Blood Pressure and Transient Postoperative Neurologic Deterioration, Following Superficial Temporal-to-Middle Cerebral Artery Anastomosis in Adult Patients with Moyamoya Disease: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Ethical Statement
2.2. Study Subjects and Data Collection
2.3. Surgical and Anaesthetic Procedures
2.4. Brain Perfusion Diamox SPECT Image Analysis
2.5. Outcome Assessment: TND
2.6. Confounders
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, T.; Oh, C.W.; Kwon, O.K.; Hwang, G.; Kim, J.E.; Kang, H.S.; Cho, W.S.; Bang, J.S. Stroke prevention by direct revascularization for patients with adult-onset moyamoya disease presenting with ischemia. J. Neurosurg. 2016, 124, 1788–1793. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, M.; Kaneta, T.; Mugikura, S.; Shimizu, H.; Tominaga, T. Temporary neurologic deterioration due to cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with adult-onset moyamoya disease. Surg. Neurol. 2007, 67, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Oh, C.W.; Kwon, O.K.; Park, S.Q.; Kim, S.E.; Kim, Y.K. Transient hyperperfusion after superficial temporal artery/middle cerebral artery bypass surgery as a possible cause of postoperative transient neurological deterioration. Cereb. Dis. 2008, 25, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Ohue, S.; Kumon, Y.; Kohno, K.; Watanabe, H.; Iwata, S.; Ohnishi, T. Postoperative temporary neurological deficits in adults with moyamoya disease. Surg. Neurol. 2008, 69, 281–286; discussion 286–287. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.J.; Kim, J.S.; Hong, S.C. Prognostic factors associated with perioperative ischemic complications in adult-onset moyamoya disease. Acta Neurochir. 2010, 152, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, M.; Mugikura, S.; Kaneta, T.; Shimizu, H.; Tominaga, T. Incidence and risk factors for symptomatic cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with moyamoya disease. Surg. Neurol. 2009, 71, 442–447. [Google Scholar] [CrossRef]
- Hwang, J.W.; Yang, H.M.; Lee, H.; Lee, H.K.; Jeon, Y.T.; Kim, J.E.; Lim, Y.J.; Park, H.P. Predictive factors of symptomatic cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in adult patients with moyamoya disease. Br. J. Anaesth. 2013, 110, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.W.; Kim, N.; Kang, J.; Park, S.H.; Kim, W.J.; Ko, Y.; Park, J.H.; Lee, J.S.; Lee, J.; Yang, M.H.; et al. Blood pressure variability and the development of early neurological deterioration following acute ischemic stroke. J. Hypertens. 2015, 33, 2099–2106. [Google Scholar] [CrossRef]
- Parray, T.; Martin, T.W.; Siddiqui, S. Moyamoya disease: A review of the disease and anesthetic management. J. Neurosurg. Anesthesiol. 2011, 23, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Iwama, T.; Hashimoto, N.; Yonekawa, Y. The relevance of hemodynamic factors to perioperative ischemic complications in childhood moyamoya disease. Neurosurgery 1996, 38, 1120–1125; discussion 1125–1126. [Google Scholar]
- So, Y.; Lee, H.Y.; Kim, S.K.; Lee, J.S.; Wang, K.C.; Cho, B.K.; Kang, E.; Lee, D.S. Prediction of the clinical outcome of pediatric moyamoya disease with postoperative basal/acetazolamide stress brain perfusion SPECT after revascularization surgery. Stroke 2005, 36, 1485–1489. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhao, Y.; Zhao, M.; Cao, P.; Liu, X.; Ren, H.; Zhang, D.; Zhang, Y.; Wang, R.; Zhao, J. High variance of intraoperative blood pressure predicts early cerebral infarction after revascularization surgery in patients with Moyamoya disease. Neurosurg. Rev. 2020, 43, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Oh, C.W.; Bang, J.S.; Kim, J.E.; Cho, W.S. Moyamoya Disease: Treatment and Outcomes. J. Stroke 2016, 18, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Lee, S.H.; Roh, J.K. Changing ischaemic lesion patterns in adult moyamoya disease. J. Neurol. Neurosurg. Psychiatry 2009, 80, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.Y.; Chung, A.M.; Farkouh, M.E.; van Diepen, S.; Weinberger, J.; Bourke, M.; Ruel, M. Defining an Intraoperative Hypotension Threshold in Association with Stroke in Cardiac Surgery. Anesthesiology 2018, 129, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Bijker, J.B.; Persoon, S.; Peelen, L.M.; Moons, K.G.; Kalkman, C.J.; Kappelle, L.J.; van Klei, W.A. Intraoperative hypotension and perioperative ischemic stroke after general surgery: A nested case-control study. Anesthesiology 2012, 116, 658–664. [Google Scholar] [CrossRef]
- Mukerji, N.; Cook, D.J.; Steinberg, G.K. Is local hypoperfusion the reason for transient neurological deficits after STA-MCA bypass for moyamoya disease? J. Neurosurg. 2015, 122, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Hillis, A.E.; Ulatowski, J.A.; Barker, P.B.; Torbey, M.; Ziai, W.; Beauchamp, N.J.; Oh, S.; Wityk, R.J. A pilot randomized trial of induced blood pressure elevation: Effects on function and focal perfusion in acute and subacute stroke. Cerebrovasc. Dis. 2003, 16, 236–246. [Google Scholar] [CrossRef]
- Kim, D.Y.; Son, J.P.; Yeon, J.Y.; Kim, G.M.; Kim, J.S.; Hong, S.C.; Bang, O.Y. Infarct Pattern and Collateral Status in Adult Moyamoya Disease: A Multimodal Magnetic Resonance Imaging Study. Stroke 2017, 48, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, M.; Niizuma, K.; Inoue, T.; Sato, K.; Endo, H.; Shimizu, H.; Tominaga, T. Minocycline prevents focal neurological deterioration due to cerebral hyperperfusion after extracranial-intracranial bypass for moyamoya disease. Neurosurgery 2014, 74, 163–170; discussion 170. [Google Scholar] [CrossRef]
- Zhao, M.; Deng, X.; Zhang, D.; Wang, S.; Zhang, Y.; Wang, R.; Zhao, J. Risk factors for and outcomes of postoperative complications in adult patients with moyamoya disease. J. Neurosurg. 2018, 1–12. [Google Scholar] [CrossRef]

| Variable | <Q1 (<120.2) (n = 57) | Q1–Q2 (120.2–125) (n = 57) | Q2–Q3 (125–133) (n = 57) | ≥Q4 (≥133) (n = 57) | p-Value * |
|---|---|---|---|---|---|
| Age (year) | 38.9 (13.2) | 39.0 (12.4) | 41.5 (12.0) | 41.7 (12.2) | 0.471 |
| Gender: Male | 20 (23) | 25 (29) | 17 (20) | 24 (28) | 0.382 |
| BMI (kg/m2) | 25.2 (4.2) | 24.8 (4.0) | 26.6 (4.3) | 26 (4.3) | 0.129 |
| Comorbidities | |||||
| Previous Stroke | 9 (32) | 5 (18) | 6 (21) | 8 (29) | 0.653 |
| Hypertension | 16 (21) | 17 (23) | 22 (29) | 20 (27) | 0.613 |
| Diabete Mellitus | 6 (18) | 12 (35) | 9 (26) | 7 (21) | 0.407 |
| Smoking | 13 (27) | 16 (33) | 8 (16) | 12 (24) | 0.333 |
| Coronary Artery Disease | 0 | 0 | 2 (100) | 0 | 0.247 § |
| Thyroid Disease | 4 (29) | 4 (29) | 3 (21) | 3 (21) | 1.000 § |
| Clinical Characteristics | |||||
| Anesthesia Time (min) | 479 (91) | 474 (100) | 499 (102) | 492 (95) | 0.487 |
| Operation Time (min) | 408 (86) | 406 (108) | 423 (99) | 424 (93) | 0.642 |
| Preop Hb (g/dL) | 13.8 (1.6) | 13.8 (1.7) | 13.5 (1.6) | 13.5 (1.6) | 0.451 |
| Preop WBC (103/uL) | 7.0 (1.9) | 7.0 (1.7) | 6.7 (1.4) | 6.7 (1.5) | 0.477 |
| LOS (day) | 13.4 (4.7) | 12.5 (4.4) | 12.4 (4.4) | 14.8 (7.5) | 0.07 |
| Operation site (Rt/Lt) | 31 (24)/26 (27) | 33 (25)/24 (24) | 34 (26)/23 (23) | 32 (25)/25 (26) | 0.949 |
| Cerebral Perfusion status | 8 (30.8) | 5 (19.2) | 4 (15.4) | 9 (34.6) | 0.399 |
| Preop mean SBP | 113.8 (13.2) | 118.5 (15.1) | 127.5 (16.2) | 128.5 (15.2) | 0.128 |
| ISBP Quartiles | TND (+) (n = 66) | TND (−) (n = 162) | p Value * | Crude OR (95% CI) § | Adjusted OR (95% CI) † |
|---|---|---|---|---|---|
| <Q1 (<120.2) | 25 (43.9%) | 32 (56.1%) | 0.005 | 4.78 (1.92, 11.91) | 5.50 (1.96, 15.46) |
| Q1–Q2 (120.2–125) | 18 (31.6%) | 39 (68.4%) | 2.83 (1.11, 7.19) | 3.24 (1.16, 9.05) | |
| Q2–Q3 (125–133) | 8 (14.0%) | 49 (86.0%) | reference | reference | |
| ≥Q3 (≥133) | 15 (26.3%) | 42 (73.7%) | 2.19 (0.84, 5.67) | 1.39 (0.48, 4.04) |
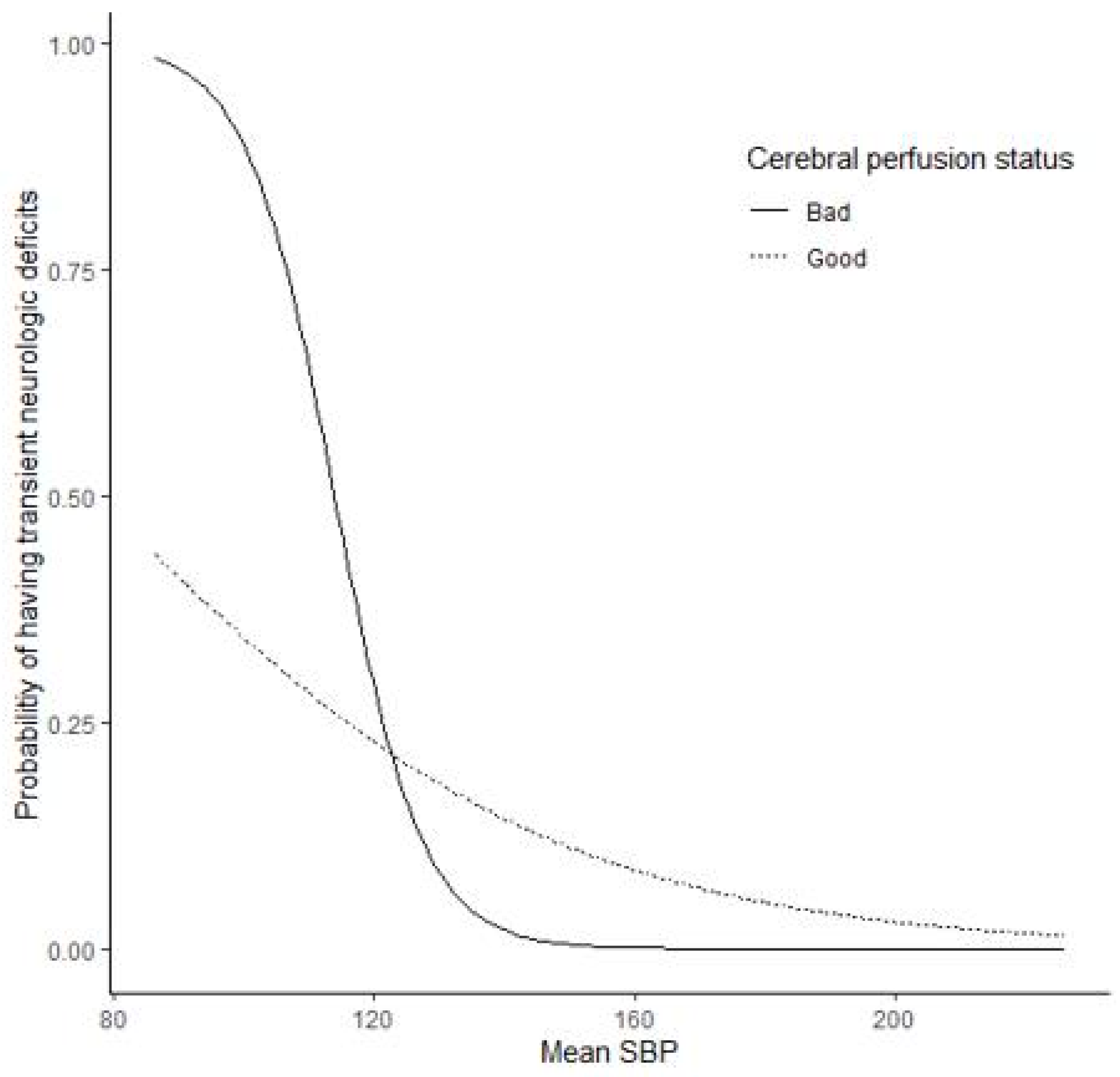
| Model | Linear | Nonlinear without Interaction | Nonlinear with Interaction | |||
|---|---|---|---|---|---|---|
| Parameter | Estimate | p-Value | Estimate | p-Value | Estimate | p-Value |
| ISBP mean | −0.0883 | 0.026 | – | – | – | – |
| Cerebral perfusion status | 7.3463 | 0.124 | −0.0558 | 0.833 | −0.2131 | 0.512 |
| ISBP mean * cerebral perfusion status | −0.0599 | 0.123 | – | – | – | – |
| Centered ISBP mean | −0.0470 | 0.01 | −0.0918 | 0.018 | ||
| Quadratic term of mean | 0.0009 | 0.355 | 0.0009 | 0.38 | ||
| Centered ISBP mean * cerebral perfusion status | – | – | −0.0538 | 0.157 | ||
| Age | −0.0280 | 0.052 | −0.0288 | 0.046 | −0.0281 | 0.053 |
| Preoperative SBP mean | 0.0149 | 0.003 | 0.0439 | 0.003 | 0.0414 | 0.006 |
| Operation time | −0.00126 | 0.484 | −0.0012 | 0.505 | −0.0012 | 0.502 |
| Operation site: left side | 0.3907 | 0.022 | 0.3809 | 0.025 | 0.3849 | 0.024 |
| Previous stroke | 0.0450 | 0.855 | 0.0787 | 0.749 | 0.0589 | 0.812 |
| Preoperative Hemoglobin | 0.3866 | 0.005 | 0.3805 | 0.006 | 0.3730 | 0.007 |
| Postoperative Hemoglobin | −0.2010 | 0.156 | −0.1746 | 0.219 | −0.1774 | 0.213 |
| Length of hospital stay | 0.1089 | 0.002 | 0.0966 | 0.004 | 0.1021 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, T.-K.; Kim, J.-H.; Lee, H.-Y.; Kim, S.-E.; Kim, T.-K.; Bang, J.-S.; Han, M.-K.; Oh, C.-W.; Bae, H.-J.; Jeon, Y.-T. Blood Pressure and Transient Postoperative Neurologic Deterioration, Following Superficial Temporal-to-Middle Cerebral Artery Anastomosis in Adult Patients with Moyamoya Disease: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 2567. https://doi.org/10.3390/jcm10122567
Oh T-K, Kim J-H, Lee H-Y, Kim S-E, Kim T-K, Bang J-S, Han M-K, Oh C-W, Bae H-J, Jeon Y-T. Blood Pressure and Transient Postoperative Neurologic Deterioration, Following Superficial Temporal-to-Middle Cerebral Artery Anastomosis in Adult Patients with Moyamoya Disease: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(12):2567. https://doi.org/10.3390/jcm10122567
Chicago/Turabian StyleOh, Tak-Kyu, Ji-Hyeon Kim, Ho-Young Lee, Seong-Eun Kim, Tac-Keun Kim, Jae-Seung Bang, Moon-Ku Han, Chang-Wan Oh, Hee-Joon Bae, and Young-Tae Jeon. 2021. "Blood Pressure and Transient Postoperative Neurologic Deterioration, Following Superficial Temporal-to-Middle Cerebral Artery Anastomosis in Adult Patients with Moyamoya Disease: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 12: 2567. https://doi.org/10.3390/jcm10122567
APA StyleOh, T.-K., Kim, J.-H., Lee, H.-Y., Kim, S.-E., Kim, T.-K., Bang, J.-S., Han, M.-K., Oh, C.-W., Bae, H.-J., & Jeon, Y.-T. (2021). Blood Pressure and Transient Postoperative Neurologic Deterioration, Following Superficial Temporal-to-Middle Cerebral Artery Anastomosis in Adult Patients with Moyamoya Disease: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(12), 2567. https://doi.org/10.3390/jcm10122567






