Changes in Cerebral Blood Flow after Erenumab Treatment in Good and Non-Responders—A Pilot Study of Migraine Patients
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Drellia, K.; Kokoti, L.; Deligianni, C.I.; Papadopoulos, D.; Mitsikostas, D.D. Anti-CGRP monoclonal antibodies for migraine prevention: A systematic review and likelihood to help or harm analysis. Cephalalgia 2021, 41, 333102421989601. [Google Scholar] [CrossRef]
- Ashina, M.; Goadsby, P.J.; Reuter, U.; Silberstein, S.; Dodick, D.; Rippon, G.A.; Klatt, J.; Xue, F.; Chia, V.; Zhang, F.; et al. Long-term safety and tolerability of erenumab: Three-plus year results from a five-year open-label extension study in episodic migraine. Cephalalgia 2019, 39, 1455–1464. [Google Scholar] [CrossRef]
- Ashina, M.; Tepper, S.; Brandes, J.L.; Reuter, U.; Boudreau, G.; Dolezil, D.; Cheng, S.; Zhang, F.; Lenz, R.; Klatt, J.; et al. Efficacy and safety of erenumab (AMG334) in chronic migraine patients with prior preventive treatment failure: A subgroup analysis of a randomized, double-blind, placebo-controlled study. Cephalalgia 2018, 38, 1611–1621. [Google Scholar] [CrossRef] [PubMed]
- Kudrow, D.; Pascual, J.; Winner, P.K.; Dodick, D.W.; Tepper, S.J.; Reuter, U.; Hong, F.; Klatt, J.; Zhang, F.; Cheng, S.; et al. Vascular safety of erenumab for migraine prevention. Neurology 2020, 94, e497–e510. [Google Scholar] [CrossRef] [Green Version]
- Messlinger, K.; MaassenVanDenBrink, A. Cardio- and cerebrovascular safety of erenumab, a monoclonal antibody targeting CGRP receptors—Important studies on human isolated arteries. Cephalalgia 2019, 39, 1731–1734. [Google Scholar] [CrossRef]
- Altamura, C.; Viticchi, G.; Fallacara, A.; Costa, C.M.; Brunelli, N.; Fiori, C.; Silvestrini, M.; Vernieri, F. Erenumab does not alter cerebral hemodynamics and endothelial function in migraine without aura. Cephalalgia 2021, 41, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Coccia, A.; Lapucci, C.; Di Poggio, M.B.; Grazzini, M.; Inglese, M.; Finocchi, C. A longitudinal clinical and MRI evaluation of the treatment with erenumab. Neurol. Sci. 2020, 41, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson, L.; Haanes, K.A.; Kronvall, E.; Xu, C.; Snellman, J.; Edvinsson, L. Erenumab (AMG 334), a monoclonal antagonist antibody against the canonical CGRP receptor, does not impair vasodilatory or contractile responses to other vasoactive agents in human isolated cranial arteries. Cephalalgia 2019, 39, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Beltrán, E.; Labastida-Ramírez, A.; Haanes, K.A.; Bogaerdt, A.V.D.; Bogers, A.J.; Dirven, C.; Danser, A.J.; Xu, C.; Snellman, J.; MaassenVanDenBrink, A. Characterisation of vasodilatory responses in the presence of the CGRP receptor antibody erenumab in human isolated arteries. Cephalalgia 2019, 39, 1735–1744. [Google Scholar] [CrossRef] [PubMed]
- Ziegeler, C.; Mehnert, J.; Asmussen, K.; May, A. Central effects of erenumab in migraine patients: An event-related functional imaging study. Neurology 2020, 95, e2794–e2802. [Google Scholar] [CrossRef] [PubMed]
- Sorond, F.A.; Hollenberg, N.K.; Panych, L.P.; Fisher, N.D. Brain blood flow and velocity: Correlations between magnetic resonance imaging and transcranial Doppler sonography. J. Ultrasound Med. 2010, 29, 1017–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Aaslid, R.; Markwalder, T.-M.; Nornes, H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J. Neurosurg. 1982, 57, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Lennihan, L.; Petty, G.W.; Fink, M.E.; Solomon, R.A.; Mohr, J.P. Transcranial Doppler detection of anterior cerebral artery vasospasm. J. Neurol. Neurosurg. Psychiatry 1993, 56, 906–909. [Google Scholar] [CrossRef]
- Faraci, F.M.; Heistad, D.D. Regulation of large cerebral arteries and cerebral microvascular pressure. Circ. Res. 1990, 66, 8–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faraci, F.M.; Heistad, D.D. Regulation of cerebral blood vessels by humoral and endothelium-dependent mechanisms. Update on humoral regulation of vascular tone. Hypertension 1991, 17, 917–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edvinsson, L.; Sams, A.; Jansen-Olesen, I.; Tajti, J.; Kane, S.A.; Rutledge, R.Z.; Koblan, K.S.; Hill, R.G.; Longmore, J. Characterisation of the effects of a non-peptide CGRP receptor antagonist in SK-N-MC cells and isolated human cerebral arteries. Eur. J. Pharmacol. 2001, 415, 39–44. [Google Scholar] [CrossRef]
- Lassen, L.H.; Jacobsen, V.B.; Haderslev, P.A.; Sperling, B.; Iversen, H.K.; Olesen, J.; Tfelt-Hansen, P. Involvement of calcitonin gene-related peptide in migraine: Regional cerebral blood flow and blood flow velocity in migraine patients. J. Headache Pain 2008, 9, 151–157. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.J.; Chu, M.K.; Choi, H.; Choi, H.A.; Lee, C.; Chung, C.-S. Longitudinal changes in cerebral blood flow velocities in different clinical courses of migraine. Cephalalgia 2016, 37, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Bellner, J.; Romner, B.; Reinstrup, P.; Kristiansson, K.-A.; Ryding, E.; Brandt, L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg. Neurol. 2004, 62, 45–51. [Google Scholar] [CrossRef]
- Czosnyka, M.; Richards, H.K.; Whitehouse, H.E.; Pickard, J.D. Relationship between transcranial Doppler-determined pulsatility index and cerebrovascular resistance: An experimental study. J. Neurosurg. 1996, 84, 79–84. [Google Scholar] [CrossRef] [Green Version]
- de Riva, N.; Budohoski, K.P.; Smielewski, P.; Kasprowicz, M.; Zweifel, C.; Steiner, L.A.; Reinhard, M.; Fábregas, N.; Pickard, J.D.; Czosnyka, M. Transcranial Doppler pulsatility index: What it is and what it isn’t. Neurocrit. Care 2012, 17, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Okazawa, H.; Tsuchida, T.; Pagani, M.; Mori, T.; Kobayashi, M.; Tanaka, F.; Yonekura, Y. Effects of 5-HT1B/1D Receptor Agonist Rizatriptan on Cerebral Blood Flow and Blood Volume in Normal Circulation. Br. J. Pharmacol. 2005, 26, 92–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savrun, F.K.; Goksan, B.; Savrun, M.; Sahin, R.; Sahin, S. Cerebral blood flow changes in patients with probable medication-overuse headache. Funct. Neurol. 2008, 23, 83–86. [Google Scholar]
- Kassab, M.Y.; Majid, A.; Bakhtar, O.; Farooq, M.U.; Patel, K.; Bednarczyk, E.M. Transcranial Doppler measurements in migraine and nitroglycerin headache. J. Headache Pain 2007, 8, 289–293. [Google Scholar] [CrossRef] [Green Version]
- Levine, S.R.; Welch, K.M.A.; Ewing, J.R.; Robertson, W.M. Asymmetric Cerebral Blood Flow Patterns in Migraine. Cephalalgia 1987, 7, 245–248. [Google Scholar] [CrossRef]
- Zaproudina, N.; Teplov, V.; Nippolainen, E.; Lipponen, J.A.; Kamshilin, A.A.; Närhi, M.; Karjalainen, P.A.; Giniatullin, R. Asynchronicity of Facial Blood Perfusion in Migraine. PLoS ONE 2013, 8, e80189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michels, L.; Villanueva, J.; O’Gorman, R.; Muthuraman, M.; Koirala, N.; Büchler, R.; Gantenbein, A.R.; Sandor, P.S.; Luechinger, R.; Kollias, S.; et al. Interictal Hyperperfusion in the Higher Visual Cortex in Patients with Episodic Migraine. Headache J. Head Face Pain 2019, 59, 1808–1820. [Google Scholar] [CrossRef]
- Coppola, G.; Di Renzo, A.; Tinelli, E.; Iacovelli, E.; Lepre, C.; Di Lorenzo, C.; Di Lorenzo, G.; Di Lenola, D.; Parisi, V.; Serrao, M.; et al. Evidence for brain morphometric changes during the migraine cycle: A magnetic resonance-based morphometry study. Cephalalgia 2014, 35, 783–791. [Google Scholar] [CrossRef]
- Coppola, G.; Tinelli, E.; Lepre, C.; Iacovelli, E.; Di Lorenzo, G.; Serrao, M.; Pauri, F.; Fiermonte, G.; Bianco, F.; Pierelli, F. Dynamic changes in thalamic microstructure of migraine without aura patients: A diffusion tensor magnetic resonance imaging study. Eur. J. Neurol. 2013, 21, 287-e13. [Google Scholar] [CrossRef]
- Mirza, M.; Tutuş, A.; Erdoğan, F.; Kula, M.; Tomar, A.; Silov, G.; Köseoğlu, E. Interictal SPECT with Tc-99m HMPAO studies in migraine patients. Acta Neurol. Belg. 1998, 98, 190–194. [Google Scholar] [PubMed]
- Giani, L.; Lovati, C.; Corno, S.; Laganà, M.M.; Baglio, F.; Mariani, C. Cerebral blood flow in migraine without aura: ASL-MRI case control study. Neurol. Sci. 2019, 40, 183–184. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Good Responders ≥50% RR | Non-Responders <50% RR | p-Value |
|---|---|---|---|
| N = 19 | N = 11 | ||
| Age (mean ± SD) | 42.05 ± 13.18 | 37.91 ± 5.70 | 0.24 |
| BMI, kg/m2 | 23.6 | 22.5 | 0.314 |
| Duration of migraine (years)(mean ± SD) | 21.84 ± 10.51 | 19.27 ± 7.24 | 0.44 |
| Type of migraine: Episodic Chronic | 7 (36.84) 12 (63.16) | 3 (27.27) 8 (72.73) | 0.7 |
| Migraine with aura, n (%) | 3 (15.79) | 2 (18.18) | 1 |
| MOH, n (%) | 8 (42.11) | 6 (54.55) | 0.78 |
| MMD-Baseline MMD-Post-treatment | 11.26 ± 5.19 3.21 ± 2.86 | 11.91 ± 4.11 9.91 ± 5.05 | 0.56 0.001 |
| p-value | 0.0001 | 0.009 | |
| MHD-Baseline MHD-Post-treatment | 18.32 ± 7.93 5.74 ± 4.76 | 20.18 ± 7.24 15.73 ± 6.51 | 0.52 0.0004 |
| p-value | 0.00005 | 0.006 | |
| AMD-Baseline AMD-Post-treatment | 13.42 ± 6.27 3.68 ± 2.98 | 16.18 ± 7.48 10.18 ± 4.73 | 0.32 0.001 |
| p-value | 0.0001 | 0.02 | |
| NRS-Baseline NRS-Post-treatment | 8.32 ± 1.06 5.37 ± 2.93 | 8.55 ± 1.21 7.36 ± 1.12 | 0.61 0.02 |
| p-value | 0.0004 | 0.01 | |
| HIT-6-Baseline HIT-6-Post-treatment | 62.53 ± 5.31 46.63 ± 8.39 | 63.45 ± 5.01 59.00 ± 7.14 | 0.81 0.0009 |
| p-value | 0.0001 | 0.04 | |
| Mood disorders, n (%) | 5 (26.32) | 5 (45.45) | 0.43 |
| Thyroid disease, n (%) | 4 (21.05) | 3 (27.27) | 1 |
| Oral contraceptives, n (%) | 3 (15.79) | 2 (18.18) | 1 |
| Acute medication used Triptans Codeine Ibuprofen or paracetamol | 9 (70.9) 7 (36.8) 1 (5.3) | 6 (54.5) 2 (18.18) 3 (27.3) | 0.82 0.06 0.11 |
| Parameters | Good Responders (≥50% RR) | Non-Responders (<50%RR) | p-Value |
|---|---|---|---|
| N = 19 | N = 11 | ||
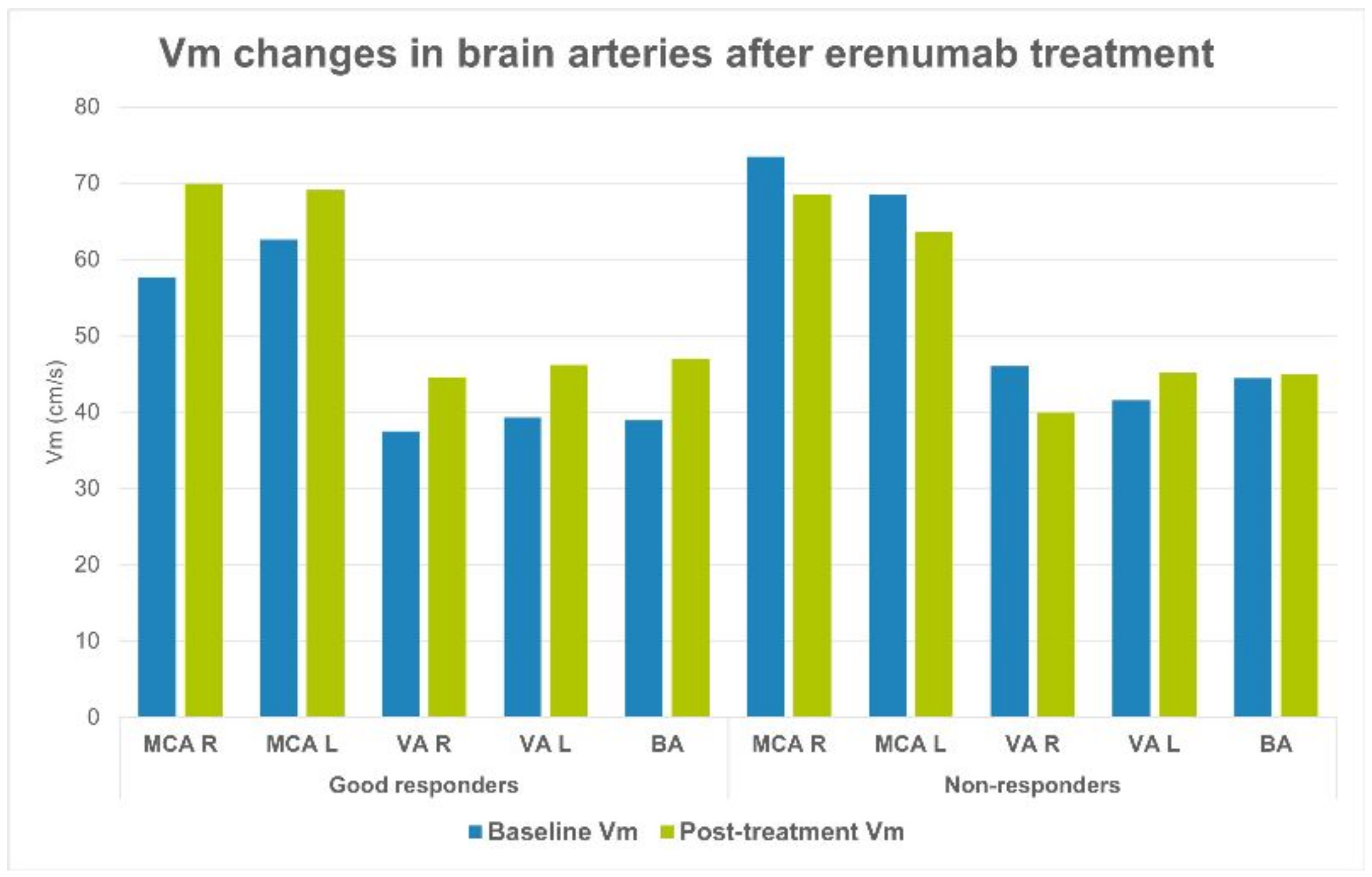
| Baseline Vm, MCA R (cm/s) | 57.8 | 73.45 | 0.008 |
| Post-treatment Vm, MCA R (cm/s) | 69.93 | 68.56 | 0.83 |
| p-value | 0.0003 | 0.18 | |
| Baseline Vm, MCA L (cm/s) | 662.6 | 68.5 | 0.17 |
| Post-treatment Vm, MCA L (cm/s) | 69.11 | 63.67 | 0.11 |
| p-value | 0.016 | 0.27 | |
| Baseline Vm, VA R | 37.5 | 46.05 | 0.02 |
| Post-treatment Vm, VA R | 44.61 | 39.94 | 0.17 |
| p-value | 0.02 | 0.07 | |
| Baseline Vm, VA L | 39.3 | 41.58 | 0.55 |
| Post-treatment Vm, VA L | 46.21 | 45.16 | 0.82 |
| p-value | 0.002 | 0.4 | |
| Baseline Vm, BA | 38.93 | 44.42 | 0.04 |
| Post-treatment Vm, BA | 47 | 44.95 | 0.3 |
| p-value | 0.0002 | 0.85 |
| Parameters | Good Responders (≥50% RR) | Non-Responders (<50%RR) | p-Value |
|---|---|---|---|
| N = 19 | N = 11 | ||
| Baseline PI, MCA R | 0.78 | 0.84 | 0.18 |
| Post-treatment PI, MCA R | 0.5 | 0.87 | 0.62 |
| p-value | 0.32 | 0.35 | |
| Baseline PI, MCA L | 0.78 | 0.78 | 0.48 |
| Post-treatment PI, MCA L | 0.8 | 0.87 | 0.17 |
| p-value | 0.58 | 0.04 | |
| Baseline PI, VA R | 0.81 | 0.76 | 0.31 |
| Post-treatment PI, VA R | 0.83 | 0.86 | 0.64 |
| p-value | 0.64 | 0.002 | |
| Baseline PI, VA L | 0.78 | 0.76 | 0.73 |
| Post-treatment PI, VA L | 0.78 | 0.82 | 0.46 |
| p-value | 0.81 | 0.23 | |
| Baseline PI, BA | 0.8 | 0.76 | 0.41 |
| Post-treatment PI, BA | 0.85 | 0.88 | 0.58 |
| p-value | 0.17 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowaczewska, M.; Straburzyński, M.; Meder, G.; Kaźmierczak, W. Changes in Cerebral Blood Flow after Erenumab Treatment in Good and Non-Responders—A Pilot Study of Migraine Patients. J. Clin. Med. 2021, 10, 2523. https://doi.org/10.3390/jcm10112523
Nowaczewska M, Straburzyński M, Meder G, Kaźmierczak W. Changes in Cerebral Blood Flow after Erenumab Treatment in Good and Non-Responders—A Pilot Study of Migraine Patients. Journal of Clinical Medicine. 2021; 10(11):2523. https://doi.org/10.3390/jcm10112523
Chicago/Turabian StyleNowaczewska, Magdalena, Marcin Straburzyński, Grzegorz Meder, and Wojciech Kaźmierczak. 2021. "Changes in Cerebral Blood Flow after Erenumab Treatment in Good and Non-Responders—A Pilot Study of Migraine Patients" Journal of Clinical Medicine 10, no. 11: 2523. https://doi.org/10.3390/jcm10112523
APA StyleNowaczewska, M., Straburzyński, M., Meder, G., & Kaźmierczak, W. (2021). Changes in Cerebral Blood Flow after Erenumab Treatment in Good and Non-Responders—A Pilot Study of Migraine Patients. Journal of Clinical Medicine, 10(11), 2523. https://doi.org/10.3390/jcm10112523







