M.; Braegelmann, K.M.; Kueffer, F.J.; Hemingway, L.; et al. Repeat Ablation for Atrial Fibrillation Recurrence Post Cryoballoon or Radiofrequency Ablation in the FIRE AND ICE Trial. Circ. Arrhythmia Electrophysiol. 2019, 12. [Google Scholar] [CrossRef]
- Strickberger, S.A.; Hummel, J.; Gallagher, M.; Hasse, C.; Man, K.C.; Williamson, B.; Vorperian, V.R.; Kalbfleisch, S.J.; Morady, F.; Langberg, J.J. Effect of accessory pathway location on the efficiency of heating during radiofrequency catheter ablation. Am. Heart J. 1995, 129, 54–58. [Google Scholar] [CrossRef]
- Safaei, N.; Montazerghaem, H.; Azarfarin, R.; Alizadehasl, A.; Alikhah, H. Radiofrequency ablation for treatment of atrial fibrillation. BioImpacts 2011, 1, 171–177. [Google Scholar] [CrossRef]
- Koruth, J.S.; Dukkipati, S.; Gangireddy, S.; McCarthy, J.; Spencer, D.; Weinberg, A.D.; Miller, M.A.; D’Avila, A.; Reddy, V.Y. Occurrence of steam pops during irrigated RF ablation: Novel insights from Microwave Radiometry. J. Cardiovasc. Electrophysiol. 2013, 24, 1271–1277. [Google Scholar] [CrossRef] [PubMed]
- Hirano, M.; Yamamoto, H.; Hasebe, Y.; Fukuda, K.; Morosawa, S.; Amamizu, H.; Ohyama, K.; Uzuka, H.; Takayama, K.; Shimokawa, H. Development of a Novel Shock Wave Catheter Ablation system—A Validation Study in Pigs in Vivo. EP Eur. 2018, 20, 1856–1865. [Google Scholar] [CrossRef]
- Tokuda, M.; Kojodjojo, P.; Epstein, L.M.; Koplan, B.A.; Michaud, G.F.; Tedrow, U.B.; Stevenson, W.G.; John, R.M. Outcomes of Cardiac Perforation Complicating Catheter Ablation of Ventricular Arrhythmias. Circ. Arrhythmia Electrophysiol. 2011, 4, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Kaszala, K.; Ellenbogen, K.A. Biophysics of the second-generation cryoballoon: Cryobiology of the big freeze. Circ. Arrhythmia Electrophysiol. 2015, 8, 15–17. [Google Scholar] [CrossRef]
- Du Pre, B.C.; van Driel, V.J.; van Wessel, H.; Loh, P.; Doevendans, P.A.; Goldschmeding, R.; Wittkampf, F.H.; Vink, A. Minimal Coronary Artery Damage by Myocardial Electroporation Ablation. EP Eur. 2013, 15, 144–149. [Google Scholar] [CrossRef]
- Neven, K.; van Driel, V.; van Wessel, H.; van Es, R.; du Pré, B.; Doevendans, P.A.; Wittkampf, F. Safety and feasibility of closed chest epicardial catheter ablation using electroporation. Circ. Arrhythm. Electrophysiol. 2014, 7, 913–919. [Google Scholar] [CrossRef]
- Stewart, M.T.; Haines, D.E.; Verma, A.; Kirchhof, N.; Barka, N.; Grassl, E.; Howard, B. Intracardiac pulsed field ablation: Proof of feasibility in a chronic porcine model. Heart Rhythm 2019, 16, 754–764. [Google Scholar] [CrossRef] [PubMed]
- Coltorti, F.; Bardy, G.H.; Reichenbach, D.; Greene, H.L.; Thomas, R.; Breazeale, D.G.; Alferness, C.; Ivey, T.D. Catheter-mediated electrical ablation of the posterior septum via the coronary sinus: Electrophysiologic and histologic observations in dogs. Circulation 1985, 72, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, H.; Jackman, M. Electroporation (revival of direct current ablation) new approach for increasing epicardial ablation safety in close proximity to a coronary artery. Circ. Arrhythmia Electrophysiol. 2014, 7, 779–780. [Google Scholar] [CrossRef]
- Ahsan, A.J.; Cunningham, D.; Rowland, E.; Rickards, A.F. Catheter Ablation without Fulguration: Design and Performance of a New System. Pacing Clin. Electrophysiol. 1989, 12, 1557–1561. [Google Scholar] [CrossRef]
- Wittkampf, F.H.M.; van Es, R.; Neven, K. Electroporation and its Relevance for Cardiac Catheter Ablation. JACC Clin. Electrophysiol. 2018, 4, 977–986. [Google Scholar] [CrossRef]
- Tung, L.; Tovar, O.; Neunlist, M.; Jain, S.K.; O’neill, R.J. Effects of Strong Electrical Shock on Cardiac Muscle Tissue. Ann. N. Y. Acad. Sci. 1994, 720, 160–175. [Google Scholar] [CrossRef] [PubMed]
- Sugrue, A.; Vaidya, V.R.; Livia, C.; Padmanabhan, D.; Abudan, A.; Isath, A.; Witt, T.; DeSimone, C.V.; Stalboerger, P.; Kapa, S.; et al. Feasibility of selective cardiac ventricular electroporation. PLoS ONE 2020, 15. [Google Scholar] [CrossRef]
- Maor, E.; Ivorra, A.; Mitchell, J.J.; Rubinsky, B. Vascular smooth muscle cells ablation with endovascular nonthermal irreversible electroporation. J. Vasc. Interv. Radiol. 2010, 21, 1708–1715. [Google Scholar] [CrossRef]
- Wittkampf, F.H.; Van Driel, V.J.; Van Wessel, H.; Vink, A.; Hof, I.E.; GrÜndeman, P.F.; Hauer, R.N.; Loh, P. Feasibility of electroporation for the creation of pulmonary vein ostial lesions. J. Cardiovasc. Electrophysiol. 2011, 22, 302–309. [Google Scholar] [CrossRef]
- Frandsen, S.K.; Gissel, H.; Hojman, P.; Tramm, T.; Eriksen, J.; Gehl, J. Direct therapeutic applications of calcium electroporation to effectively induce tumor necrosis. Cancer Res. 2012, 72, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Weaver, J.C. Electroporation of cells and tissues. IEEE Trans. Plasma Sci. 2000, 28, 24–33. [Google Scholar] [CrossRef]
- Neumann, E.; Rosenheck, K. Permeability changes induced by electric impulses in vesicular membranes. J. Membr. Biol. 1972, 10, 279–290. [Google Scholar] [CrossRef]
- Semenov, I.; Zemlin, C.; Pakhomova, O.N.; Xiao, S.; Pakhomov, A.G. Diffuse, non-polar electropermeabilization and reduced propidium uptake distinguish the effect of nanosecond electric pulses. Biochim. Biophys. Acta Biomembr. 2015, 1848, 2118–2125. [Google Scholar] [CrossRef][Green Version]
- Al-Khadra, A.; Nikolski, V.; Efimov, I.R. The role of electroporation in defibrillation. Circ. Res. 2000, 87, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Stewart, M.T.; Cheek, D.S.; Francischelli, D.E.; Kirchhof, N. Cardiac ablation via electroporation. In Proceedings of the 31st Annual International Conference of the IEEE Engineering in Medicine and Biology Society: Engineering the Future of Biomedicine, EMBC 2009, Minneapollis, MN, USA, 3–6 September 2009; Volume 2009, pp. 3381–3384. [Google Scholar]
- Vižintin, A.; Vidmar, J.; Ščančar, J.; Miklavčič, D. Effect of interphase and interpulse delay in high-frequency irreversible electroporation pulses on cell survival, membrane permeabilization and electrode material release. Bioelectrochemistry 2020, 134, 107523. [Google Scholar] [CrossRef]
- Andrei, G.; Pakhomov, D.; Miklavcic, M.S.M. Advanced Electroporation Techniques in Biology and Medicine. Available online: https://books.google.ie/books?id=sTHNBQAAQBAJ&pg=PA160&lpg=PA160&dq=U.+Zimmermann,+Ed.,+The+Effects+of+High+Intensity+Electric+Field+Pulses+on+Eukaryotic+Cell+Membranes:+Fundamentals+and+Applications.+Boca+Raton,+FL:+CRC,+1996&source=bl&ots=WvQ3rRMyfg&sig (accessed on 27 March 2020).
- Kotnik, T.; Pucihar, G.; Reberšek, M.; Miklavčič, D.; Mir, L.M. Role of pulse shape in cell membrane electropermeabilization. Biochim. Biophys. Acta Biomembr. 2003, 1614, 193–200. [Google Scholar] [CrossRef]
- Stankevic, V.; Simonis, P.; Zurauskiene, N.; Stirke, A.; Dervinis, A.; Bleizgys, V.; Kersulis, S.; Balevicius, S. Compact square-wave pulse electroporator with controlled electroporation efficiency and cell viability. Symmetry 2020, 12, 412. [Google Scholar] [CrossRef]
- Sano, M.B.; Fan, R.E.; Xing, L. Asymmetric Waveforms Decrease Lethal Thresholds in High Frequency Irreversible Electroporation Therapies. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef]
- Polajžer, T.; Dermol-Cerne, J.; Erne, J.; Reberšek, M.; O’connor, R.; Miklavčič, D. Cancellation effect is present in high-frequency reversible and irreversible electroporation. Bioelectrochemistry 2019. [Google Scholar] [CrossRef]
- Caluori, G.; Odehnalova, E.; Jadczyk, T.; Pesl, M.; Pavlova, I.; Valikova, L.; Holzinger, S.; Novotna, V.; Rotrekl, V.; Hampl, A.; et al. AC Pulsed Field Ablation Is Feasible and Safe in Atrial and Ventricular Settings: A Proof-of-Concept Chronic Animal Study. Front. Bioeng. Biotechnol. 2020, 8, 1374. [Google Scholar] [CrossRef]
- Van Es, R.; Konings, M.K.; Du Pré, B.C.; Neven, K.; Van Wessel, H.; Van Driel, V.J.H.M.; Westra, A.H.; Doevendans, P.A.F.; Wittkampf, F.H.M. High-frequency irreversible electroporation for cardiac ablation using an asymmetrical waveform. Biomed. Eng. Online 2019, 18. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Koruth, J.; Jais, P.; Petru, J.; Timko, F.; Skalsky, I.; Hebeler, R.; Labrousse, L.; Barandon, L.; Kralovec, S.; et al. Ablation of Atrial Fibrillation With Pulsed Electric Fields: An Ultra-Rapid, Tissue-Selective Modality for Cardiac Ablation. JACC Clin. Electrophysiol. 2018, 4, 987–995. [Google Scholar] [CrossRef] [PubMed]
- Cemazar, M.; Sersa, G.; Frey, W.; Miklavcic, D.; Teissié, J. Recommendations and requirements for reporting on applications of electric pulse delivery for electroporation of biological samples. Bioelectrochemistry 2018, 122, 69–76. [Google Scholar] [CrossRef]
- Semenov, I.; Grigoryev, S.; Neuber, J.U.; Zemlin, C.W.; Pakhomova, O.N.; Casciola, M.; Pakhomov, A.G. Excitation and injury of adult ventricular cardiomyocytes by nano- to millisecond electric shocks. Sci. Rep. 2018, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Azarov, J.E.; Semenov, I.; Casciola, M.; Pakhomov, A.G. Excitation of murine cardiac myocytes by nanosecond pulsed electric field. J. Cardiovasc. Electrophysiol. 2019, 30, 392–401. [Google Scholar] [CrossRef]
- Xie, F.; Varghese, F.; Pakhomov, A.G.; Semenov, I.; Xiao, S.; Philpott, J.; Zemlin, C. Ablation of Myocardial Tissue With Nanosecond Pulsed Electric Fields. PLoS ONE 2015, 10, e0144833. [Google Scholar] [CrossRef]
- Krassowska, W. Effects of Electroporation on Transmembrane Potential Induced by Defibrillation Shocks. Pacing Clin. Electrophysiol. 1995, 18, 1644–1660. [Google Scholar] [CrossRef] [PubMed]
- Kaminska, I.; Kotulska, M.; Stecka, A.; Saczko, J.; Drag-Zalesinska, M.; Wysocka, T.; Choromanska, A.; Skolucka, N.; Nowicki, R.; Marczak, J.; et al. Electroporation-induced changes in normal immature rat myoblasts (H9C2). Gen. Physiol. Biophys. 2012, 31, 19–25. [Google Scholar] [CrossRef]
- Hunter, D.W.; Kostecki, G.; Fish, J.M.; Jensen, J.A.; Tandri, H. In Vitro Cell Selectivity of Reversible and Irreversible Electroporation in Cardiac Tissue. Circ. Arrhythmia Electrophysiol. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhan, D.; Naksuk, N.; Killu, A.K.; Kapa, S.; Witt, C.; Sugrue, A.; Desimon, C.V.; Madhavan, M.; de Groot, J.R.; O’Brien, B.; et al. Electroporation of epicardial autonomic ganglia: Safety and efficacy in medium-term canine models. J. Cardiovasc. Electrophysiol. 2019, 30, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Koruth, J.; Kuroki, K.; Iwasawa, J.; Enomoto, Y.; Viswanathan, R.; Brose, R.; Buck, E.D.; Speltz, M.; Dukkipati, S.R.; Reddy, V.Y. Preclinical Evaluation of Pulsed Field Ablation: Electrophysiological and Histological Assessment of Thoracic Vein Isolation. Circ. Arrhythmia Electrophysiol. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Neuzil, P.; Koruth, J.S.; Petru, J.; Funosako, M.; Cochet, H.; Sediva, L.; Chovanec, M.; Dukkipati, S.R.; Jais, P. Pulsed Field Ablation for Pulmonary Vein Isolation in Atrial Fibrillation. J. Am. Coll. Cardiol. 2019. [Google Scholar] [CrossRef]
- Mercadal, B.; Arena, C.B.; Davalos, R.V.; Ivorra, A. Avoiding nerve stimulation in irreversible electroporation: A numerical modeling study. Phys. Med. Biol. 2017, 62, 8060–8079. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Anter, E.; Rackauskas, G.; Peichl, P.; Koruth, J.S.; Petru, J.; Funasako, M.; Minami, K.; Natale, A.; Jaïs, P.; et al. A Lattice-Tip Focal Ablation Catheter that Toggles Between Radiofrequency and Pulsed Field Energy to Treat Atrial Fibrillation: A First-in-Human Trial. Circ. Arrhythmia Electrophysiol. 2020, 13. [Google Scholar] [CrossRef]
- Loh, P.; Van Es, R.; Groen, M.H.A.; Neven, K.; Kassenberg, W.; Wittkampf, F.H.M.; Doevendans, P.A. Pulmonary vein isolation with single pulse irreversible electroporation: A first in human study in 10 patients with atrial fibrillation. Circ. Arrhythmia Electrophysiol. 2020, 13, 1083–1091. [Google Scholar] [CrossRef]
- Deodhar, A.; Dickfeld, T.; Single, G.W.; Hamilton, W.C.; Thornton, R.H.; Sofocleous, C.T.; Maybody, M.; Gónen, M.; Rubinsky, B.; Solomon, S.B. Irreversible electroporation near the heart: Ventricular arrhythmias can be prevented with ECG synchronization. Am. J. Roentgenol. 2011, 196, W330. [Google Scholar] [CrossRef]
- Kim, S.C.; Vasanji, A.; Efimov, I.R.; Cheng, Y. Spatial distribution and extent of electroporation by strong internal shock in intact structurally normal and chronically infarcted rabbit hearts. J. Cardiovasc. Electrophysiol. 2008, 19, 1080–1089. [Google Scholar] [CrossRef]
- Xie, F.; Zemlin, C.W. Effect of Twisted Fiber Anisotropy in Cardiac Tissue on Ablation with Pulsed Electric Fields. PLoS ONE 2016, 11, e0152262. [Google Scholar] [CrossRef]
- Neven, K.; Van Driel, V.; Van Wessel, H.; Van Es, R.; Doevendans, P.A.; Wittkampf, F. Myocardial Lesion Size after Epicardial Electroporation Catheter Ablation After Subxiphoid Puncture. Circ. Arrhythmia Electrophysiol. 2014, 7, 728–733. [Google Scholar] [CrossRef]
- Neven, K.; Van Driel, V.; Van Wessel, H.; Van Es, R.; Doevendans, P.A.; Wittkampf, F. Epicardial linear electroporation ablation and lesion size. Hear. Rhythm 2014, 11, 1465–1470. [Google Scholar] [CrossRef] [PubMed]
- Wittkampf, F.H.M.; Van Driel, V.J.; Van Wessel, H.; Neven, K.G.E.J.; Gründeman, P.F.; Vink, A.; Loh, P.; Doevendans, P.A. Myocardial lesion depth with circular electroporation ablation. Circ. Arrhythmia Electrophysiol. 2012, 5, 581–586. [Google Scholar] [CrossRef]
- Desimone, C.V.; Ebrille, E.; Syed, F.F.; Mikell, S.B.; Suddendorf, S.H.; Wahnschaffe, D.; Ladewig, D.J.; Gilles, E.J.; Danielsen, A.J.; Holmes, D.R.; et al. Novel balloon catheter device with pacing, ablating, electroporation, and drug-eluting capabilities for atrial fibrillation treatment - Preliminary efficacy and safety studies in a canine model. Transl. Res. 2014, 164, 508–514. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Driel, V.J.H.M.; Neven, K.G.E.J.; Van Wessel, H.; Du Pré, B.C.; Vink, A.; Doevendans, P.A.F.M.; Wittkampf, F.H.M. Pulmonary vein stenosis after catheter ablation electroporation versus radiofrequency. Circ. Arrhythmia Electrophysiol. 2014, 7, 734–738. [Google Scholar] [CrossRef] [PubMed]
- Kuroki, K.; Whang, W.; Eggert, C.; Lam, J.; Leavitt, J.; Kawamura, I.; Reddy, A.; Morrow, B.; Schneider, C.; Petru, J.; et al. Ostial Dimensional Changes After Pulmonary Vein Isolation: Pulsed Field Ablation vs Radiofrequency Ablation. Hear. Rhythm 2020. [Google Scholar] [CrossRef]
- Madhavan, M.; Venkatachalam, K.L.; Swale, M.J.; Desimone, C.V.; Gard, J.J.; Johnson, S.B.; Suddendorf, S.H.; Mikell, S.B.; Ladewig, D.J.; Nosbush, T.G.; et al. Novel Percutaneous Epicardial Autonomic Modulation in the Canine for Atrial Fibrillation: Results of an Efficacy and Safety Study. PACE - Pacing Clin. Electrophysiol. 2016, 39, 407–417. [Google Scholar] [CrossRef]
- Van Driel, V.J.H.M.; Neven, K.; Van Wessel, H.; Vink, A.; Doevendans, P.A.F.M.; Wittkampf, F.H.M. Low vulnerability of the right phrenic nerve to electroporation ablation. Hear. Rhythm 2015, 12, 1838–1844. [Google Scholar] [CrossRef]
- Witt, C.M.; Sugrue, A.; Padmanabhan, D.; Vaidya, V.; Gruba, S.; Rohl, J.; DeSimone, C.V.; Killu, A.M.; Naksuk, N.; Pederson, J.; et al. Intrapulmonary vein ablation without stenosis: A novel balloon-based direct current electroporation approach. J. Am. Heart Assoc. 2018, 7. [Google Scholar] [CrossRef]
- Neven, K.; Van Es, R.; Van Driel, V.; Van Wessel, H.; Fidder, H.; Vink, A.; Doevendans, P.; Wittkampf, F. Acute and Long-Term Effects of Full-Power Electroporation Ablation Directly on the Porcine Esophagus. Circ. Arrhythmia Electrophysiol. 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Jin, E.S.; Wang, P.J. Cryoballoon ablation for atrial fibrillation: A comprehensive review and practice guide. Korean Circ. J. 2018, 48, 114–123. [Google Scholar] [CrossRef]
- Macle, L.; Weerasooriya, R.; Jais, P.; Scavee, C.; Raybaud, F.; Choi, K.-J.; Hocini, M.; Clementy, J.; Haissaguerre, M. Radiation Exposure During Radiofrequency Catheter Ablation for Atrial Fibrillation. Pacing Clin. Electrophysiol. 2003, 26, 288–291. [Google Scholar] [CrossRef]
- Es, R.; Groen, M.H.A.; Stehouwer, M.; Doevendans, P.A.; Wittkampf, F.H.M.; Neven, K. In vitro analysis of the origin and characteristics of gaseous microemboli during catheter electroporation ablation. J. Cardiovasc. Electrophysiol. 2019, 30, 2071–2079. [Google Scholar] [CrossRef] [PubMed]
- Groen, M.H.A.; van Es, R.; van Klarenbosch, B.R.; Stehouwer, M.; Loh, P.; Doevendans, P.A.; Wittkampf, F.H.; Neven, K. In vivo analysis of the origin and characteristics of gaseous microemboli during catheter-mediated irreversible electroporation. EP Eur. 2021, 23, 139–146. [Google Scholar] [CrossRef]
- Neven, K.; Füting, A.; Byrd, I.; Heil, R.W.; Fish, J.M.; Feeney, D.A.; Donskoy, E.; Jensen, J.A. Absence of (sub-)acute cerebral events or lesions after electroporation ablation in the left-sided canine heart. Hear. Rhythm 2021, 18, 1004–1011. [Google Scholar] [CrossRef]
- Bradley, C.J.; Haines, D.E. Pulsed field ablation for pulmonary vein isolation in the treatment of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2020, 31, 2136–2147. [Google Scholar] [CrossRef]
- Kambakamba, P.; Bonvini, J.M.; Glenck, M.; Castrezana López, L.; Pfammatter, T.; Clavien, P.A.; DeOliveira, M.L. Intraoperative adverse events during irreversible electroporation–a call for caution. Am. J. Surg. 2016, 212, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Koruth, J.S.; Kuroki, K.; Iwasaw1, J.; Viswanathan, R.; Richard; Brose; Buck, E.D.; Donskoy, E.; Dukkipati, S.R.; Reddy, V.Y. Endocardial Ventricular Pulsed Field Ablation: A Proof-Of-Concept Preclinical Evaluation. EP Eur. 2020, 22, 434–439. [Google Scholar] [CrossRef]
- Livia, C.; Sugrue, A.; Witt, T.; Polkinghorne, M.D.; Maor, E.; Kapa, S.; Lehmann, H.I.; DeSimone, C.V.; Behfar, A.; Asirvatham, S.J.; et al. Elimination of Purkinje Fibers by Electroporation Reduces Ventricular Fibrillation Vulnerability. J. Am. Heart Assoc. 2018, 7, e009070. [Google Scholar] [CrossRef]

| Ref. | Subject | Follow-Up | Energy | Parameters | Monophasic/Biphasic Waveform | Monopolar/Bipolar Electrode Configuration | Reported Outcome |
|---|---|---|---|---|---|---|---|
| In Vitro | |||||||
| [3] | HL-1 cell line | N/A | 200 V; 1000 V/cm | PD- 50 µs, F- 10 Hz, PF- 10, 50, 99 pulses. | Not specified | Not specified | (1) IRE is effective for creating lesions on HL-1 cell line. |
| [73] | Cardiac strand-2D model | N/A | 0.4–0.5 V; 25 V/cm | PD- 5 ms | Monophasic | Not specified | (1) Cardiac fibre exposed to a strong stimulus responds by developing pores in the first layer of cells immediately adjacent to the electrode. (2) IRE stops the growth of the macroscopic transmembrane potential, it does not affect intra- and extracellular potentials in the bulk of the tissue. |
| In Vivo Animal | |||||||
| [2] | Rat | 1 month | 50, 250, 500 V | PD- 70 vs. 100 μs, F- 1, 2, 3, 4 Hz, PF- 10 V’s 20. | Not specified | Not specified | (1) Longer pulse duration (100 μs vs. 70 μs) is associated with larger volume reduction. (2) More pulses (20 vs. 10) are associated with larger volume reduction. (3) Pulse voltage (500 V vs. 250 V, 50 V) has an important effect on tissue damage. (4) Lower pulse frequency (10 Hz vs 20 Hz) is correlated with harsher tissue damage. |
| [9] | Porcine | 24 h | 1500–2000 V | PD- 100 μs, PF- 8, 16, 32. | Not specified | Not specified | (1) Lesions were mean 0.9 cm in depth. (2) Complete transmural destruction of atrial tissue at the site of the electrode application. (3) No local temperature change and with demonstration of electrical isolation. |
| [40] | Porcine | 7 days | Not specified | F- 1 Hz, PF- 35 | Not specified | Bipolar | (1) Unlike RF lesions, SW lesions showed only mild denaturation and little disruption of endocardium. (2) Lesion depth from SW correlated to amount of energy used. (3) SWCA lesions showed transient inflammatory responses followed by accelerated healing process with preserved myocardial blood flow. |
| [43] | Porcine | 3 weeks | Not specified | Not specified | Monophasic | Not specified | (1) Mean depths ranged from 2.9 + 1.2 mm–6.5 + 2.7 mm. (2) 32% of lesions were transmural. (3) Coronary arteries do not develop significant stenosis within 3 weeks after epicardial IRE. |
| [44] | Porcine | 3 months | Not specified | PF- 3. | Monophasic | Not specified | (1) Mean value of the median lesion depths was 6.4 ± 2.6 mm. (2) 31% of lesions were transmural. (3) Apart from short-lasting (<30 min) coronary spasm, no long-term luminal narrowing was seen. |
| [45] | Porcine | 2 weeks | 500 V | PD- 90 µs, PF- 60. | Biphasic | Bipolar | (1) PFA lesions comparable to RFA lesions and had no collateral damage. |
| [51] | Canine | 29 days | 750 V | PD- 20 µs, F- 30–500 Hz, PF-10. | Not specified | Bipolar | (1) PEF can safely ablate Purkinje fibres. (2) Minimal collateral damage to myocardium. |
| [53] | Porcine | 3 weeks | Not specified | PF- 4. | Monophasic | Bipolar | (1) Low energy IRE is safe and efficient in creating lesions on the PV ostia. |
| [57] | Rat | N/A | 20 kV; 36 kV/cm | PD- 10 ns, F- 2 Hz, PF- 3. | Not specified | Not specified | (1) nsEP produces smaller pore size and reduced non-polar distribution of electro-pores over the cell body. (2) At near threshold intensities, both nsEPo and msEPo triggered Ca2+ transients. |
| [58] | Rabbit | N/A | 50–500 V | F- 1–2 kHz, PF- 6–10. | Monophasic | Bipolar | (1) IRE thresholds were 229 ± 81 and 318 ± 84 V for the endocardium and the epicardium, respectively. (2) Selective transient impairment of electrical activity in endocardial bundles is caused by IRE. (3) IRE might transiently reduce myocardial vulnerability to arrhythmias. |
| [59] | Ovine | N/A | Not specified | PD- 100–400 µs, F- 1–5 Hz, PF- 10–40 pulses. | Not specified | Bipolar | (1) Lesions were well demarcated from the unaffected tissue. (2) The induced inflammatory reaction within these acute ablations was minimal. |
| [67] | Porcine | 3 weeks | 600 V | PD- 2 ms, F- 10 kHz, PF- 10. | Biphasic | Not specified | (1) Demonstrated the feasibility of a novel asymmetrical high frequency (aHF) waveform for IRE. (2) The aHF waveform led to significantly deeper lesions than the symmetrical HF waveform. (3) Both methods showed lesions of more than 4 mm deep. |
| [70] | Murine, rat, porcine | N/A | 100 V; 12.2 kV/cm | PD- 400 ns, PF- 20. | Not specified | Not specified | (1) Stimulation by 200 ns shocks can elicit Ca2+ transients. (2) Shortest shocks cause the least damage and their threshold energy is minimal. (3) Orientation of cardiomyocytes with respect for electric field does not affect threshold for ns shocks. |
| [71] | Murine | N/A | Not specified | PD- 200 µs | Not specified | Not specified | (1) 200 ns stimuli induced action potentials. (2) nsPEF caused Ca2+ entry, associated with a slow sustained depolarisation. |
| [72] | Rabbit | N/A | 200 V | PD- 350 ns, F- 1, 3 Hz, PF- 20, 6. | Not specified | Monopolar | (1) Nonconducting lesions created in less than 2 s with nsPEF application per site and minimal heating (<0.2 °C) of the tissue. (2) Lesion was smoother and more uniform throughout the wall in comparison to RF lesions. |
| [76] | Canine | 113 ± 7 days | 1000 V | PD- 100 µs, PF- 10 | Not specified | Bipolar | (1) Cardiac GP permanently damaged using DC for IRE. (2) Preservation of atrial myocardial architecture and absence of inflammatory reaction and fibrosis. |
| [77] | Porcine | 63 ± 3.3 days | 800–1800 V | Not specified | Monophasic | Bipolar | (1) Both waveforms created confluent myocardial lesions. (2) Biphasic PFA was more durable than monophasic PFA and radiofrequency ablation lesions. |
| [83] | Rabbit | 4 weeks | 300 V | Not specified | Monophasic | Bipolar | (1) Shock-induced IRE was spatially dependent on the location and dimension of the active region of the shock electrode. (2) The surviving anterior epicardial layers in the infarcted region were more susceptible to IRE. |
| [84] | Rabbit | Not specified | 200 V; 3 kV/cm | PD- 350 ns, F- 3 Hz, PF- 6. | Not specified | Not specified | (1) High anisotropy ratio substantially affects the ablation outcome, low anisotropy ratio does not. |
| [85] | Porcine | 3 months | Not specified | Not specified | Monophasic | Not specified | (1) Lesion size, depth and width corresponds to magnitude of energy used. (2) Initial spasm of coronary vasculature was noted, but this did not persist and was not recorded at follow-up. |
| [86] | Porcine | 3 months | Not specified | Not specified | Not specified | Not specified | (1) Mean depth of the 30 J, 100 J and 300 J lesions was 3.2 ± 0.7, 6.3 ± 1.8 and 8.0 ± 1.5 mm, respectively. (2) Mean width of the 30 J, 100 J, and 300 J lesions was 10.1 ± 0.8, 15.1 ± 1.5 and 17.1 ± 1.3 mm, respectively. (3) No luminal arterial narrowing was observed after 3 months. |
| [87] | Porcine | 3 weeks | 950–2150 V | PD- <10 ms, PF- 4. | Monophasic | Monopolar | (1) 200 J applications yielded median lesion depth of 5.2 ± 1.2 mm. (2) No signs of tissue heating. (3) Lesion would be sufficient for inducing PVI. |
| [88] | Canine | N/A | Not specified | PD- 60–300 s, F- 7 kHz. | Not specified | Not specified | (1) Device can successfully deliver both RF and IRE energy. (2) Addition of porous configuration on balloon can aid in enhancing drug delivery. |
| [89] | Porcine | 3 months | Not specified | Not specified | Monophasic | Not specified | (1) IRE ablation: PV ostial diameter decreased 11 ± 10% directly after ablation but had increased 19 ± 11% after 3 months. (2) RF ablation: PV ostial diameter decreased 23 ± 15% directly after ablation and remained 7 ± 17% smaller after 3 months than pre-ablation diameter, despite a 21 ± 7% increase in heart size during aging from 6 to 9 months. |
| [91] | Canine | N/A | Not specified | F- 1 Hz. | Not specified | Bipolar | (1) No evidence of collateral damage to surrounding structures. (2) Ventricular arrhythmias can occur during DC application and are more likely with use of higher energy. |
| [93] | Canine | 27 days | 2 kV/cm | PD- 100 µs, PF- 100. | Not specified | Bipolar | (1) No significant PV stenosis or oesophageal injury occurred. |
| [3] | Porcine | N/A | 500 V; 1200 V/cm | PD- 50 µs, F- 10 Hz, PF- 50. | Not specified | Not specified | (1) IREis effective for creating lesions on PV tissue. |
| [102] | Porcine | 35 days | 2200 V | PD- <60 s | Biphasic | Bipolar | (1) Fibrous tissue homogeneously replaced myocytes. (2) When present, nerve fascicles and vasculature were preserved within surrounding fibrosis. |
| [103] | Canine ex vivo | N/A | 750–2500 V; 250–833 V/cm | PD- 200 µs, F- 1 Hz, PF- 10 | Biphasic | Not specified | (1) Delivery of IRE energy significantly reduced the window of vulnerability to ventricular arrhythmia. (2) No evidence of myocardial damage. |
| Ref. | Follow-Up | Energy | Parameters | Monophasic/Biphasic Waveform | Monopolar/Bipolar Electrode Configuration | Reported Outcome Reported Outcome |
|---|---|---|---|---|---|---|
| [68] | N/A | 900–2500 V | PF- 3. | Not specified | Bipolar | (1) PEF is a safe method for treating AF both endocardially and epicardially. (2) No incidences of atrial or ventricular arrythmia during procedure. (3) No collateral damage or PV stenosis recorded. |
| [78] | 4 months | 900–1000 V | Not specified | Monophasic | Bipolar | (1) Acute PVI achieved in 100% of patients using 6.4 ± 2.3 applications. (2) No injury to oesophagus or phrenic nerve. |
| [80] | 12 months | 0.011 ± 0.006 mV | PD- 3–5 s | Biphasic | Bipolar | (1) No adverse effects recorded related to PEF. (2) Freedom from AF was 94.4 ± 3.2%. |
| [81] | N/A | 2154 ± 59 V | Not specified | Monophasic | Monopolar | (1) Acute bidirectional electrical PVI achieved in all 40 PVs. (2) No PV reconnections occurred during waiting period (30 min). |
| [90] | 3 months | 900–1000 V | Not specified | Monophasic | Monopolar and Bipolar | (1) No change (0%) in PV diameter and no stenosis in PFA patients, but reduction in diameter in 32.5% of patients who received RFA. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McBride, S.; Avazzadeh, S.; Wheatley, A.M.; O’Brien, B.; Coffey, K.; Elahi, A.; O’Halloran, M.; Quinlan, L.R. Ablation Modalities for Therapeutic Intervention in Arrhythmia-Related Cardiovascular Disease: Focus on Electroporation. J. Clin. Med. 2021, 10, 2657. https://doi.org/10.3390/jcm10122657
McBride S, Avazzadeh S, Wheatley AM, O’Brien B, Coffey K, Elahi A, O’Halloran M, Quinlan LR. Ablation Modalities for Therapeutic Intervention in Arrhythmia-Related Cardiovascular Disease: Focus on Electroporation. Journal of Clinical Medicine. 2021; 10(12):2657. https://doi.org/10.3390/jcm10122657
Chicago/Turabian StyleMcBride, Shauna, Sahar Avazzadeh, Antony M. Wheatley, Barry O’Brien, Ken Coffey, Adnan Elahi, Martin O’Halloran, and Leo R. Quinlan. 2021. "Ablation Modalities for Therapeutic Intervention in Arrhythmia-Related Cardiovascular Disease: Focus on Electroporation" Journal of Clinical Medicine 10, no. 12: 2657. https://doi.org/10.3390/jcm10122657
APA StyleMcBride, S., Avazzadeh, S., Wheatley, A. M., O’Brien, B., Coffey, K., Elahi, A., O’Halloran, M., & Quinlan, L. R. (2021). Ablation Modalities for Therapeutic Intervention in Arrhythmia-Related Cardiovascular Disease: Focus on Electroporation. Journal of Clinical Medicine, 10(12), 2657. https://doi.org/10.3390/jcm10122657






